(pt 2) exam #3 - immunohematology (cls 544)
1/85
Earn XP
Description and Tags
other common blood group systems
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
where are most blood group genes located?
on autosomal chromosomes
Some genes code for structures carrying more than one antigen
Most blood group systems alleles exhibit co-dominant expression
Antigen expressed when gene present and one gene does not suppress another
ex: inheritance of K/k alleles will result in both being expressed on the individual's RBCs
phenotype
The result obtained from testing RBCs with known reagent antisera
Phenotype results estimate genotype
alleles vs antithetical
Alleles
Alternative alleles at a single gene locus
Designated by italics
Antithetical
When locus can have different alleles, there are corresponding antigens
null phenotype
occurs when RBC has no detectable antigens in system
where paired chromosomes carry the same silent allele → e.g. Lu (a-b-)
in some blood group systems, the null phenotype may result in RBC abnormalities
silent/amorphic alleles
rare—alleles exist but do not produce any antigen
regulator/modifying genes
Seen in some blood groups—alter antigen expression
e.g. dominant type of Lu(a-b-) suppresses expression of all other Lutheran blood group antigens including other blood group antigens P1 and I
This gene is inherited independently from genes coding for Lutheran, P1, and i antigens
writing convetions for genes and antigens
Genes
Written in italics or underlined; their allele number or letter is always superscript
Antigen names
Regular type without italics or underlining
Some antigens have numbers or superscript letters
antigen and phenotype nomenclature
For letter antigens, a plus sign (+) or minus (-) written on the same line as the antigen is used to designate that the antigen is present or absent
e.g., M+, K-
For antigens that have superscripts: the letter of the superscript is placed in parentheses on the same line as the letter defining the antigen
e.g., Fya -> Fy (a+), Jka -> Jk (a-)
For antithetical antigens: both results are written with the parentheses
e.g., Fya and Fyb -> Fy(a-b+)
antigen/antibody nomenclature
antigens with a numerical designation, the letters(s) defining the system is followed by a colon, then the number representing the antigen. No plus sign written to denote presence of antigen, but a minus sign is written before the negative result. Multiple results are separated by a comma
e.g. Sc: -1,2
Antibodies are described by their antigen notation with the prefix "anti-," including a hyphen before the antigen symbol
e.g., anti-C, anti-k
history of ISBT nomenclature
Related antigens placed in blood group system once genetic basis confirmed
Antigens where genetic basis unknown placed in collections
Each antigen given a six-digit number
First three digits – identify the system, collection, or series
Second three digits – identify the antigen
Numbered sequentially in order of discovery
Each system has an alphabetical symbol
To date, 48 blood group systems have been identified
antigen collections
antigens that have a biochemical, serologic, or genetic relationship but do not meet the criteria for a system
Antigens classified as a collection are assigned a 200 number
All remaining RBC antigens that are not associated with a system or collection are catalogued into the 700 series of low-prevalence antigens or the 901 series of high-prevalence antigens
Low prevalence antigens occur in less than 1-2% of the population
High prevalence antigens occur in greater than 90% of the population
clinically significant antibodies
can cause shortened survival of transfused RBCs
Hemolytic transfusion reaction (HTR)
Hemolytic disease of the fetus and newborn (HDFN)
list of commonly encountered antibodies
Rh, Kell, Duffy, Kidd, MNS, and Lutheran
Lewis, P1, I
carbohydrate blood groups (3)
include: Lewis, P, and I
Like ABH antigens, these are NOT encoded directly by genes
The genes encode specific glycosyltransferases that in turn synthesize the carbohydrate epitopes by sequential addition of sugars to a precursor
Carbohydrates (sugars) attached to glycoproteins or glycolipids
(general) lewis blood group system (LE)
ISBT system symbol: LE, Number: 007
Lewis antigens are NOT intrinsic to RBC membrane (unique)
Adsorbed from plasma onto RBC membrane
Le gene (FUT3) codes for L-fucosyltransferase = adds L-fucose to type 1 precursor chains
Le gene needed for expression of Lea substance
Le and Se genes (FUT2) needed for formation of Leb substance
Antigens result from presence of Lewis gene
Poorly expressed at birth, 6 antigens
(LE blood group) where are the lewis ANTIGENS located?
on Type 1 glycosphingolipids that are passively adsorbed onto the RBC membrane from the plasma
Lewis antigens of primary concern: Lea and Leb
Not antithetical antigens (not alternative alleles of a single gene)
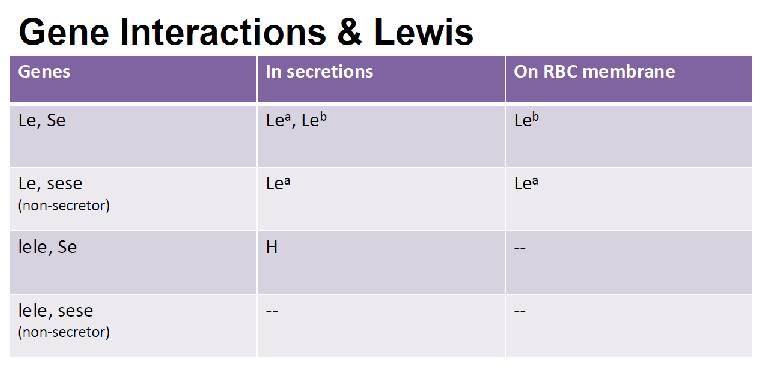
Result from the interaction between two fucosyltransferases encoded by independent genes → Le (FUT3) and Se (FUT2)
Two alleles at the Lewis locus
Le + amorph le
Two alleles at the Secretor locus
Se + amorph se
(LE blood group) where are the Le and Se GENES located?
CHROMOSOME 19
Le gene must be present for a precursor substance to be converted to Lea
Se gene must be present for conversion to Leb
Individuals with Le(a+) mostly non-secretors of ABH antigens
(LE blood group) possible phenotypes
caused by interaction between Le and Se gene
Le(a+b-): ABH non-secretors
Le(a-b+): ABH secretors
Le(a-b-): More frequent among African American population, either secretors or non-secretors
Le(a+b+): More frequent among Asian population
(LE blood group) expression of lewis antigens
Depending upon the genes inherited, both Lea and Leb glycoproteins will be present in the saliva of newborns
Lewis glycolipids are NOT detectable in the plasma until about 10 days after birth
Not expressed on cord RBCs and diminished on maternal RBCs during pregnancy
Found on lymphocytes, platelets and other tissues such as pancreas, stomach, intestine, skeletal muscle, renal cortex, and adrenal glands
Soluble Le antigens found in saliva as glycoproteins (RBC antigens are glycolipids)
(LE blood group) effect of enzyme treatment on lewis antibodies?
reactivity of Lewis antibodies enhanced by testing with enzyme-treated RBCs
(LE blood group) development/inheritence of lewis antigens
Inheritance of Le and Se gene
Inherit BOTH Le and Se genes
Le(a-b-) at birth →Le(a+b-) after 10 days →Le(a+b+) → Le(a-b+) also known as the “true Lewis phenotype” after 6 years
Inherit Le and sese genes
Le(a-b-) at birth →Le(a+b-) after 10 days
Le(a+b-) persists through rest of life
Inherit lele genes
Le(a-b-) phenotype at birth and throughout rest of life
(LE blood group) changes in lewis phenotype may be caused by?
Pregnancy
Decreased Lewis antigens on RBC
Le(a-b-)
Increased incidence of formation of Lewis antibodies
Transient change
Lewis antigens easily dissociate from red blood cell membrane
(LE blood group) lewis blood group antibodies
Frequently naturally occurring antibodies made by Le(a-b-) persons
Occur without any known RBC stimulus
Generally IgM, do not cross placenta, and can activate complement
Anti-Lea and Anti-Leb may occur together
May be seen in pregnant women who transiently exhibit Le(a-b-) phenotype
Anti-Lea more commonly encountered, can be clinically significant, may cause in vitro hemolysis
Lewis antibodies neutralized by Lewis substances in plasma or saliva
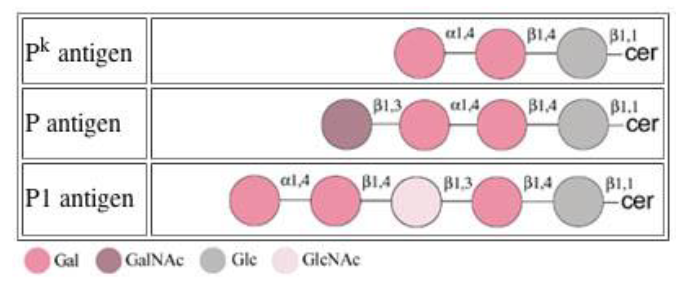
(general) P blood group system (P1Pk)
Traditionally comprised of P, P1, and Pk and later, Luke (Lke), PX2, ExtB, and NOR
Currently the ISBT nomenclature are assigned as follows:
P1, Pk and NOR assigned to P1PK blood group system (P1Pk, 003)
P, ExtB, and PX2 to Globoside Blood Group System (GLOB, 028)
LKE is assigned to the 901 series (901017)
Overall, referred to as the "P blood group"
Two common phenotypes in the P blood group system are P1 and P2
Three rare phenotypes: p, P1k, and P2k
(P blood group) main phenotypes associated with this system (3)
P1 Phenotype (P1, P, Pk antigens)
RBCs react with anti-P1 and anti-P
P2 Phenotype (P, Pk antigens)
RBCs react with anti-P
p (P null) Phenotype
Rare, RBCs do not react with anti-P1, anti-P, or anti-Pk
Make anti-P, P1, Pk
(P blood group) where are the P1Pk and P genes located?
P1PK (located on chromosome 22) and P (located on chromosome 3) genes are inherited independently
Antibodies can be clinically insignificant OR potently hemolytic
(P blood group) P1 antigen
poorly expressed at birth—can take up to 7 years to be fully expressed on RBCs
Strength of antigen expression may vary based on ethnicity → stronger expressed noted in AA population
Deteriorates rapidly in storage
(P blood group) anti-P1 antibody
Common, naturally occurring IgM antibody in the sera of P1 individuals
Reacts below 37C = clinically insignificant
IgG forms are rare = not associated with HDFN
Rare reactions at 37C may result in both immediate and delayed HTRs
Neutralized by P1 substance, hydatid cyst fluid
Transfusion considerations
Provide units crossmatch-compatible at 37C/AHG without typing for P1 is acceptable!
(P blood group) expression of P blood group antigens
Similar to ABH antigens, synthesized by sequential action of glycosyltransferases--exist as glycosphingolipids
P1, P, or Pk may be found on RBCs, lymphocytes, granulocytes, and monocytes
P can be found on platelets, epithelial cells, and fibroblasts
P and Pk found in plasma as glycosphingolipids and as glycoproteins in hydatid cyst fluid
Antigens have NOT been identified in secretions
(P blood group) effect of enzyme treatment
reactivity of P blood group antibodies enhanced with enzyme treated RBCs
(P blood group) luke (LKS) antigen
Phenotypically-related because the antibody reacts with all RBCs except 2% of P1 and P2 phenotypes and rare p and Pk phenotypes
All individuals with the p and Pk phenotype are referred to as Luke(-)
(P blood group) disease associations
Parasitic infections → anti-P1
Early abortion → anti-PP1Pk or anti-P
PCH → autoanti-P
P is the receptor of human parovirus B19
Pk provides some protection against HIV infection of PMNs, Shiga toxin receptor
(P blood group antibodies) anti-PP1Pk
Produced by p individuals early in life without RBC sensitization
Reacts with all RBCs except those of the p phenotype
IgM and IgG--react at a wide thermal range
Can bind complement--cause severe HTRs and HDFN
Associated with increased incidence of spontaneous abortions early in pregnancy
(P blood group antibodies) alloanti-P
naturally occurring alloantibody in the sera of Pk individuals—-rare but clinically significant in transfusion
(P blood group antibodies) autoanti-P
associated with paroxysmal cold hemoglobinuria (PCH)
Anti-P associated with the cold-reactive IgG autoantibody in patients with PCH (biphasic)
Does not react in routine serological testing—identified via the Donath-Landsteiner test
Post viral infection or tertiary syphilis
(P blood group) testing considerations
Soluble P1 antigen is available as a reagent
Can be used in antibody identification to neutralize (inhibit) anti-P1
Anti-P1 is considered a RT-nuisance antibody
Elimination of IS phase
Use of monospecific anti-IgG in IAT
Use of non-tube testing techniques
(general) I blood group system (I) & i antigen
"I" stands for "individuality", symbol I, system number 027; i antigen, Ii Collection 207
Located on chromosome 6
I and i antigens are NOT antithetical, reciprocal relationship
Most adult RBCs are rich in I antigen--trace amounts of i antigen
At birth, infant RBCs are rich in i antigen--I antigen undetectable
The i antigen on infant RBCs convert to I antigen over an 18 month period
Antibodies usually IgM autoantibodies, enhanced by enzyme treatment
Soluble substances in plasma, secretions such as milk and amniotic fluid
(I blood group antibodies) anti-I
benign, weak, naturally occurring IgM autoagglutinin that is usually detectable at 4 C
Anti-I = common autoantibody that can be found virtually all sera
Testing the sera at 4C and against enzyme-treated RBCs may be required to detect the reactivity
The production of autoanti-I may be stimulated by microorganisms carrying I-like antigen on their RBC surface
e.g. patients with mycoplasma pneumoniae
Anti-I is NOT associated with HDFN
(I blood group antibodies) pathogenic autoanti-I
Strong IgM cold agglutinin that reacts at 4C and over a wide thermal range up to 30C
Existence of cold agglutinins in the serum of normal individuals and in patients with acquired hemolytic anemia
May mask clinically significant antibodies
(I blood group antibodies) autoanti-i
may present as a rare IgM agglutinin that reacts at 4C
Potent examples associated with infectious mononucleosis (Epstein-Barr virus infection)
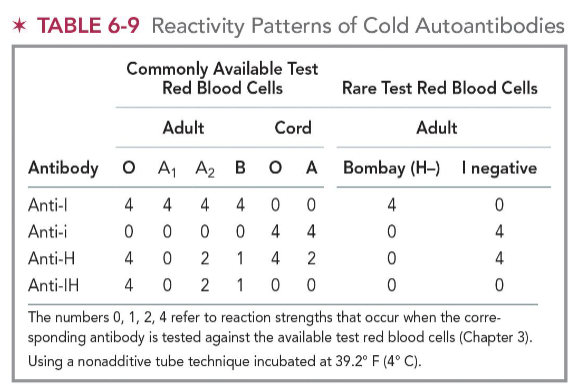
(reactivity patterns of cold autoantibodies) anti-I
O, A1, A2, B cells = 4+
Cord O & A cells: 0
Bombay (H-): 4+
I negative cells: 0
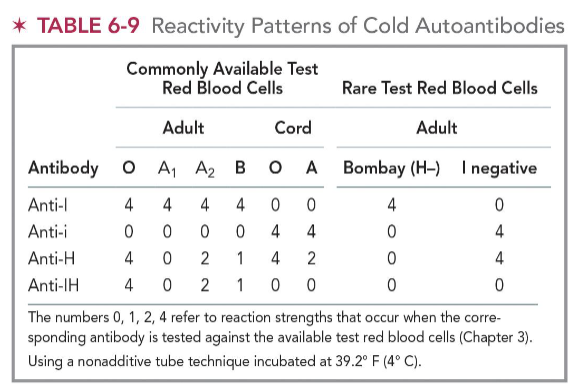
(reactivity patterns of cold autoantibodies) anti-i
O, A1, A2, B cells: 0
Cord O & A cells: 4+
Bombay (H-): 0
I negative cells: 4+
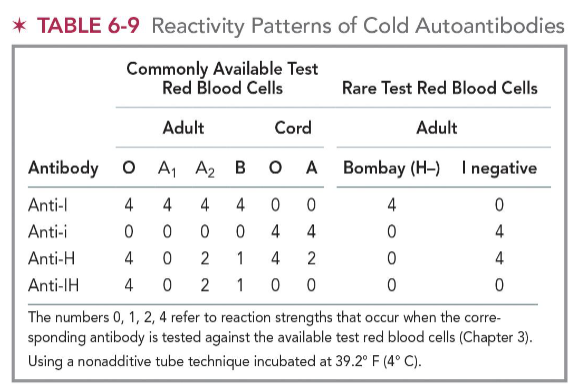
(reactivity patterns of cold autoantibodies) anti-H
O cells; cord O cells; I neg cells: 4
A1 cells: 0
A2 cells: 2
B cells: 1
Cord A cells: 2
Bombay (H-): 0
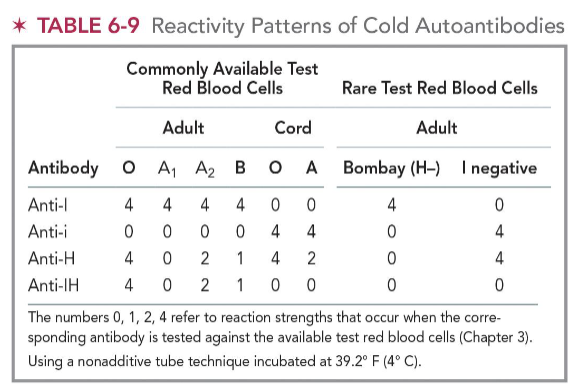
(reactivity patterns of cold autoantibodies) anti-IH
O cells: 4
A1 cells: 0
A2 cells: 2
B cells: 1
Cord O & A cells: 0
Bombay (H-) & I negative cells: 0
(general) MNS blood group system (MNS)
includes 50 antigens ; on chromosome 4
ISBT assigned symbol MNS and number 002
M and N antigens are found on glycoprotein structures also referred to as glycophorins
GYPA gene controls M and N antigen production, antithetical antigens
GYPB gene controls S,s, and U antigen production
MNS antigens are well developed at birth
MNS antigens all show dosage
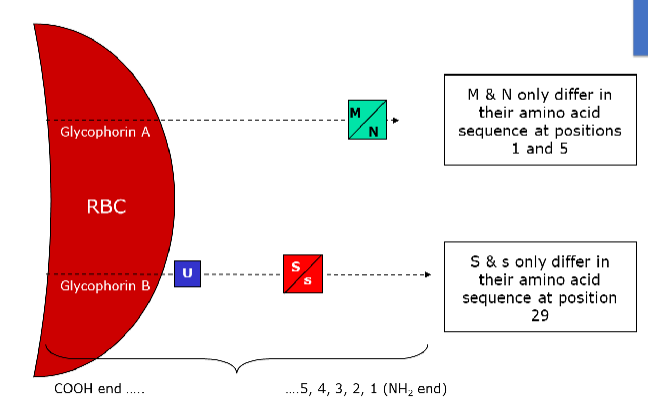
(MNS blood group) where are the M and N antigens located?
on Glycophorin A (GPA)
M & N give a stronger reaction when homozygous, (M+N-) or (M-N+)
Weaker reactions occur when in the heterozygous state (M+N+)
(MNS blood group) where are S, s, and U antigens located?
on a smaller glycoprotein called Glycophorin B (GPB)
Differentiated by the amino acid at positive 29 on GPB
U antigen is ALWAYS present when S and s are inherited (high prevalence)
About 85% of S-s- individuals are U-negative (RARE)
U-negative cells are only found in the African American population
(MNS blood group) effect of enzyme treatment on M & N antigens
due to location on the outer end of GPA, M & N antigens easily destroyed by ficin, papain, bromelin, trypsin, and pronase
(MNS blood group) effect of enzyme treatment on S & s antigens
Less easily destroyed by enzyme treatment since they are located further down the glycoprotein (less accessible)
Can be destroyed by ficin, papain, bromelin, pronase, and chymotrypsin
NOT destroyed by trypsin, DTT, AET, chloroquine or glycine-acid EDTA treatment
MNS blood group antibodies (general)
M and N antibodies are heterogenous
Some recognize only specific amino acids; others recognize both amino acids and carbohydrate chains
Anti-M and Anti-N are cold-reactive saline agglutinins
Many examples are naturally occurring saline agglutinins that react below 37C
Usually IgM
Do NOT bind complement
Not clinically significant unless antibodies react at 37C
Demonstrate dosage
e.g. strong anti-M reactions are seen with M+N- RBCs vs M+N+ RBCs
(MNS blood group antibodies) anti-M
Rarely causes HTRs, HDFN, or decreased red blood cell survival
More common in children than in adults
Seen in patients with bacterial infections
(MNS blood group antibodies) anti-N
Seen in renal patients who were dialyzed on equipment sterilized with formaldehyde (anti-Nf)
Antibody titer decreased with dialysis treatment stops
(MNS blood group antibodies) anti-S & anti-s
IgG antibodies
Reactive at 37C and the antiglobulin (AHG) phase
Can bind complement—associated with HDFN and HTR
Dosage effect can be exhibited
May or may not react with enzyme-treated RBCs
(MNS blood group) transfusion considerations
11% Caucasian and 3% Afriacan American (AA) populations are s-
45% Caucasian and 69% AA populations are S-
Notably, S-s-U- phenotype is found in AA populations (<1% of AA)
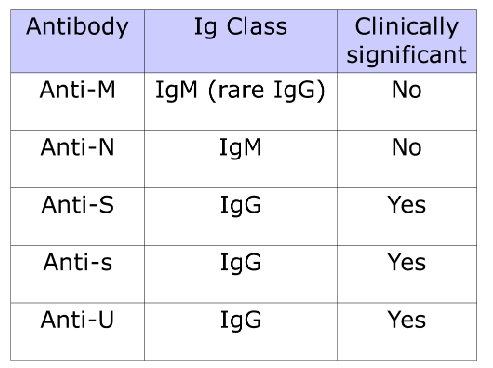
(MNS blood group) GPA- & GPB- deficient phenotypes (3)
RBCs of three rare phenotypes lack either GPA or GPB or both and, consequently lack all MNS antigens that are normally expressed on those structures
U- phenotype: S-, s-, cells lack GPB
U antigen located on GPB; high prevalence antigen
U antigen resistant to enzyme treatment
Anti-U (IgG) assoc with both HTR and HDFN
En(a-) phenotype: M-, N-, cells lack GPA
Ena located on GPA (high prevalence antigen)
Most produce anti-Ena; has caused severe HTRs and HDFN
Mk phenotype: cells lack both GBA and GPB
Rare silent gene (M and N alleles not produced, null phenotype in MNS system)
Single, near-complete deletion of both GYPA and GYPB
(MNS blood group) other antibodies
can usually be grouped into two categories:
Those directed against high-prevalence antigens
Those directed against low-prevalence antigens
Autoantibodies
U and Ena more common
Associated with warm-type autoimmune hemolytic anemia
Disease associations
GPAM receptor for pyelonephritogenic strains of E coli
Plasmodium falciparum uses receptors for cell invasion
(general) kell blood group system (KEL)
ISBT symbol KEL, number 006
38 antigens
Kell antigens present on the single gene, KEL located on chromosome 7
k (cellano) antigen is high prevalence
Kx Blood Group System
ISBT symbol KX, Number 019, located on X chromosome
Kx = high frequency antigen
Only known antigen in the Kx blood group system
Kell antigens expression greatly reduced when Kx protein is absent
(KEL blood group) kell antigen characteristics
Cellular distribution of the antigen
Found only on RBCs
K can be detected on fetal RBCs as early as 10 weeks (!!)
Well developed at birth
Cannot be destroyed with routine blood bank enzymes
Can be destroyed with 0.2M DTT, ZZAP, 2-ME, 2-AET, and glycine-acid EDTA
With the exclusion of ABO, the K antigen is rated second to the D antigen in terms of immunogenicity
(KEL blood group) list of high incidence antigens (3)
k, Kpb and Jsb antigens all high incidence
(KEL blood group) Kpa and Kpc antigens
Rarely encountered and not routinely tested with antibody identification panels
Most often detected through incompatible crossmatches of HDFN
Kpa and Kpc are low prevalence mutations of their high-prevalence partner, Kpb
(KEL blood group) Jsa and Jsb antigens
Jsa antithetical to the high prevalence antigen, Jsb
Found in 20% Black population (less than 0.1% Caucasian population)
Both antigens linked to the Kell system due to K0 RBCs phenotype of Js(a-b-)
(KEL blood group) major antigens encoded by kell gene
K1 = K = Kell = 9%
K2 = k = Cellano = 99.8%
K3 = Kpa = Penney = 2%
K4 = Kpb = Rautenberg = >99%
K6 = Jsa = Sutter = <0.1% W 20% B
K7 = Jsb = Matthews = 99.9 %
K17 = Wka = Weeks = 0.3
K11 = Cote = >99.9%
K10 = Ula no allele
Most common: k/Kpb/Jsb/K11
kell blood group system antibodies (general)
Outside of ABO and Rh antibodies, anti-K is the most common antibody encountered in the blood bank
Anti-K is usually IgG antibody
Reactive in the AHG phase
Most anti-K appear to be induced by pregnancy and transfusion
Implicated in severe HDFN (attributed to suppression of erythropoiesis) and severe HTR
Naturally occurring IgM anti-K is rare and associated with bacterial infection
Antibodies to k antigen are seldom encountered
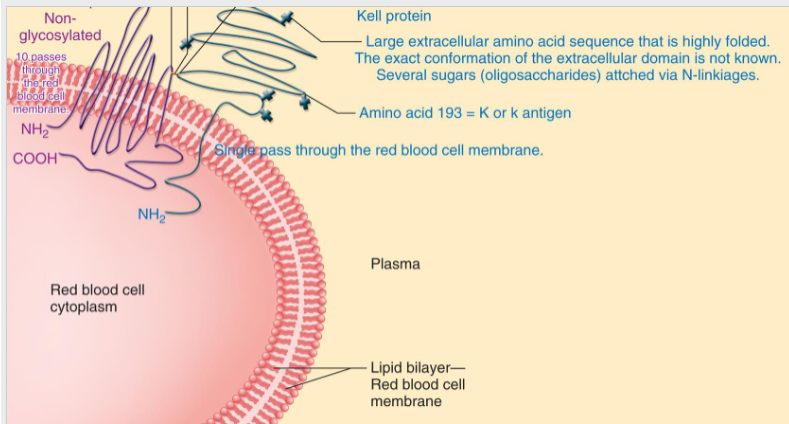
(KEL blood group) biochemistry of kell antigens
Located on a glycoprotein that consists of 731 amino acids and spans the RBC membrane once
Kell antigen expression dependent on the presence of the Xk protein
Located on chromosome 7
(KEL blood group) Kx antigen
Present on all RBCs except those with rare McLeod phenotype
Expression of Kx increases with denaturing of Kell antigens by AET or DTT
(KEL blood group) K0 phenotype + anti-Ku (K5)
lacks expression of all Kell antigens and produces anti-Ku(K5), causes HDFN and HTRs
(KEL blood group) McLeod phenotype + syndrome
Rare phenotype with decreased Kell system antigen expression that ONLY AFFECTS MALES
Some males with this phenotype have the X-linked chronic granulomatous disease (CGD)
Clinical Manifestations
Abnormal RBC morphology (acanthocytes)
Associated with hemolytic anemia
Neurological and muscular abnormalities
McLeod males with CGD make anti-Kx + Km (lack Kx and Km antigens)
McLeod males without CGD make anti-Km
(kell blood group) altered antigen expression + autoantibodies assoc w kell antigens
Altered expressions of Kell antigens
Weaker than normal Kell antigen expression with McLeod phenotype
Kmod phenotype
Autoantibodies associated with Kell antigens
Directed against undefined high prevalence Kell antigens
K, Kpb, and K13
(general) duffy blood group system (FY)
ISBT symbol FY, number 008, chromosome 1
5 antigens—Fya and Fyb, Fy3, Fy5, and Fy6
Most important antigens: Fya and Fyb
Majority of AA population duffy null Fy(a-b-) (FY genotype)
FyFy common genotype in the AA population, especially in West Africa
Fy gene exceedingly rare in white population
Disease association
Fy(a-b-) RBCs resist infection by Plasmodium knowlesi and vivax
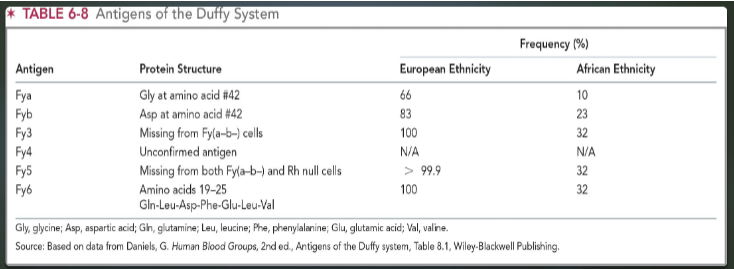
(FY blood group) duffy antigen phenotypes
Fya and Fyb are receptors for Plasmodium vivax and knowlesi, may offer protection against malaria
Fy(a+b-) 17% Whites, 9% Blacks, 91% Chinese
Fy(a+b+) 49% Whites, 1% Blacks, 9% Chinese
Fy(a-b+) 34% Whites, 22% Blacks, 0.3 Chinese
Fy(a-b-) very rare Whites, 68% Blacks, 0% Chinese
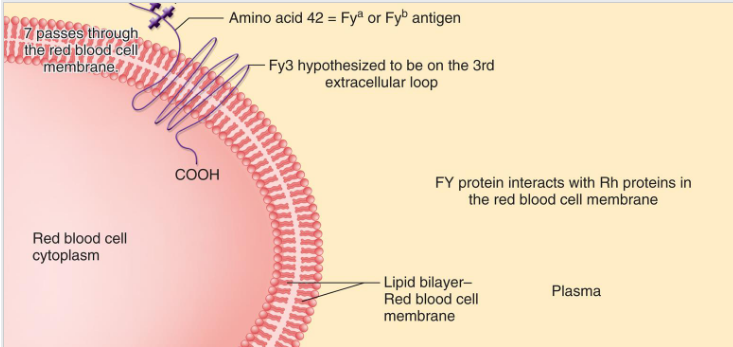
(FY blood group) expression + effect of enzyme treatment
Well developed at birth
Detected on fetal RBCs as early as 6 weeks (gestation)
Enzyme treatment
Destroyed by enzymes and ZZAP
(FY blood group) antibodies of concern (anti-Fya + Fyb)
Usually IgG antibodies & react at the AHG phase (Anti-Fya > anti-Fyb)
Rarely bind complement
Do not react with enzyme treated RBCs
Show dosage (RBCs react strongly with double dose)
Both antibodies implicated in acute and delayed HTRs; associated with HDFN
(FY blood group) other antigens (Fyx, Fy3, Fy5)
Fyx – does not produce an antigen but an inherited weak form of Fyb
Individuals type as Fy(b-)
No anti-Fyx
Fy3
not destroyed by enzymes
Rare anti-Fy3 found in serum of Fy(a-b-) phenotype
Fy5
appears to be an interaction between Rh complex and Fy glycoprotein
Fy5 not destroyed by enzymes
Fy(a-b-) and Rhnull do not produce Fy5 antigen
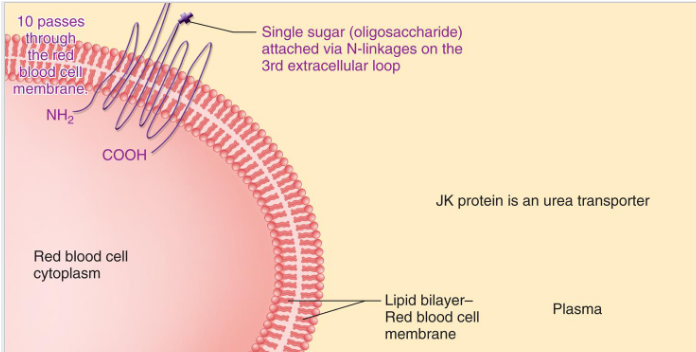
(general) kidd blood group system (JK)
ISBT symbol JK, number 009, chromosome 18
Glycoprotein carrying antigens transports urea across RBC membrane
Three antigens
Jka, Jkb, and high incidence antigen, Jk3 (Jka and Jkb one or the other present for Jk3)
Anti-Jka and anti-Jkb are NOTORIOUS for causing delayed HTRs
Titers go away very quickly
(kidd blood group) Jka + Jkb antigens
commonly found on the RBCs of most individuals
well developed at birth
Jka detected on fetal RBCs as early as 11 weeks (Jkb = 7 weeks)
Not very immunogenic
Rarely indicated in HDFN
Enzyme/chemical treatment
Not denatured with routine blood bank enzymes (enhanced)
Not affected by DTT, AET, chloroquine, or glycine-acid EDTA
(kidd blood group system) phenotypes
Jk(a+b-) 28% White, 57% Black, 23% Asian
Jk(a+b+) 49% White, 34% Black, 50% Asian
Jk(a-b+) 23% White, 9 Black, 27% Asian
Jk(a-b-) rare in white and Black ppl; more common in Polynesians
kidd blood group system antibodies (anti-Jka/Jkb)
Can be difficult to detect (weak) and often found in combination with other antibodies; Anti-Jka more common than anti-Jkb
Typically, IgG and react at the AHG phase
Bind complement + demonstrate dosage
Reactivity enhanced with enzymes, LISS, and PeG
Produced in response to foreign RBC exposure during pregnancy or transfusion
Common cause of delayed HTRs
Antibody tiers decline quickly in vivo
(kidd blood group system) Jk(a-b-)
aka Jk null phenotype
most abundant among Polynesian population
Delayed lysis of null RBCs in 2M urea (used to screen families for phenotype)
No associated clinical abnormalities
(kidd blood group system) anti-Jk3 + autoantibodies
Anti-Jk3
Associated with severe immediate and delayed HTRs, mild HDFN
Autoantibodies
Associated with AIHA
(general) lutheran blood group system (LU)
ISBT symbol LU, number 005
LU gene located on chromosome 19
Linkage exist between the LU and Se gene
First example of autosomal linkage described in humans
Three genetic explanations for the Lu(a-b-) phenotype
Dominant type, recessive type, and recessive X linked inhibitor type
Lu(a-b-) phenotype = rare
Only individuals with the recessive type Lu(a-b-) produce anti-Lu3
LU blood group system antigens
29 antigens in Lutheran system
Lua and Lub (more common) produced by codominant alleles
Poorly developed at birth
Most individuals are Lub pos = low number of antigen sites
Lu (a-b-) null phenotypes arises from genetic situations
Enzyme treatment
Resistant to ficin, papain, glycine-acid EDTA
Destroyed by trypsin, alpha-chymotrypsin
(LU blood group antibodies) anti-Lua
Naturally occurring IgM saline agglutinins
React better at room temp (IS) than at 37°C
Some capable of binding complement
In vitro hemolysis not reported
Often undetected bc most reagent RBCs are Lua neg
Characterized by loose, mixed-field reactivity
Rare and mild delayed HTRs
(LU blood group antibodies) anti-Lub
Most are IgG – reactive at 37°C & AHG phase
Produced in response to pregnancy or transfusions of foreign RBCs
Shortens survival of transfused cells and may cause post-transfusion jaundice
RARE DONOR BANK of Lub antigen negative units!
(LU blood group antibodies) anti-Lu3
Rare antibody – reacts with all RBCs except for Lu(a-b-) RBCs
Usually reacts at the AHG phase
Antibody produced by individuals with recessive type Lu(a-b-)
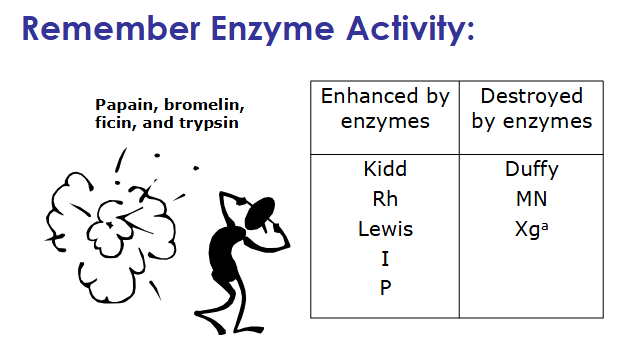
effect of enzyme treatment for the common blood group antigens
ehanced by papain, bromelian, ficin, trypsin: Kidd, Rh, Lewis, I, P
destroyed by enzymes: Duffy, MN, Xga
unaffected by treatment: K, U, Lutheran
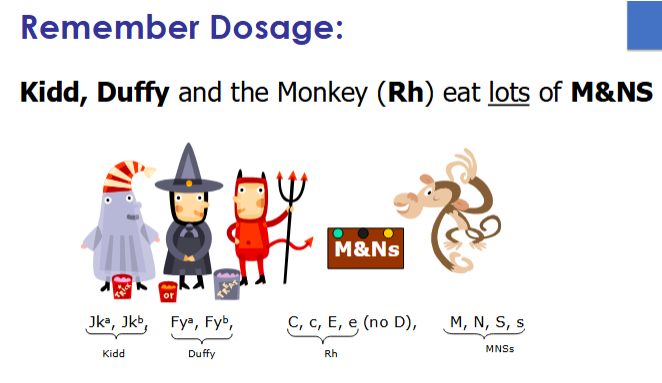
list of antigens that show dosage
Jka + Jkb
Fya + Fyb
C, c; E, e
M, N, S, s