Nervous System Pathology
1/140
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
141 Terms
Monro-Kellie Hypothesis
-A supposition that states the cranial cavity cannot be compressed, and the volume inside the cavity is fixed (normal intracranial pressure is 4-15 mmHg).
-The skull and its components create a state of volume equilibrium, such that any increase in volume of one component must be compensated by a decrease in volume of another component.
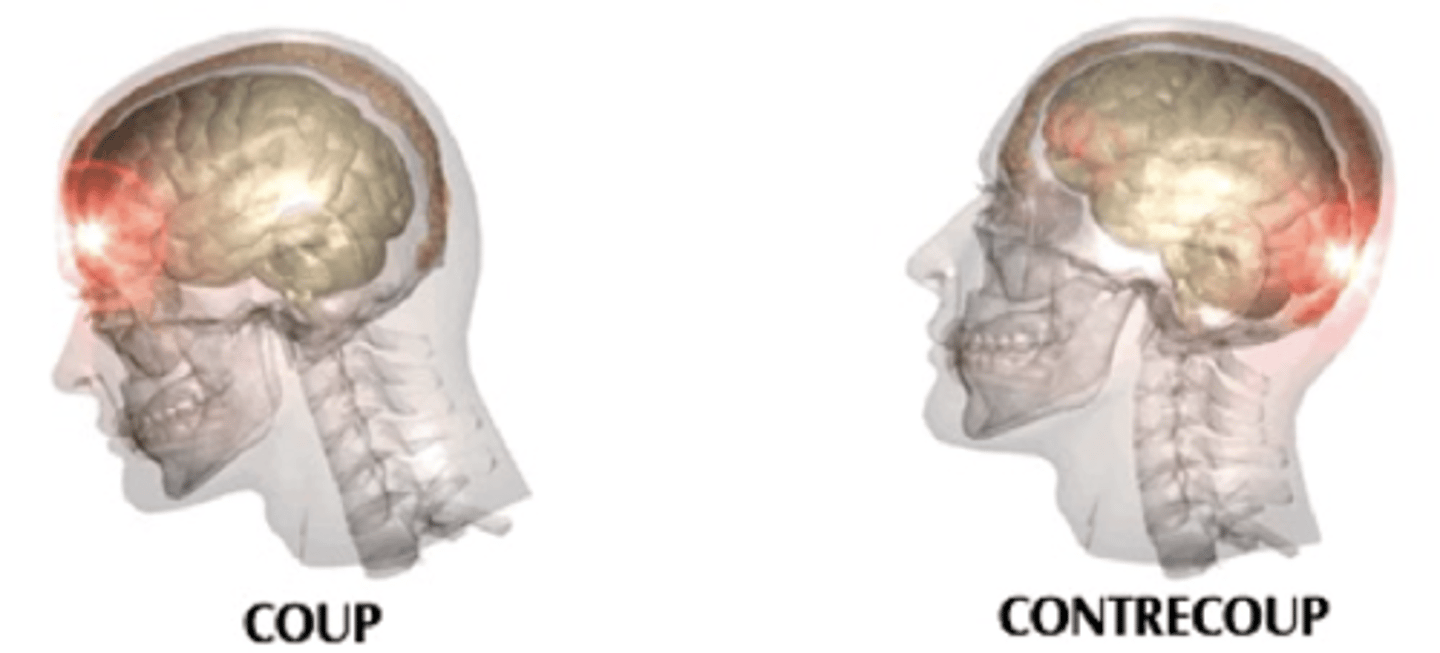
Cerebral Contusion
Acceleration-deceleration injury
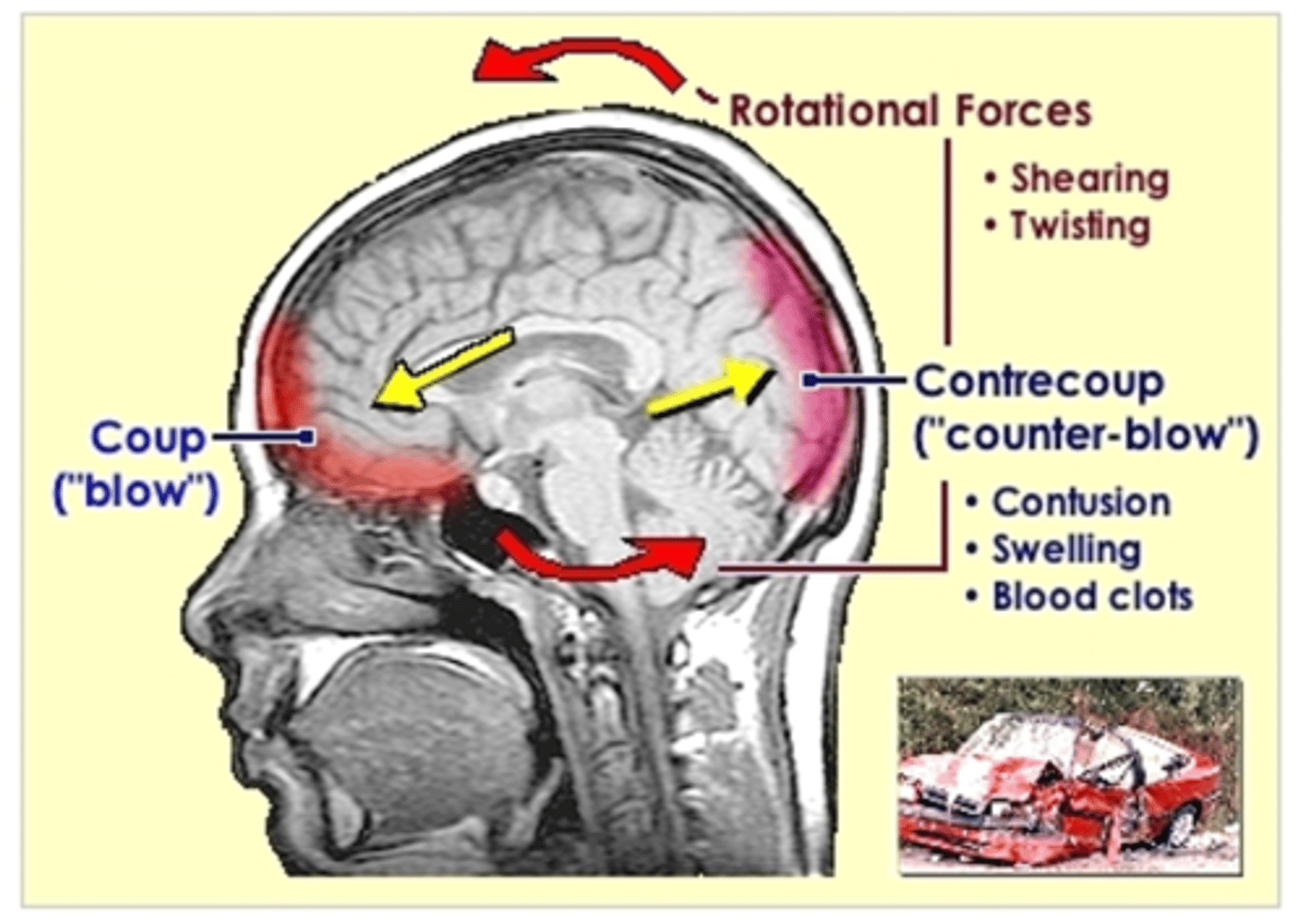
Location of coup injuries
site of impact
Counter-coup injury location
opposite the site of impact
countercoup is most common in
frontal and temporal lobes
Cerebral contusion causes permanent damage to
-small blood vessels
-surface of brain
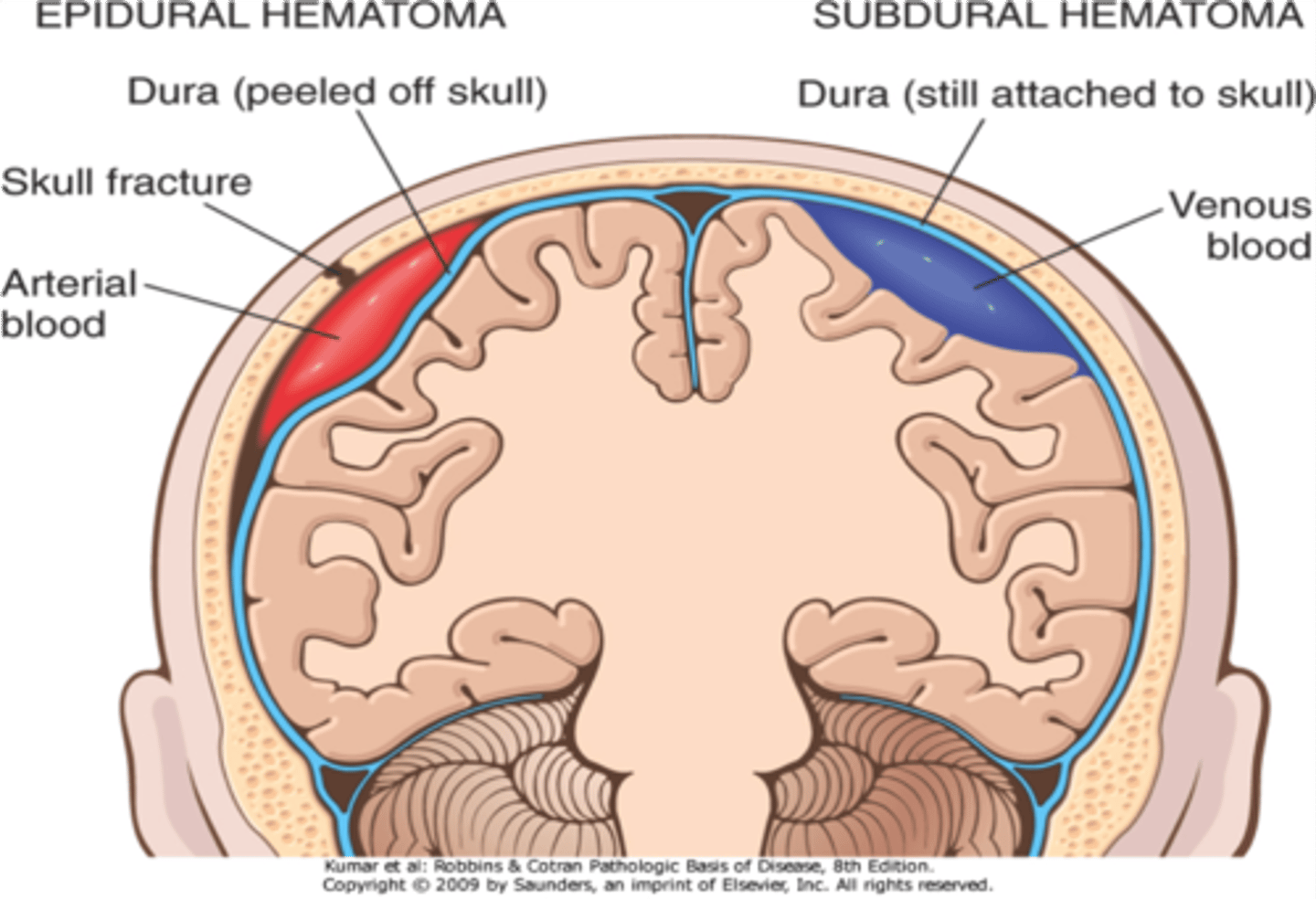
Major characteristic of an epidural hematoma
arterial bleed
location of epidural hematomas
-between bone and dura
(rarely crosses midline)
-middle meningeal artery
Cause of epidural hematoma
direct blow to head
Epidural hematoma pathogenesis
*middle meningeal artery tear
-blood between dura and bone
-increased intracranial pressure
-herniation (shift in brain tissue)
-death
How is an epidural hematoma diagnosed?
-CT
-Mass-effect on brain
(crescent-shaped)
Epidural hematoma treatment if minor
observation
Epidural hematoma treatment
Burr holes to relieve pressure
Major characteristic of subdural hematoma
Venous bleed
Location of subdural hematoma
between dura and arachnoid mater
causes of a subdural hematoma
-blunt trauma
-anticoagulation
-child abuse
-spontaneous
Subdural hematoma pathogenesis
tear in bridging veins between brain and dural sinuses
enlarging clot
-slow
-covers convexity of brain
-consciousness flunctuates
-herniation
-death
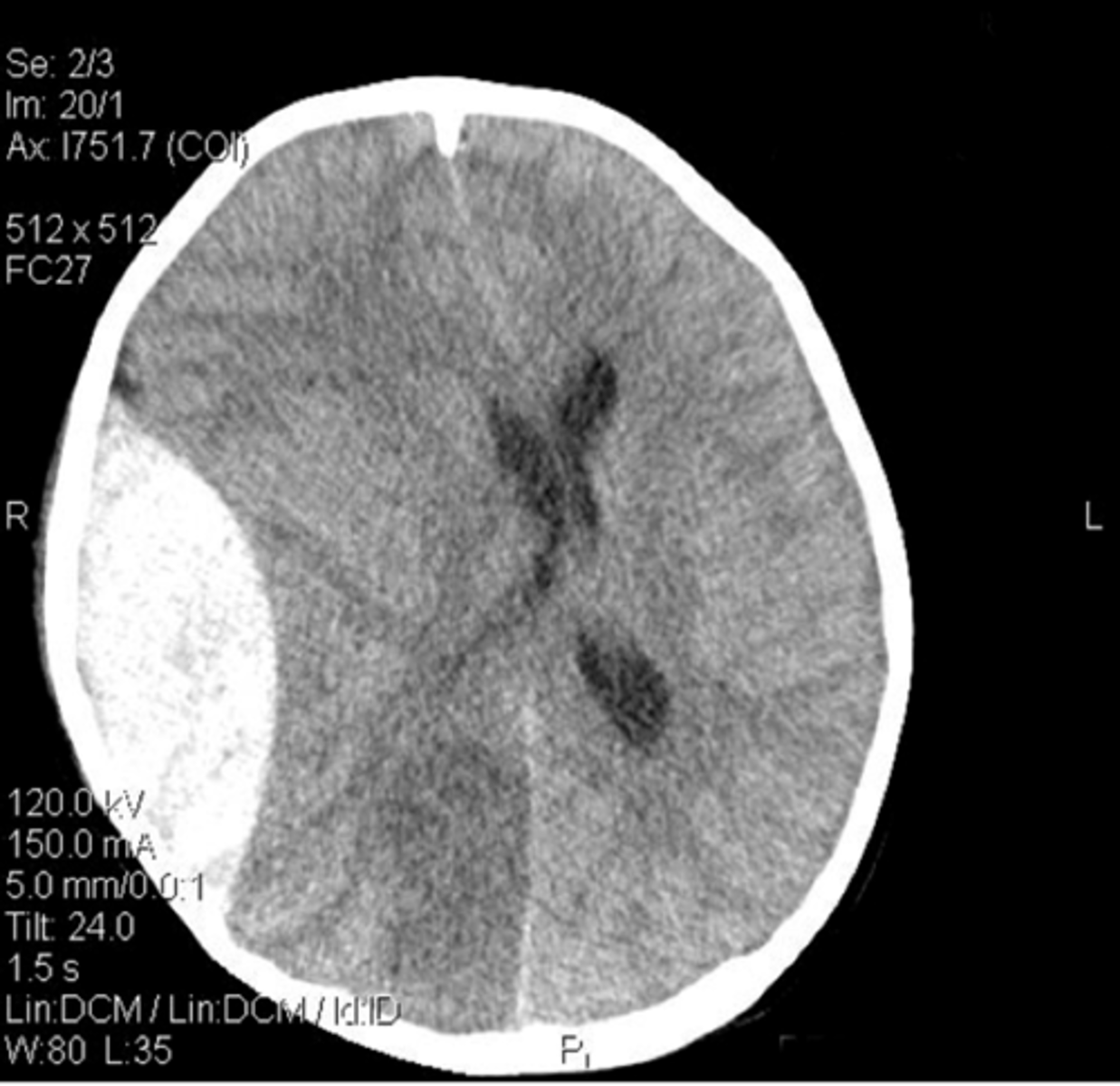
subdural hematoma diagnosis
-CT
-Mass effect:
A. midline shift
B. follows the shape of the brain

Subdural hematoma treatment
If minor -> observation
-Burr holes to relieve pressure
Hematomas: Epidural vs. Subdural
Traumatic Brain Injury (TBI)
Complex pathophysiologic process affecting the brain
-induced by traumatic biomechanical forces secondary to direct or indirect forces to the head
Hallmark of TBI
Diffuse axonal injury
Traumatic Brain Injury: 2 Phases
1. Diffuse axonal injury
-> rotational forces
2. Delayed phase
->inflammation, edema, ischemia
-free radicals, apoptosis
Pathophysiology of cerebrovascular diseases
Decreased blood supply/ oxygenation due to:
-hypoxia
-ischemia
-infarction
Global Hypoxic Injury underlying cause
lack of O2 to the brain
Global Hypoxic Injury causes
Cardiac arrest
Shock
CO poisoning
High altitudes
Choking
Stroke

Global Hypoxic Injury pathology
-Cerebral atrophy
-apoptosis of neurons
(known as red neurons)
-pyknotic nuclei
-spaces for apoptotic neurons
-laminar necrosis
Global Hypoxic Injury pathophysiology
-Watershed infarcts
-Blood distributions don't quite overlap
-Most common location = ant. + middle cerebral arteries
stroke
-loss of blood flow to an area of the brain
-specific neurologic deficits

Types of Strokes
-Ischemic
-Intracerebral hemorrhage
-Subarachnoid hemorrhage
-Lacunar stroke
most common type of stroke
ischemic (atherosclerotic)
Stroke diagnosis
-CT scan
(hemorrhagic vs. nonhemorrhagic)
-MRI to confirm
Stroke acute treatment
-thrombolytics if they qualify
-surgical evacuation of hemorrhagic strokes
Treatment for chronic strokes
-antiplatelets (ASA, clopidogrel)
-warfarin for embolic strokes
-treat underlying diseases
Thrombotic stroke pathogenesis
Platelet thrombosis over atherosclerotic plague
most common thrombotic stroke location
middle cerebral artery
thrombotic stroke locations
-middle cerebral artery
-Bifurcation of common carotid
(int. carotid artery)
-Basilar artery
Pale infarctions
-peripheral of cortex
-no hemorrhage
Swelling of brain
-loss of grey/white matter borders
-myelin breakdown
gliosis
-reaction to injury
-astrocytes proliferate
-microglial (macrophages) cells remove debris
Clinical findings for MCA thrombotic stroke
-contralateral hemiparesis
-sensory loss in face and UE
-Broca's aphasia
-visual defects
-head and eyes deviate toward lesion
Clinical findings for ACA thrombotic stroke
contralateral hemiparesis
sensory loss in LE
Clinical findings for Vertebrobasilar thrombotic stroke
vertigo
ataxia
ipsilateral sensory loss in face
contralateral hemiparesis
sensory loss in trunk and limbs
Thrombotic stroke clinical findings are _ dependent
location
Thrombotic strokes commonly precede a
TIA (ischemia w/o infarction)
Thrombotic stroke treatment
-Prevention:
(ASA, clopidogrel, statins)
-PT/OT
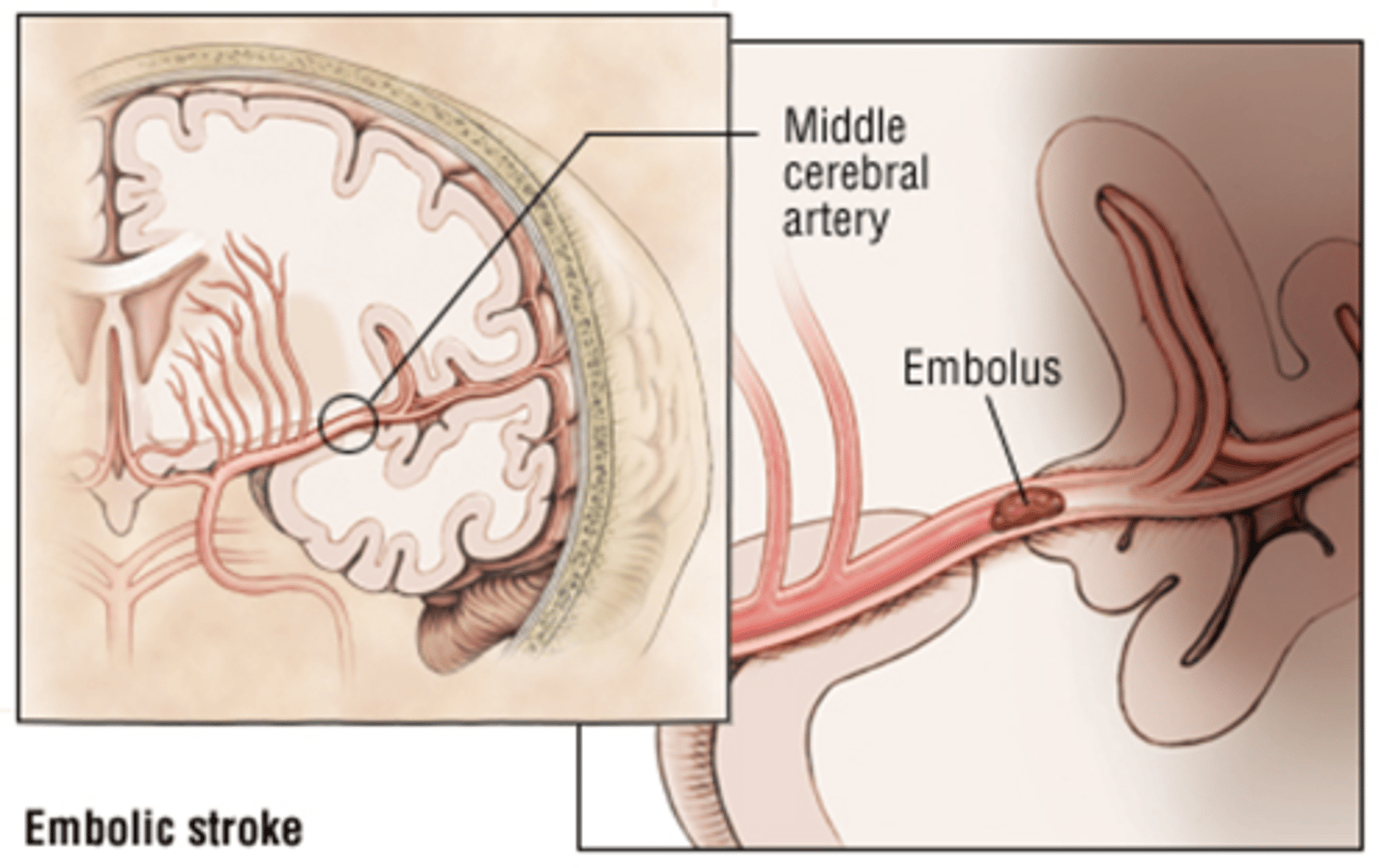
Embolic Stroke
Ischemic stroke due to embolus
(AKA -> hemorrhagic stroke)
Sources of emboli
1. left heart
2. atrial fibrillation
3. fat embolus
4. amniotic fluid
5. Tumor emboli (in cancer patient)
Embolic stroke common locations
-MCA
-Vessel reperfusion
Intracerebral Hemorrhage pathogenesis
-HTN causes stress on vessels
-Microaneurysms develop
-Aneurysms rupture
-Hemorrhage / hematoma
Intracerebral Hemorrhage location
basal ganglia (most common)
Thalamus
Pons
Cerebellum
Subarachnoid Hemorrhage causes
Rupture of a berry aneurysm (most common)
AV malformation
Berry aneurysm risk factors
-Normal hemodynamic stresses
-HTN
-Coarctation of aorta
-Atherosclerosis
-Smoking
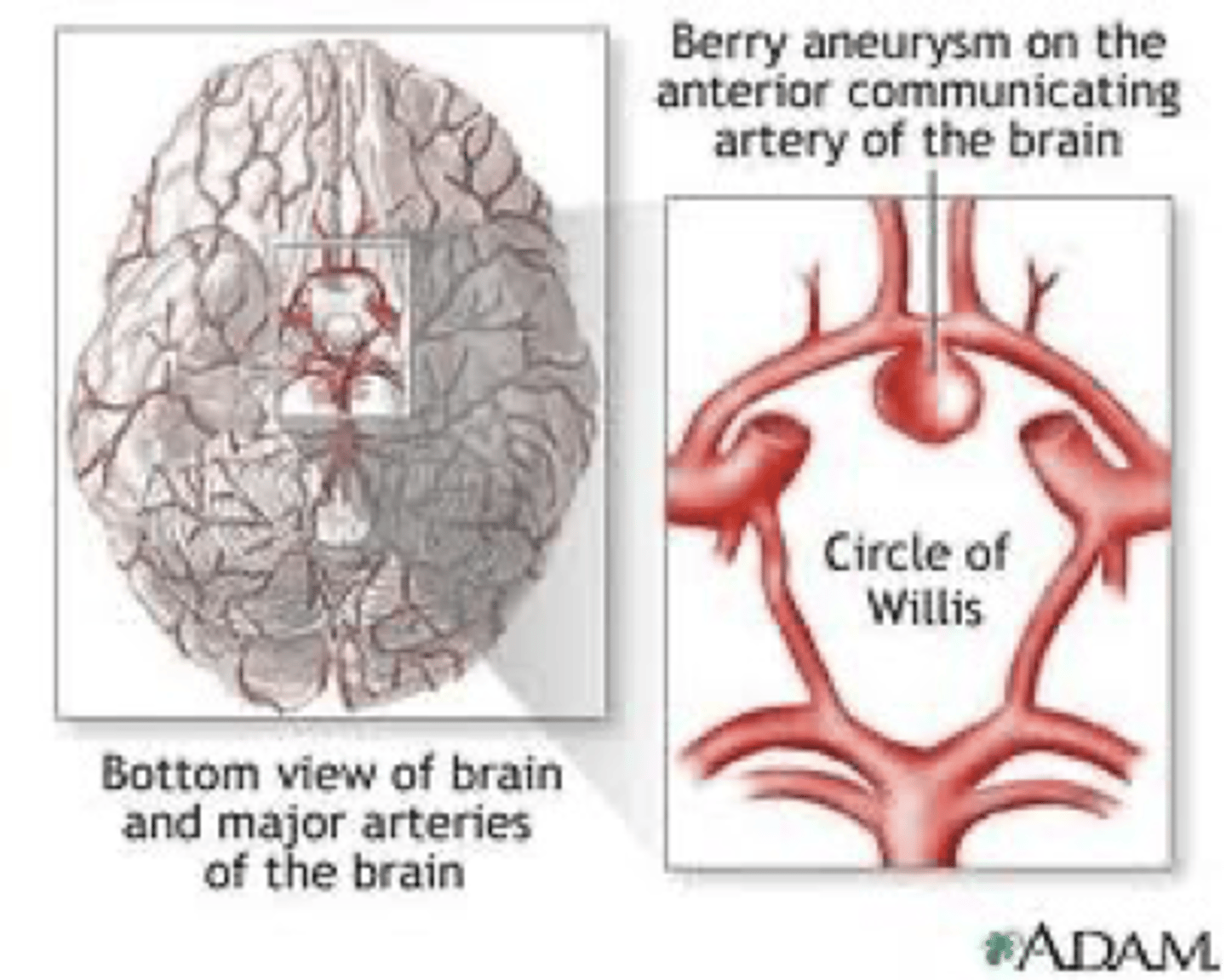
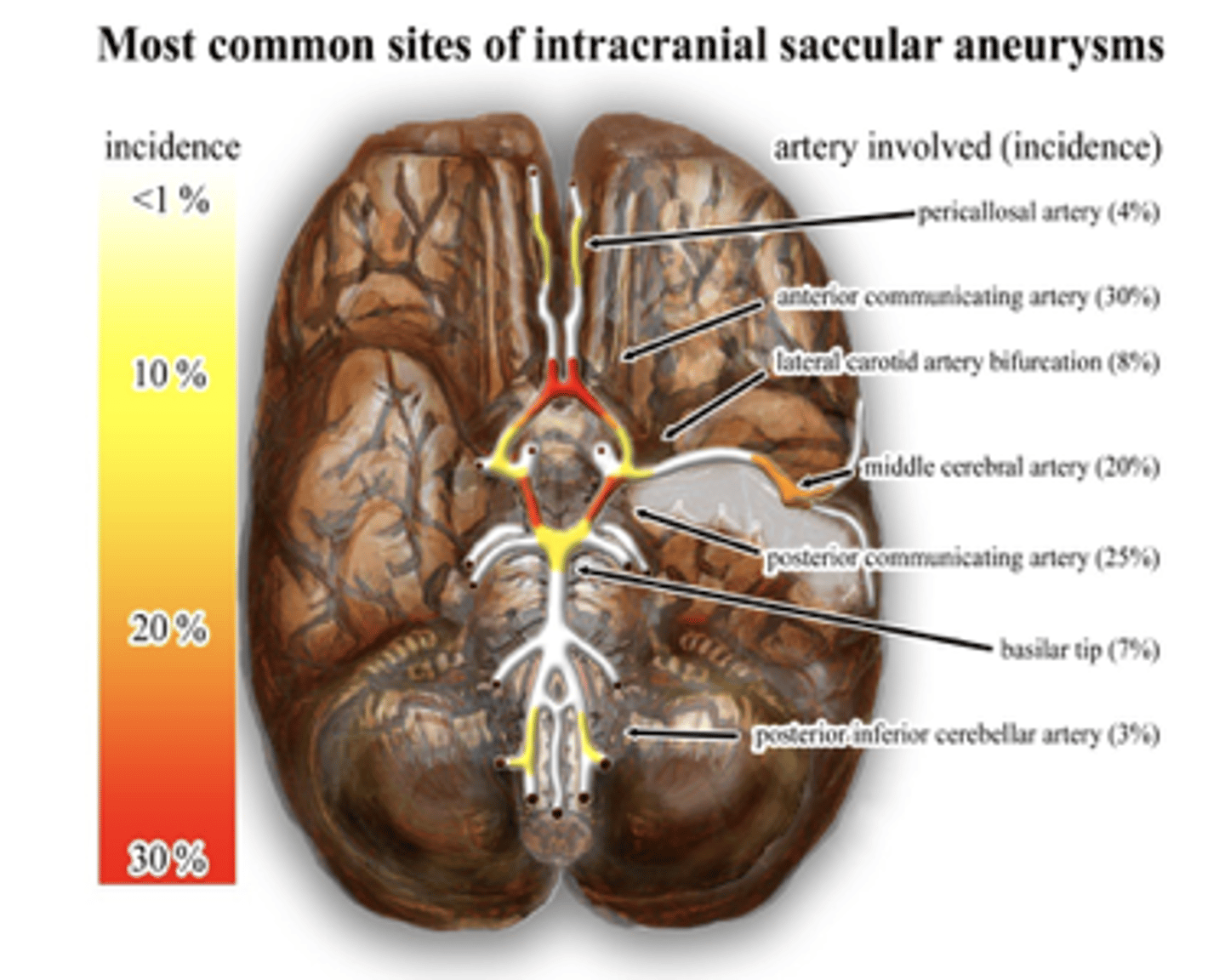
Berry aneurysm locations
-Communicating branches with main cerebral artery
-Anterior communicating branch (Most common)
Rupture of a berry aneurysm causes a
subarachnoid bleed
(blood covers surface of brain)
berry aneurysm clinical findings
***Worst headache of their life
(thunderclap headache)
-50% mortality
-CSF becomes yellow: AKA: xanthochromia
(Bilirubin from breakdown of RBC's)
Lacunar Infarcts pathogenesis
Arteriosclerosis
Lacunar Infarcts most common cause
Hypertension
Neural tube defects
-birth defects in brain, spine & sp. Cord
-due to improper circulation
Anencephaly
absence of most of brain
Spina bifida
fetal spinal column doesn't close
Meningocele
herniation of meninges through spinal column defect
Neural tube defects can be prevented with
folic acid
hydrocephalus pathology
too much CSF within skull
2 classifications of hydrocephalus
1. Communicating = too much CSF
2. Noncommunicating = obstruction of CSF flow
Hydrocephalus: infant Clinical Manifestations
large head
rapid increase in head size
bulging fontanelles
vomiting
lethargy
irritability
high-pitched cry
seizures
developmental delays
Hydrocephalus: older kids/adult Clinical Manifestations
headache
nausea / vomiting
vision issues
sluggish pupils
problems with balance, coordination or gait
extreme fatigue
slowing or regression of development
confusion
irritability
personality, memory, cognition changes
Hydrocephalus diagnosis
Exam:
-head circumference
-neurologic exam
Imaging:
-prenatal US, CT head, MRI, skull x-ray, cranial US
hydrocephalus treatment goal
minimize brain damage (by decreasing CSF flow)
hydrocephalus treatment
*Surgery
placement of shunts:
ventriculoperitoneal
ventriculoatrial
Leading cause of childhood disability in the US
Cerebral Palsy
(Group of disorders that appear in infancy or early childhood)
Cerebral palsy permanently affects
1. motor movement
2. muscle coordination
3. cerebral function (cognition & communication)
cerebral palsy is most commonly due to
damage to the cerebellum during birth or prenatal
Risk factors / contributing factors for cerebral palsy
prematurity
low birth weight
breech births
multiple fetuses
hypoxia
hypoglycemia
cerebral hemorrhage
neurologic infections
head injury
maternal infections
maternal toxin exposure
Clinical manifestations of cerebral palsy
persistence of early reflexes
developmental delays
ataxia
spasticity
flaccidity
hyperreflexia
asymmetrical gait
unusual limb positioning
tremors
difficulty with precise movements
balance and coordination issues
scoliosis
Cerebral Palsy diagnosis
-exam
-head CT and / or MRI
-EEG
-vision screen
-hearing screen
Cerebral palsy treatment
-muscle relaxants
-antiseizure meds
-pain management
-PT / OT
-assistive devices
-surgery to relieve contractures
Arnold-Chiari Malformation
medulla & cerebellum extend through foramen magnum
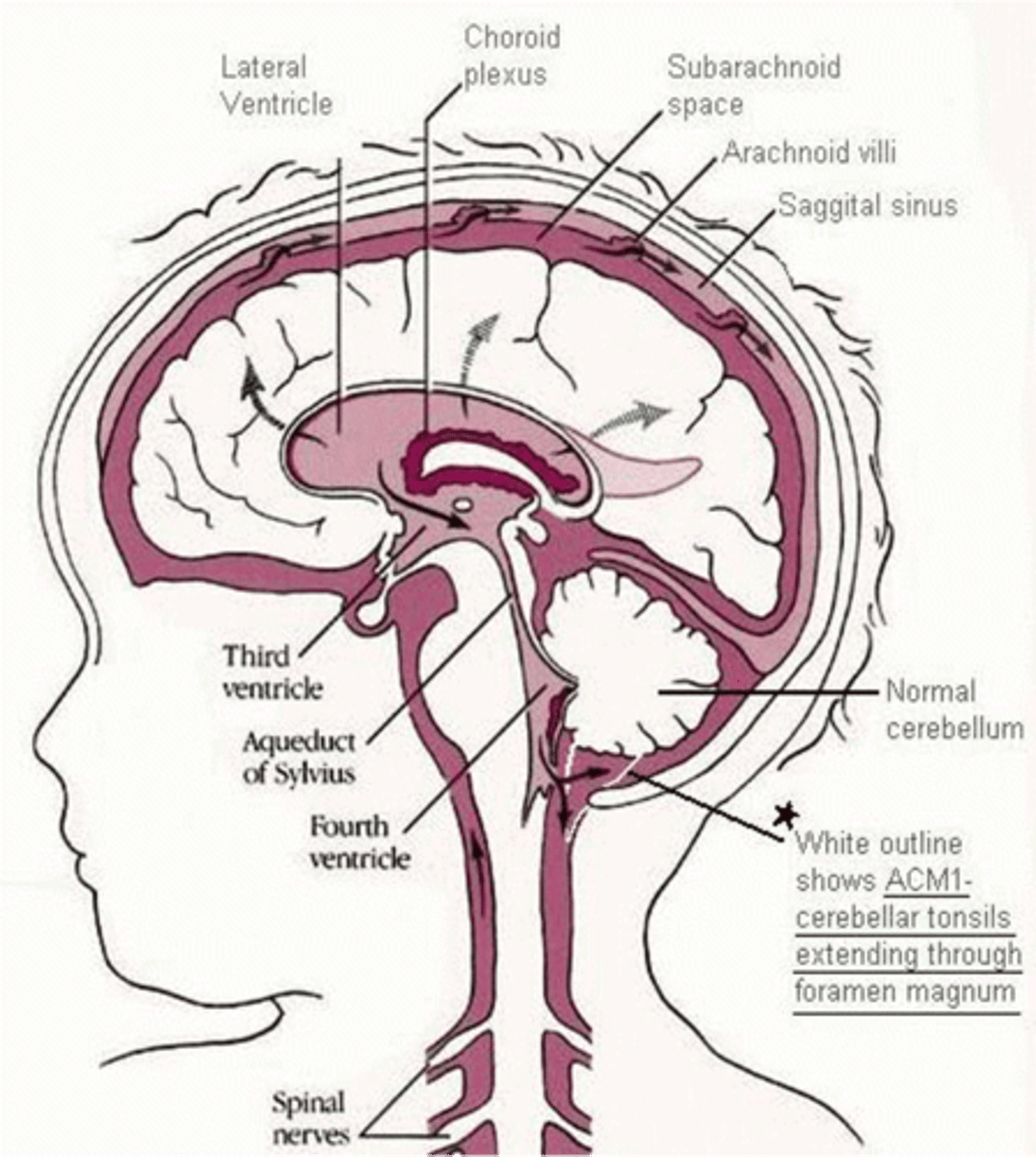
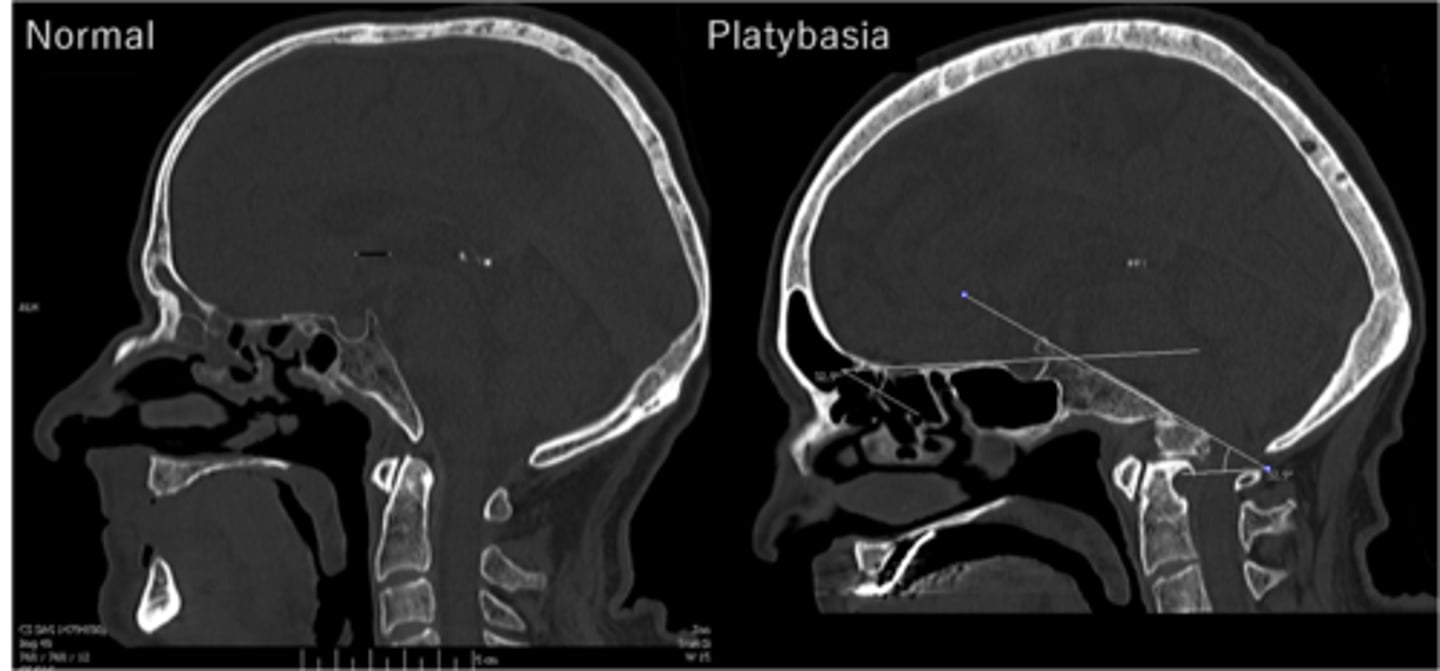
Platybasia
flat skull
Arnold-Chiari Malformation treatment
decompression
Dandy-Walker Malformation
partial or complete absence of the cerebellum
-Leads to dilation of 4th ventricle
-Noncommunicating hydrocephalus
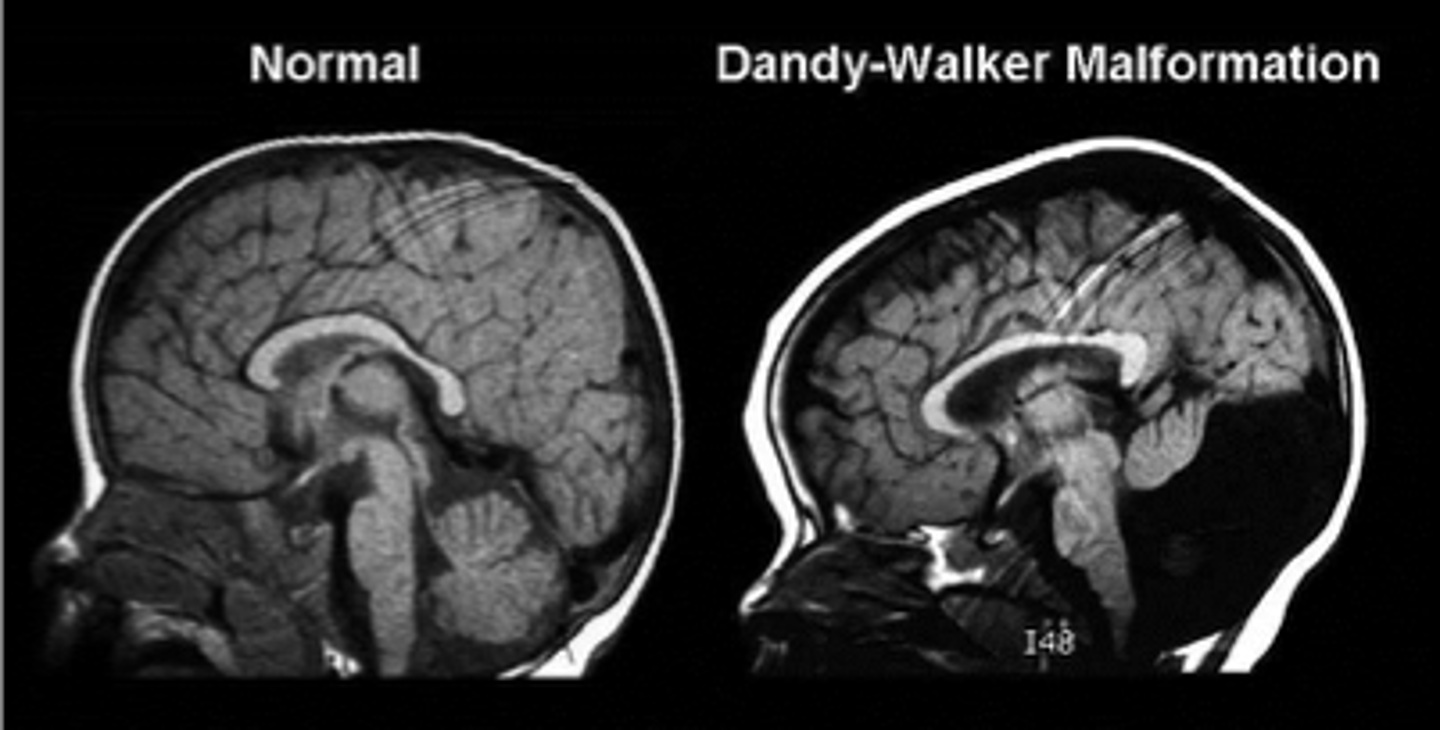
Dandy-Walker Malformation treatment
shunt
Syringomyelia
-cyst within spinal cord (fluid filled)
*Leads to cloak-like distribution of loss of pain and temp sensation

Neurofibromatosis
Two types NF1 and NF2

Neurofibromatosis clinical findings
-Disordered growth of ectodermal tissue
-Tumors or malformations of the CNS
Most common demyelinating disease
Multiple Sclerosis
Multiple Sclerosis pathogenesis
-CD4 TH1 and TH17 cells react against myelin antigens
-CD4 TH1 cells secrete interferon to activate macrophages (releases TNF)
-TH17 cells secrete cytokines to recruit neutrophils and monocytes
-WBC and TNF attack myelin and oligodendrocytes
-demyelination occurs
-antibodies created to continue process
MS gross pathology
demyelinating plagues in white matter
MS histopathology
inflammatory infiltrate
MS symptoms
sensory dysfunction
UMN disease
muscle spasms
spasticity
weakness
fatigue
optic neuritis
scanning speech
MS treatment
DMARDs
symptomatic tx
MS diagnosis
MRI
Amyotrophic Lateral Sclerosis
AKA: ALS or Lou Gehrig's disease
ALS involves
damage to UMN + LMN
ALS does not involve
-sensory neurons
-cognitive function
-CN III, IV, or VI
Possible causes of ALS
-Increased glutamate levels
-Free radical damage
Early clinical manifestations of ALS
footdrop
LE weakness
hand weakness or clumsiness
muscle cramps / twitching
later symptoms of ALS
paralysis
respiratory failure
difficulty swallowing
difficulty chewing
ALS diagnosis
-EMG
-muscle biopsy
-lumbar puncture with CSF testing
ALS treatment
NO CURE!!!
-some meds will slow progression
-symptomatic meds -> Rilutek
-PT / OT
-therapy