L2, Ch 6: Professional Attitudes and Communications
1/42
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
43 Terms
Issues of Cultural Diversity (4)
The scope of diversity
Culturally significant attitudes that may impact communication
how cultural issues may affect care
professional responsibilities and ethics in relation to diversity
The Scope of Diversity
Examples of cultural groups one may encounter
Gender groups: M/f
Racial groups: Distinguished by skin color and other
physical characteristics
Generational groups: millennial, boomers, gen z
Geographic groups: North or south; east coast or west
coast; native cultures in Hawaii, Alaska etc
Sexual-preference groups: Heterosexual, gay, lesbian,
bisexual, and transgender
Religious groups
Groups based on nonracial physical characteristics (the blind, the deaf, the disabled, the obese)
Socioeconomic groups
Groups with various types of family structure (singles, unmarried couples with and without children, traditional nuclear families, single parents, parents with children and grandchildren, and large, close-knit extended families)
Culturally Significant Attitudes That Can Affect Communication
Eye contact, touch, and gestures have different meanings in different cultures
Eye contact may be seen as impolite
Touching in professional setting should be confined to that needed to provide health care
important to know the meanings in the cultures that live in your area
How Cultural Issues May Affect Care
Some ethnic cultures have a high level of sensitivity surrounding modesty and physical contact in health care
Elders have observed advances in medicine and is unlikely to question the need vs Boomers more conservative/questioning attitude toward medical establishment
Geographical differences
Religion (some groups prohibit specific practices)
Inability to pay for health insurance
Sizeism - discriminating against someone based on his or her size
Review Box 6.1 Suggestions for Improving Communication and Care With Specific Ethnic Groups
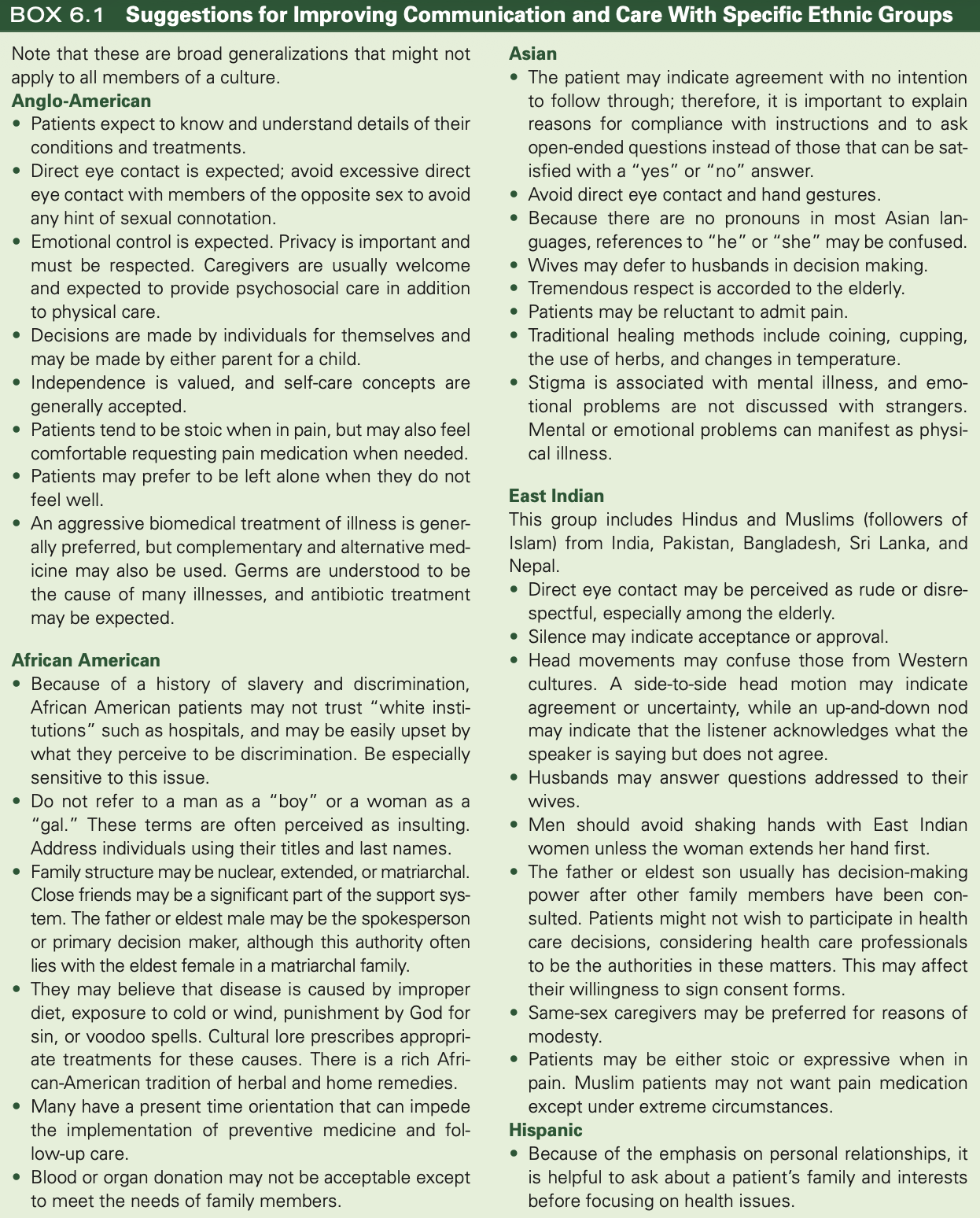
Review Box 6.1 Suggestions for Improving Communication and Care With Specific Ethnic Groups
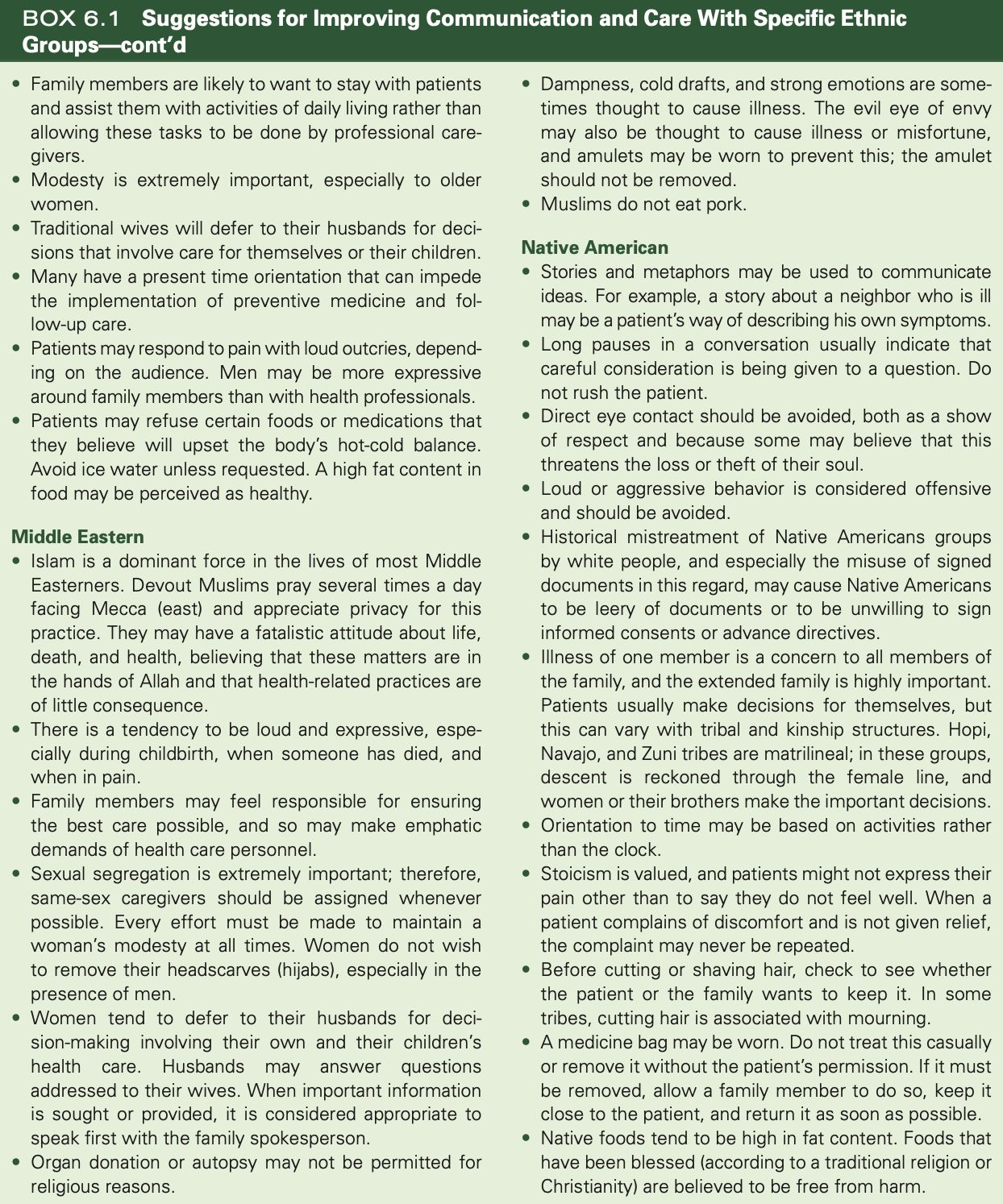
Review Box 6.1 Suggestions for Improving Communication and Care With Specific Ethnic Groups
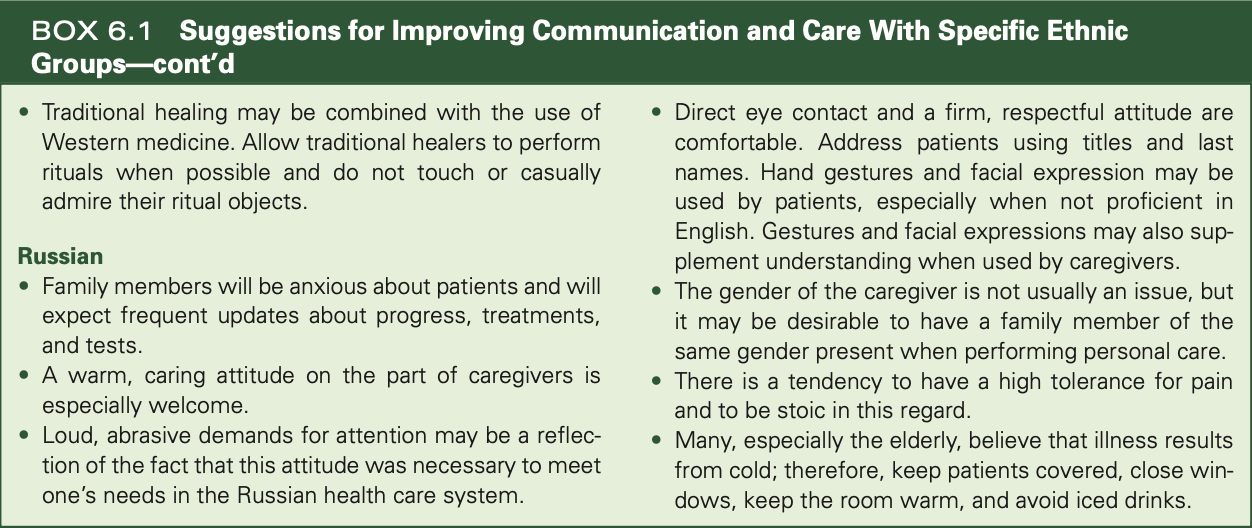
important to recognize that not all individuals in a cultural group will share the same characteristics
Professional Responsibility and Ethics in Relation to Diversity
The American Registry of Radiologic Technologists Code of Ethics requires radiographers to put aside all personal prejudice and emotional bias, rendering services to humanity with full respect for the dignity of individuals
conduct themselves in professional manner
support colleagues
respond to patient needs
deliver patient care/service unrestricted by concerns of personal attributes or the nature of the disease and without discrimination on the basis of sex, race, creed, religion, socioeconomic status
Communication Skills (6)
Nonverbal communication
listening skills
verbal skills
attitude
validation of communication
communication under stress
Nonverbal Communication
eye contact
touching
professional purpose that is clear to patient
appearance
Appearance communicates how we feel about our work and our patients
Neat uniforms
Clean examination room
Interpreted based on cultures
Listening Skills
Requires more than waiting for your turn to speak
Ability to give the speaker your full attention and focus
Verbal Skills
Ability to use language and content that is appropriate for your patient
age appropriate language (ex: pediatric pain vs ow)
Attitude
Nonverbal cues communicate attitude (ex: crossed arms, stoic face, tense)
Assertiveness is often necessary (calm, firm, neutral feelings)
Not to be confused with aggressiveness (hostile, impatient, anger, frustration)
Validation of Communication
An indication of a clear understanding of the message
smile, nod, ok
Without validation, neither party can be certain that all
elements of a message have been correctly understood.
Communication Under Stress
Stress interferes with our ability to process information accurately and appropriately
Suggestions to improve communication effectiveness in a crisis situation:
Lower your voice, speak slowly, and clearly.
Be nonjudgmental in both verbal and nonverbal cues.
Do not allow another’s inappropriate actions or speech to goad you into a similar response
Request confirmation when you are uncertain of the listener’s understanding.
Communication With Patients (6)
Addressing the patient
Valid choices
Avoiding assumptions
Assessment through communication
Therapeutic communication
Addressing the Patient
Introductions are normally first
Avoid impersonalizing patients, such as identifying patient by the exam rather than by name
Address patient appropriately
don’t use “honey, sweetie etc”
For many people, the stress of hospitalization is reflected in a strong feeling of helplessness or loss of autonomy (self-determination)
Valid Choices
Defined as alternatives that are all acceptable to you
Provide patient with a sense of participation in his or her care
“gowns vs pants”
“do you want to use the bathroom before exam?”
Avoiding Assumptions
Helps in preventing errors during procedures (ask patient to clarify)
Examples
Use of routine positioning techniques for all outpatients
Patient understood and followed preparation procedures for contrast
Assessment Through Communication
Combining observation with therapeutic communications to determine patient’s ability to cooperate with the examination
“how much more can you move, can you get on the table?”
Therapeutic Communication
Process in which the health care professional consciously influences a client or helps the client to a better understanding through verbal and/or nonverbal communication
involves the use of specific strategies that convey acceptance and respect and that encourage the patient to express feelings and ideas
See Table 6-1
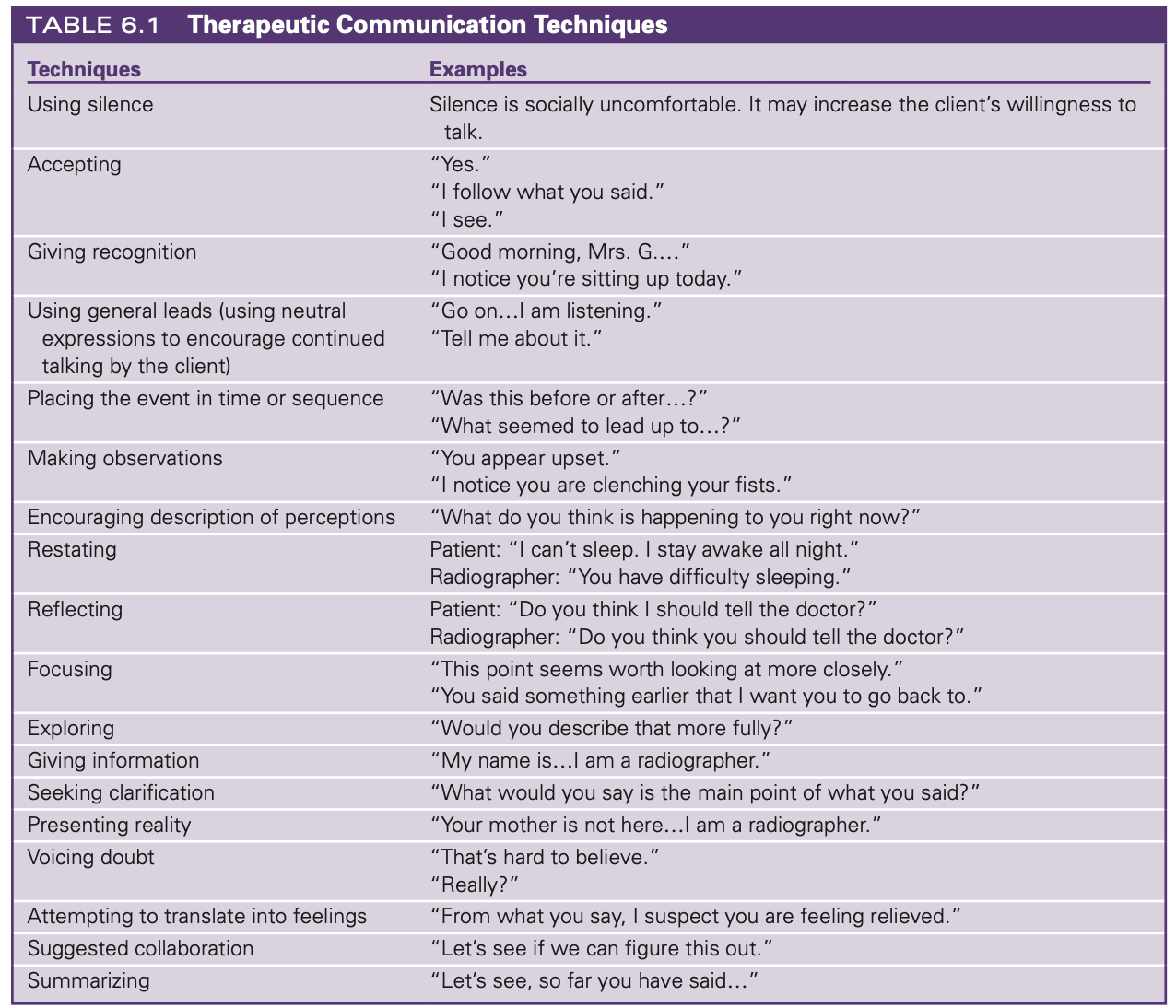
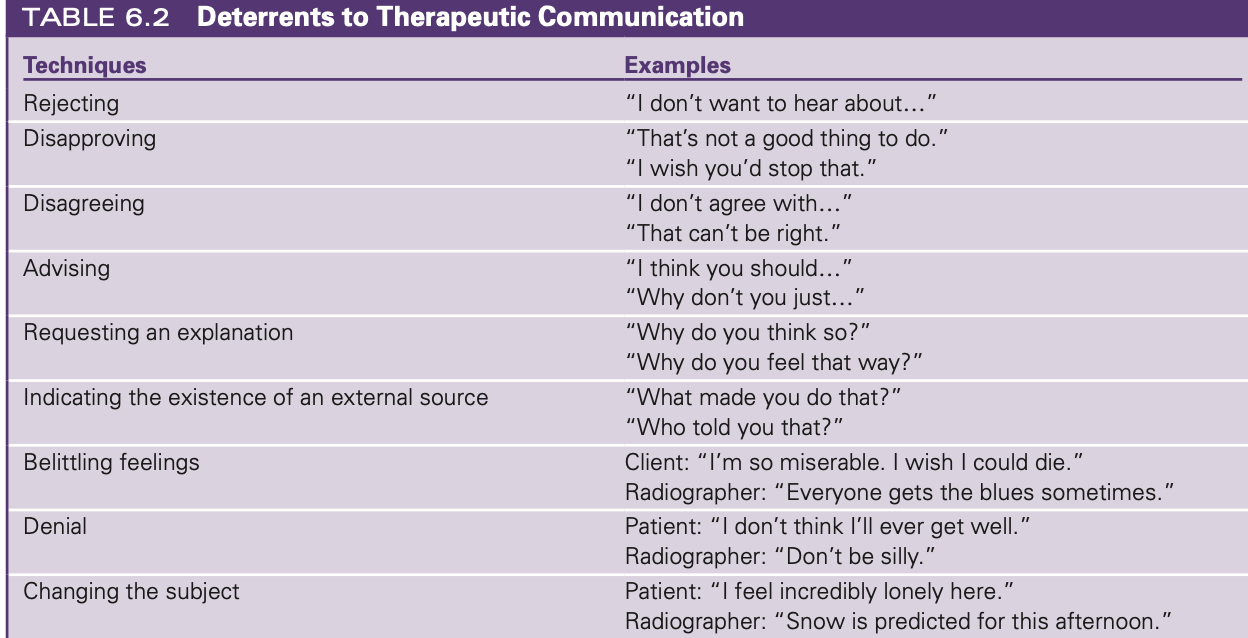
Table 6.2 Deterrents to Therapeutic Communication
Special Circumstances That Affect Communication (7)
Patients who do not speak English
The hearing impaired
Deafness
Impaired vision
Inability to speak
Impaired mental function
Altered states of consciousness
Important to recognize that sensory deprivation or loss does not affect mental capacity
Treat patients who are deaf, blind, or speech impaired with respect
Patients Who Do Not Speak English
Federal law guarantees patients the right to effective communications
Larger hospitals commonly employ interpreters and provide signs in several languages
Other facilities have “on-call” interpreters
Use of family members as interpreters often problematic
can’t rely on the info they relay
simple instructions are ok
When using an interpreter, look at the patient when speaking
Looking at the interpreter makes the patient feel excluded
The Hearing Impaired
Talk to, not about, these persons
show lips so they can read
Get the patient’s attention before starting to speak.
Face the person, preferably with light on your face.
Hearing loss is frequently in the upper register, so speak lower as well as louder.
Speak clearly at a moderate pace, and do not shout.
Avoid noisy background situations.
Rephrase when you are not understood the first time
Be patient
Deafness
Deaf persons have their own culture
chart should be flagged to alert care providers that patient is deaf
Certified interpreters usually necessary for effective communications
don’t shout; use lower voice/deeper voice
Impaired Vision
Ability to function depends on degree of vision loss and length of time since sight was lost or impaired
Useful to ask what assistance is needed
some prefer to touch your elbow as guide
others prefer description of surroundings
effective communication essential
Knock on door before entering
Inability to Speak
Aphasia is a defect or loss of language function in which comprehension or expression of words is impaired because of injury to language centers in the brain
Helpful to ask nursing staff about useful methods of communication
Some can write; others will nod to indicate understanding
One tool for those who cannot otherwise talk is the handheld electrolarynx. This device is placed on the external throat wall and operates by amplifying vibrations transmitted through the tissues of the neck
Impaired Mental Function
Abilities vary, so individual assessment is key
Inappropriate to treat adults with mental disabilities as if they were children
Repeating instructions is often useful.
Altered States of Consciousness
Important to communicate as if the patient can hear and respond
Constant observation is required to avoid accidents.
Tips:
Do not rely on patient to remember instructions.
Patients are not responsible for their actions/answers
Age-Specific Communication
Neonate and infant (birth to 1 year)
Toddler (1–2 years)
Preschooler (3–5 years)
School age (6–12 years)
Adolescent (13–18 years)
Young adult (19–45 years)
Middle adult (46–64 years)
Late adult (65–79 years)
Old adult (80 years and older)
Important to learn and practice age-specific communication skills
get on kid’s eye level
Avoid stereotypes.
Ageism is a discriminatory attitude toward the elderly that includes a belief that all elderly are ill, disabled, worthless, or unattractive.
Patient Education
Patient teaching
Communication with patients’ families
Communication with coworkers
Dealing with death and loss
when you don’t know answer to question, don’t tell patient “I don’t know”
offer to find the answer and/or tell them to ask physician
Patient Teaching
Opportunities
During the explanation of procedures
While responding to patient concerns
As part of the instructions needed to prepare for a procedure
During instruction for follow-up care
Written materials useful for complex preparation or follow-up
Communication with Patient’s Families
Empathy and patience are required
Useful information:
Restrooms
Cafeteria
Waiting areas
Length of procedure
Delays encountered
Follow-up care
Although you should always refer inquiries about diagnosis (identification of condition) or prognosis (prediction of outcome) directly to the physician in charge, an expression of concern can demonstrate empathy. “I know you are worried about Barbara, Mr. Rudd. I’ve let the doctor know you’re waiting for the results.
Communication with Coworkers
Cooperation with other healthcare providers makes it easier to accomplish common goals for patient.
Good interpersonal communication skills are essential.
Effective, efficient communications
Be a good listener.
Avoid gossip
Know legal implications of communications with others in the healthcare environment
Dealing with Death and Loss
Kübler-Ross stages of grief:
Denial—refuses to accept the truth; may refuse to discuss the possibility of loss or death
Anger—experiences frustration, outrage; may vent on healthcare workers
Bargaining—attempts to earn forgiveness or mitigate loss by being “very good”
Depression—often acquiescent, quiet, and withdrawn, and may cry easily
Acceptance—accepts the loss or impending death and deals with life and relationships on a more realistic, day- to-day basis
Hospice
an approach to care for the terminally ill that seeks to provide comfort without treating the underlying disease.
Palliative
a substance or treatment that soothes or relieves but is not intended to cure.
The principle of providing healthcare services with full respect for the dignity of humankind is:
A. established by law.
B. included in the ASRT Code of Ethics.
C. applicable only to physicians.
D. impossible to implement
B. included in the ASRT Code of Ethics.
Belief in the ancient superstition of the mal ojo, or "evil eye," is most likely to be encountered in individuals whose ethnic background is:
A. Asian.
B. Islamic.
C. Hispanic.
D. Native American.
C. Hispanic.
When confidential patient information is to be transmitted by fax, it should be:
A. transmitted in the standard medical private code.
B. seen only by the receiving physician.
C. preceded by a phone call to the recipient.
D. reconsidered and sent by mail.
C. preceded by a phone call to the recipient.
In the United States, a patient's right to communicate effectively in healthcare situations, regardless of language barriers, is guaranteed by:
A. the Constitution.
B. the ASRT Code of Ethics.
C. the American Hospital Association's Patient's Bill of Rights.
D. federal law.
D. federal law.
Which of the following strategies is NOT an appropriate way to deal with an uncooperative toddler?
A. Use praise and rewards for any good behavior.
B. Set limits in clear terms.
C. Insist that a parent enforce cooperation.
D. Immobilize the child as a last resort.
C. Insist that a parent enforce cooperation.