Gas exchange and transport - chapter 18
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
What is hypoxia?
the result of:
impaired diffudion of gasses between the alveoli and the blood
inadequate oxygen transport in the blood
What is hypercapnia?
elecavated concentration of CO2
How does the body avoid hypoxia and hypercapnia?
the body uses sensors that monitor arterial blood composition. these sensors respodn to;
oxygen — arterial oxygen delivery must be adequate
carbon dioxide
pH — maintaining the pH homeostasis is critical to prevent denaturation of proteins. the respiratory system monitors plasma pH and uses changes in ventilation to alterr pH
Why is the excretion of CO2 important?
high levels of CO2 are central nervous system depressant
elevated CO2 causes a state of acidosis
What is diffusion?
the movement of a molecule from a region of higher concentrations to one of lower concentration.
Gases move from regions of … partial pressure to regions of … partial pressure.
Gases move from regions of higher partial pressure to regions of lower partial pressure.
Why does oxygen diffuse from the alveoli into the capillaries?
Normal alveolar PO2 at sea level is 100 mm Hg. the PO2 of “deoxygenated venous blood arriving in the lungs is 40 mm Hg.
oxygen therefore diffuses down its partial pressure gradient from the alveoli into the capillaries.
Diffusion goes to equilibrium, and the PO2 of arterial blood leaving the lungs is the same as in the alveoli: 100 mm Hg.
Why does oxygen diffuse from the capillaries into the tissue?
When arterial blood reaches tissue capillaries, the gradient is reversed. Cells are continuously using oxygen for oxidative phosphorylation.
In the cells of a person at rest, intracellular PO2 averages 40 mm Hg.
Arterial blood arriving at the cells has a PO2 of 100 mm Hg.
thus PO2 is lower in the cells, oxygen diffuses down its partial pressure gradient from the blood plasma into the cell
diffusion goed to equilibrium
Why does carbon dioxide move from the cells into the capillaries?
PCO2 is higher in tissues than in systemic capillary blood because of CO2 production during metabolism.
Cellular PCO2 in a person at rest is about 46 mm Hg,
arterial plasma PCO2 is 40 mm Hg.
The gradient causes CO2 to diffuse out of cells into the capillaries.
Diffusion goes to equilibrium, and systemic venous blood averages a PCO2 of 46 mm Hg.
Why does carbon dioxide move from the capillaries into the alveoli?
Venous blood bringing waste CO2 from the cells has a PCO2 of 46 mm Hg. Alveolar PCO2 is 40 mm Hg. Because PCO2 is higher in the plasma, CO2 moves from the capillaries into the alveoli.
By the time blood leaves the alveoli, it has a PCO2 of 40 mm Hg, identical to the PCO2 of the alveoli.
What are the 3 variables that influence the efficiency of alveolar gas exchange?
adequate oxygen must reach the alveoli — a decrease in PO2 means that less oxygen is available to enter the blood
there can be problems with the transfer of gasses between the alveoli and pulmonary capillaires
blood flow, or perfusion, of the alveoli must be adequate
What are the possible causes of low alveolar PO2?
the inspired air has low oxygen content
alveolar ventilation is inadequate
What is the main factor that affects atmospheric oxygen content?
altitude
The partial pressure of oxygen in air decreases along with total atmospheric pressure as you move from sea level to higher altitudes. water vapor pressure at 100% humidity is the same no matter what the altitude, making its contribution to total pressure in the lungs more important as you go higher.
What is the characteristic of hypoventilation?
low alveolar ventilation
it is characterized by lower than normal volumes of fresh air entering the alveoli.
The transfer of oxygen from alveoli to blood requires diffusion across?
The transfer of oxygen from alveoli to blood requires diffusion across the barrier created by type I alveolar cells and the capillary endothelium.
The diffusion rate is proportional to?
the surface area
concentration gradient
barrier permeability
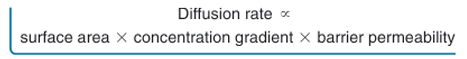
Diffusion is inversely proportional to?
the square of the distance(diffusion distance).
diffusion is more rapid over short distances.
Gas exchange in the lungs is … , blood flow through pulmonary capillaries is …, and diffusion reaches equilibrium in less than … .
Gas exchange in the lungs is rapid, blood flow through pulmonary capillaries is slow, and diffusion reaches equilibrium in less than 1 second.
What is the primary factor affecting gas exchange in healthy people?
the concentartion graident between alveoli and blood
Which parameter can be changed in pathologies that affect gas exchange?
diffusion distance
surface area for gas exchange
barrier permeability
What is a pulmonary adema and what is the cause?
accumulation of interstitial fluid increases the diffusion distance and slows gas exchange
pulmonary blood pressure rises → the normal filtration/reabsorption balance at the capillary is disrupted. When capillary hydrostatic pressure increases, more fluid filters out of the capillary. If filtration increases too much, the lymphatics are unable to remove all the fluid and excess accumulates in the pulmonary interstitial space, creating pulmonary edema.
The movement of gas molecules from air into a liquid is directly proportional to which three factors?
the pressure gradient of the gas
the solubility of the gas in liquid
“temperature” — relatively stable in mammals
When a gas is placed in contact with water and there is a pressure gradient, gas molecules …?
move from one phase to the other
If gas pressure is higher in the water than in the gaseous phase, …?
then gas molecules leave the water
If gas pressure is higher in the gaseous phase than in water, …?
then gas dissolved into the water
What is the partial pressure of the gas in a solution?
the concentration of a gas dissolved in the water at any given Px
The concentration of dissolved oxygen depends on?
the solubility of oxygen in water
What is the solubility of a gas?
The ease with which a gas dissolves in a liquid.
If a gas is very soluble, large numbers of gas molecules go into solution at a low gas partial pressure.
With less soluble gases, even a high partial pressure may cause only a few molecules of the gas to dissolve in the liquid.
Is oxygen soluble or insoluble in an aqueous solution?
Oxygen is not very soluble in water or any aqueous solution
Is carbon dioxide soluble or insoluble in an aqueous solution?
Carbon dioxide is 20 times more soluble in water than oxygen is.
Oxygen’s … solubility in aqueous solutions means that … oxygen can be carried dissolved in plasma. Its … solubility also means oxygen is … to cross the increased diffusion distance present in pulmonary edema.
Diffusion of oxygen into alveolar capillaries does … to come to equilibrium before the blood has left the capillaries. The result is … arterial PO2 even though alveolar PO2 may be … .
Oxygen’s low solubility in aqueous solutions means that very little oxygen can be carried dissolved in plasma. Its low solubility also means oxygen is slower to cross the increased diffusion distance present in pulmonary edema.
Diffusion of oxygen into alveolar capillaries does not have time to come to equilibrium before the blood has left the capillaries. The result is decreased arterial PO2 even though alveolar PO2 may be normal.
Gases that enter the capillaries first…?
dissolve in the plasma
What is the role of red blood cells in the respiratory system?
they have a critical role in ensuring that gas transport between the lung and cells is adequate.
Without hemoglobin the red blood cell wouldn’t be able to transport sufficient oxygen.
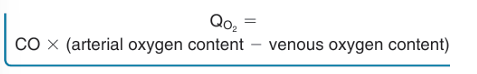
What doe we understand under the term mass flow?
the amount of X moving per minute, where mass flow = concentration * volume.
in the case of the lungs to cells its is: oxygen content of the arterial blood * cardiac output
How can you calculate the venous O2 transport?
arterial O2 transport - cell use of O2
What doe sthe Fick equation tell us?
the Fick equation combined the mass flow equation and mass balance equation to relate oxygen consumption, cardiac output and blood oxygen content
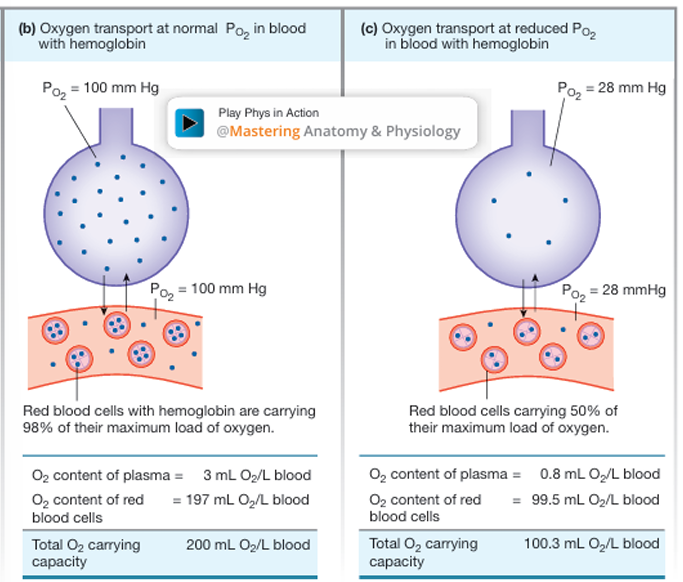
What are the 2 components oxygen transport has in blood?
oxygen that is dissolved in the plasma
oxygen bound to hemoglobin
What is the total blood O2 content?
dissolved O2 + O2 bound to Hb
What is the structure of hemoglobin?
a tetramer with four globular protein chains, each centered around an iron containing heme group. the central iorn atom of each heme group can bind reversibly with one oxygen molecule.
What makes the binding of hemoglobin with oxygen reversible?
the iron oxygen interaction is a weak bond that can be easily broken without altering the hemoglobin or the oxygen
What does Oxyhemoglobin(Hb(O2)1-4) mean?
hemoglobin is bound to 4 oxygen molecules
Which law does the hemoglobin binding reaction obey?
the law of mass action.
as the concentrations of oxygen increases, more oxygen binds to the hemoglobin and the equation shifts to the right producing more HbO2
What is the pathway oxygen takes from the pulmonary capillaries to the hemoglobin?
In the pulmonary capillaries,
oxygen from the alveoli first dissolves in plasma.
Dissolved O2 then diffuses into the red blood cells, where it can bind to hemoglobin. This happens until the reaction reaches equilibrium.
What is the pathway oxygen takes from the hemoglobin to the tissues?
dissolved oxygen idffuses out of the systemic capillaries, which have a lower PO2.
this decreases plasma PO2 and disturbs the equilbrium of the oxygenhemoglobin binding reaction.
the equilibrium shifts to the leftt, causing gemoglobin molecules to release their oxygen stores
On which 2 factors does the amount of oxygen binding to hemoglobin depend?
the PO2 in the plasma surrounding the red blood cells — primary factor
the number of potential Hb binding sites available in the red blood cells
By what is the arterial PO2 established?
the composition of inspired air
the alveolar ventilation rate
the efficiency of gas exchange from alveoli to blood
On What does the number of oxygen-binding sites depend?
on the number of hemoglobin molecules in red blood cells
What is the percent saturation of hemoglobin?
the amount of oxygen bound to hemoglobin at any given PO2
What does the shape of the oxyhemoglobin saturation curve reflect?
the proper ties of the hemoglobin molecule and its affinity for oxygen
At normal alveolar and arterial PO2 (100 mm Hg), 98% of the hemoglobin is bound to oxygen. The curve is nearly flat
at PO2 levels higher than 100 mm Hg., even large changes in PO2 cause only minor changes in percent saturation.
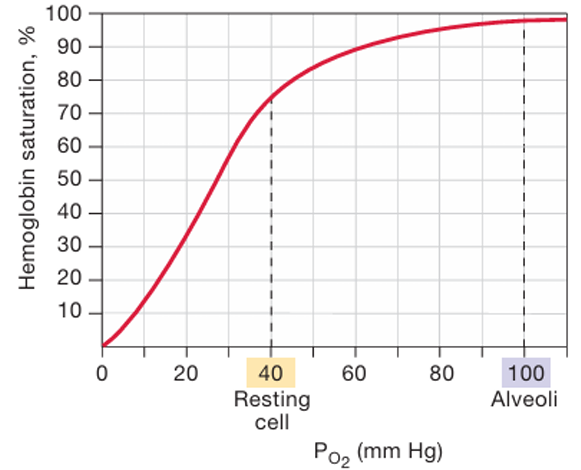
What does the flattening of the saturation curve at higher PO2 mean?
The flattening of the saturation curve at higher PO2 also means that alveolar PO2 can fall a good bit below 100 mm Hg without significantly lowering hemoglobin saturation.
In blood leaving systemic capillaries with a PO2 of 40 mm Hg, hemoglobin is still 75% saturated. What does this mean?
This means that at the cells, blood releases only one-fourth of the oxygen it is capable of carrying.
The oxygen that remains bound serves as a reservoir that cells can draw on if metabolism increases.
What factors change the conformation of hemoglobin, and so its ability to bind oxygen?
plamsa pH
temperature
PCO2
What decreases the affinity of hemoglobin to oxygen?
decrease in pH
increased temperature
increased PCO2
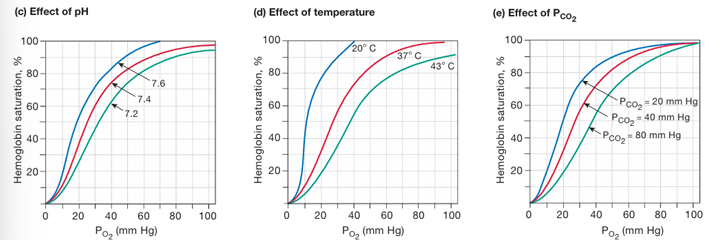
What decreases the affinity of hemoglobin to oxygen?
increase in pH
decrease in temperature
decrease in PCO2
What is the Bohr effect?
a shift in the hemoglobin saturation curve that results from a change in pH
What is the affect of 2,3-BPG on the binding affinity of oxygen?
Increased levels of 2,3-BPG lower the binding affinity of hemoglobin and shift the HbO2 saturation curve to the right. so more O2 is released
What does chronic hypoxia(extended period of low oxygen) trigger?
an increase in 2,3-BPG production in red blood cells
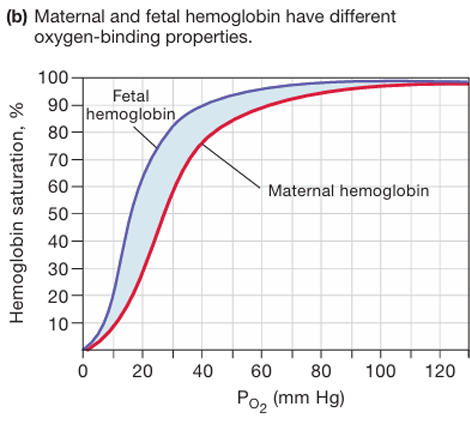
What are the characteristics of Fetal hemoglobin (HbF)?
it has 2 gamma protein chains in place of the 2 beta chains found in adutlt hemoglobin.
The presence of gamma chains enhances the ability of fetal hemoglobin to bind oxygen in the low-oxygen environment of the placenta.
Gas transport in the blood includes?
Gas transport in the blood includes carbon dioxide removal from the cells as well as oxygen delivery to cells.
What are the consequences of elevated CO2?
Elevated PCO2 (hypercapnia) causes; the pH disturbance acidosis.
Extremes of pH interfere with hydrogen bonding of molecules and can denature proteins.
Abnormally high PCO2 levels also depress central nervous system function.
For these reasons, CO2 must be removed, making CO2 homeostasis an important function of the lungs.
93% of CO2 diffuses into red … , where 23% binds to … while the remaining 70% is converted to …
93% of CO2 diffuses into red blood cells, where 23% binds to hemoglobin (HbCO2) while the remaining 70% is converted to bicarbonate ion (HCO3 -)
What are the 2 purposes of CO2 to HCO3- convertion?
it provides an additonal way to transport CO2 from the cells to the lungs
HCO3- is available to act as buffer for metabolic acids
What is the pathway CO2 takes the tissue to the lungs?
CO2 diffuses out of the cells into systemic capillaries
only 7% of the CO2 remains dissolved in the plasma
nearly a fourth of the CO2 binds to hemoglobin, forming carbaminohemoglobin
70% of the CO2 load is converted to HCO3- and H+. hemoglobin buffers H+.
HCO3- enters the plasma in exchange for Cl- —> the chloride shift
at the lungs, dissolved CO2 difusses out of the plasma
by the law of mass action, CO2 unbinds from hemoglobin and diffuses out of the red blood cell
the carbonic acid reaction reverses, pulling HCO3 back into the red blood cell and converting it back to CO2
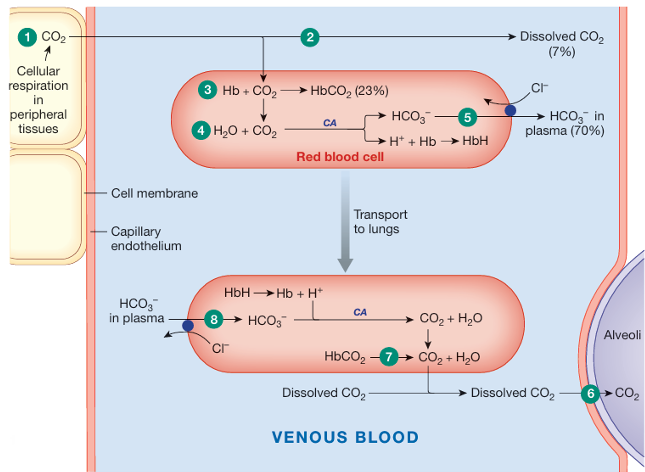
How do CO2 and H+ facilitate the formation of carbaminohemoglobin?
The presence of CO2 and H+ facilitates formation of carbaminohemoglobin because both of these factors decrease hemoglobin’s binding affinity for oxygen
What happens to bicarbonate (HCO₃⁻) and protons (H⁺) in red blood cells as CO₂ is exhaled in the lungs, and how does this facilitate CO₂ removal from the body?
As CO2 levels in the red blood cells decrease, the equilibrium of the CO2-HCO3 - reaction is disturbed, shifting toward production of more CO2. H+ unbinds from hemoglobin molecules and HCO3 - moves back into the red blood cells when the chloride shift reverses.
The HCO3 - and newly released H+ are converted back into water and CO2.
This newly made CO2 is then free to diffuse out of the red blood cell into the plasma and from there into the alveoli.
What increases the binding affinity of hemoglobin for oxygen?
a decrease in carbon dioxide (CO2) levels, an increase in pH (alkalosis), a decrease in temperature.
Additionally, the binding of one oxygen molecule to hemoglobin increases the affinity of the other binding sites for oxygen.
How is the contraction of the diaphragm and other muscles is initiated?
by a spontaneously firing network of neurons in the brain stem
On which 3 substances in the arterial blood and extracellular fluid does the ventilation pattern depend?
CO2
O2
H+
How does the brain stem network that controls breathing behave?
it behaves like a central pattern generater with intrinsic rhtyhmic activity that probably arises from pacemaker neurons with unstable membrane potentials
The model for the control of ventilation states that?
respiratory neurons in the medulla control inspiratory and expiratory muscles
neurons in the ppons integrate sensory information and interact with medullary neurons to influence ventilation
the rhythmic pattern of breathing arises from a brainstem neural networ with spontaneously discharging neurons
ventilation is subject to continuous modulation by various chemoreceptor and mechanoreceptor-linked reflexes and by higher brain centers
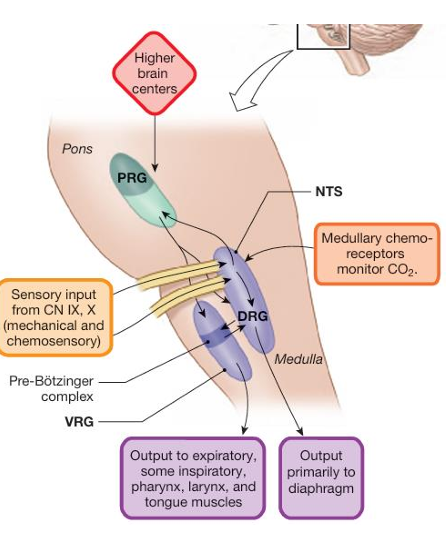
Respiratory neurons are concentrated bilaterally in which two areas of the medulla oblongata?
dorsal respiratory group (DRG) of neurons → controls mostly muscles of inspiration
ventral respiratory group (VRG)
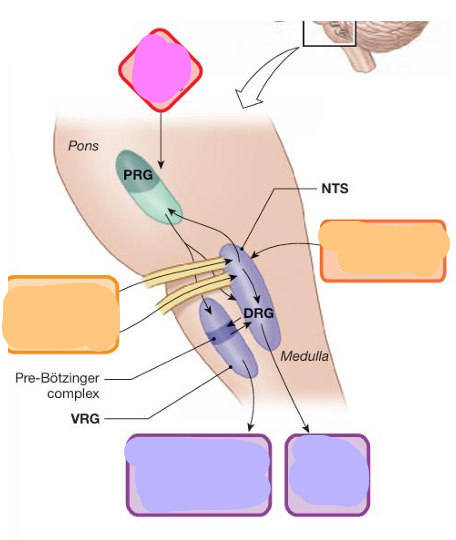
explain this figure
the PRG innervates both DRG and VRG
Output from the DRG goes via the phrenic nerves to the diaphragm and via the intercostal nerves to the intercostal muscles.
The NTS receives sensory information from peripheral chemo- and mechanoreceptors through the vagus and glossopharyngeal nerves.
Respiratory neurons in the pons receive sensory information from the DRG and in turn influence the initiation and termination of inspiration.
The VRG, contians the pre-Bötzinger complex, which contains spontaneously firing neurons that may act as the basic pacemaker for the respiratory rhythm.
nerve fibers from the VRG innervate muscles of the larynx, pharynx, and tongue to keep the upper airways open during breathing.
How does the firing rate of neurons influence the respiratory cyle?
A few inspiratory neurons fire to begin the ramp.
The firing of these neurons recruits other inspiratory neurons to fire in an apparent positive feedback loop.
As more neurons fire, more skeletal muscle fibers are recruited.
The rib cage expands smoothly as the diaphragm contracts.
At the end of inspiration, the inspiratory neurons abruptly stop firing, and the respiratory muscles relax.
Over the next few seconds, passive expiration occurs because of elastic recoil of the inspiratory muscles and elastic lung tissue.
With active expiration, expiratory neurons from the VRG activate?
the internal intercostal and abdominal muscles
What is the primarily stimulus for changes in ventilation?
CO2
If too little oxygen is present in arterial blood destined for the brain and other tissues, the rate and depth of breathing … ?
If too little oxygen is present in arterial blood destined for the brain and other tissues, the rate and depth of breathing increase.
"If the rate of CO₂ production by cells exceeds the rate of its removal by the lungs, arterial PCO₂ … . This triggers a rapid … , … ventilation to restore balance between CO₂ production and removal."
"If the rate of CO₂ production by cells exceeds the rate of its removal by the lungs, arterial PCO₂ rises. This triggers a rapid positive feedback loop, intensifying ventilation to restore balance between CO₂ production and removal."
What does the sensory input from the central and peripheral chemoreceptors modify?
Sensory input from central and peripheral chemoreceptors modifies the rhythmicity of the control network to help maintain blood gas homeostasis.
What do the peripheral chemoreceptors outside the CNS sense?
Peripheral chemoreceptors outside the CNS sense changes in:
PO2 ,
pH,
PCO2 of the plasma.
To what do the central chemoreceptors in the brain respond?
Central chemoreceptors in the brain respond to changes in;
the concentration of CO2 in the cerebrospinal fluid.
The primary central receptors lie on the ventral surface of the medulla, close to neurons involved in respiratory control.
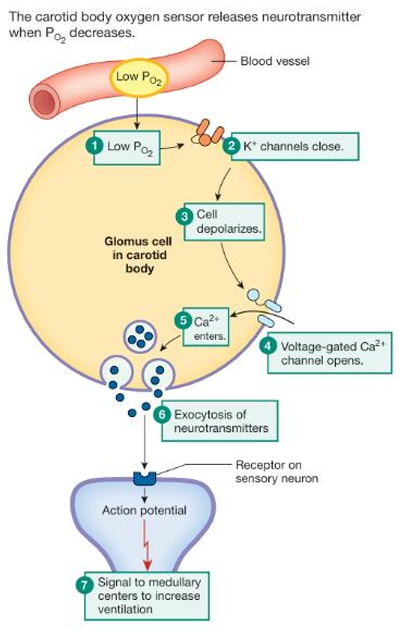
What is the molecular action of the caroid receptor when PO2 is decreased?
Low PO2
K+ channels close
cell depolarizes
voltage gated Ca2+ channels open
Ca2+ enters the cell
exocytosis of neurotransmitters
signal to medullary centers to increase ventilation
When are peripheral chemoreceptors activated?
when there is a decrease in;
PO2 → PO2 must fall to less than 60 mm Hg to stimulate ventilation.
pH
or an increase in:
PCO2
What is the molecular action of the central chemoreceptor when PCO2 is increased?
Central chemoreceptors respond to pH changes in the cerebrospinal fluid (CSF).
Carbon dioxide that diffuses across the blood-brain barrier into the CSF is converted to bicarbonate and H+.
The produced H+ by this reaction is what initiates the chemoreceptor reflex.
Although plasma PCO2 enters the CSF readily, plasma H+ crosses the blood-brain barrier very slowly and therefore has little direct effect on the central chemoreceptors.
When plasma PCO2 increases, the chemoreceptors initially respond strongly by increasing ventilation.
CO2 crosses the blood-brain barrier and activates the central chemoreceptors
these receptors signal the control network to increase the rate and depth of ventilation
enhancing alveolar ventilation and removing CO2 from the blood
However, if PCO2 remains elevated for several days, ventilation falls back toward normal rates as the chemoreceptor response adapts.
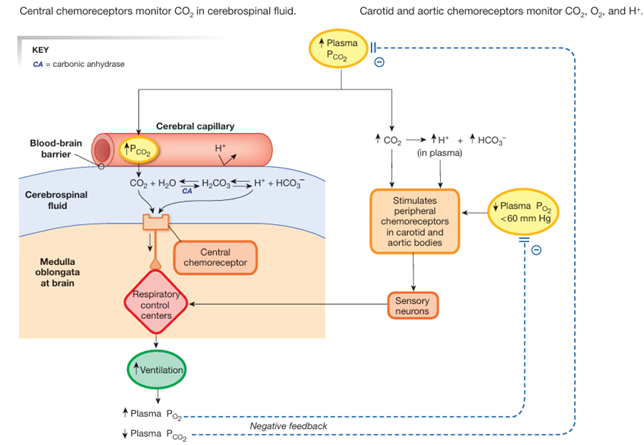
if PCO2 remains elevated for several days, ventilation falls back toward normal rates as the chemoreceptor response adapts.
How is this possible?
The adaptation appears to be due to increased CSF bicarbonate concentrations that buffer the H+.
How is bronchoconstriction initiated?
Inhaled particles or noxious gases stimulate irritant receptors in the airway mucosa.
the irritant receptors send signals through sensory neurons to integrating centers in the CNS
this triggers bronchoconstriction
How is bronchoconstriction mediated?
through parasympathetic neurons that innervate bronchiolar smooth muslce
Which parts of the brain influence respiratory activity beyond the brain stem control centers?
The hypothalamus and cerebrum can influence respiratory activity by altering the activity of the brain stem control network. The limbic system also affects respiration through emotional and autonomic responses.
Is input from higher brain centers required for normal breathing?
No, higher brain center input is not required for basic ventilation, which is primarily controlled by the brain stem.
How are the cardiovascular and respiratory systems connected in the brain?
Both systems have integrating centers in the brain stem, and interneurons connect the two networks, allowing for coordination of signals between them.
What three systems work together to maintain fluid and acid-base homeostasis?
The cardiovascular, respiratory, and renal systems work together to maintain fluid and acid-base balance in the body.