Exam 1 (Cardiac Phys- Pathology)
1/113
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
114 Terms
Cardiac Output
___________________ is the amount of blood the heart ejects per minute (L/min).
CO= Heart rate (bpm) x Stroke volume (mL)
Cardiac Output (L/min) is equal to _____________________ multiplied by _______________.
1. Vg Na+ channels open and cause depolarization to travel
2. Depolarization allows voltage gated "L type" Ca+ channel to open.
2. Extracelluar Ca+ rushes into muscle cell.
3. Excess Ca+ interacts with ryanodine receptor located on the sarcoplasmic reticulum.
4. Ryanodine receptor releases and Ca+ flows out of sarcoplasmic reticulum and remains intracellular.
5. Intracellular Ca+ interacts with troponin C, allowing myosin interaction to occur, and thus muscle contraction.
Describe the steps involved in the contraction of cardiac muscle.
T
True or False
Cardiac muscle depolarization relies on both extracellullary and intracellulary sourced Ca+.
A-V Bundle
In order for an impulse to pass from the atrium and into the ventricles, the impulse must pass through the ____________________ (specialized cardiac muscle).
F
While the heart is able to beat without nerve input, the atrial & ventricular muscle cells should never fire on their own in a healthy animal. Only the SA node, AV node, and Purkinje fibers have to ability to fire on their own. Their firing would allow for the atrial/ventricle muscle cells to depolarize(fire) and contract.
True or False
Atrial muscle and ventricular muscle are able to fire on their own, allowing the heart to beat without input from a nerve.
SA node is leaky to Na+ and Ca+. Ion's leak in and allow cell to depolarize.
Associated leaky channels:
-If(funny) Na+
-ICa(T) Transiant Ca+
-ICa(L) Long lasting Ca+
Why is the SA node able to fire on its own?
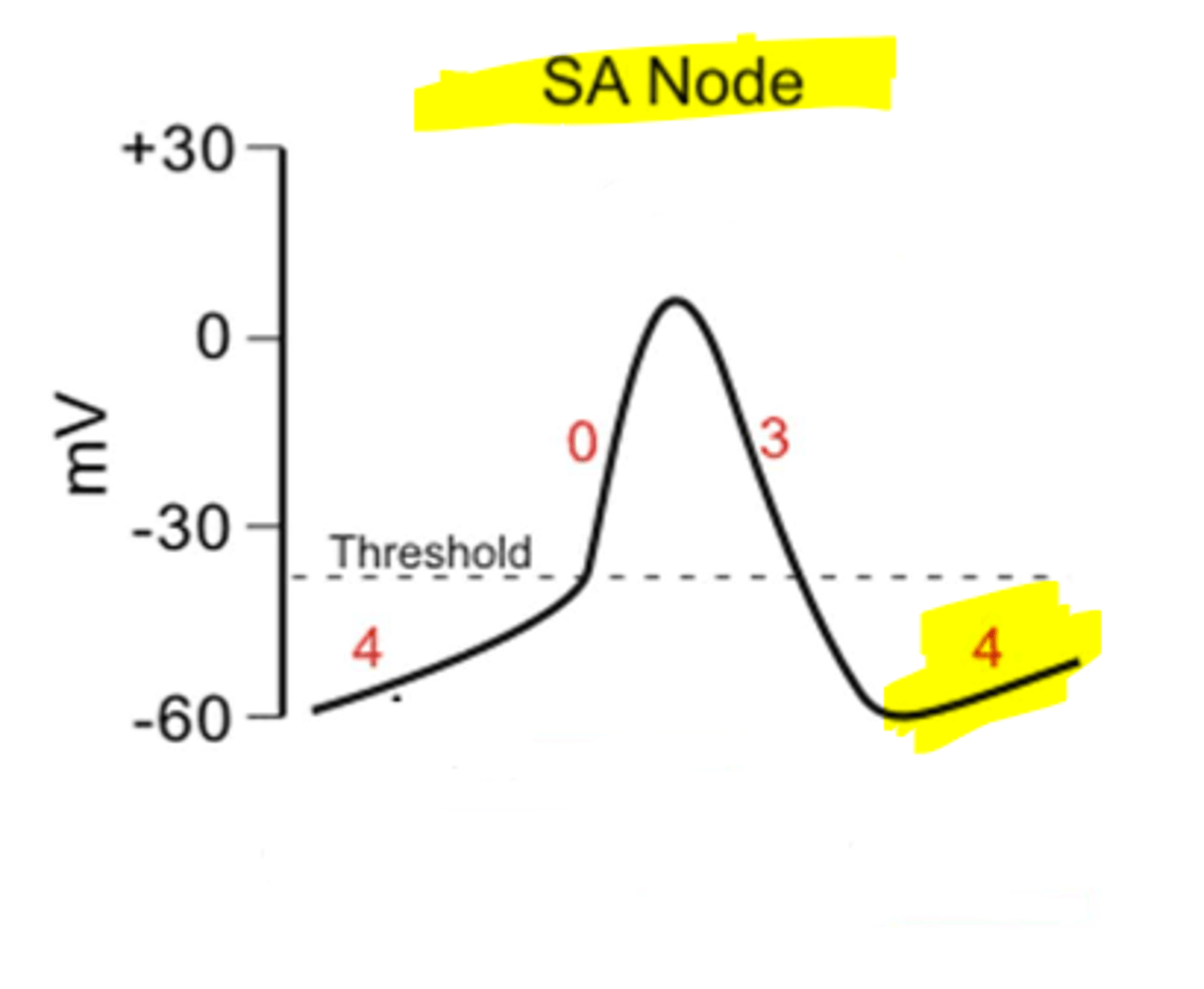
Post-ganglionic sympathetic nerves release norepinephrine and activates Beta-Adrenergic Receptors. Beta Adrenergic receptors make the SA Node more leaky to Na+ and Ca+, making it easier for the SA Node to fire. Increase SA Node firing means increased rate of conduction, increased excitability of all heart, and increased force on contraction.
Why does an increase in sympathetic stimulation lead to an increase in heart rate and force of contraction?
Post-ganglionic parasympathetic nerves release acetylcholine and acetylcholine interacts with muscarinic receptors. Activation of muscarinic receptors opens K+ channels, causing hyperpolarization of the SA node, meaning it is less likely to fire. Therefore, there is slower heart rate.
Why does an increase in parasympathetic (vagal) stimulation decrease heart rate?
Closure of the AV valves as the ventricle begins to contract, pushing blood back against the AV valves and forcing them to close.
This causes the 1st hear sound and signals that start of systole
The first heart sound is caused by ______________________.
All valves (AV valves and semilunar valves) are shut.
During isovolumetric contraction, the ventricle is contracting, causing an increase in pressure but no change in volume due to the closed valves.
During isovolumetric contraction, what valves are open? what valves are shut?
end diastolic volume - end systolic volume
*The heart is never completely full or empty. There is always some amount of blood left over in the ventricles. ESV is the volume of blood in the ventricle at the end of systole. EDV is the volume of blood in the ventricle at the end of diastole.
What is stroke volume?
Patient is likely in heart failure.
ejection fraction is the % of end diastolic volume ejected in each heart beat. Normal is considered 55% and higher.
A patient's ejection fraction is 40%. In general, what does this reflect about the patients overall cardiac health?
Patient's heart is functioning normally.
ejection fraction is the % of end diastolic volume ejected in each heart beat. Normal is considered 55% and higher.
A patients end diastolic volume is 100mL. During the ejection phase, 65mL are ejected by the heart. In general, what does reflect about the patients overall cardiac health>
Closure of the semilunar valves (aortic and pulmonic).
The semilunar valves close when the pressure in the ventricles falls below the pressure in the aorta/pulmonary artery. This begins diastole.
What causes the 2nd heart sound?
1. Isovolumetric Relaxation (all valves closed, decrease in ventricular pressure, no change in volume)
2. Ventricular Filling (once pressure in atria becomes greater than pressure in ventricles, AV valves open and blood passively fills ventricles; SA node fires and atria depolarizes/contracts and adds a little more blood to ventricle)
What are the phases of diastole?
1. Intrinsically: Starling Mechanism
2. Extrinsically: ANS (SANS increase HR; PANS decrease HR)
What are the 2 basic ways that the volume pumped by the heart is regulated?
Aortic Stenosis
Your stethoscope is over the aortic valve and you hear a murmur during systole. What type of heart murmur does this patient have?
pulmonic regurgitation
You are listening at the pulmonary valve and hear a murmur during diastole. What type of murmur is this?
diastolic murmur
A dog comes in with a history of mitral stenosis. When in the heart cycle would you expect to hear a murmur?
Tricuspid regurgitation
You are listening at the tricuspid valve and hear a murmur during systole. What type of murmur would you diagnosis the dog with?
Origin: SA Node
SA Node -->Atrial pathways-->Atrioventricular Node--> AV Bundle--> Left & Right Bundle Purkinje Fibers
Under normal conditions, where does the impulse pacing the heart originate? What path does this impulse take to move through the heart?
atrial depolarization
What produces the P wave?
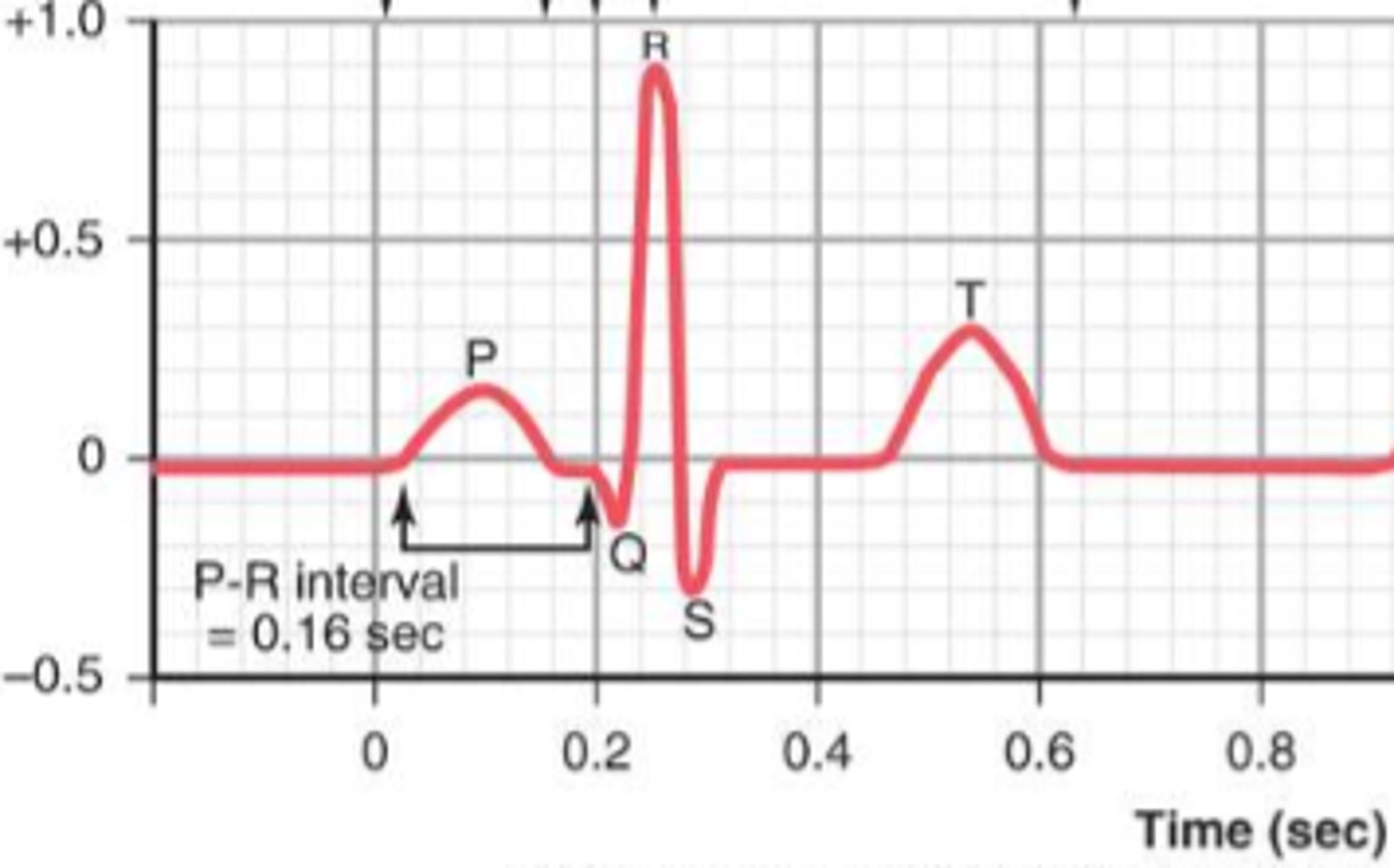
ventricular depolarization
What produces the QRS complex?
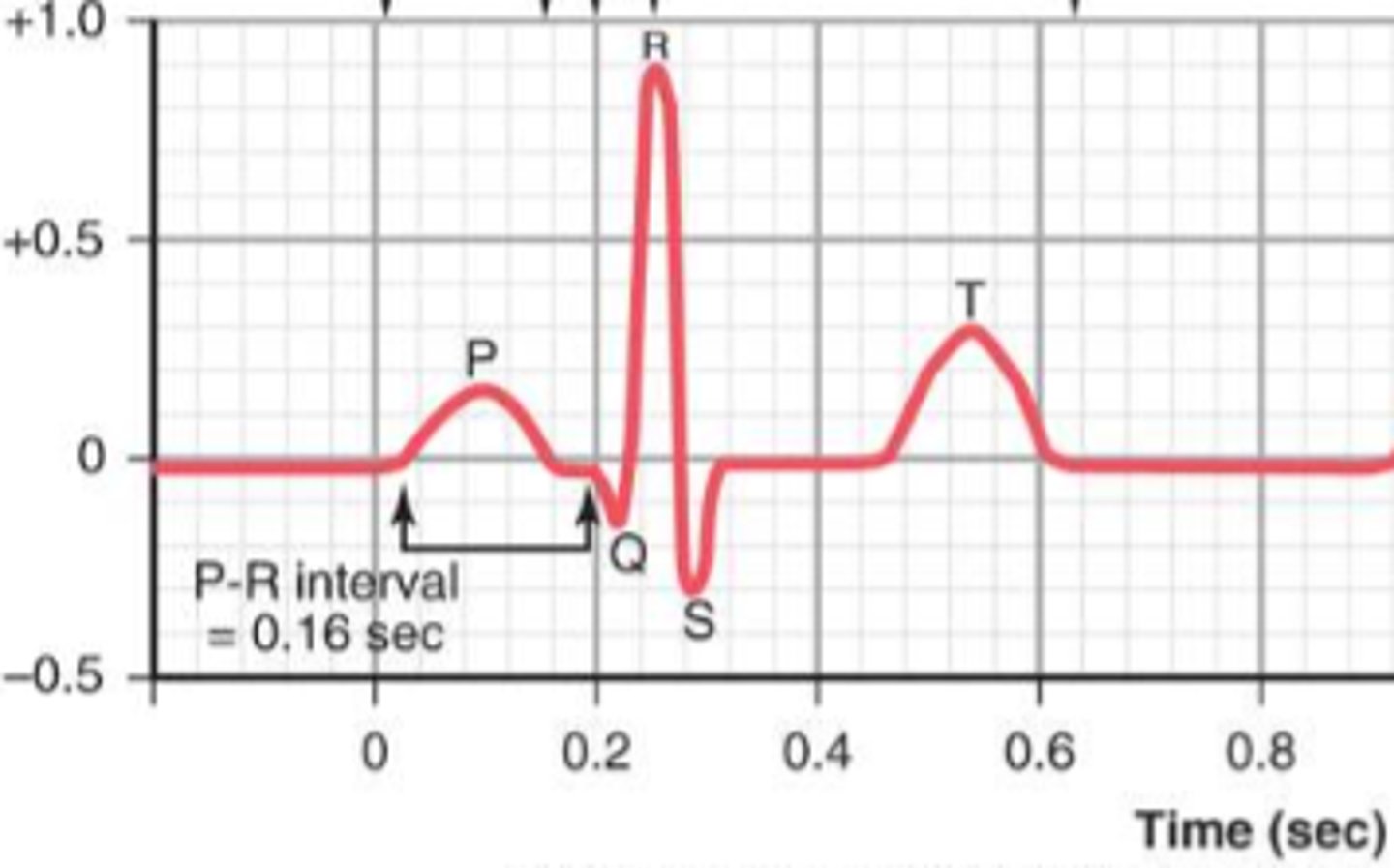
ventricular repolarization
What produces the T wave?
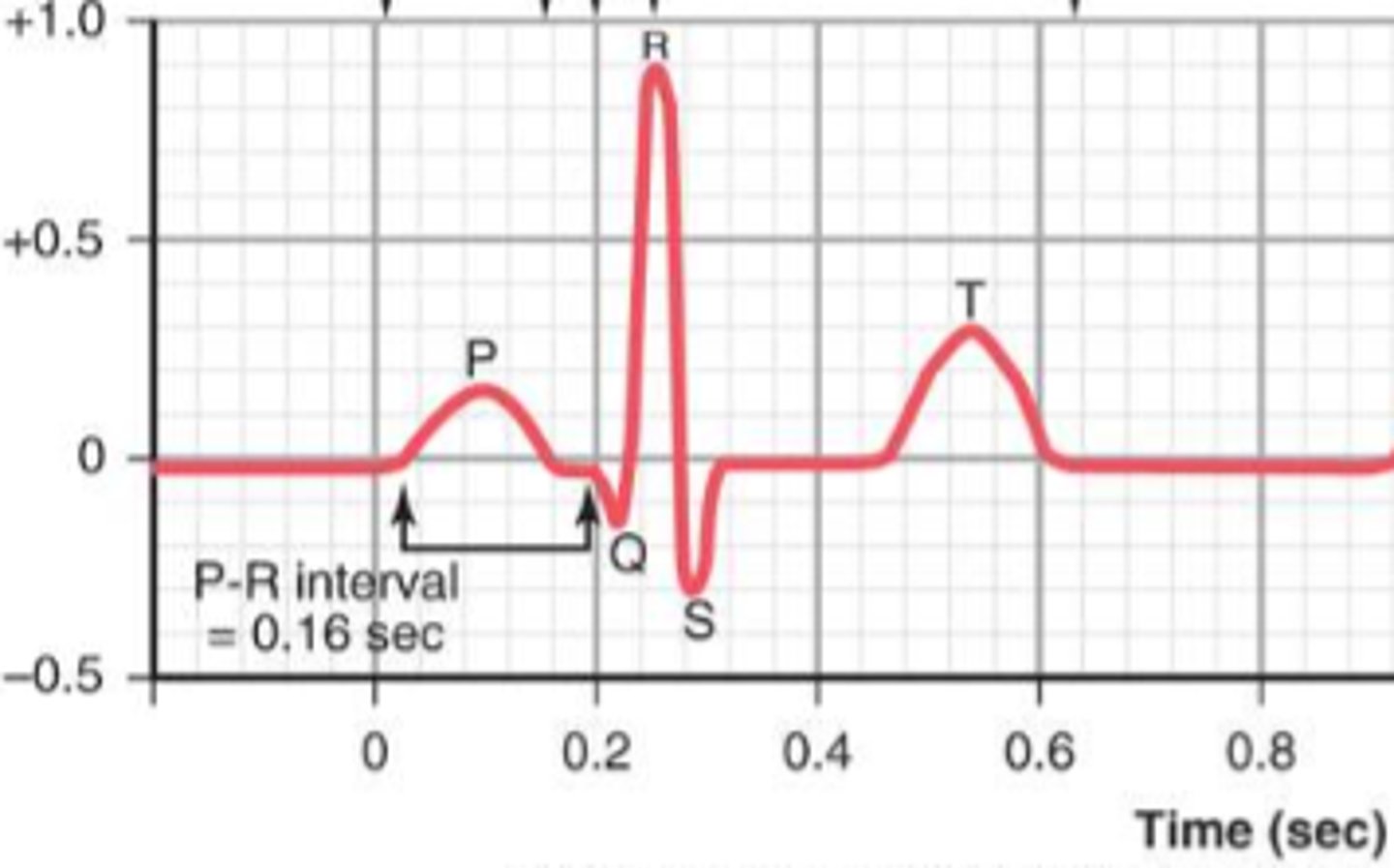
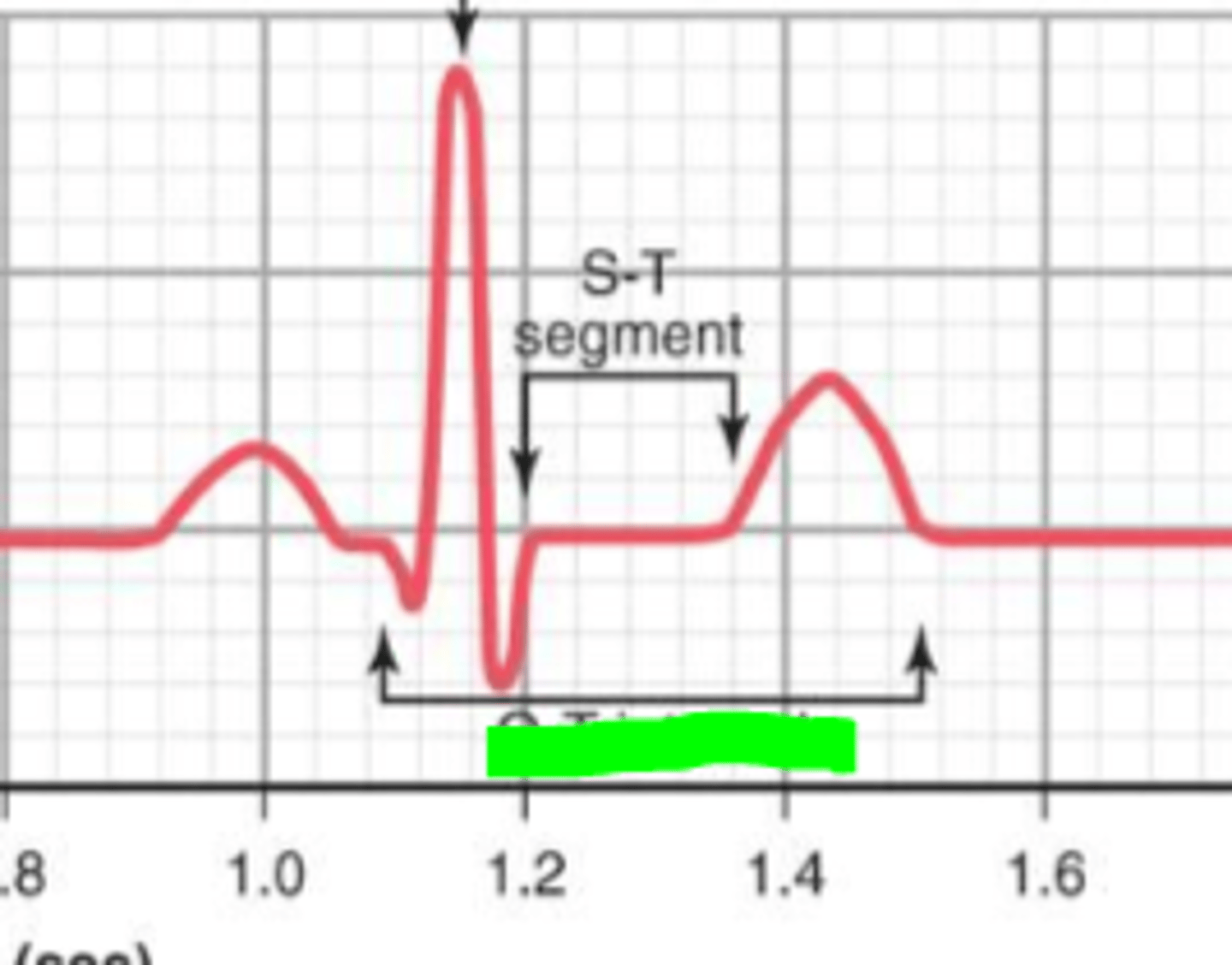
P-R interval: time between the electrical excitement of the atria and the beginning of the electrical excitement of the ventricle
What the does green interval represent?
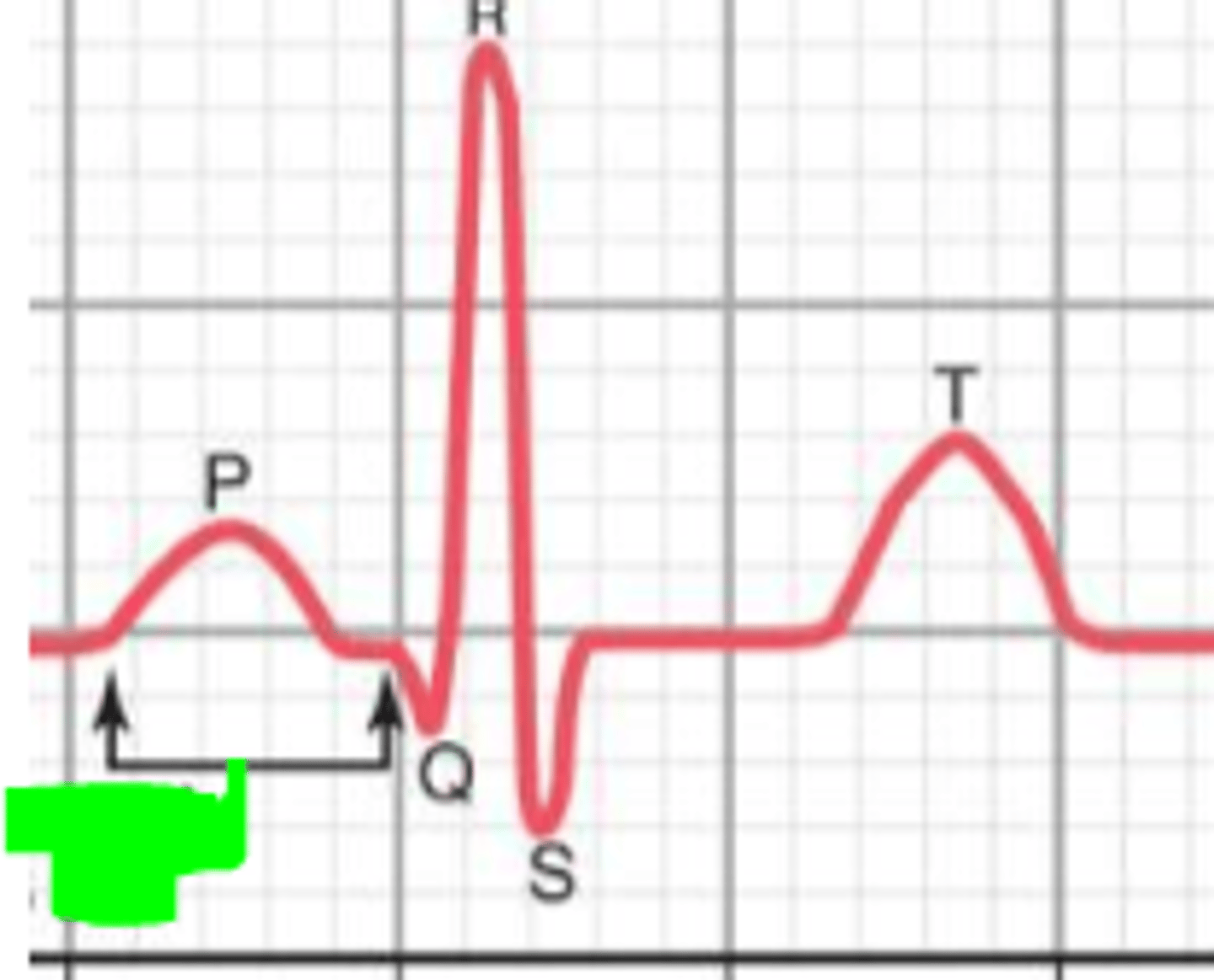
Q-R interval represents the approximate time of ventricular contraction
What does the interval in green represent?
Multiply the number of QRS complexes in 3 seconds (30 large squares) by 20.
How do you calculate the average heart rate of a patient from an EKG? Assume paper speed is at 50mm/sec.
50mm/sec: count # of small boxes in one R-R interval and divide into 3000.
25mm/sec: count # of small boxes in one R-R interval and divide into 1500.
How do you calculate the instantaneous heart rate from an EKG paper at 50mm/sec? What about 25mm/sec)
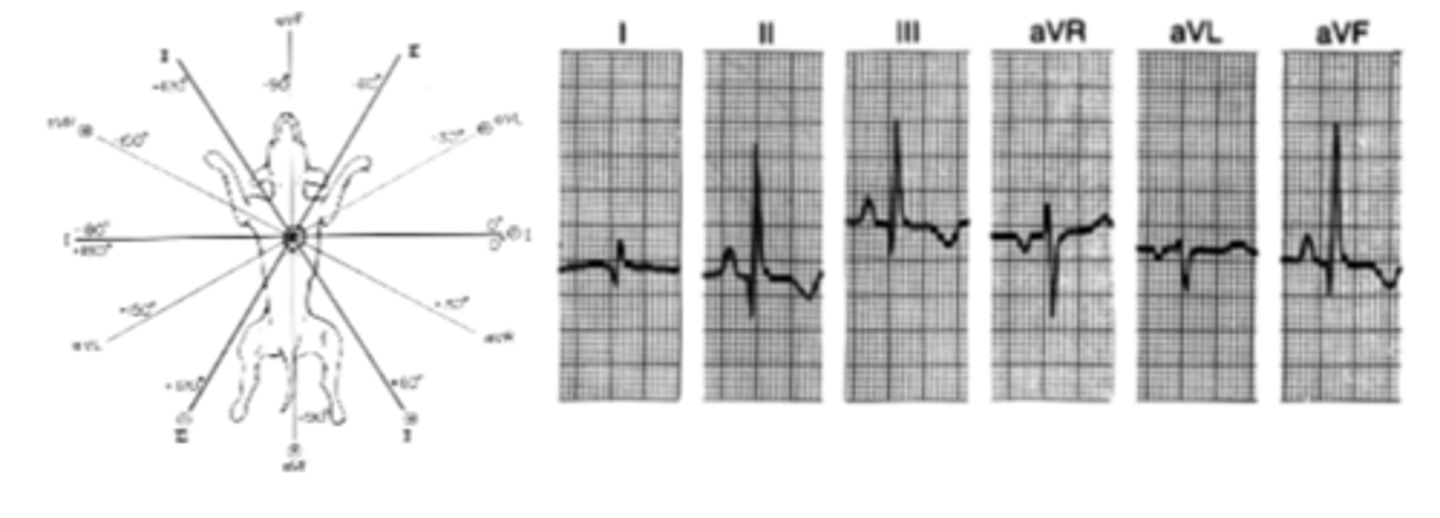
MEA: 90 degrees
Normal MEA for dogs (40-100) & cat (0-160)
What is the Mean Electrical Axis of this dog? Is it normal or abnormal? What if this was a cat?
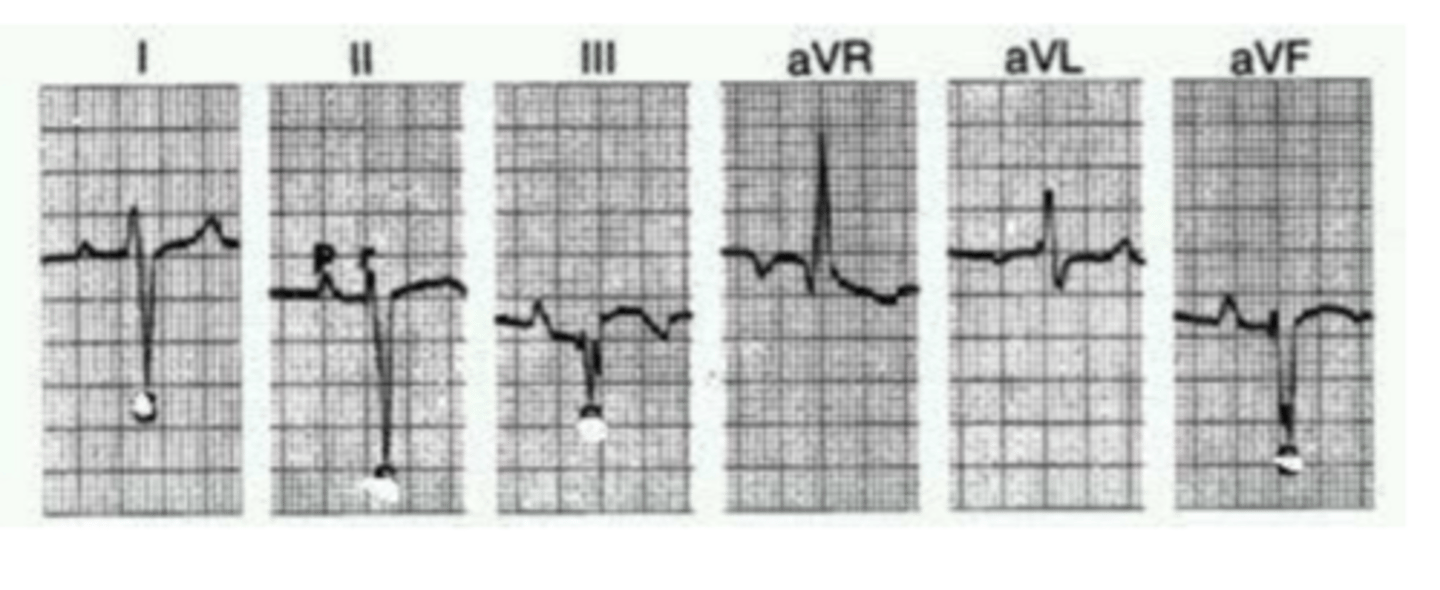
MEA: -120 degrees
Abnormal for cats and dogs
What is the Mean Electrical Axis of this dog? Is it normal or abnormal? What if this was a cat?
Multiple number of QRS complexes in 6 seconds (30 large squares) by 10.
How do you calculate the average heart rate of a patient from an EKG? Assume paper speed is at 25mm/sec.
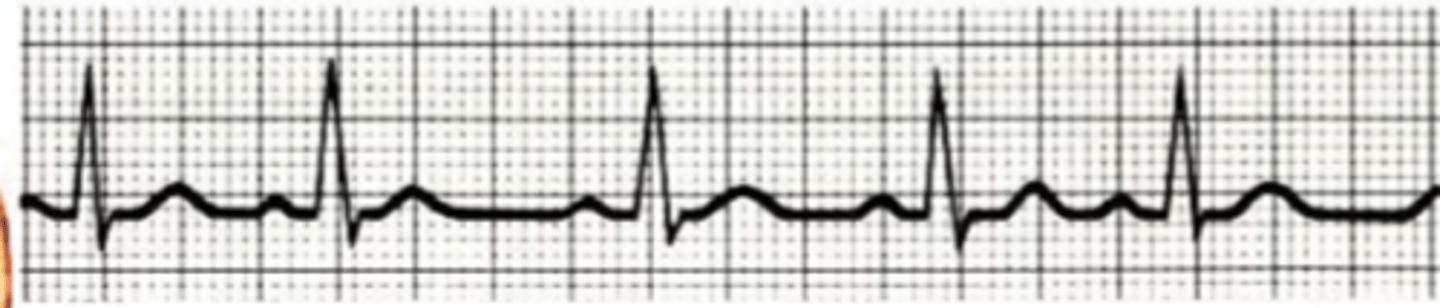
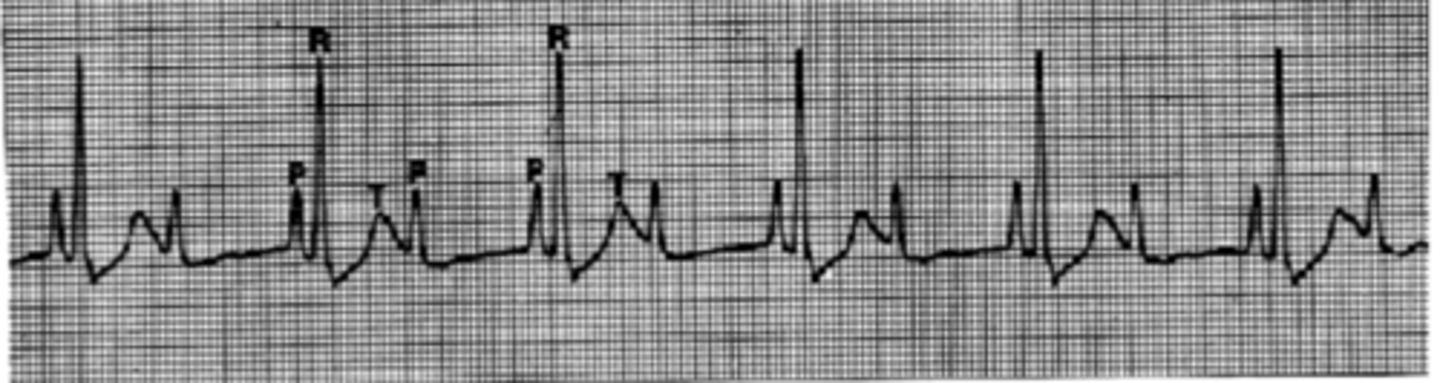
Sinus arrhythmia (normal arrhythmia)
Describe the arrhythmia.
Wandering pacemaker (normal arrhythmia)
Describe the arrhythmia
Dog: 70-160 bpm
Cat: 140-220 bpm
What is the normal heart rate of a dog? Of a cat?
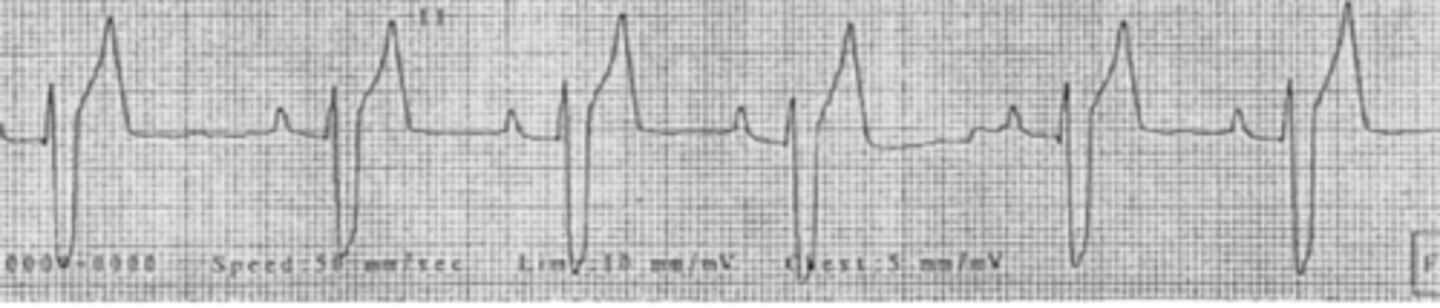
Right Bundle branch block (peep dat deep and wide S wave
Describe the heart rhythm shown by lead II
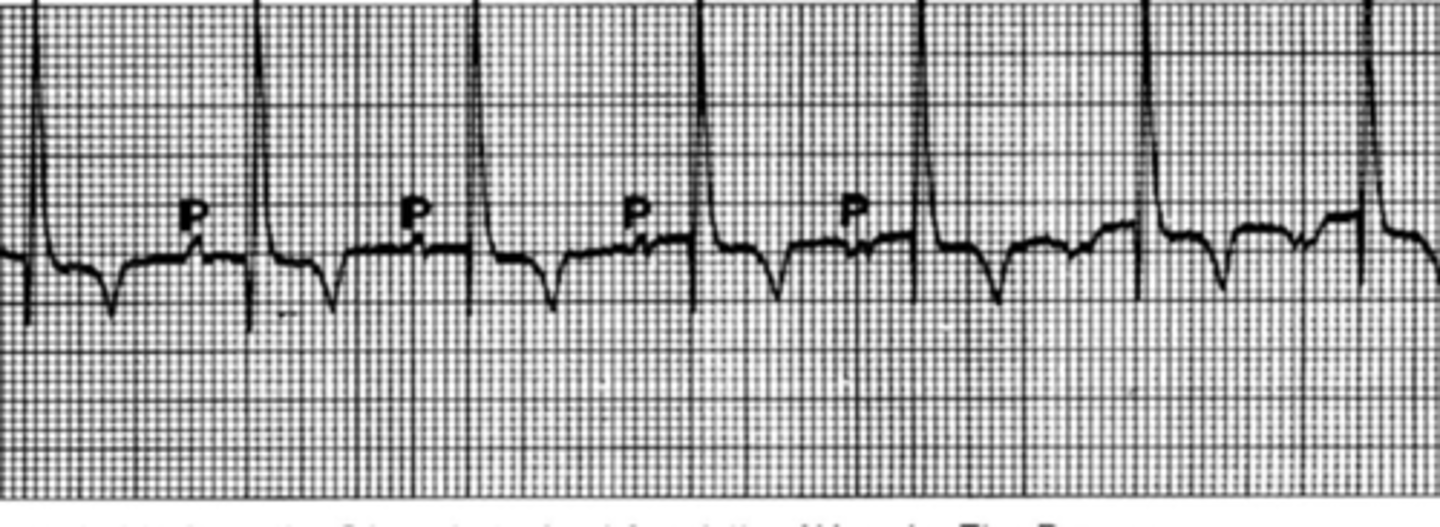
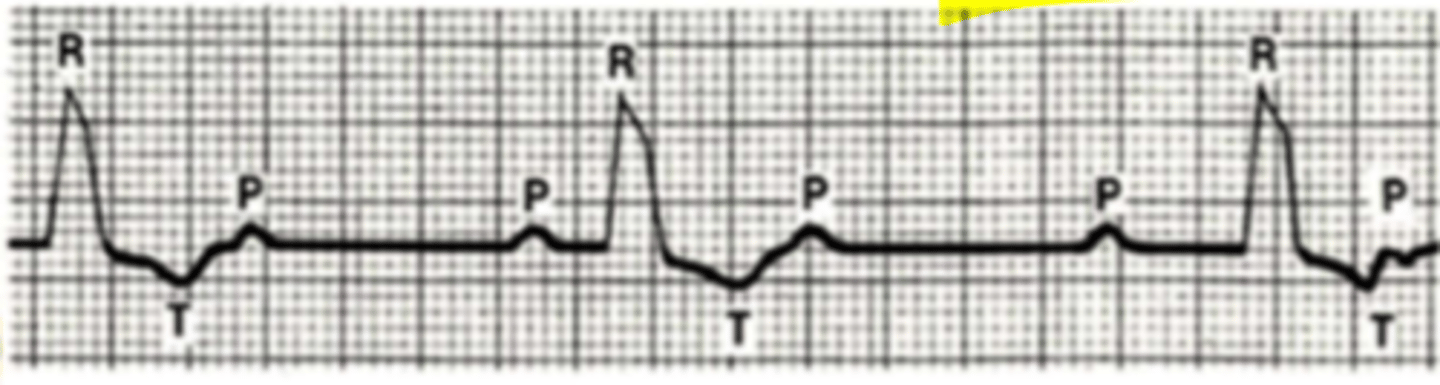
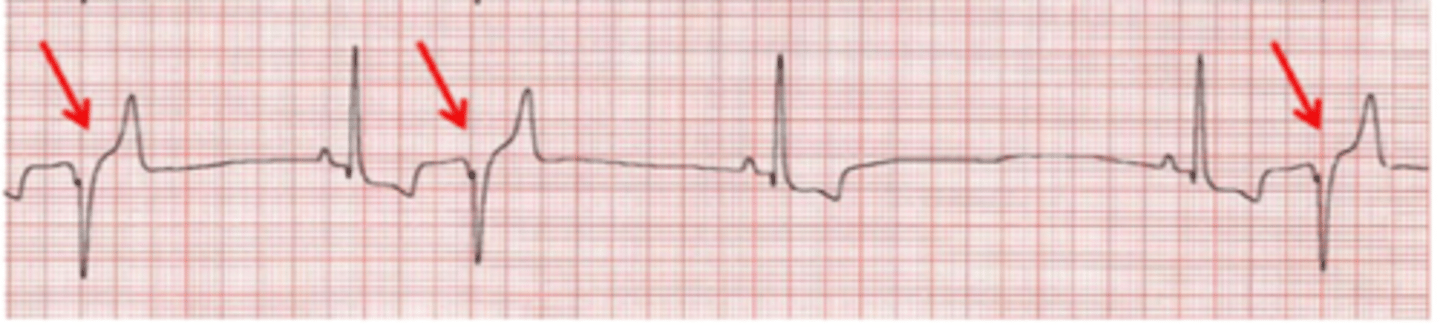
Second degree AV Block: Type 1
*There is a progressive lengthening of the PR interval and then a dropped beat
Describe the heart rhythm
Second degree AV Block: Type 2
*sudden drop beats without lengthening of PR interval
Describe the heart rhythm
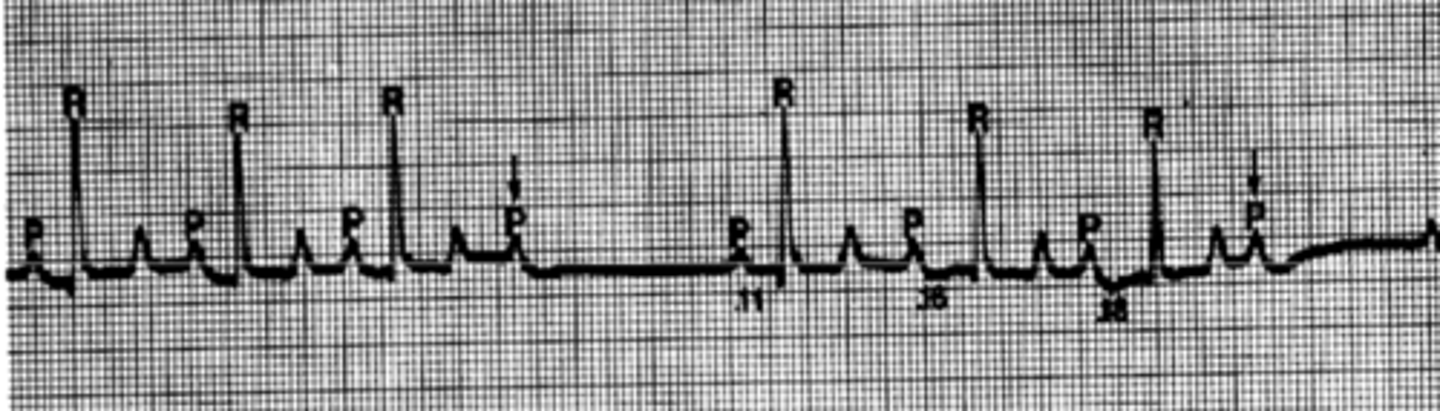
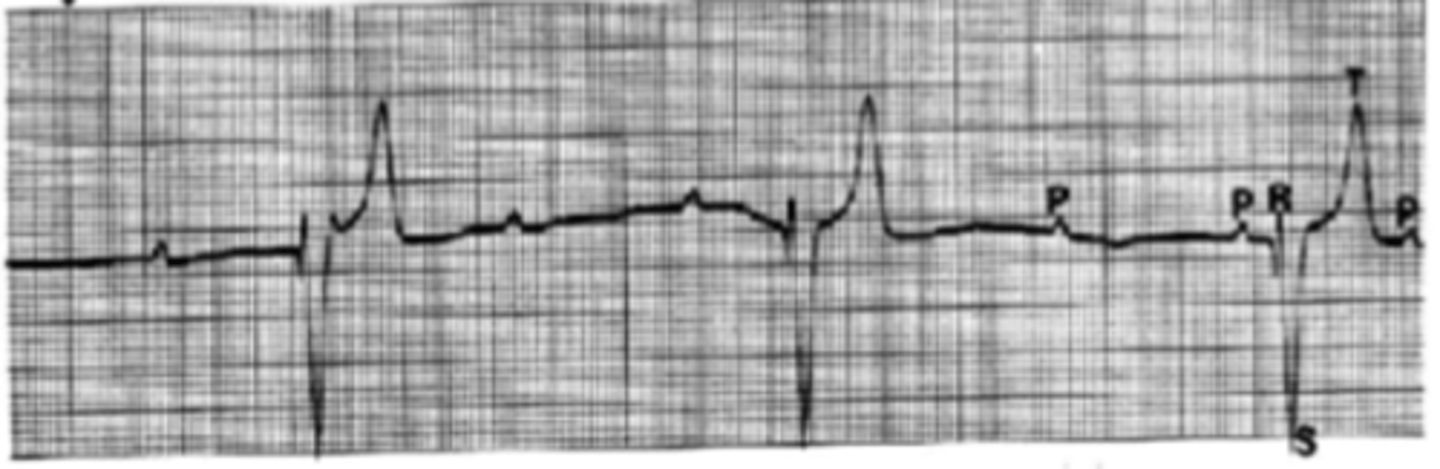
Third degree AV Block
*No correlation between P waves and QRS wave. Atria and Ventricle contractions are not coordinated. Since there is a wide and bizarre R wave, ventricular depolarization is starting in right bundle branch
Describe the EKG of lead II
Third degree AV Block
*No correlation between P waves and QRS wave. Atria and Ventricle contractions are not coordinated. Since there is a wide and bizarre S wave, ventricular depolarization is starting in left bundle branch
Describe EKG of lead II
Atrial Premature Contraction
Describe EKG
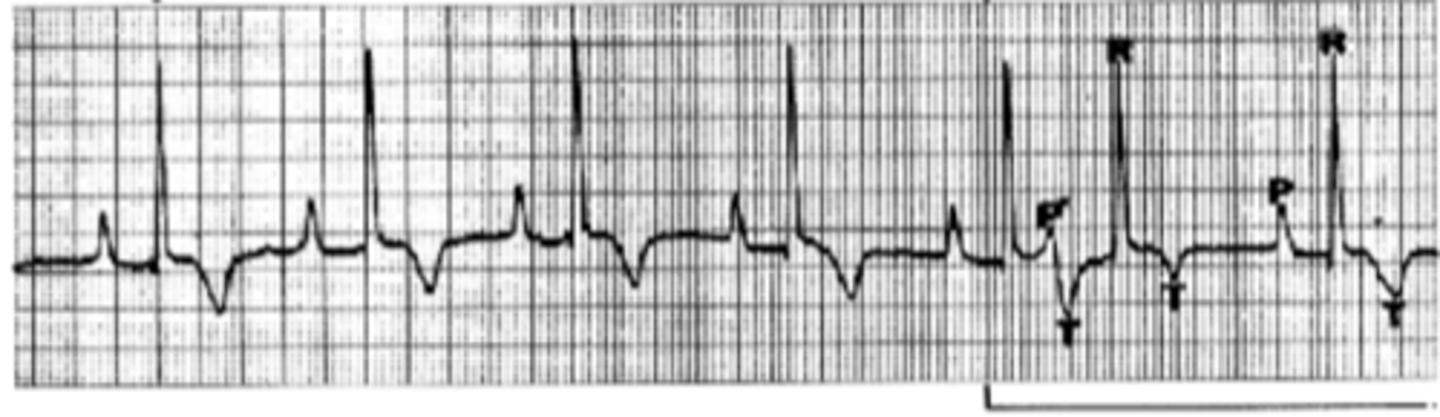
Ventricular Premature Contraction
*QRS complex is wide & bizarre, No P wave before contraction.
Describe EKG
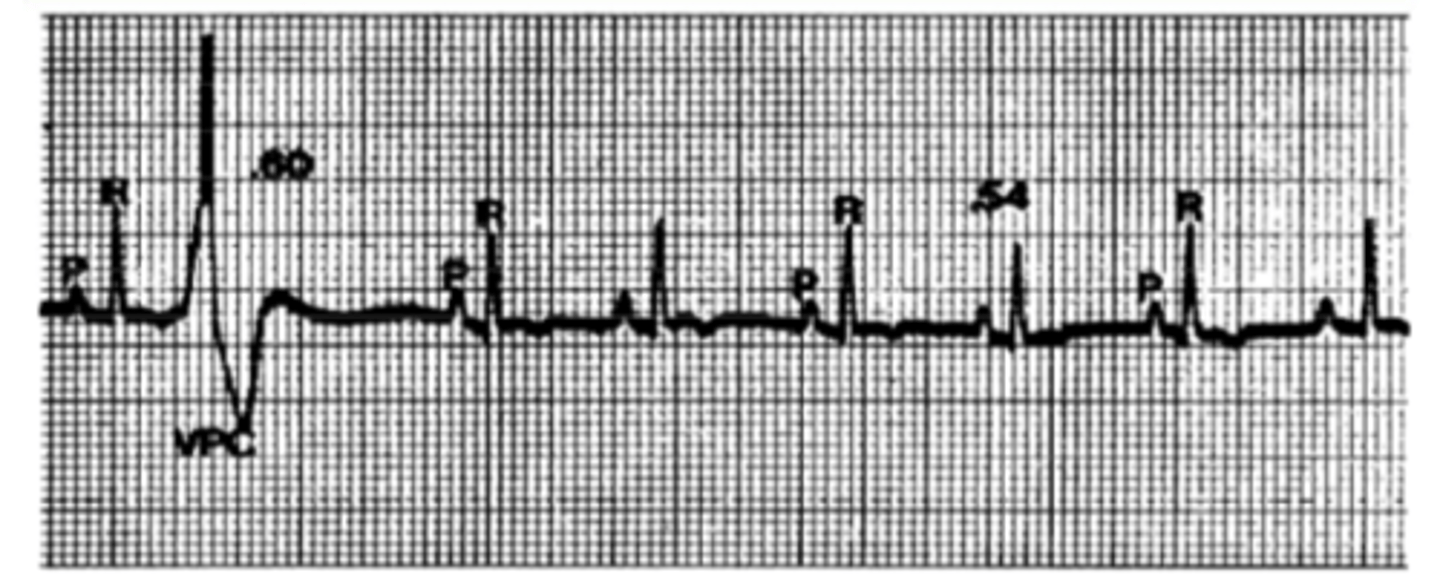
Ventricular Premature Contraction
*QRS complex is wide & bizarre, No P wave before contraction.
Describe EKG
tacchycardia
If a dog experiences 3 premature ventricular contractions in a row, it is referred to as ________________
Paroxysmal Atrial Tachycardia
*QRS normal, so impulse is starting in atria. Paroxysmal because it is a sudden burst. Tachycardia because there are 3 or more.
Describe EKG
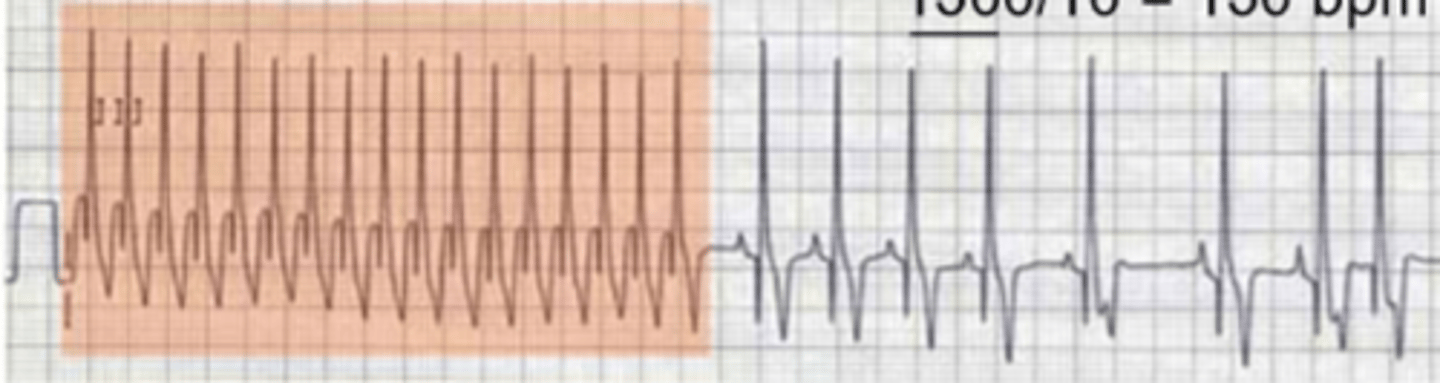
Paroxysmal Ventricular Tachycardia
Describe EKG
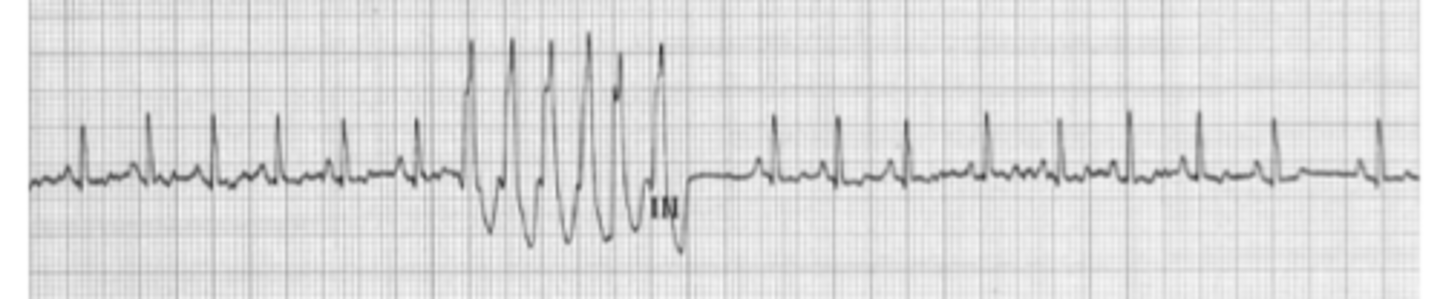
Atrial Fibrillation
*Normal QRS, No distinct P waves
Describe EKG
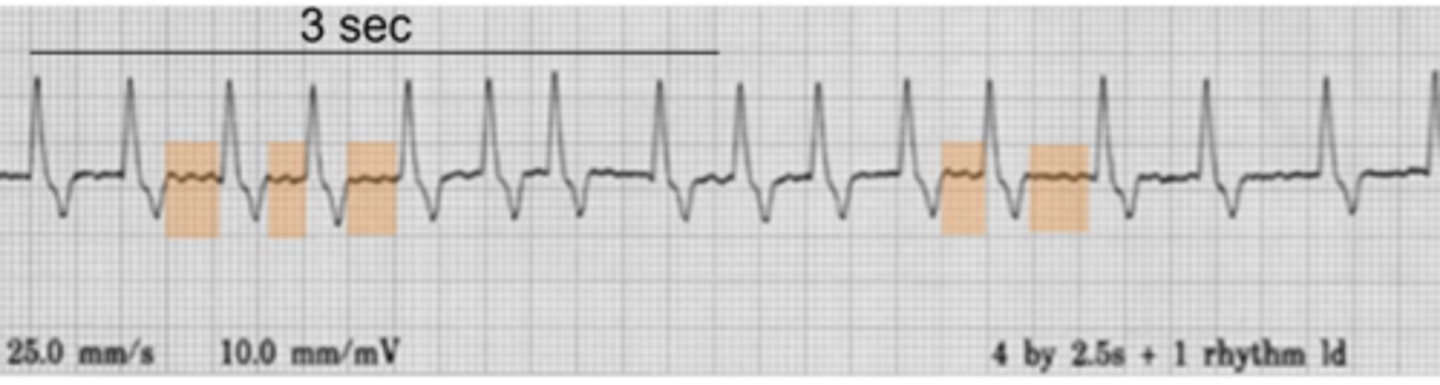
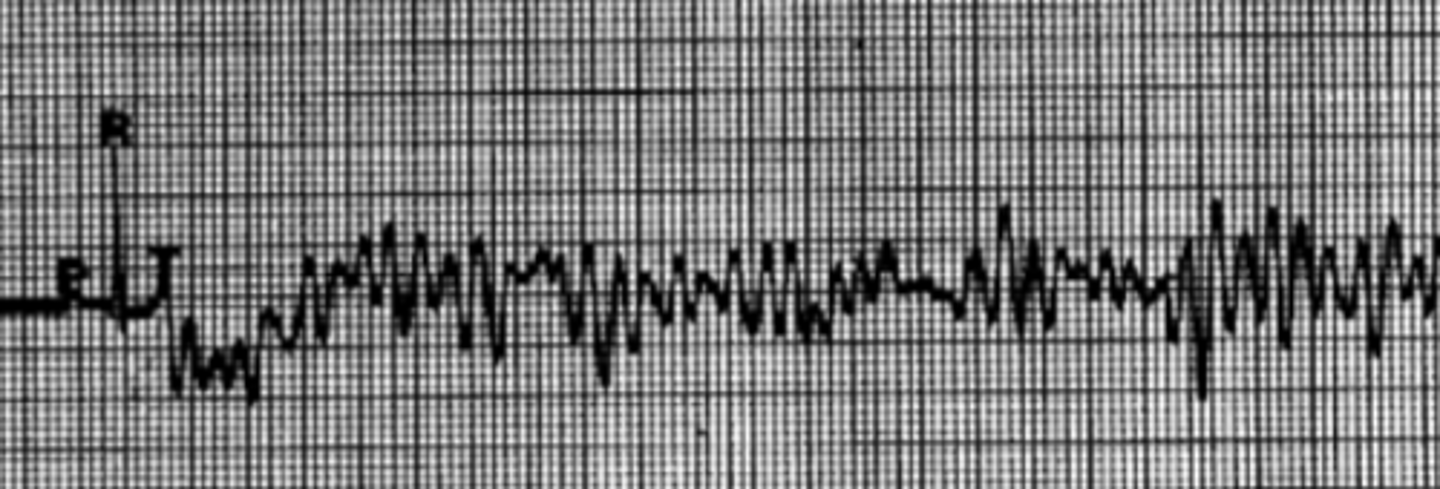
Ventricular Fibrillation
*ventricles are quivering rather than contracting. Pulse is likely not detectable.
Describe EKG
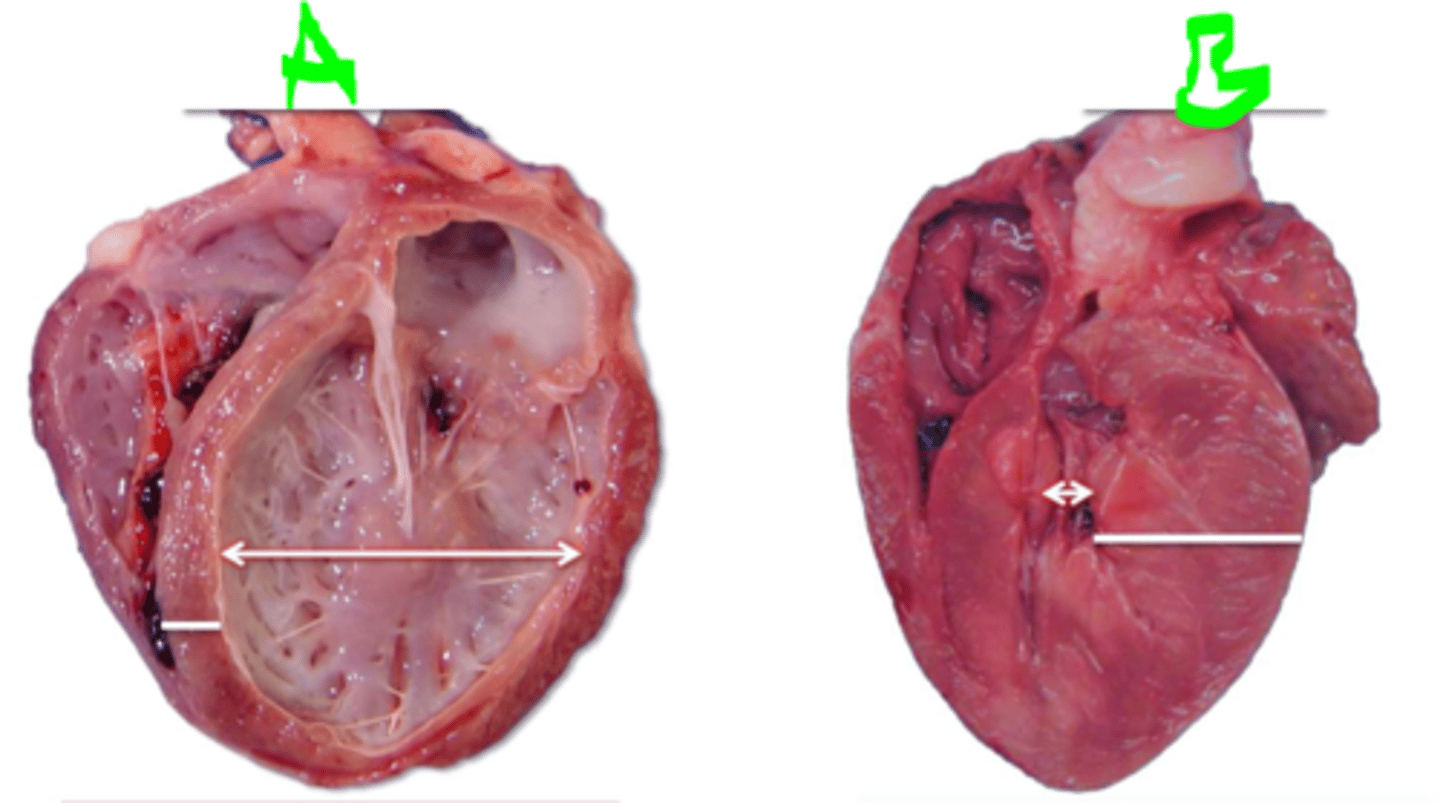
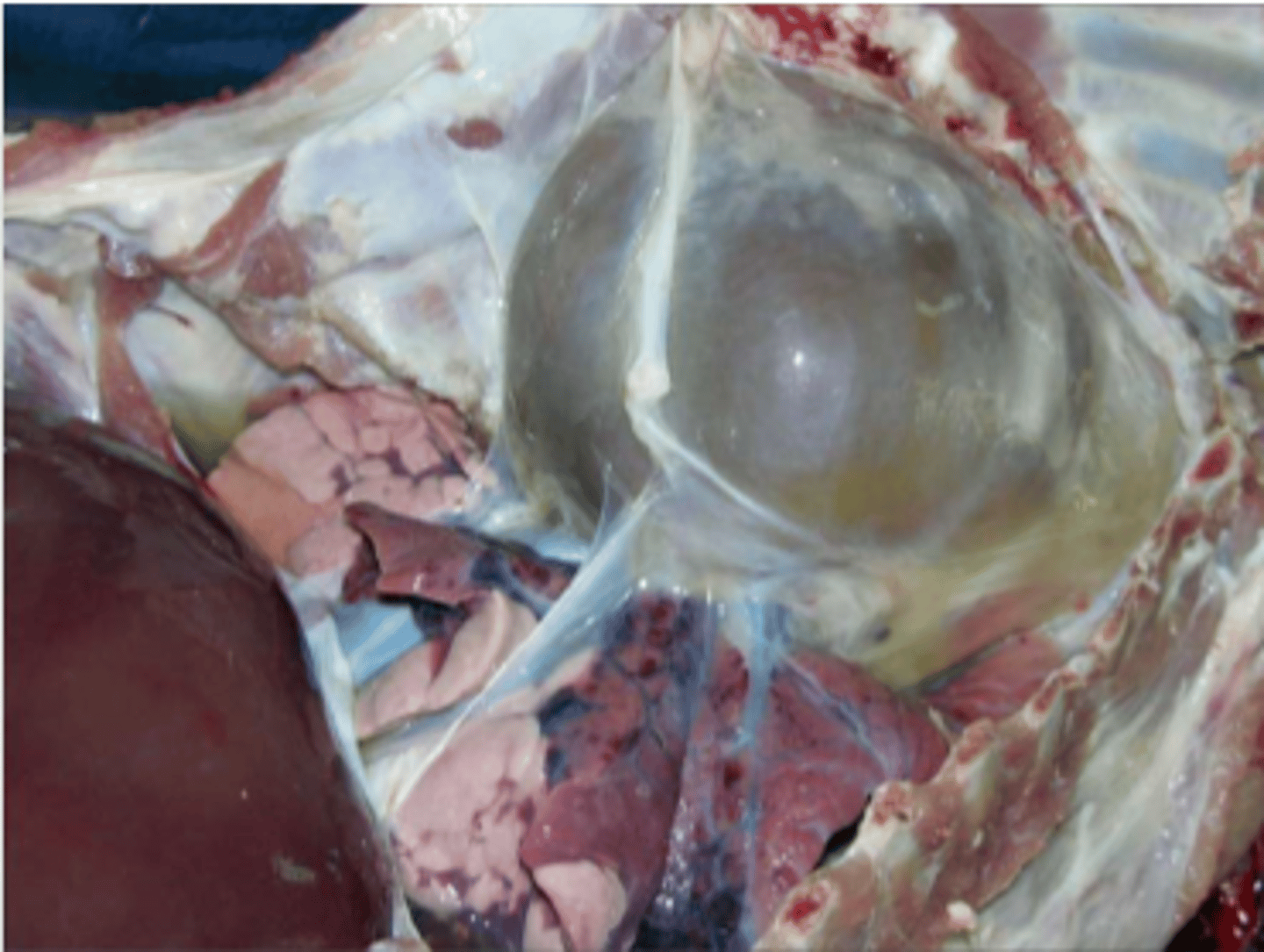
Under pressure-overload, heart undergoes concentric hypertrophy in order to compensate. (heart is working harder to pump out, increase cardiomyocyte size)
examples causing pressure-overload:
-aortic stenosis
-arterial hypertension
-resistance training
A healthy heart encounters chronic pressure-overload. The heart undergoes [concentric/eccentric] hypertrophy in order to compensate. What are some examples that would cause pressure overload in the heart?
![<p>A healthy heart encounters chronic pressure-overload. The heart undergoes [concentric/eccentric] hypertrophy in order to compensate. What are some examples that would cause pressure overload in the heart?</p>](https://knowt-user-attachments.s3.amazonaws.com/42a5d1ae-e19a-4724-8372-a2139e053ad8.png)
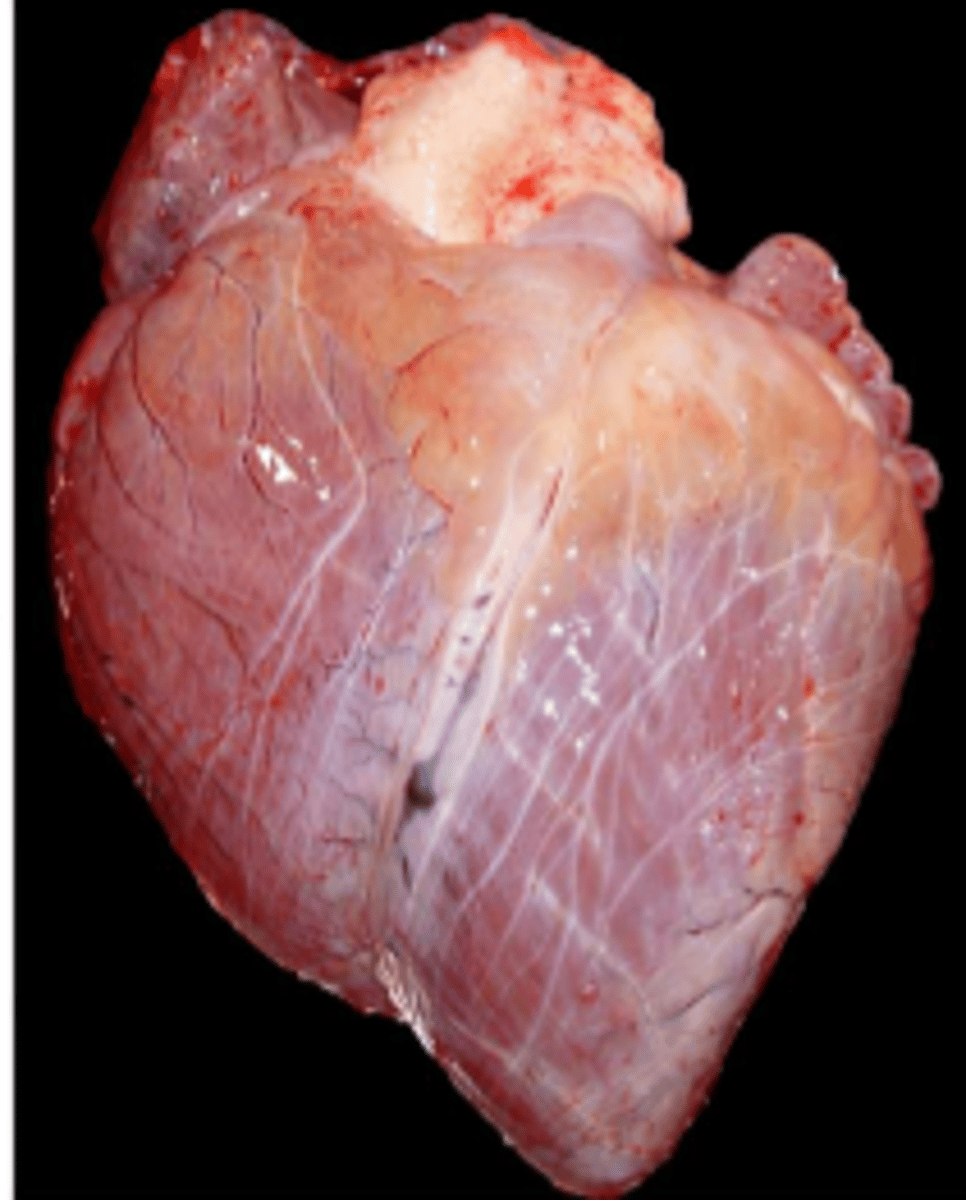
With volume over-load, the heart would undergo eccentric hypertrophy in order to compensate (heart dilates but still increase cardiomyocyte size)
examples causing volume overload:
-valvular regurgitation
-endurance training
A healthy heart encounters chronic volume-overload. The heart undergoes [concentric/eccentric] hypertrophy in order to compensate. What are some examples that would lead to volume overload in the heart?
![<p>A healthy heart encounters chronic volume-overload. The heart undergoes [concentric/eccentric] hypertrophy in order to compensate. What are some examples that would lead to volume overload in the heart?</p>](https://knowt-user-attachments.s3.amazonaws.com/45bd73e3-af4d-4cde-b218-c60200583415.png)
Valvular insufficiency
*causes blood to flow back into the ventricles, causing ventricles to stretch
Which of the following increases the preload on the ventricles? There may be more than one correct answer.
AV valve stenosis
Valvular insufficiency
Pericardial disease
Outflow tract stenosis
Hypertension
Semilunar valve stenosis
AV valve stenosis and pericardial diseases
Which of the following decreases the preload on the ventricles? There may be more than one correct answer.
-AV valve stenosis
-Valvular insufficiency
-Pericardial disease
-Outflow tract stenosis
-Hypertension
-Semilunar valve stenosis
semilunar valve stenosis
hypertension
outflow tract stenosis
*all of these increase the pressure the heart must work against in order to eject blood out during systole
Which of the following increases the afterload on the ventricles? There may be more than one correct answer.
-AV valve stenosis
-Valvular insufficiency
-Pericardial disease
-Outflow tract stenosis
-Hypertension
-Semilunar valve stenosis
nutmeg liver
Which of the following pathogenic lesions is associated with right-sided heart failure? Nutmeg liver, heart failure cells, pulmonary edema, & subaortic stenosis
Increased diastolic volume stretches myofibers. Increased volume also requires more force to eject additional blood out, therefore there is an increase in contractile force. This allows for the increased stroke volume and cardiac output.
Why does a chronic increase in diastolic volume lead to an eccentric hypertrophied heart?
T
True or False
Physiological hypertrophy causes a mild increase in heart weight, but still allows for normal cardiac function.
F
there will be depressed cardiac function
True or False
Pathological hypertrophy causes a significant increase in heart weight (up to 4x), causing the heart to have increased function.
Physiological: capillary network increased and sufficient for nourishment
Pathological: capillary network insufficient for nourishment/oxygenation
What happens to the capillary network of the heart when the heart experiences physiological hypertrophy? What if the heart experiences pathological hypertrophy?
Physiological: unchanged or decreased fetal gene expression
Pathological: increase fetal gene expression
What happens to the expression of fetal gene in the heart when the heart experiences physiological hypertrophy? What if the heart experiences pathological hypertrophy?
A: eccentric (peep the then ventricular wall and distended ventricle)
B: concentric (peep the thick ventricular wall and reduced ventricular chamber)
Which heart represents an eccentric hypertrophy of the heart? Which represents concentric hypertrophy of the heart?
1. Initiation: increase cell size
2. Compensation: stable hyperfunction
3. Deterioration: degeneration of hypertrophied cardiomyocytes (loss of contractility/compliance)
What are the cellular stages of cardiac hypertrophy?
Heart would have a very broad base (heart 2 in image)
caused by pulmonic stenosis or pulmonic hypertension b/c right side is having to contract harder to eject blood
Describe the gross appearance of a heart that has undergone right-side cardiac hypertrophy. Which of the following may lead to right-sided hypertrophy?
-Pulmonic stenosis
-Aortic stenosis
-Mitral valve disease
-HCM
-Pulmonary hypertension
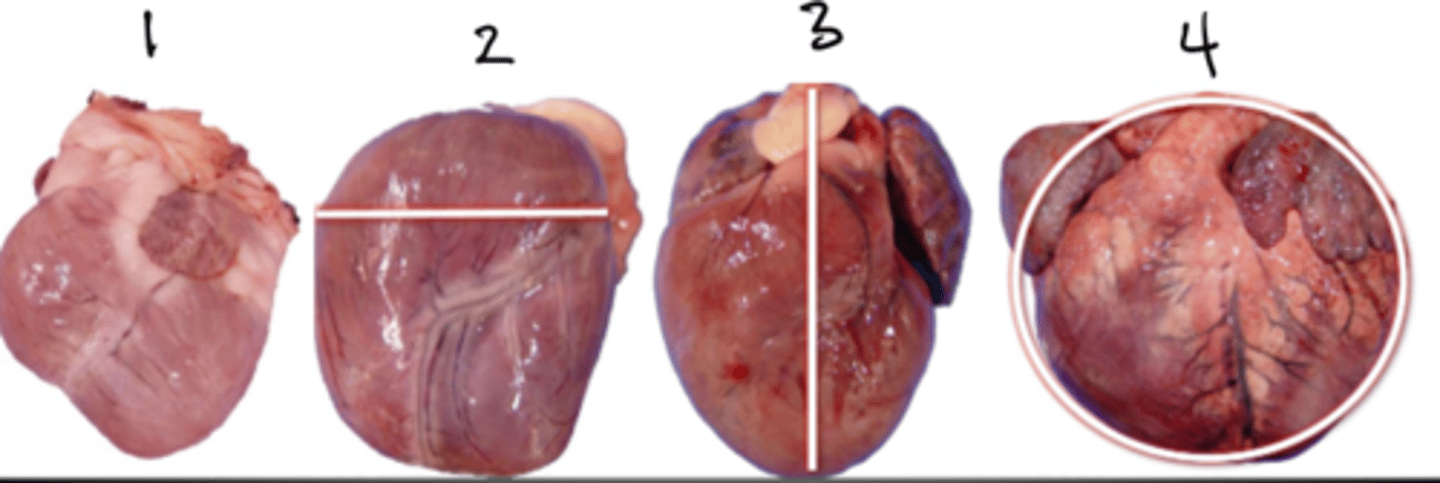
Heart would have increased length (heart 3 in image)
caused by mitral valve disease, aortic stenosis, or HCM
Describe the gross appearance of heart that has undergone left-sided cardiac hypertrophy. Which of the following may lead to left-sided hypertrophy?
--Pulmonic stenosis
-Aortic stenosis
-Mitral valve disease
-HCM
-Pulmonary hypertension
18
In cats, a heart weight more than ________ grams is considered hypertrophied irrespective of the cats body weight.

2.8-4
The normal ratio of (LV+S/RV) in mature animals is:
A. <2.8
B. 2.8-4
C. >4.0
>4
The ratio of (LV+S/RV) in mature animals with left ventricular hypertrophy is:
A. <2.8
B. 2.8-4
C. >4.0
<2.8
The ratio of (LV+S/RV) in mature animals with right ventricular hypertrophy is:
A. <2.8
B. 2.8-4
C. >4.0
Both are signs of heart failure.
Backward heart failure is the inability to empty the venous reservoirs.
Forward heart failures is decreased blood flow via the great vessels.
Compare and Contrast "backward heart failure" and "forward heart failure"
Right sided heart failure led to system venous congestion, causing generalized edema and therefore a more congested liver.
ex of R-sided heart failure: pulmonic stenosis, pulmonary hypertension, tricuspid dysplasia.
A patient with a history of heart disease is found to have a "nutmeg liver" at necropsy. What type of heart failure did the patient have? Why did the liver undergo these pathological changes?
Left-sided heart failure caused pulmonary venous congestion, leading to pulmonary edema and increases in intra-alveolar macrophages. The alveolar macrophages phagocytose RBCs, taking up hemosiderin and therefore iron.
ex of L sided heart failure: mitral valve disease, aortic stenosis, HCM
A patient with a history of heart disease is found to have "heart failure cells" present. What type of heart failure did the patient have? Where were these cells found and why did this region undergo these pathological changes?
bilateral heart failure
A ventricular septal defect is most likely to result in which type of heart failure:
left sided
bilateral
right sided
1. Ductus venosus (umbilical to IVC; bypass liver)
2. Foramen ovale (RA-->LA)
3. Ductus arteriosus (Pulmonary A-->Aorta)
What are the 3 main fetal shunts? What are their purposes in fetal lfie?
PDA: volume overload
blood leaving aorta will flow the the area with lowest pressure (ie pulmonary artery). This increases BF to lungs and thus LA and LV, leading to an increase in overall blood volume. Overall causes LV eccentric hypertrophy.
A patient with Patent Ductus Arteriosus (PDA) would most likely cause [volume/pressure] overload. Why?
ASD: volume overload
blood shunts from LA to RA, increasing the blood volume entering the RV and causing volume overload of RV. Overall causes RV eccentric hypertrophy.
A patient with Atrial Septal Defect (ASD) would most likely cause cardaic [volume/pressure] overload. Why?
Ventricular septal defect (VSD): volume overload
blood from L ventricle flows back to RV; Increase volume in RV; This excess volume is pumped to lungs an thus LA and LV; equalization of pressures across ventricles; LV and RV hypertrophy.
A patient with a Ventricular Septal Defect (VSD) would most likely cause cardiac [volume/pressure] overload. Why?
Aortic stenosis: pressure overload
It is harder for blood to leave the L V, so the heart must increase pressure in order to expel blood.
A patient with Aortic stenosis would most likely suffer from cardiac [volume/pressure] overload. Why?
Pulmonic stenosis: pressure overload
harder for blood to flow through pulmonic valve, so heart must increase pressure to allow for blood flow into lungs
A patient with Pulmonic stenosis would most likely suffer frmo cardiac [volume/pressure] overload. Why?
In rare cases of PDA, there is such high pulmonary hypertension that blood shunts from the pulmonary artery into the aorta, bypassing the lungs. This leads to an increased amount of deoxygenated blood entering the systemic circulation, increasing risk of cyanosis.
(this is referred to as Eisenmenger syndrome)
Why may a patient with Patent Ductus Arteriosus suffer from cyanosis? aka Eisenmenger syndrome
horses and cattle
While ventricular septal defects occur in all species, what two species experience ventricular septal defects more often?
-horses
-cats
-dogs
-cattle
-sheep
-llammas
-pigs
High VSD: defect in membranous portion of septum (more common)
Low VSD: defect in muscular portion of septum
There are two different types of ventricular septal defects- High VSD and Low VSD. What is the difference between them? Which is more common?
VSD results in LV and RV hypertrophy :)
Typically, VSD causes blood to shunt from the L ventricle into the right ventricle, increasing the amount of volume in the RV. Pressure equalizes across the ventricles. LV and RV hypertrophy.
Ventricular septal defects result in [LV/RV] hypertophy. Why?
Stenotic valve restricts outflow
Pressure overload of RV
RV concentric hypertrophy
Right heart failure
What are the hemodynamic consequences of a patient suffering from pulmonic stenosis?
Stenotic valve restricts outflow, causing pressure overload of LV and resulting in LV concentric hypertrophy.
In severe enough cases, this can lead to R heart failure or life-threatening arrhythmias
What are the hemodynamic consequences of a patient suffering from subaortic stenosis?
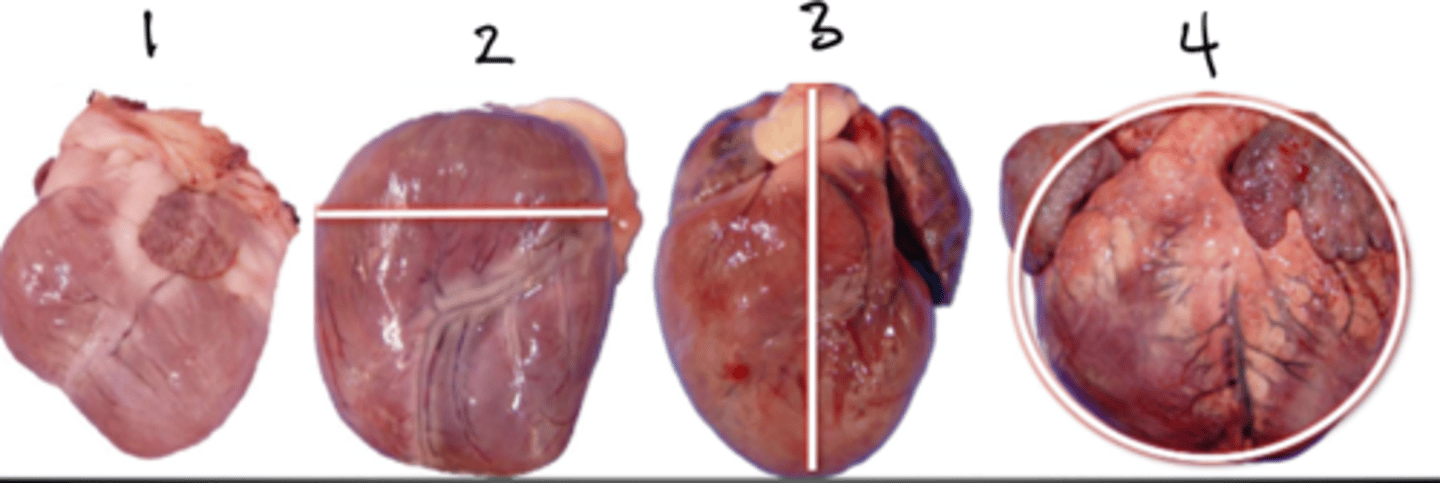
hydropericardium
-Occurs due to increased hydrostatic pressure/R heart failure
-Occurs due to hypoproteinemia (emaciation, protein losing enteropathy/nephropathy)
______________________ occurs when there is transudate in the pericardial sac. Where are the 2 most common reasons this may occur?
Cardiac puncture
A necropsy, a pig has a hemopericardium. Which of the following is the most likely cause of this pathology?
-Atrial Hemangiosarcoma
-Ulcerative atrial endocarditis
-Aortic rupture
-Cardiac puncture
aortic rupture
A necropsy, a horse has a hemopericardium. Which of the following is the most likely cause of this pathology?
-Atrial Hemangiosarcoma
-Ulcerative atrial endocarditis
-Aortic rupture
-Cardiac puncture
aortic rupture
A necropsy, a turkey has a hemopericardium. Which of the following is the most likely cause of this pathology?
-Atrial Hemangiosarcoma
-Ulcerative atrial endocarditis
-Aortic rupture
-Cardiac puncture
cardiac tamponade
Fluid build up in the pericardium may lead to ___________________ ______________________, where there is compression of the heart and diastolic filling is reduced
T
Emaciation is the most common cause of serous atrophy of pericardial fat. Epicardial fat appears more gelantinous.
True or False
Emaciation may lead to serous atrophy of the pericardial fat.
bacterial infections most commonly cause fibrinous pericarditis.
Issue is that fibrous tissue limits diastolic expansion, leading to restrictive ventricular filling
What is the main issue regarding fibrinous pericarditis? What is it most commonly caused by?
restricts ventricular filling because of limited diastolic expansion
What effect does purulent pericarditis have on ventricular filling?
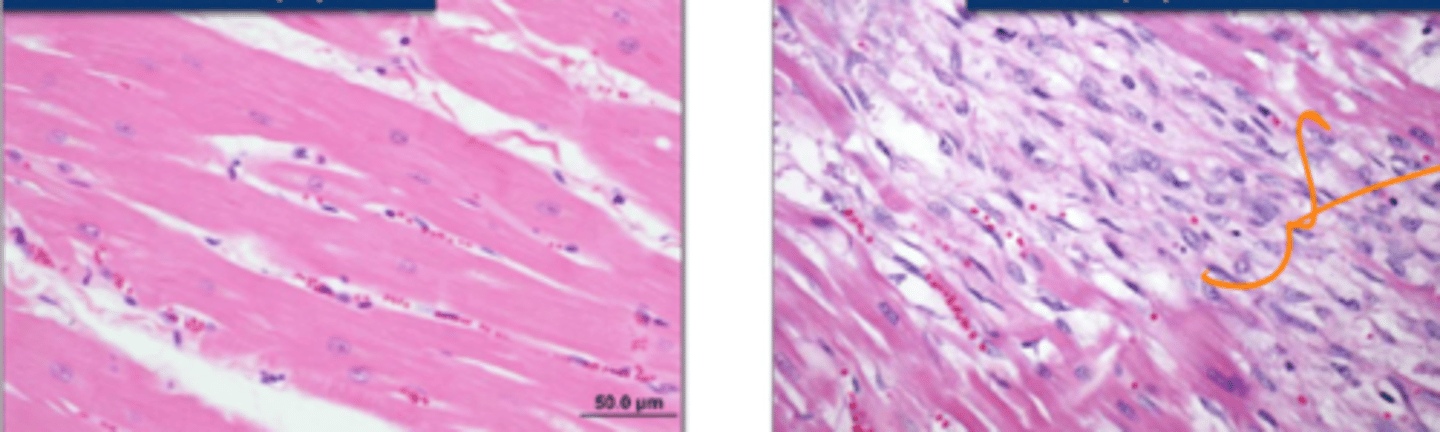
12-24 hours: Coagulative necrosis
1-3 days: infiltration by leukocytes
10-20 days: fibroblast proliferation; "healing" with fibrous tissue replacing myocytes.
6-12 weeks: fibrosis complete
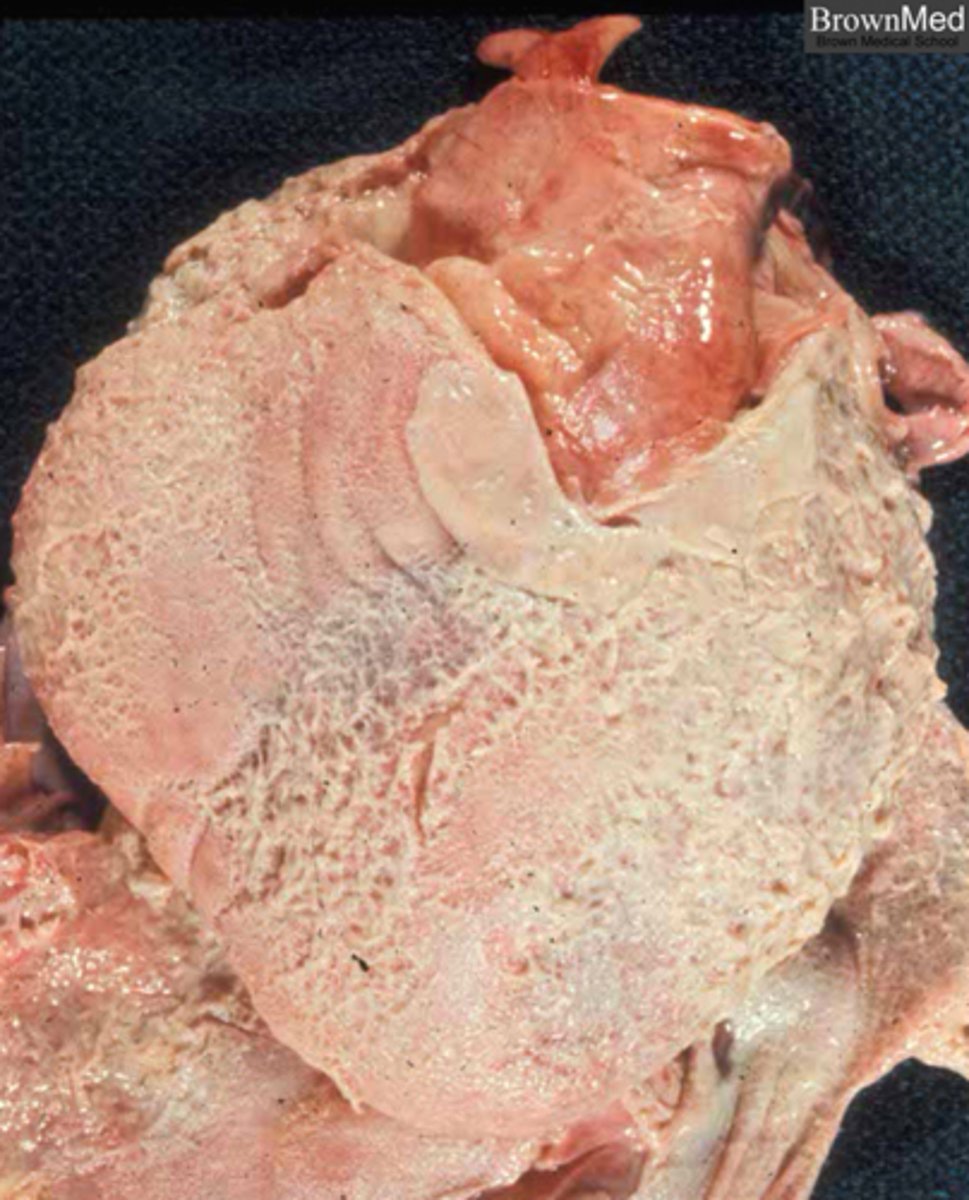
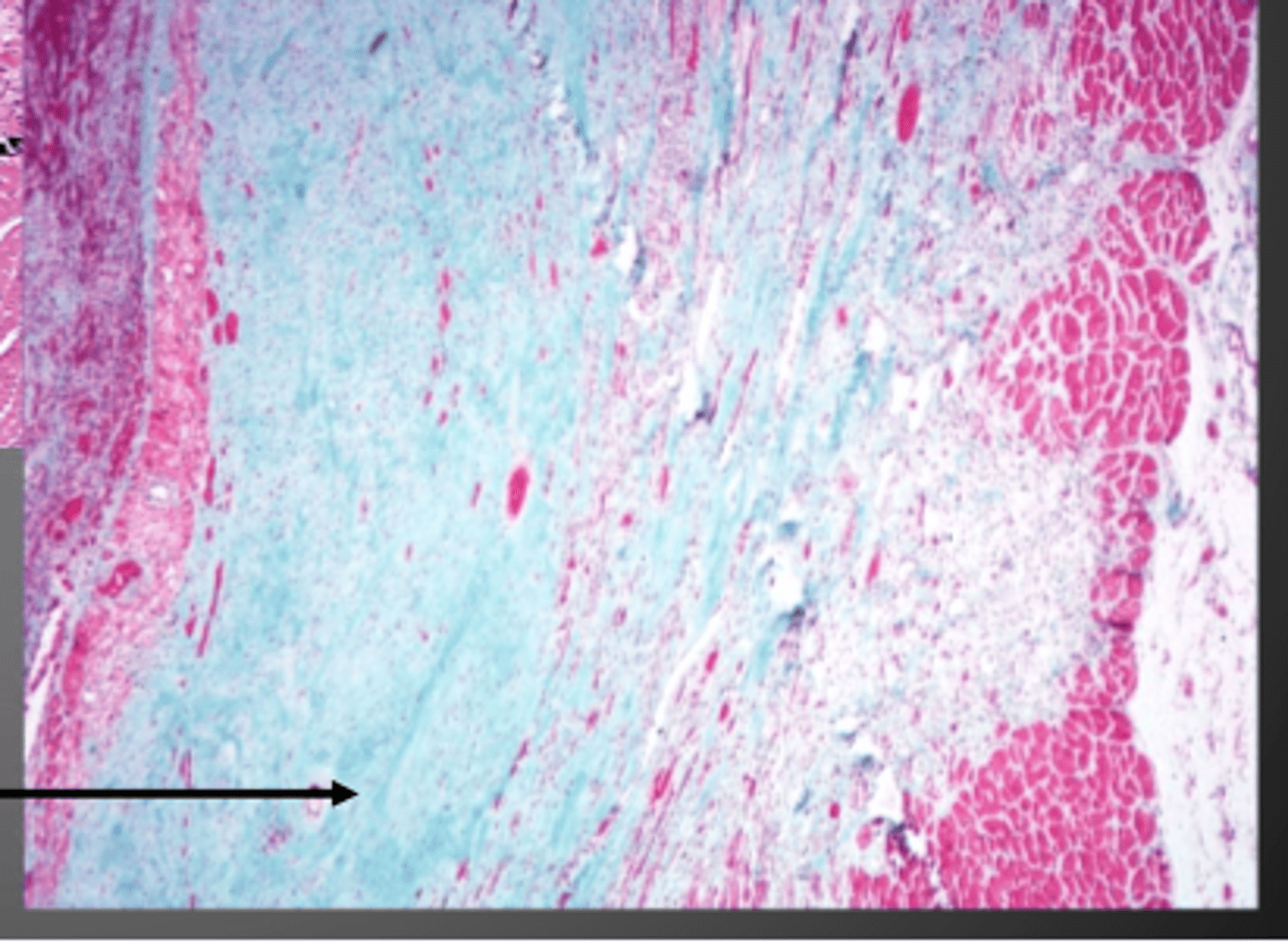
Describe the timing of myocardial necrosis and changes in gross appearance.
12-24 hours - peep da coagulation
What stage in myocardial necrosis is this section in?
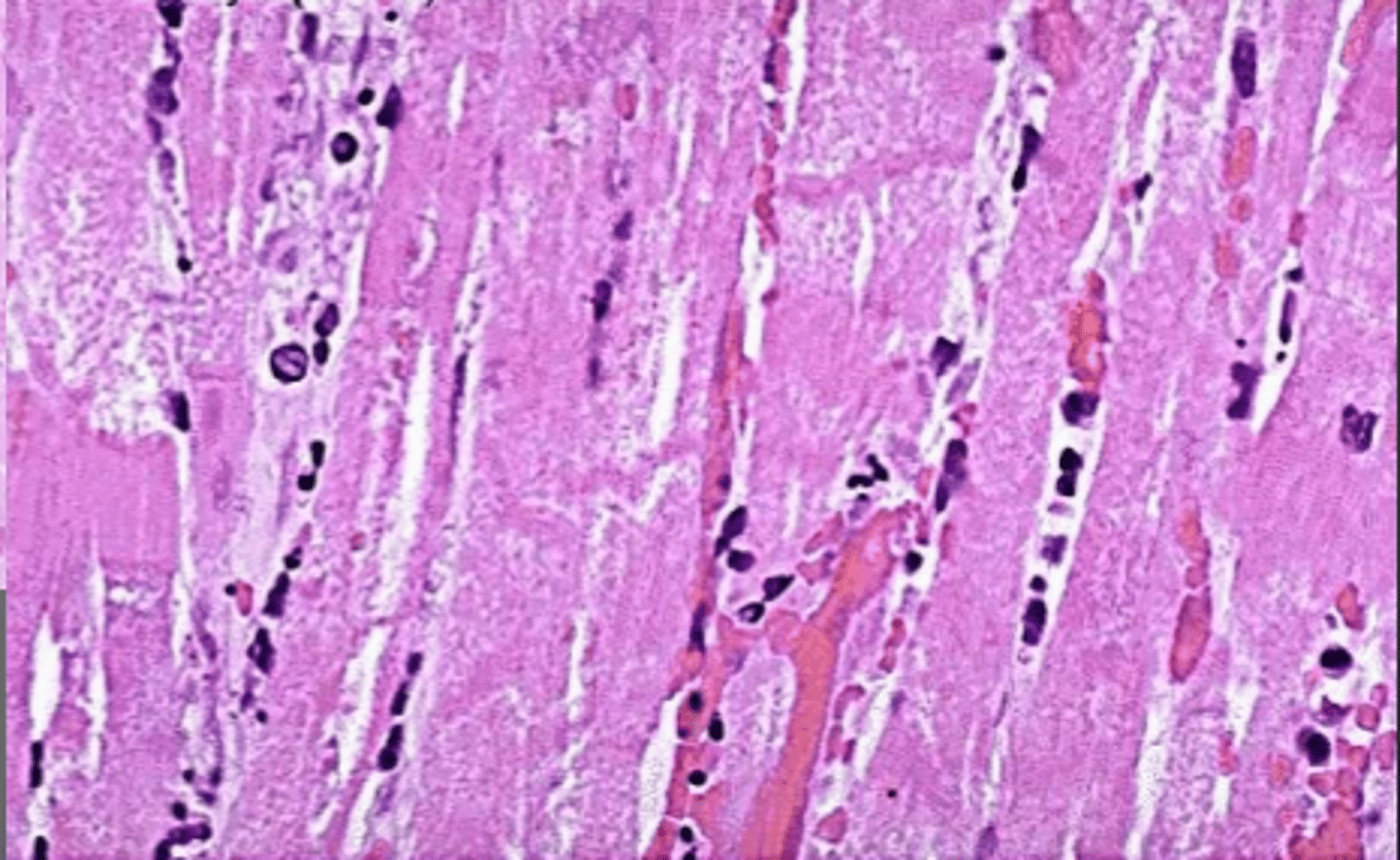
1-3 days
peep all dah leukocytes
What stage in myocardial necrosis is this section in?
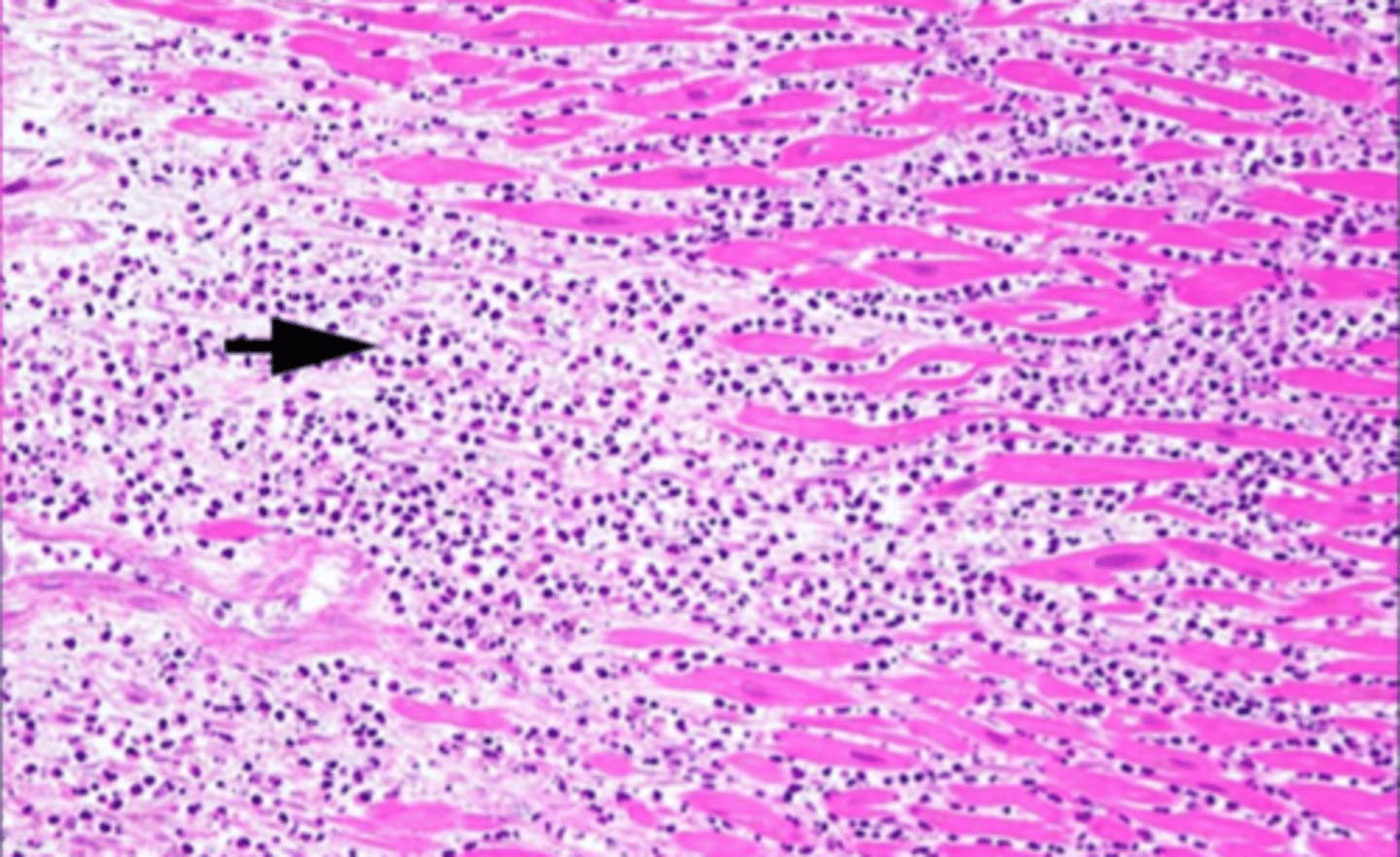
>12-20 days
peed da fibrous tissue replacing the myocytes
What stage in myocardial necrosis is this section in?
ischemic (BF restriction)
What is the LEAST LIKELY cause of mycocaridal necrosis in animals?
ischemic (BF restriction)
toxicity
nutritional
neurogenic
subendocardial fibers because they are the part that are under the most pressure
What part of the heart is most susceptible to myocardial necrosis?
White muscle disease (may effect cardiac or skeletal muscles)
Deficiency in selenium/vitamin E leads to excess free radicals. Free radicals lead to necrosis/mineralization of muscle
Deficiency in selenium and vitamin E may result in what muscular disease?
calves: left ventricle
lambs: right ventricle
White muscle disease is from deficiency in selenium/vitamin E
In calves, the [left/right] ventricle is most commonly effected by white muscle disease.
In lambs, the [left/right] ventricle is most commonly effected by white muscle disease.
T
excess catecholamine's can be toxic to the heart (Brain-heart syndrome)
True or False
Prolonged administration of NE may lead to myocardial necrosis.