Bones
1/14
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
15 Terms
What are the structural and homeostatic roles of the skeleton?
Structural Functions:
• Support: It gives shape to your body and holds everything in place.
• Movement: Muscles attach to bones; when they contract, they pull on the bones and you move.
• Protection: Your ribs shield your heart and lungs, your skull protects your brain.
Homeostatic Functions:
• Mineral Storage: 99% of your calcium and 85% of your phosphorus is stored in your bones. These minerals can be released into the bloodstream when your body needs them.
• Blood Cell Production (Hematopoiesis)
Red bone marrow inside certain bones makes all your blood cells:
Red blood cells (carry oxygen)
White blood cells (fight infection)
Platelets (help with clotting)
• Hormone Production
Bone cells (like osteoblasts) release a hormone called osteocalcin.
Osteocalcin helps:
Boost insulin production in the pancreas
Improve insulin sensitivity in body cells
Regulate blood sugar levels
Energy storage: Yellow bone marrow stores fat (in the middle of long bones).
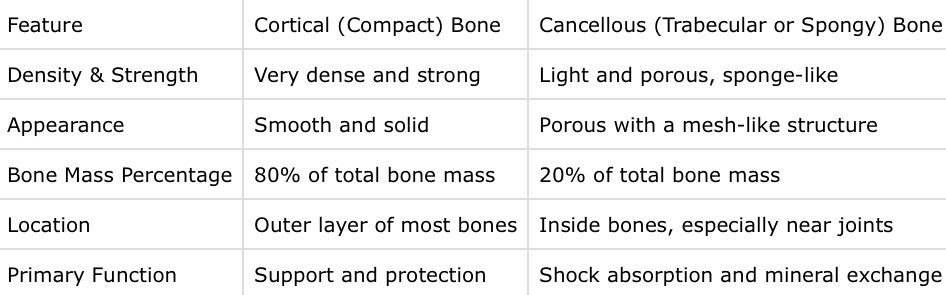
What are the two main types of bone tissue and their characteristics?
What two components form the bone matrix and what are their roles?
1. Collagen.
A protein fiber made by osteoblasts.
Provides tensile strength — resists stretching and pulling.
Without it, bones are brittle.
• Vitamin C is crucial for collagen synthesis; a deficiency (like in scurvy) causes bones to become weak and prone to fractures.
2. Hydroxyapatite
• Hydroxyapatite is a crystalline mineral made primarily of calcium and phosphate.
Gives bones hardness and compressive strength (resists squashing).
Without it, bones are too soft and bend easily.
• Without hydroxyapatite, bones would be too soft — like rubbery cartilage — and would deform under pressure.
Why is a balance between collagen and hydroxyapatite crucial for bone health?
• Too much mineral and too little collagen → bone becomes brittle and can shatter under stress.
• Too much collagen and not enough mineral → bone becomes too soft and bendy, unable to support weight.
What is bone remodeling and why is it important?
• To repair tiny cracks and damage
• To adapt to stress (e.g., lifting weights makes bones stronger)
• To maintain calcium levels in your blood (Essential for blood clotting, nerve function, muscle contraction)
What are the key stages of the bone remodelling? (Activation)
Purpose:
To find areas of bone that need fixing and get them ready for cleanup.
Who’s Involved:
Osteocytes: Long-living “sensor” cells inside the bone that detect stress or damage.
Bone-lining cells: Flat cells on resting bone surfaces — they move aside to expose the area.
What Triggers It?
Exercise or heavy use (mechanical stress)
Hormones (like PTH)
Low calcium levels
Inflammation from injury or disease
What Happens:
Osteocytes sense a problem (like a crack or stress).
They send out signals (like RANKL and prostaglandins).
These signals call in immature osteoclasts (bone-breaker cells) from the blood.
Bone-lining cells move out of the way, uncovering the bone so cleanup can begin.
What are the key stages of the bone remodelling? (Resorption phase)
Purpose: To remove old or damaged bone tissue.
Who’s involved:
• Osteoclasts: Large, multinucleated cells derived from monocyte/macrophage lineages.
What happens:
• Osteoclasts attach to the exposed bone surface and form a ruffled border, which increases surface area for secretion.
• They create a sealing zone that traps secretions in a closed environment.
The cell then secretes:
• Hydrochloric acid (HCl) to dissolve hydroxyapatite (mineral part)
• Enzymes like cathepsin K and TRAP (tartrate-resistant acid phosphatase) to degrade collagen and protein matrix
What are the key stages of the bone remodelling? (Reversal phase)
Purpose:
To clean up after bone breakdown and prepare for new bone formation.
Who’s Involved:
Reversal cells: Small cells (likely from immune origins) that act as cleaners.
Pre-osteoblasts: Early-stage cells that will soon become bone-building osteoblasts.
What Happens:
Reversal cells clean up any leftover debris from the osteoclasts’ work.
They smooth the bone surface and get it ready for new bone.
These cells also send signals to bring in and activate pre-osteoblasts.
Communication between cells helps keep things balanced, so bone breakdown and bone building happen in sync.
What are the key stages of the bone remodelling? (Formation phase)
Purpose: Lay down new bone matrix to replace what was removed.
Who’s involved:
• Osteoblasts: Bone-forming cells derived from mesenchymal stem cells.
What happens:
•the osteoblasts start laying down a soft base layer called osteoid. This layer is mostly made of collagen and is like the frame of a new building.
• Some osteoblasts get trapped inside the new bone and change into osteocytes — long-living cells that help monitor the bone’s health.
• Others become bone-lining cells or die via apoptosis.
Additional molecules released:
Alkaline phosphatase – helps minerals like calcium and phosphate stick to the bone.
Osteocalcin and P1NP – signals that bone is being formed.
What roles do osteoblasts, osteoclasts, and osteocytes play in bone biology?
1. Osteoblasts
• They form new bone by laying down collagen and then mineralizing it.
• Derived from stem cells in connective tissue.
• Some osteoblasts become osteocytes, others rest on the surface as bone lining cells.
2. Osteoclasts
• Derived from immune cells in the blood (hematopoietic lineage).
• They break down bone by releasing acid and enzymes.
• This releases calcium and phosphate back into the bloodstream.
3. Osteocytes
• Osteoblasts that have become trapped inside the bone matrix.
• They sense mechanical stress and communicate with osteoblasts and osteoclasts to regulate bone remodelling.
How do flat bones delevop and what process is involved?
Mesenchymal stem cells gather in a cluster and differentiate into osteoblasts.
Osteoblasts secrete osteoid, a soft matrix rich in collagen.
Minerals (calcium + phosphate) are deposited → form hydroxyapatite → bone hardens.
Bone forms thin fibers called trabeculae which grow outward and fuse.
Cells on the outside form the periosteum (outer protective layer).
Around the edges, compact lamellar bone forms (smooth and strong outer shell).
No cartilage is involved in this process — bone is made directly from connective tissue.
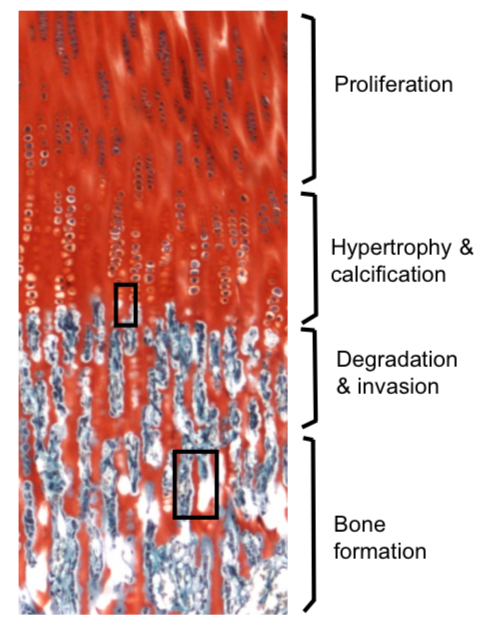
Describe how long bones grow and the role of endochondral ossification.
Begins with mesenchymal stem cells → differentiate into chondrocytes (cartilage cells)
These chondrocytes form a cartilage model shaped like the future bone
The cartilage grows longer and wider, and chondrocytes enlarge (hypertrophy)
In the center, the chondrocytes die as the area calcifies (hardens)
Blood vessels invade this area (called the primary ossification center)
Bring in osteoclasts to remove dead cartilage
Bring in osteoblasts to lay down osteoid
Osteoid is mineralized → becomes real bone
The medullary cavity (marrow space) forms
After birth, secondary ossification centers appear in the bone’s ends (epiphyses)
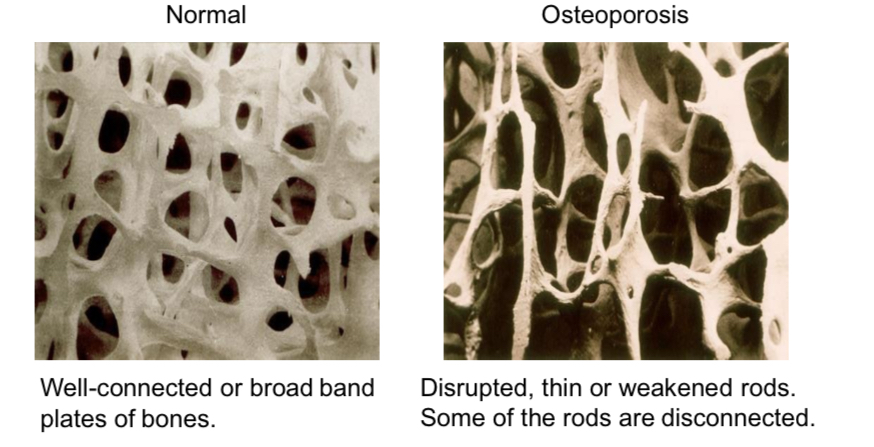
What is osteoporosis and what causes it?
Osteoporosis is a condition where bones become fragile and porous because bone breakdown outpaces bone formation.
Why does this happen?
• Hormonal changes (especially drop in estrogen after menopause)
• Aging
• Low physical activity
• Poor diet (low calcium/vitamin D)
What are the effects?
• Bones become weaker and easier to fracture
• Common in the spine, hip, and wrist
What are the risk factors and lifestyle contributors to osteoporosis?
• Weight-bearing exercise (like walking, dancing, resistance training)
• Healthy diet with enough calcium and vitamin D
• Avoid smoking and alcohol
• Hormone therapy for some postmenopausal women
How do sex hormones like estrogen and testosterone influence bone health
Estrogen:
Helps inhibit osteoclasts (bone breakdown)
Supports osteoblasts (bone building)
When estrogen drops (e.g. after menopause), there’s rapid bone loss
Testosterone:
Helps promote bone growth and muscle strength
Its levels drop gradually, so men tend to lose bone slower over time
Some testosterone gets converted into estrogen, which also helps protect bone