MP322 Master Deck
1/272
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
273 Terms
Approx how many people in UK living with a stoma?
130,000
Where is a colostomy usually created?
left-hand side of the abdomen
Why do stomas require a pouch?
stoma has no end sphincter (muscle) to control defecation so need a bag to collect waste
What is a stoma?
procedure where part of bowel is brought to surface of abdomen to form the stoma
What is a loop colostomy for?
Is it temporary or not
rests on the abdomen with the help of a support rod
generally temporary
gives bowel a temporary rest to aid in healing
When would a loop colostomy occur?
injury, infections where part of bowel is weakened/affected and requires healing
Where is colostomy located?
Where is ileostomy located?
(typically)
left side of abdomen
right side of abdomen
What kind of bag for colostomy and ileostomy?
Why this kind of bag?
colostomy = non-drainable bag (due to stool being more formed)
ileostomy = drainable bag (stool is mainly liquid)
What is a loop colostomy procedure?
bowel is lifted above skin level and held in place with a rod
a cut is made on exposed bowel loop, ends are rolled down and sewed onto the skin - so actually 2 stomas that are jointed together
temporary generally
What is end colostomy procedure?
parts of colon/ rectum has been removed
remaining large bowel brought to abdominal surface to form a stoma
can be temp or permanent
Are colostomy bigger or smaller than ileostomy?
colostomy = bigger
ileostomy = smaller
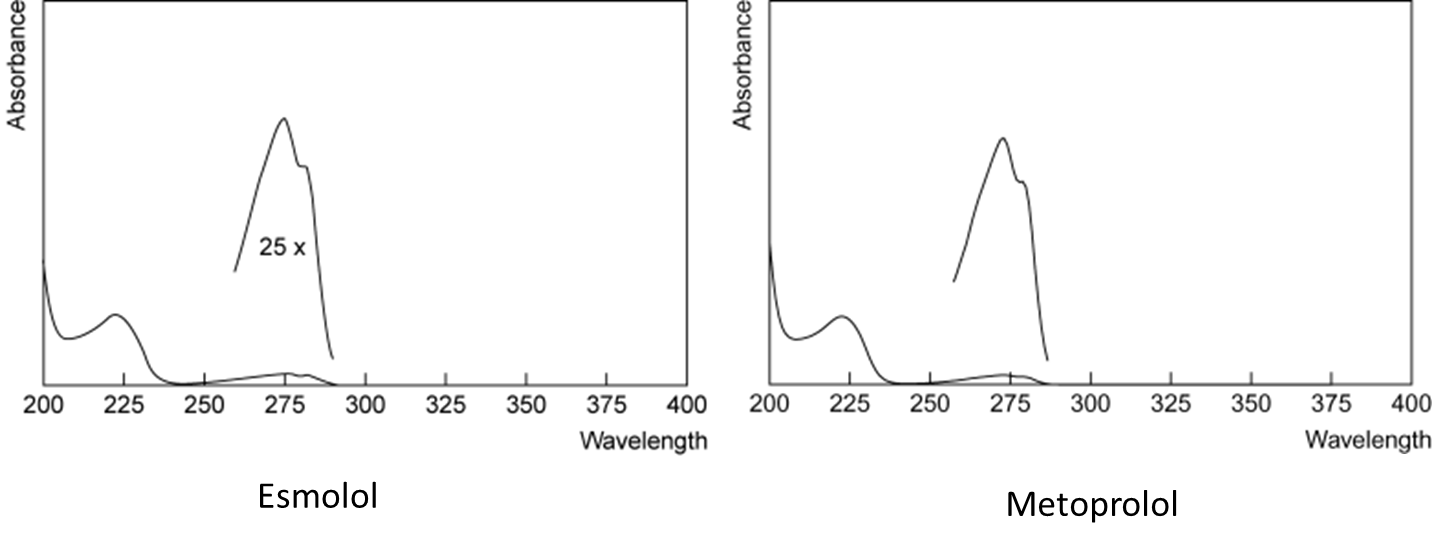
How does electronic spectra work?
basically electron excitation when a light of the correct wavelength interacts with molecule resulting in the molecules reaching a higher energy state (electronic transition)
also results in increase in the energy levels of rotational and vibrational states
What are stages of molecular absorption spectra?
rotational
vibrational
electronic
(increasing in energy as going down list)
What is Beer-Lambert Law?
absorption is relative to concentration (strength of absorption indicate high conc in solution etc.)
What is specific absorbance equation?
A= A(1%, 1cm).b.c
A = absorbance
C is in g/100ml (%w/v)
b is in cm
A(1%, 1cm) is the absorbance of a 1g/100ml solution in 1cm cell at a specific wavelength
When do errors due to light scattering increase?
at shorter wavelengths
What is the downside to UV/ Vis analysis of a molecule?
lacks specificity e.g.
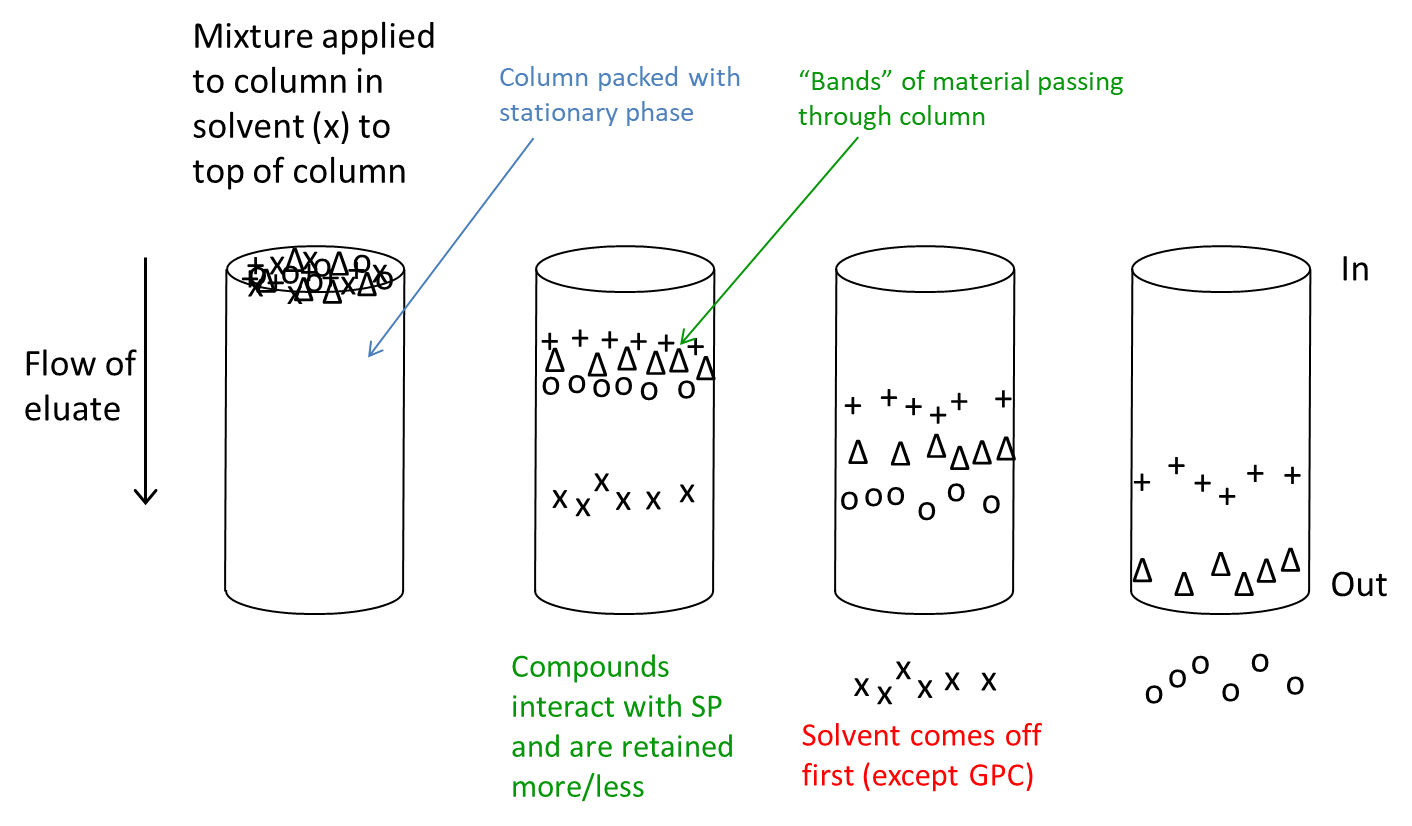
What is planar chromatography?
using a flat stationary phase to separate and identify compounds in a mixture (example would be paper chromatography)
How does column chromatography work?
mixture applied to top of column in solvent
compounds interact with SP and are retained more/less
What does infrared (IR) absorption cause transitions in?
rotational energy levels
vibrational energy levels
(not electronic energy levels)
Does IR or UV/vis light absorption have less energy?
IR has less energy
What must absorption of IR cause a change in?
in the dipole moment of the molecule (how close/far dipoles in a molecule are from each other)
What is polymorphism?
ability of a compound to crystallise in more than one 3d arrangement
What kinds of x-ray diffraction are available?
powder or single crystal x-ray diffraction
single crystal x-ray diffraction is gold standard
What is gold standard pharmaceutical analysis technique?
single crystal x-ray diffraction
What are water soluble vitamins?
B and C (ascorbic acid)
What are fat soluble vitamins?
A D E K
What is vitamin B12 also called?
What is vitamin b9 also called?
cobalamin (think hydroxycobalamin)
folate
What are sources of vitamin B12?
Can humans self produce vitamin B12?
animal origin - meat, fish and dairy products
no only from diet
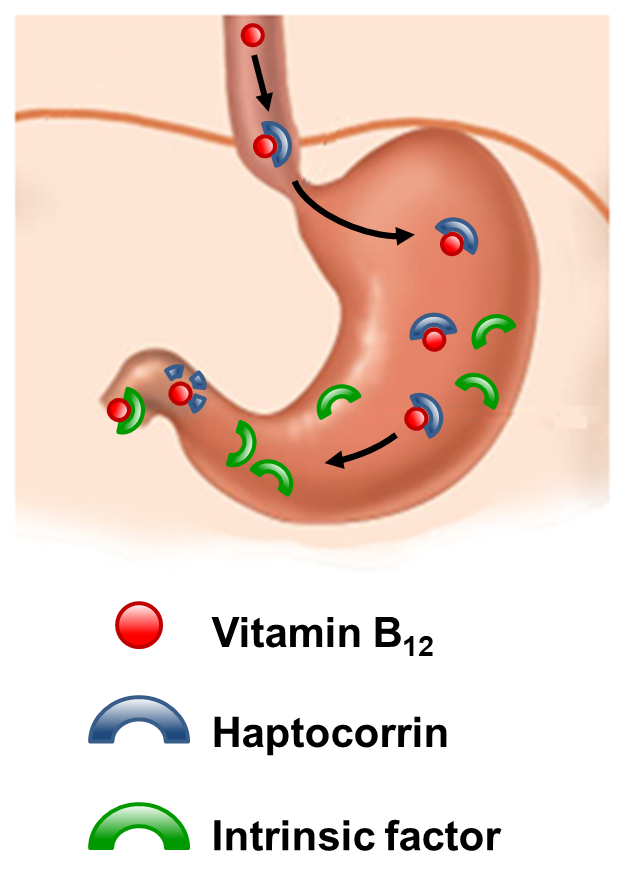
What are the 2 mechanisms of vit B12 absorption and how do they occur?
passive absorption
through buccal, duodenal and ileal mucosa
rapid but inefficient (<1% of an oral dose absorbed)
active transport
occurs through ileum
mediated by gastric intrinsic factor
approx 70% of ingested amount of vit is absorbed
Describe active absorption of vit B12.
vit B12 is released from food and bound to haptocorrin (transcobalamin I)
haptocorrin produced by salivary glands
intrinsic factor (glycoprotein) is secreted by parietal cells
once reached the duodenum, haptocorrin is degraded = releasing B12
vitamin B12 is captured by intrinsic factor
captured complex passes along intestine
in terminal ileum, the complex is endocytosed by cubam
intrinsic factor is degraded releasing B12
ABC transporter releases the B12 into the blood
B12 binds to transcobalamin II
B12 transported in the plasma while bound to transcobalamin I, II, OR III and then taken in by cells
Excess B12 stored in liver
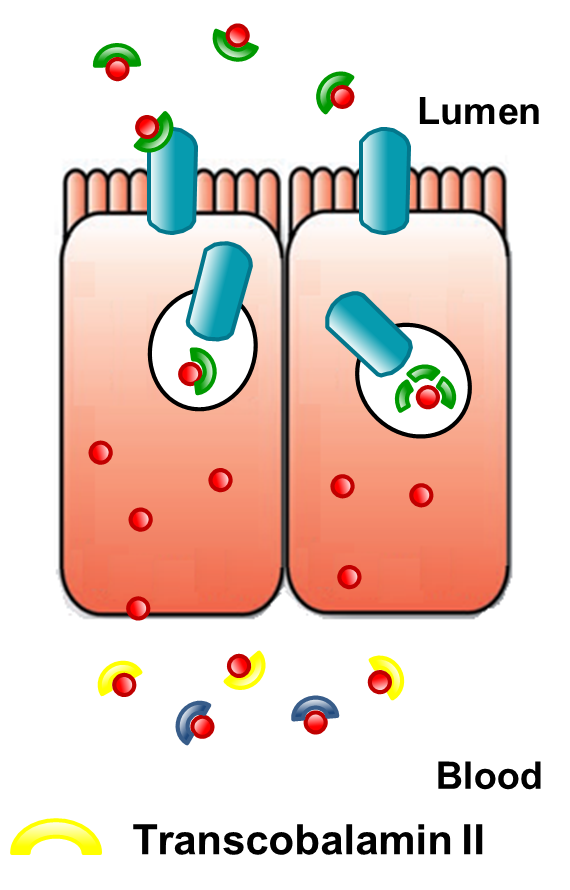
What transcobalamin is most important for cellular uptake of B12?
transcobalamin II
Where is excess B12 stored?
in the liver
What kind of molecule is intrinsic factor?
glycoprotein
What kind of anaemia occurs in B12 deficiency?
What kind of anaemia is it when it is B12 deficiency due to absence of intrinsic factor?
megaloblastic anaemia
pernicious anaemia
What is the cause of true pernicious anaemia?
autoimmune response that leads to destruction of gastric parietal cells (think body attacking itself)
parietal cells are where intrinsic factor is produced → so no intrinsic factor
also results in less/no gastric acid being produced (as also produced in parietal cells)
What is autoimmune atrophic gastritis and what does it cause?
underlying cause of pernicious anaemia
autoimmune response where antibodies attack gastric parietal cells
immunes response directed against H+/K+ATPase
can also be caused by antibodies directed against Intrinsic Factor
What can be causes of B12 deficiency?
loss of gastric parietal cells
loss of intrinsic factor
abnormal intrinsic factor
bacterial overgrowth in the intestine (e.g. stagnant loop syndrome)
disorders of the ileal mucosa (e.g. resection)
disorders of plasma transport proteins (the transcobalamins)
dysfunctional uptake and use of B12 by cells
inadequate dietary intake (rare)
What drugs can induce B12 deficiency?
PPIs and H2 antagonists (less acid → less separation of B12 from food)
oral contraceptives and HRTs
metformin (reduces absorption)
cholchicine (inhibits receptors in terminal ileum)
What are neurological consequences of B12 deficiency?
paresthesia (pins and needles) in hands and feet
sensory loss
gait ataxia (affected walking pattern)
weakness in legs
subacute combined degeneration of the spinal cord (can also affect brain and peripheral nerves)
What are digestive consequences of B12 deficiency?
Hunters Glossitis (geographic tongue)
What are cardiovascular consequences of B12 deficiency?
angina
venous thromboembolic disease
What is a gynaecological consequences of B12 deficiency?
infertility
What is treatment for B12 deficiency?
Is it lifelong?
What condition requires parenteral administration?
oral cyanocobalamin or parenteral hydroxocobalamin
yes, lifelong treatment is necessary
gastric intrinsic factor deficiency (pernicious anaemia)
What are sources of B9 (folic acid)?
dark green veg
dried legumes
fruit/ fruit juices
meat, seafood, poultry and eggs
fortified breads and cereals
What is RDA of B9 per day?
What about in pregnancy?
200mcg/day
in pregnancy 400mcg/day
What is RDA per day for B12?
1-2.5mcg/day
Where is folate mostly absorbed?
in proximal small intestine (duodenum and jejunum)
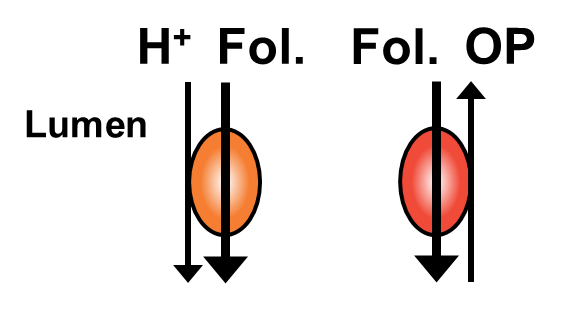
How is folate absorbed from the lumen into the cell?
by a proton-coupled folate transporter (PCFT)
also via a reduced folate carrier (RCF), with folate being exchanged for organic phosphate (OP)
What is the main dietary folate?
5-MTHF
How do enterocytes aid in folate absorption?
located on small intestine surface, have large surface area due to villi
binds to folate and internalises it (into enterocyte cell) by receptor mediated endocytosis
What transporter protein exports folate and reduced from 5-MTHF, from enterocyte?
organic anion transporter (OAT)
How does folate circulate in the blood?
What is plasma conc of folate?
most circulates freely
some bound to albumin
plasma conc = 10-30nmol/L
How is folate uptaken into cells?
same mechanisms as it being uptaken into enterocytes
proton-coupled folate transporter (PCFT), reduced folate carrier (RFC) and folate receptor
What are natural occurring folates found as?
What are synthetic folates made up as?
polyglutamate folates
monoglutamate folates
What does intracellular folate exist as and why?
polyglutamate folate
because is more negatively charged so is less likely to leak out of cell membrane (think phopholipid bilayer)
Why is folate crucial (bio molecularly)?
crucial for the transfer of one-carbon units to amino acids, nucleotides and other biomolecules
What are causes of folate deficiency?
inadequate dietary intake
defects in the uptake system (problem with the transporters)
intestinal disease (e.g. IBD, coeliac)
drug interactions (sulfasalazine, trimethoprim, methotrexate, metformin)
chronic alcohol use
increased cellular requirement (e.g. pregnancy)
What are symptoms of folate deficiency?
sore tongue (glossitis)
GI symptoms (nausea, vomiting, abdominal pain, diarrhoea especially after meals)
neurologic (cogn impairment, dementia and depression
neural tube defects in foetus
What is treatment of folate deficiency?
oral folic acid for 1-4 months
treated until recovery occurs
What is malabsorption?
inadequate absorption of nutrients form the GI tract
Where does most absorption occur?
through the small intestine walls
What is the difference between mucosal and pre-mucosal malabsorption?
mucosal = relating directly to small intestine wall (something wrong with the adsorptive surface of the wall)
pre-mucosal = before reaching small intestine and is because the nutrients arent available for adsorption (e.g. because food source hasnt been broken down enough)
What are conditions that cause mucosal malabsorption?
crohns, coeliac and certain kinds of surgery
What are conditions that cause pre-mucosal malabsorption?
pancreatitis
cystic fibrosis
lactase deficiency
What is Crohn’s disease’ effect on absorption?
Is Crohn’s mucosal or pre-mucosal malabsorption?
abnormal epithelium → deficient absorption
mucosal (problem with small intestine itself)
Why does surgical resection effect absorption?
Is this mucosal or pre-mucosal?
shortens bowel = less surface area for absorption
is mucosal (small intestine itself)
Why do cystic fibrosis, pancreatitis and lactase deficiency effect absorption?
Is this mucosal or pre-mucosal malabsorption?
because there are insufficient quantity of digestive agents →macronutrients cant get broken down so cant get absorbed
pre-mucosal (as not to do with small intestine directly, but before it)
What are typical deficiencies associated with Crohns?
iron deficiency anaemia
B12/ folate deficiency
Vit D and calcium deficiency
What is a drawback to treating crohns/ IBD with steroids?
steroids over long-term can cause negative effect on bones causing bone loss
What is villous atrophy?
What condition does this result in?
villi become inflamed and flattened → worst case can disappear completely
body cant absorb nutrients properly
coeliac
What is coeliac disease?
gluten causes abnormal mucosal response = chronic inflammation, damage to small intestine and villous atrophy
What are symptoms of coeliac disease?
How is coeliac diagnosed?
fatigue, gastric upset, weight loss
via serological testing
What deficiencies/conditions can occur in patients with coeliac?
anaemia, osteoporosis (due to vit D and calcium deficiency)
Is short bowel syndrome mucosal or pre-mucosal malabsorption?
Why do certain drugs need to be delivered in higher doses to patients with short bowel syndrome?
mucosal due to lest surface are available for absorption
if drug is mainly absorbed in small intestine, require higher dose as these patients have smaller surface area so less absorption takes place, why they need a higher dose
What sex is more affected by pancreatitis?
What does pancreatitis lead to?
men (any age)
deficiency in pancreatic enzymes
What is chronic pancreatitis?
What is it associated with pancreatitis?
chronic inflammation of pancreas leading to impaired function of the organ (pre-mucosal malabsorption)
long term excess alcohol consumption
What is steatorrhea and what condiditon is associated with it?
presence of excess fat in faeces (cystic fibrosis)
What is cystic fibrosis?
What can cystic fibrosis lead to?
genetic condition where decreased Cl secretion, increased Na absorption = thick mucus in pancreas mainly → inhibits absorption
osteoporosis, malnutrition, weight loss, intestinal obstruction
treat with pancreatic enzyme supplements (Creon capsules), fat soluble vit replacement and calorie replacement
What is small intestine bacterial overgrowth (SIBO)?
What does SIBO result in?
when after an incident, passage of food and waste products in GI tract slows, creating a breeding ground for bacteria
diarrhoea, weight loss and malnutrition
Is fat malabsorption pre-mucosal or mucosal?
In what conditions is fat malabsorption common?
What deficiencies does fat malabsorption result in?
pre-mucosal as problem with digestion
in Crohn’s and Coeliac
deficiencies in fat-soluble vitamins (A,D, E, K as cant be absorbed without dissolving (i think?))
What does vitamin D deficiency result in?
What does vitamin K deficiency result in?
rickets, osteoporosis
clotting problems
What is treatment options for malabsorption of protein, fat and carbohydrates (when pancreatitis or cystic fibrosis)?
What is problem with pancreatic enzyme replacement therapy?
supplementation of pancreatic enzymes (lipase, amylase and protease)
Creon
derived from pork, so muzzys and veggies need to reconsider some stuff blah blah blah
Specific signs and symptoms linked to malabsorption conditions (list them)
Nutrients | Main signs/symptoms of malabsorption |
Fat | Steatorrhoea |
Protein | Muscle wasting, malnutrition, oedema |
Carbohydrate | Bloating, flatulence, diarrhoea |
Vitamin D +/- calcium | Bone problems – osteoporosis, fractures |
Vitamin E | Neurological problems |
Vitamin K | Coagulation (bleeding) problems |
Vitamin A | Night blindness |
What does MCR stand for?
medicines care and review service
What were the main drivers for MCR being introduced?
prescribing, dispensing errors
compliance/concordance of patients (not adhering to meds)
workload
What kind of patient conditions can be aided with MCR?
registered with a Scottish GP permanently
at least one long term condition that requires medication
new medications
high risk medication e.g. warfarin, methotrexate, lithium
smoking cessation
gluten free foods
What patients are eligible for MCR?
at least one long term condition
permanently registered with Scottish GP
What sorts of drugs are excluded from MCR?
drugs subject to dose titrations
CD 2-4 and cytotoxic drugs (eg methotrexate)
drugs that require close monitoring (may not be suitable)
patients subject to frequent medication changes
How does kaolin work as a treatment for acute diarrhoea?
acts as an adsorbent and is bulk forming
What are examples of anti-motility drugs used to treat acute diarrhoea?
diphenoxylate and atropine (called co-phenotrope)
codeine
morphine (with kaolin)
loperamide
racecadotril
How do codeine and morphine act as antimotility drugs?
act on mu opioid receptors as agonists, causes decrease in ACh release → less peristaltic activity → slows transit time through gut
Which receptors does ACh bind to?
nicotinic and muscarinic acetylcholine receptors
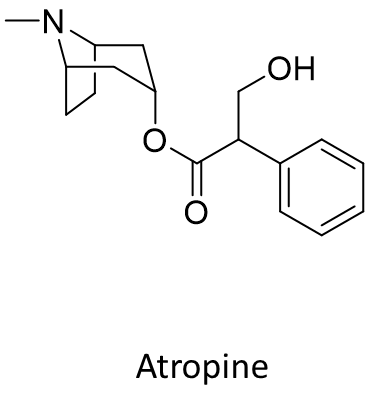
What is co-phenotrope composed of?
How does co-phenotrope act as an antimotility drug?
diphenoxylate and atropine
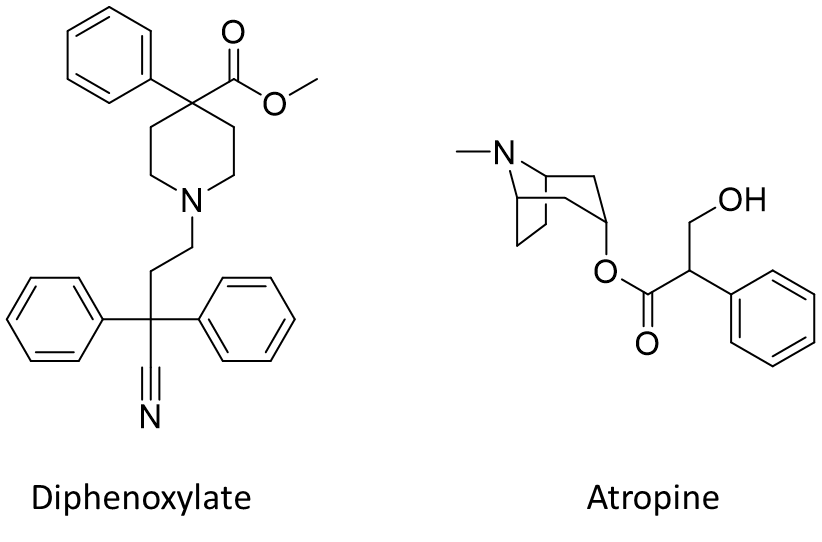
atropine acts as an inverse agonists on muscarinic receptors (baseline activity of receptor lowered)
diphenoxylate acts similarly to codeine by binding to mu opioid receptors as an agonist → decrease in ACh release → decrease in peristaltic activity
How does atropine affect muscarinic acetylcholine receptors?
is an inverse agonist on the receptor (lowers baseline activity)
Where is racecadotril molecule cleaved to become thiorphan (prodrug→active drug)?
cleaved between the ester bond (ester hydrolysis via esterases)
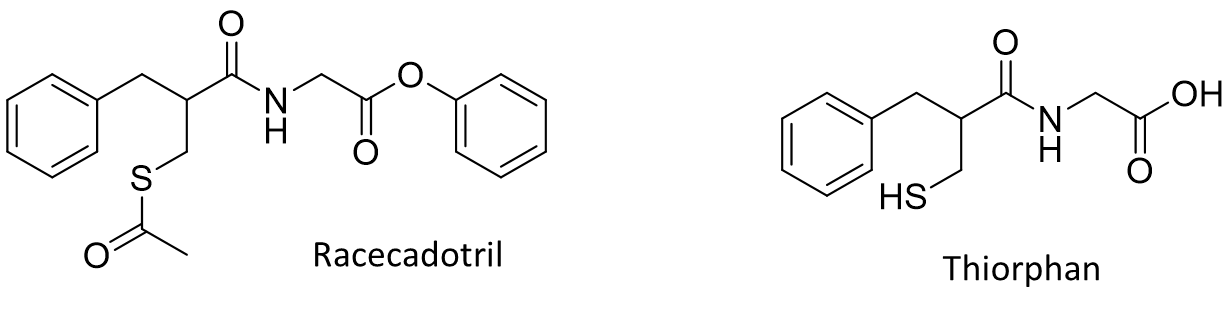
Why is raceacadotril/thiorphan not formulated as a salt?
due to there being no ionisable groups (is an overall neutral molecule)
What salt is loperamide made into?
loperamide hydrochloride
What salt is diphenoxylate made into?
What salt is atropine made into?
diphenoxylate hydrochloride
atropine sulphate
What salt is codeine made into?
codeine phosphate