Surgical disease of the urethra
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
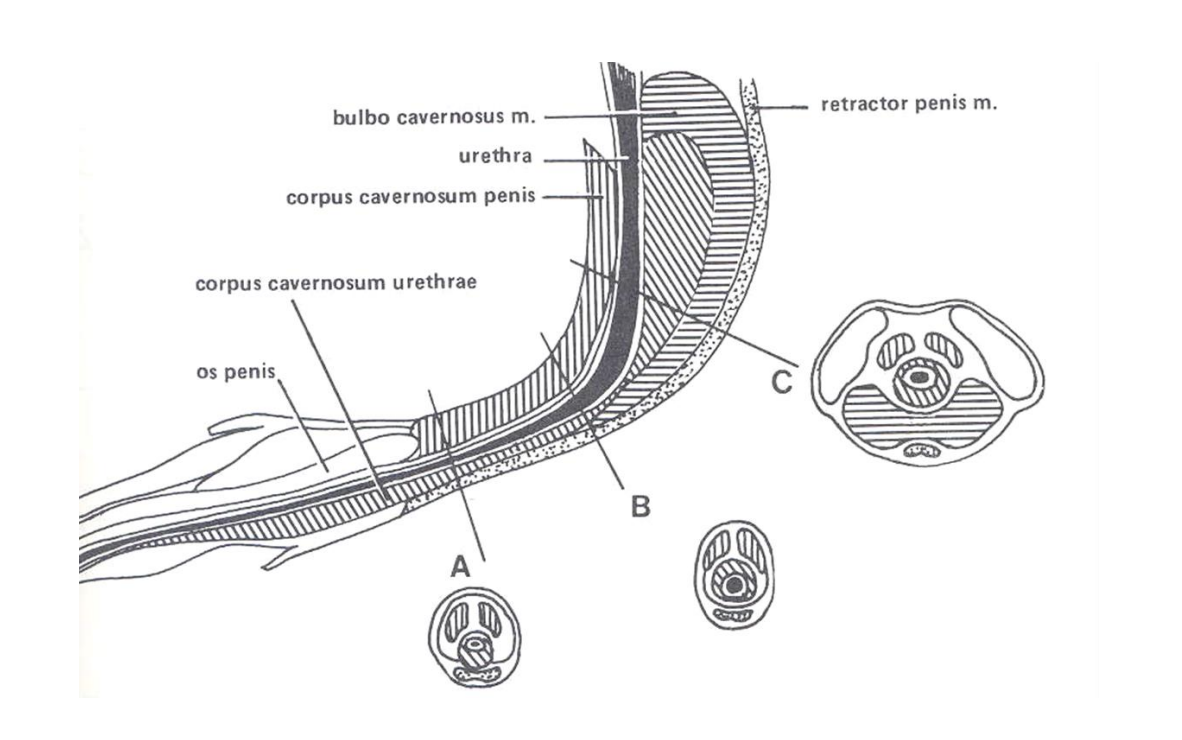
Describe the anatomical portions of the urethra in males
Prostatic
At neck of bladder
Surrounded by prostate
Pelvic (membranous)
From prostate to ischial arch
Vulnerable to injury by pelvic fractures
Penile (cavernous)
Canine urethra occupies groove in os penis
Limited distension, prone to obstruction
(Most urethral disease occurs in males —> reflection of narrow diameter and long length)
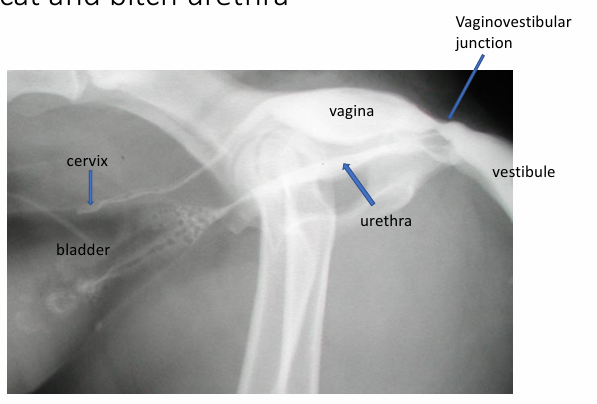
Describe the anatomy of the urethra in females
Urethra enters vestibule 2-5mm caudal to the vaginovestibular junction
Dorsal urethral wall is in close association with the ventral wall of the vagina
Urethra is relatively straight and short compared to male urethra
Urethra is wider and mucosa is folded, allows distension compared to male urethra
How does cats urethra differ in cats compared to dogs?
Cats have long abdominal portion
Two bends- one at caudal border of ischium and the other---
Obstruction is common

List the congenital urethral abnormalities
Hypospadias, epispadias: uncommon
Incomplete formation of urethra, cleft scrotum, incomplete formation of prepuce, hypoplastic penis
Urothrorectal fistula:
Development abnormality of foetal cloaca, communication between urethra and rectum persists
Urine is passed from anus and vulva/penis, recurrent UTIs
How are hypospadias, epispadias treated?
Resection of hypoplastic penis if becoming self traumatised or dessicated
How is urethrorectal fistula treated?
Resection of fistula
List some of the common acquired urethral lesions
Urethritis
Urethral prolapse
Urethral obstruction
Neoplasia
Stricture
What is urethritis usually associated with? What are the predisposing factors?
Other inflammatory disorders of the urogenital tract: Cystitis, prostatitis, vaginitis
Trauma from urethral calculi or iatrogenic (catheterisation), or neoplasia predisposes
What can urethritis lead to?
Stricture formation
Urethral prolapse
What are the clinical signs of urethritis and how is it treated?
Clinical signs associated with underlying disease
Treat underlying cause
What is the pathogenesis of urethral prolapse?
urethral infection, sexual excitement
brachycephalic breeds predisposed
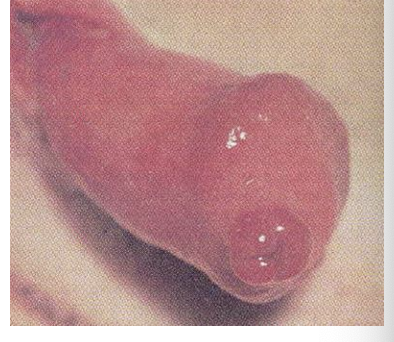
What are the clinical signs of urethral prolapse?
Excessive licking penis/prepuce
Protruding urethral mucosa (pink/red mass at tip of penis)
Profuse intermittent bleeding from traumatised prolapsed urethral mucosa
How is urethral prolapse treated?
Reduce prolapse and place purse string suture around tip of penis
Resection of prolapsed tissue and suture penile mucosa to urethra (simple interrupted)
Castration is recommended
Why is urethral obstruction so urgent?
Failure to eliminate urea and potassium
Hyperkalaemia can cause cardiac arrhythmias
Can cause permanent renal damage
Very painful
Overstretches bladder: risk of atony or rupture
(partial or complete)
What are the causes of urethral obstruction?
Urethral calculi (more common in males – why?)
Urethral plugs (cats)
Prostatic disease (dogs)
Displacement of the bladder through hernia or body wall rupture
Urethral neoplasia (bitches)
Bladder neck neoplasia
Secondary to urethral stricture (more common in male cats and dogs)
Fracture of the os penis associated with trauma, bite wounds, etc (male dogs)
Blood clots (haematuria is more common than passing blood clots)
Granulomatous urethritis (bitches: rare)
What are the clinical signs of urethral obstruction?
Repeatedly straining to urinate
Dysuria
Anuria
Haematuria
Excessive licking of prepuce/penis (especially male cats)
Dripping urine
Inappetence, lethargy, vomiting
Abdominal distension/pain
Collapse
How is urethral obstruction diagnosed?
History
Clinical findings
Large firm bladder upon abdominal palpation, inability to pass urinary catheter in male dog
Serum biochem: assess urea, creatinine, potassium
Radiography- pull hindlimbs back because fabellae can look like urethral calculi
Positive contrast urethrography (displaced bladder, radiolucent calculi, soft tissue lesions)
Ultrasound
How is urethral obstruction managed?
Immediate priorities
Empty bladder: by cystocentesis or catheterisation
Start IVFT
Check electrolyte status and treat hyperkalaemia if present
Provide pain relief
Then investigate cause of urethral obstruction
How would you manage urethral obstruction due to urethral calculi?
Empty bladder by cystocentesis
Fluid therapy (correct acid/base and electrolyte disturbances)
Attempt catheterisation- pass catheter to obstruction and flush with saline
Check bladder size whilst flushing and empty bladder by cystocentesis
Once obstruction is relieved pass catheter to bladder and empty
Perform retrograde urethrogram to confirm urethral patency
Retrieve calculi by cystotomy
When is a urethrotomy in male dogs indicated?
Firmly lodged urethral calculi at base of os penis that can't be flushed to bladder
How would a urethrotomy be performed?
Pass catheter to site
Make ventral longitudinal midline skin incision (caudal to os penis)
Reflect retractor penis muscle
Make longitudinal incision through urethra over calculus
Remove calculus
Advance catheter
Suture urethra (simple interrupted or continuous)
Remove catheter
What are the potential complications of a urethrotomy?
Haemorrhage from urethra
Can be profuse (2-7d post-op), exacerbated by urination and self trauma so must wear collar
Urine passing into subcut tissues complicated wound healing causing local cellulitis and skin slough
Stricture formation (post-op) with recurrent urethral obstruction+
*Retrograde flushing is preffered option
What is a urethrostomy? When is it indicated?
Creation of a permanent urethral opening
Indications
Failure to retrograde flush urethral calculi to bladder
Recurrent urolithiasis with repeat urethral obstruction despite medical management
Urethral stricture
Severe penile trauma
What are the potential sites for urethrostomy?
Scrotal (only male dogs)
Preferred site if dog is/can be castrated
Urethra wide and superficial
Less cavernous tissue surrounding urethra so less intra and post op haemorrhage
Pre-scrotal (only male dogs)
Perineal (only in cats)
Prepubic (rarely performed, salvage of intrapelvic urethral rupture in cats and dogs)
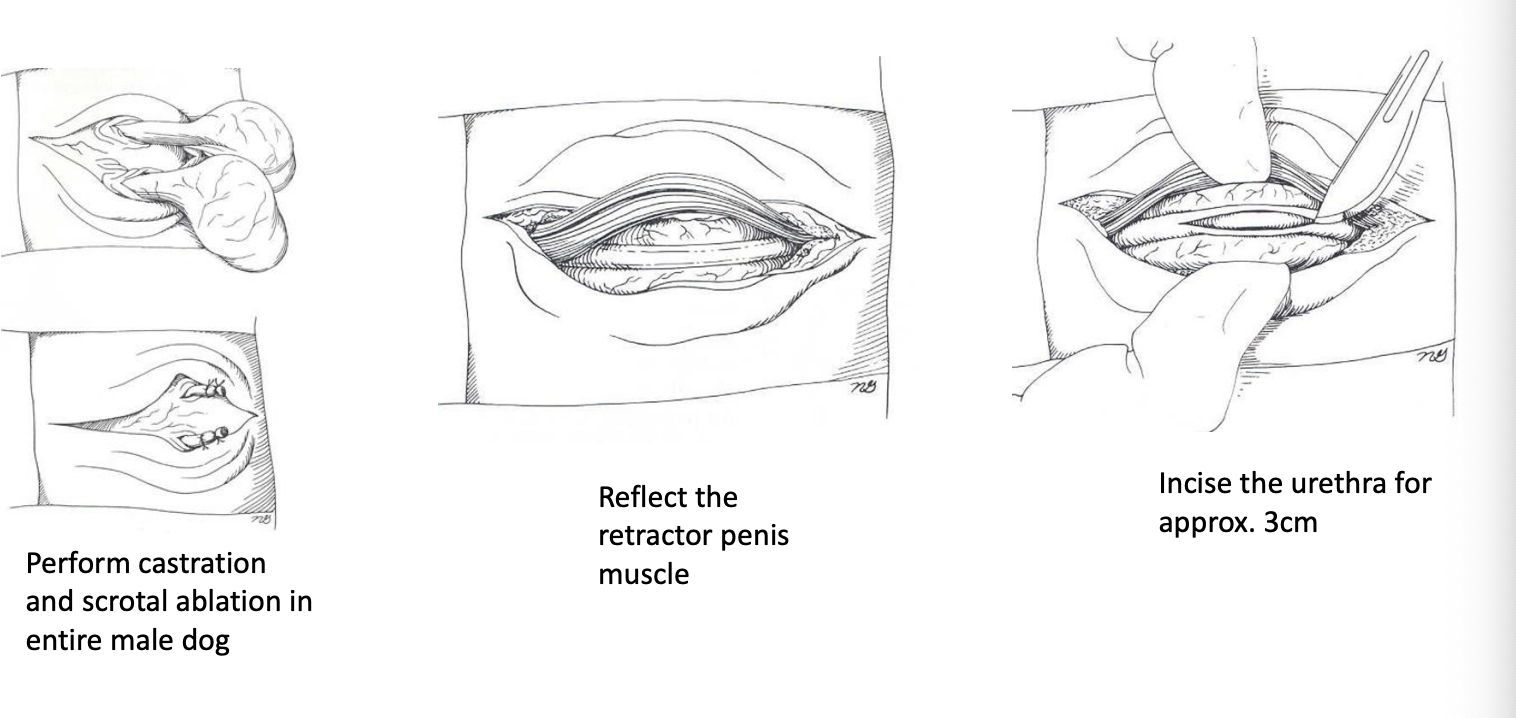
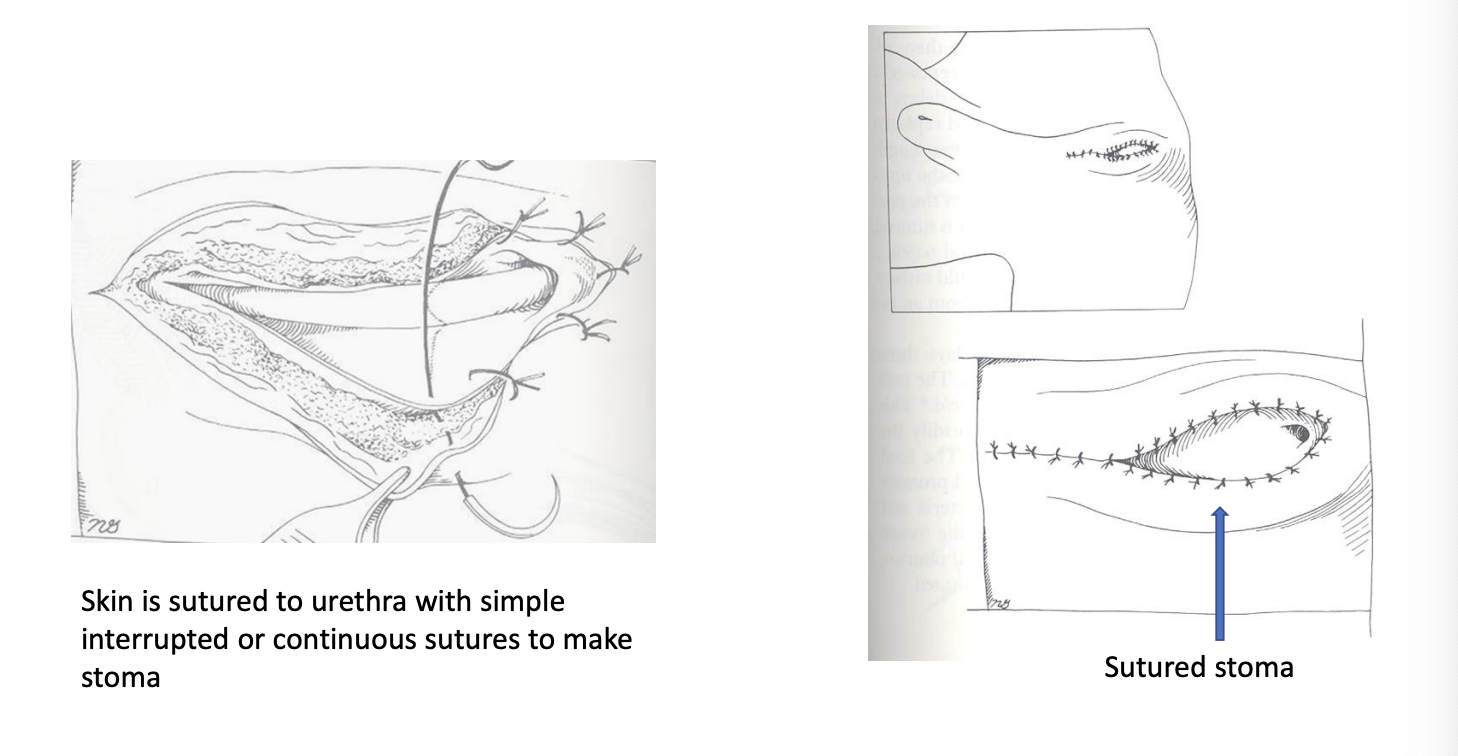
How is scrotal urethrostomy performed in dogs?
If dog not castrated, perform castration and scrotal ablation
Midline incision (if castrated midline scrotum)
Reflect retractor penis
Suture urethra to skin
Close skin and subcut tissues cranial and caudal to stoma as necessary
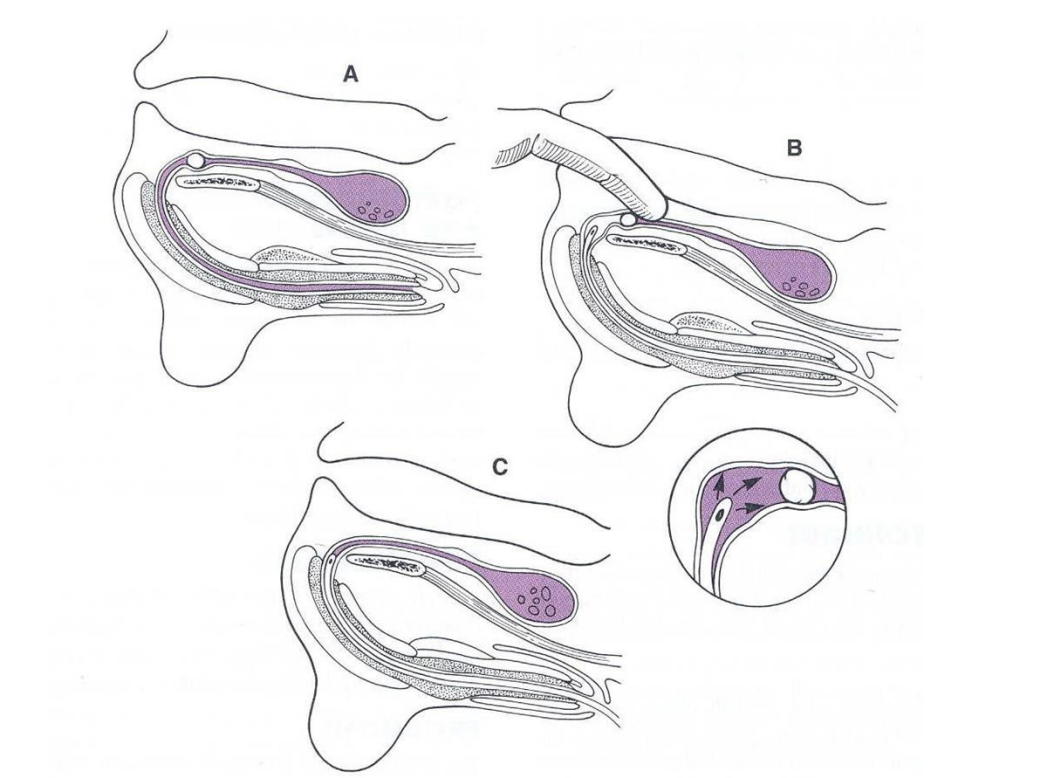
How must urethral catheterisation be performed in cats?
Grab very base of prepuce to keep penis exteriorised
Pull caudally and lift dorsally to draw urethral bends into straight line
What is perineal urethrostomy indicated for?
Failure to relieve urethral obstruction by retrograde flushing
Recurrent/chronic urethral obstruction
Penile urethral stricture
Severe penile urethral trauma
What are the possible complications of feline perineal urethrostomy?
Wound breakdown/cellulitis
Stricture formation
Recurrent UTI
Perineal hernia
What are the causes of urethral trauma?
Abdominal trauma
Pelvic fracture (laceration of intrapelvic urethra by fracture fragments)
Iatrogenic during catheterisation
What are the clinical signs of urethral trauma?
Haematuria, dysuria, anuria
Pain
Abdominal distension
Inappetence, lethargy, vomiting
Collapse
Discolouration of skin/cellulitis of perineum, thighs, caudal abdomen
How is urethral injury diagnosed?
History
Radiography
Plain
Retrograde urethrogram
Serum biochemistry (elevated urea, creatinine, potassium)
How is urethral injury treated?
Establish urethral patency if possible by gentle catheterisation
Stabilise patient before treatment
Conservative treatment: : leave indwelling urethral catheter for 3-10 days if minor trauma
Refer for surgery if extensive trauma
How is prepubic urethrostomy performed?
Salvage procedure for intrapelvic urethral injury
A new urethral opening is created on ventro-caudal abdomen
Performed when insufficient urethral length to perform urethrostomy at other sites