Chapter 5 Membrane Dynamics単語カード | Quizlet
1/95
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
96 Terms
intracellular fluid
2/3 of body fluid
fluid within cells
extracellular fluid
1/3 of body fluid
fluid outside the cell
permeable membrane
a membrane that allows for diffusion of certain solutes and water
freely moving
Semi-permeable membrane
membrane that is selective on what it allows through
ECF:
a lot of Na+, Cl-, Ca+ and very little K+
ICF:
a lot of K+, very little Na+, very little Cl-, very little Ca+
What ions are found in the concentration of ECF and ICF?
osmotic equilibrium
fluid concentrations on both sides of the cell membrane are equal
osmosis
the movement of water across a membrane in response to solute concentration gradient
water moves to dilute more concentrated solution
moves from from high water concentration to low water concentration
meaning ---
water moves from low solute to high solute
once conc. are equal, net movement of water stops
diffusion is constant
net movement/diffusion will stop after concentration equilibrium
Which stops and which continues?
net movement/diffusion or diffusion
osmotic pressure
pressure that must be applied to oppose osmosis
water is constantly moving between cells so the free movement of water between two creates the eq.
Why do the ECF and ICF reach state of osmotic equilibrium?
chemical disequilibrium
the imbalance of chemicals that creates a concentration gradient
electrical disequilibrium
imbalance of charges/ions that can create a membrane potential and an electrical gradient
age: water content decrease as you age
gender: men have a higher % body water than women
% lean body mass: the more lean body mass you have, the more water you have in your body
How does age, gender, and % lean body mass impact body water content?
NO - dynamic steady state
Is homeostasis at equilibrium?
no
Does concentration = volume?
molarity
M = moles/Liter
the number of moles of solute per liter of solution
Osmolarity
molarity (mol/L) X particles/molecule (osmol/mol) = osmol/L
total of particles of solute per volume
290 +/- 50 mOsM (300 mOsM)
What is the normal range of osmolarity in the human body?
compares concentrations in different solutions
# of solute particles dissolved in a volume of solution
looks at both PENETRATING AND NON-PENETRATING SOLUTES
What does osmolarity compare?
Solution A is HYPERosmotic to solution B.
Solution B is HYPOosmotic to solution A.
If solution A has a higher osmolarity (has more solute particles per unit volume, more concentrated) than solution B, what is solution A to solution B? What is solution B to solution A?
compares a solution and a cell by describing the solution
looks at the consequence of concentrations of soltions
looks at ONLY NON-PENETRATING SOLUTES
What does tonicity compare?
Solution A has a lower solute concentration than Solution B
HYPOosmotic means
Solution A has more solute concentration than Solution B
HYPERosmotic means
two solutions contain the same number of solute particles per unit volume
ISOosmotic means
tonicity
Which tells you what happens to a cell when placed into a solution?
tonicity or osmolarity?
hypotonic
NP<300 mOsM
means that the solution is hypotonic to the cell - there is a low concentration of solutes in the solution than inside of cell
cell swells/lyse - gains water
hypertonic
NP>300 mOsM
means that the solution is hypertonic to the cell - there is more concentration of solutes in the solution than inside of cell
cell shrinks/crenate - loses water
1. if the CELL has a HIGHER conc. of NONpenetrating solutes than the solution, there will be net movement of water INTO the cell. The cell swells and the solution is hypotonic.
2. if the cell has a LOWER conc. of nonpenetrating solutes that the solution, there will be net movement of water OUT of the cell. The cell shrinks and the solution is hypertonic.
3. if the conc. of nonpenetrating solutes are the same in the cell and solution, there will be no net movement of water at equilibrium. The solution is isotonic to the cell.
What are the rules for predicting tonicity?
NaCl
if a cell is placed in a solution of NaCl, the Na+ and Cl- ions do not enter the cell.
What is the most important nonpenetrating solute in physio?
bulk flow
most general form of biological transport = (gas or liquid) within a compartment
a pressure gradient causes fluid to flow from regions of high pressure to low pressure.
ex. blood moving through the circ. system.
heart acts as pump that creates region of high P, pushing plasma with its dissolved solutes and suspended blood cells through the blood vessels.
ex. air flow in the lungs
the lipid and protein composition.
permeability is variable and can sometimes be changed by altering the proteins or lipids of the membrane
What determines which molecules will enter and exit the cell?
size of molecule and its lipid solubility
What are 2 factors of molecules that influence its movement across cell membranes?
dissolve easily in a solution
When something is soluble, that means it can do what?
very small molecules and those that are lipid soluble
What types of molecules can cross directly through the phospholipid bilayer?
through vesicles
How do very large lipophobic molecules enter/exit the cells?
movement that doesn't require the input of energy other than the potential energy stored in the concentration gradient
What is passive transport?
movement that requires the input of energy from outside source (ATP)
What is active transport?
- simple diffusion (conc. gradient)
protein mediated:
- facilitated diffusion (conc. gradient)
- ion channel (electrochemical gradient)
- aquaporin channel (osmosis)
What are types of passive transport?
Vesicular transport (ATP)
- exocytosis
- endocytosis
- phagocytosis
Protein-mediated:
- direct or primary active transport (ATPases)
- indirect or secondary active transport (conc. gradient created by ATP)
What are the types of active transport?
- passive transport
- move from high to low conc.
- net movement occurs UNTIL conc. are equal
- rapid over short distance and slow over long dist
- directly related to temp (high temp= fast rate)
- rate is inversely related to molecular weight and size. The bigger the weight/size, the slower the rate
- can take place in an open system or across a partition that separates two compartments
What are some characterisitics of diffusion?
along higher conc. gradients
over shorter distances
at higher Temps
for smaller molecules
When is diffusion faster?
flux
a state of continual change or movement
diffusion rate/unit of membrane surface area
net flux
compares the movement between 2 compartments (movement in both directions)
diffusion equilibrium
movement occurred - equally
so the next flux is 0
yes
When net flux is 0, is there still movement?
- lipid solubility
- molecular size
- concen. gradient
- membrane surface area
- composition of lipid layer
What are some factors affecting the rate of diffusion through a cell membrane?
permeability constant
the permeability of a molecule when given temperature and a particular membrane
flux will increase if either of these increase
because it is too large of a distance.
instead we count on specialized systems for access and long distance transport
Why can't humans rely on simple diffusion from outside the body to cells?
because they can more easily move through the non polar membrane.
O2,CO2, fatty acids, steroids move through well
water is small enough to move through
Why do nonpolar molecules have a higher P through a lipid bilayer than polar molecules?
osmosis - movement of water across membrane
diffusion - movement of water and solutes across a membrane
Compare and contrast osmosis and diffusion.
channel proteins
carrier proteins
What are two types of transport proteins?
channel proteins
create water-filled passageways that directly link the ICF and ECF
allow more rapid transport across the membrane but generally are limited to moving small ions and water
carrier proteins
aka transporters
bind to the substrates that they carry but never form a direct connection between ICF and ECF
slower, but move larger molecules than a channel protein
aquaporin
a water channel that allows water to move in large amounts across a membrane
ion channel
a channel that allows for atoms with a charge (ions) to move across a membrane
Open channels (leak channels)
gated channels that spend most of their time open, allowing ions to move back and forth without regulation
gated channels
gated channels that spend most of their time closed which regulates ions moving through them
- ligand gated: chemical substrate
- voltage: charged ions
- mechanically gated: physical force
uniport carrier
a carrier protein that move only one kind of molecule
cotransport
a carrier protein that moves more than one kind of molecule at one time
symport carrier
a carrier protein that moves molecules in the same direction (in or out of the cell)
antiport carrier
a carrier protein that moves molecules in both directions (in or out of cell)
1. chemical specifity
2. conformation change
3. limited rate of transport
- solute conc. and affinity
- # transporters
- rate of conformational change
- competitors
The binding site of a carrier protein has:
facilitated diffusion
diffusion w/ protein carrier (i.e. sugars, amino acids)
like GLUT transporters, move glucose and related hexose sugars across membranes (usually never reaches equilibrium, almost always have a gradient coming into the cell)
reversible transport depending on concentration gradient.
uses ATP
moves against conc. gradient
moves from low to high conc.
active transport
primary/direct active transport
the energy to push molecules against its conc. gradient comes directly from ATP
secondary/indirect active transport
uses PE stored in the conc. gradient of one molecule to push other molecules against their conc. gradient.
it ultimately depends on primary active transport, because the conc. gradients that drive secondary are created using ATP
because primary active transport uses ATP as the energy source.
ATPases (aka pumps) hydrolyze (breaks down) ATP to ADP and Pi harnessing energy.
Primary active transporters are also known as ATPases, why?
- pumps 3 Na+ (in higher conc. in ECF) out of the cell
- pumps 2 K+ into the cell
Na+/K+ ATPase pump
how much of each is pumped in and out of cell?
Na+: low in cell, high out of cell
K+: high in cell, low out of cell
Na+ conc. is high and low where?
K+ conc. is high and low where?
1. 3 Na+ from ICF bind to high affinity sites
2. ATPase is phosphorylated with Pi from ATP, protein changes conformation
3. Na binding site loses their affinity for Na and releases the 3 Na+ into ECF; high affinity binding sites for K+ appear
4. 2 K+ from ECF bind to high affinity sites; protein changes conformation and Pi is released
5. K binding sites lose their affinity for K and release 2 K into ICF; high affinity binding sites for Na appear.
Mechanism of the Na/K pump
Na+ has leaky channels and follows its concentration and electrical gradient into the cell.
K+ channels open and it follows its concentration gradient out of the cell but is going against its electrical gradient.
Then the Na+/K+ ATPase will restore them back to the correct place and move them both against their concentration gradients.
Be able to explain the action of the Na+/K+ ATPase pump.
How does this pump help to maintain the electrochemical gradient and the membrane potential of a cell?
carrier protein specificity
the ability of the transporter to move only one molecule or only a group of closely related molecules
binding sites have 3D properties
12 known GLUT transporters (GLUT 1- GLUT 12)
each specific GLUT has a higher affinity for a specific monosaccharide hexose sugar.
carrier protein competition and competitive inhibition
similar solutes may be transported by the same protein thus creating competition
GLUT: glucose and other hexose sugars: fructose, galactose, mannose
GLUT: may bind but not transport disaccharides (like maltose) (competitive inhibition) even at the same conc. of fructose and GLUT, if you add maltose you will have inhibition.
carrier protein saturation
transport maximum
# of transporters are saturated with solute
concentration is high
increase solute concentration and expect an increase in amount being moved until you have reached the transport max, plateaus.
Vesicular transport
type of active
transport of macromolecules that are too large to enter or leave through protein channels or carriers.
two types for import into cell:
endocytosis and phagocytosis
out of cell: exocytosis
across cell: transcytosis
Phagocytosis
actin-mediated process by which a cell engulfs a bacterium or other particle into a large membrane bound vesicle called a phagosome.
the phagosome pinches off from the cell membrane and moves to the interior of the cell, where it fuses with a lysosome whose digestive enzymes destroy the bacterium .
requires energy from ATP for the movement of cytoskeleton and for the intracellular transport of the vesicles.
a ligand binds to a membrane receptor protein to activate the process
occurs in regions of the cell memb. called coated pits, indentions where the cytoplasmic side of the memb. has high conc. of protein. (clathrin)
Where does receptor mediated endocytosis occur and what is it?
Epithelial transport
movement between compartments
movement into and out of body must cross layer of epith cells that are connected to one another by adhesive and tight junctions
apical membrane
Which membrane faces the lumen?
basolateral membrane
Which membrane faces the ECF?
absorption
transport of material from the lumen of an organ into the ECF
GI tract absorbs digested nutrient
also respiratory system
secretion
when materials moves from ECF to the lumen
ex: salivary glands secrete saliva to help moisten food
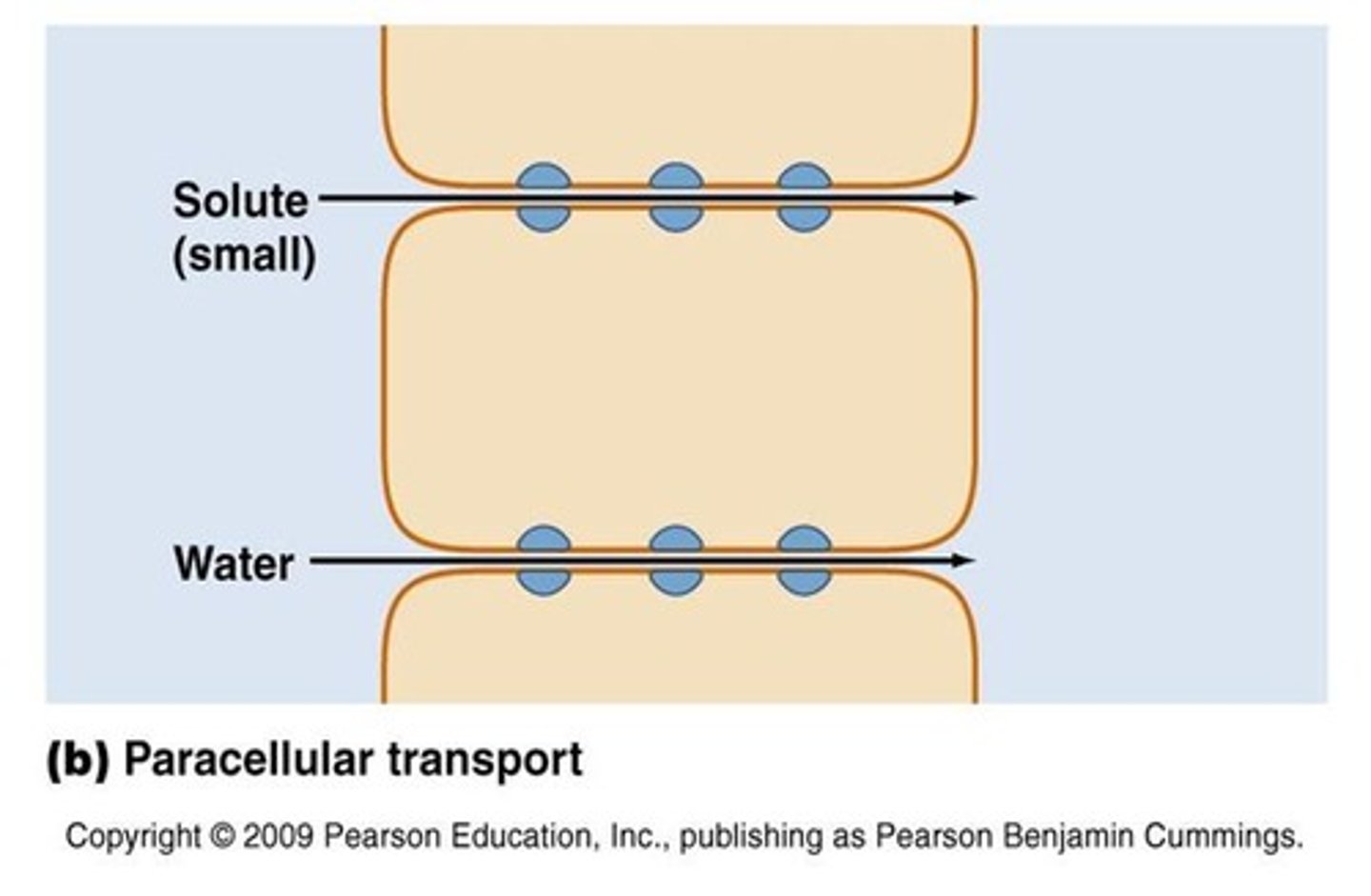
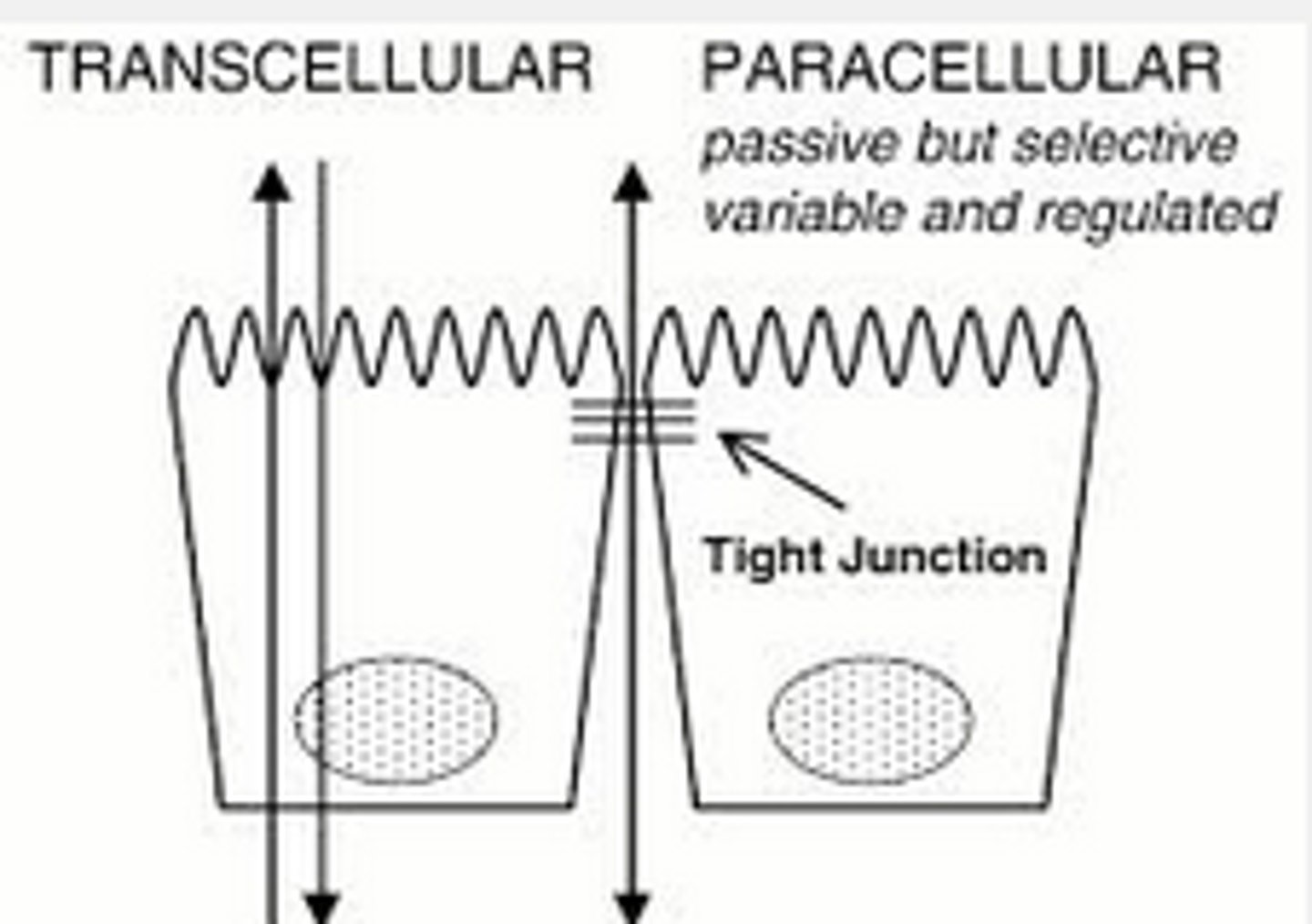
Paracellular transport
movement takes place through the junctions between adjacent cells
not happening much in tight junctions
transcellular transport
movement through epithelial cells
must move across 2 membranes
uses both active and passive transport
ion conc. gradients between the ICF and ECF
the selectively permeable cell membrane
What creates the membrane potential?
2. we insert a leak channel for K+ into the membrane, making the cell freely permeable to K+, so K+ starts to move out of the cell down its conc. gradient so then there is electrical disequilibrium, the ECF has a net + charge and the ICF has a net - charge.
As add'l K ions leave the cell, going down their conc. gradient, the inside of the cell becomes more negative and the outside becomes more +.
1. When we begin the cell has no membrane potential: The ECF and ICF are electrically neutral
resting membrane potential
-70mV
K+ follows its gradient (electrical gradient)
how much K+ will diffuse?
- balance between the [K+] gradient and the electrical gradient.
normally along a conc. gradient it would all diffuse until equ. but because like charges repel and diff charges attract, this will reach a diff kind of balance.
What happens when a K+ leak channel is added?
equilibrium potential
for any given conc. gradient of a single ion, the membrane potential that exactly opposes the concentration gradient
example: when the conc. gradient is 150 mM K+ inside, and 5 mM K+ outside the cell, the equilibrium potential for potassium is Ek = -90 mV.
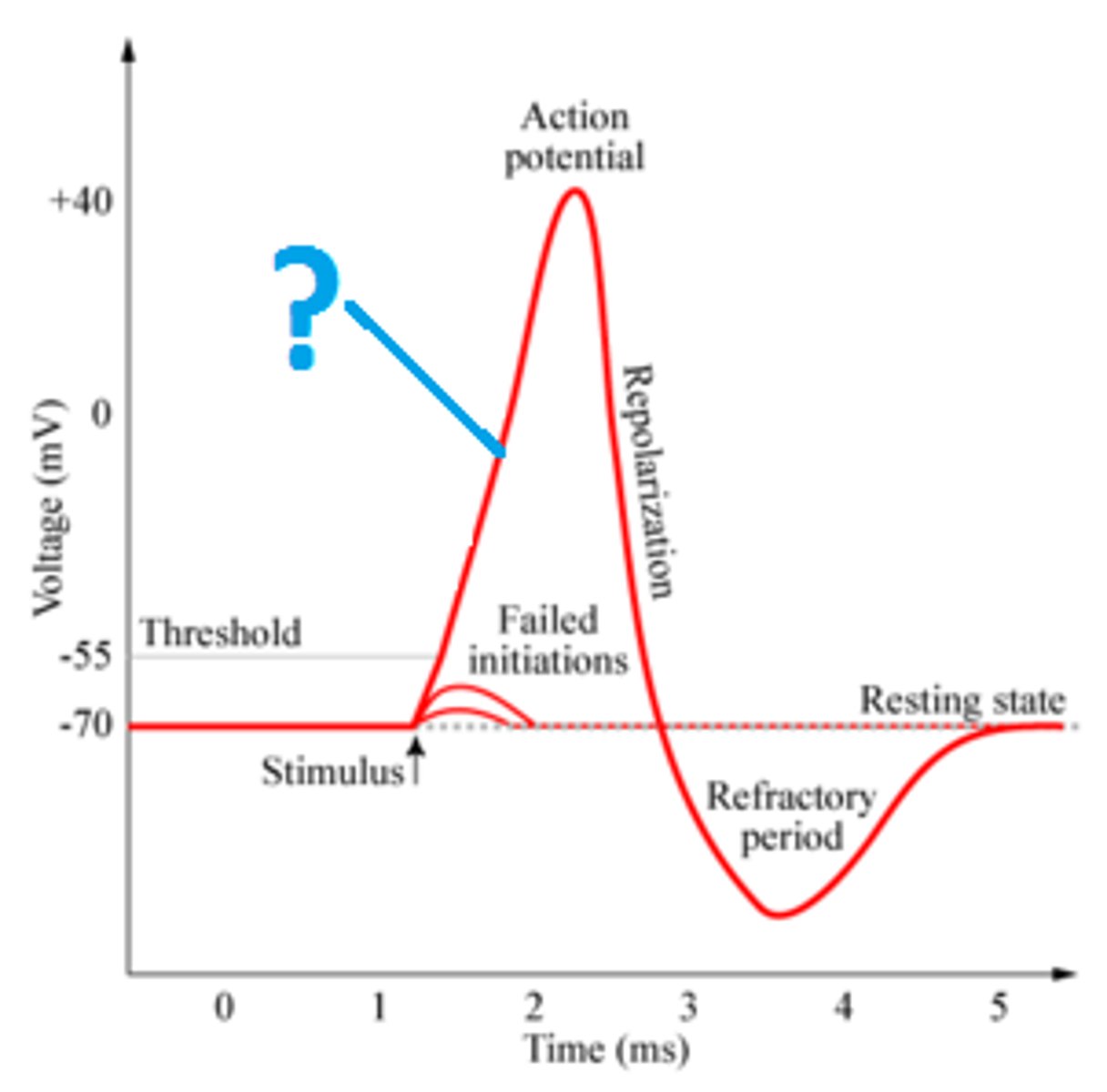
depolarization
membrane potential becomes less negative
Repolarization
membrane would return to its original state (would become more negative -70)
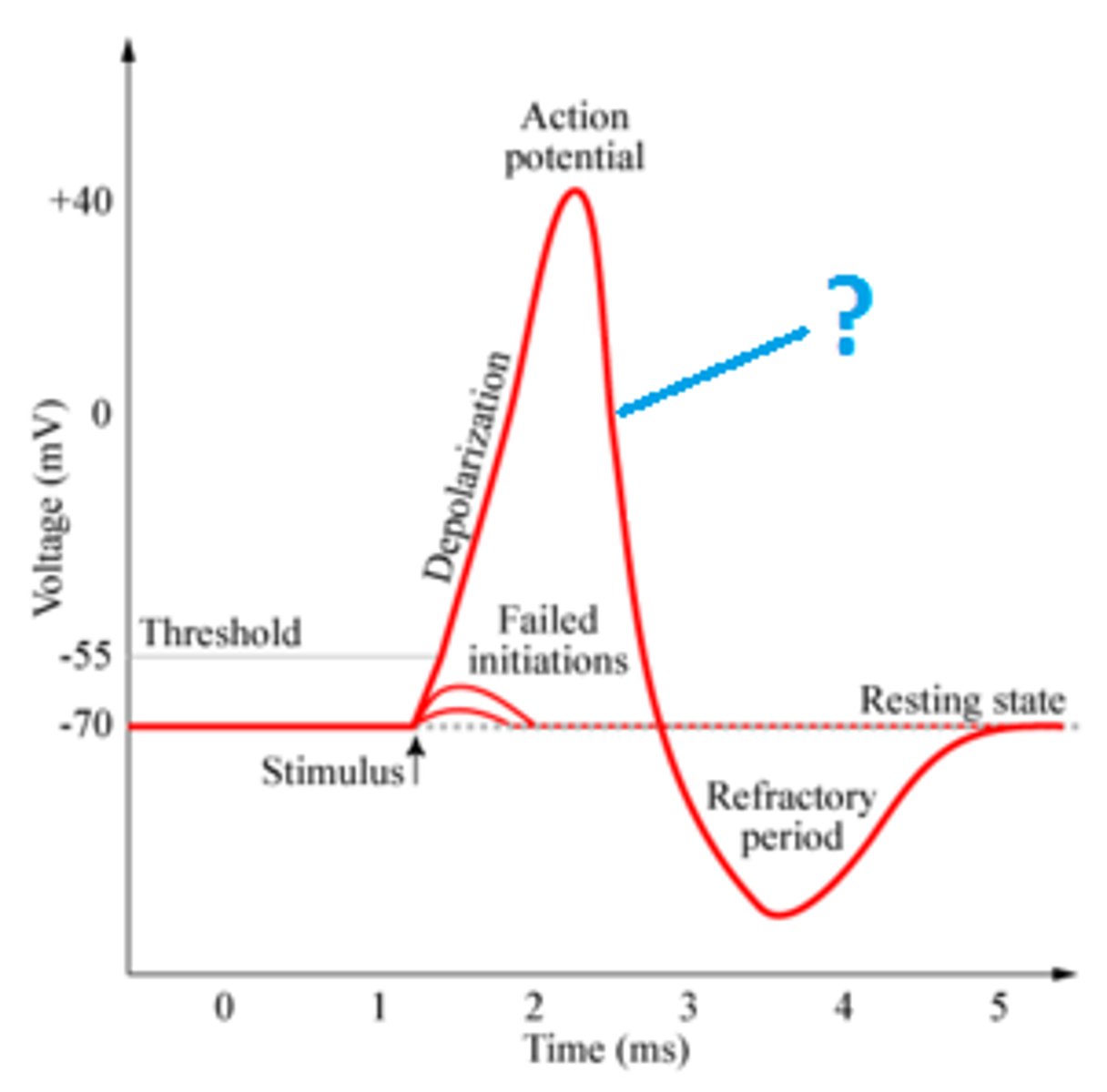
Hyperpolarization
the membrane goes past its resting potential and is more negative before eventually depolarizing to get back to its original state
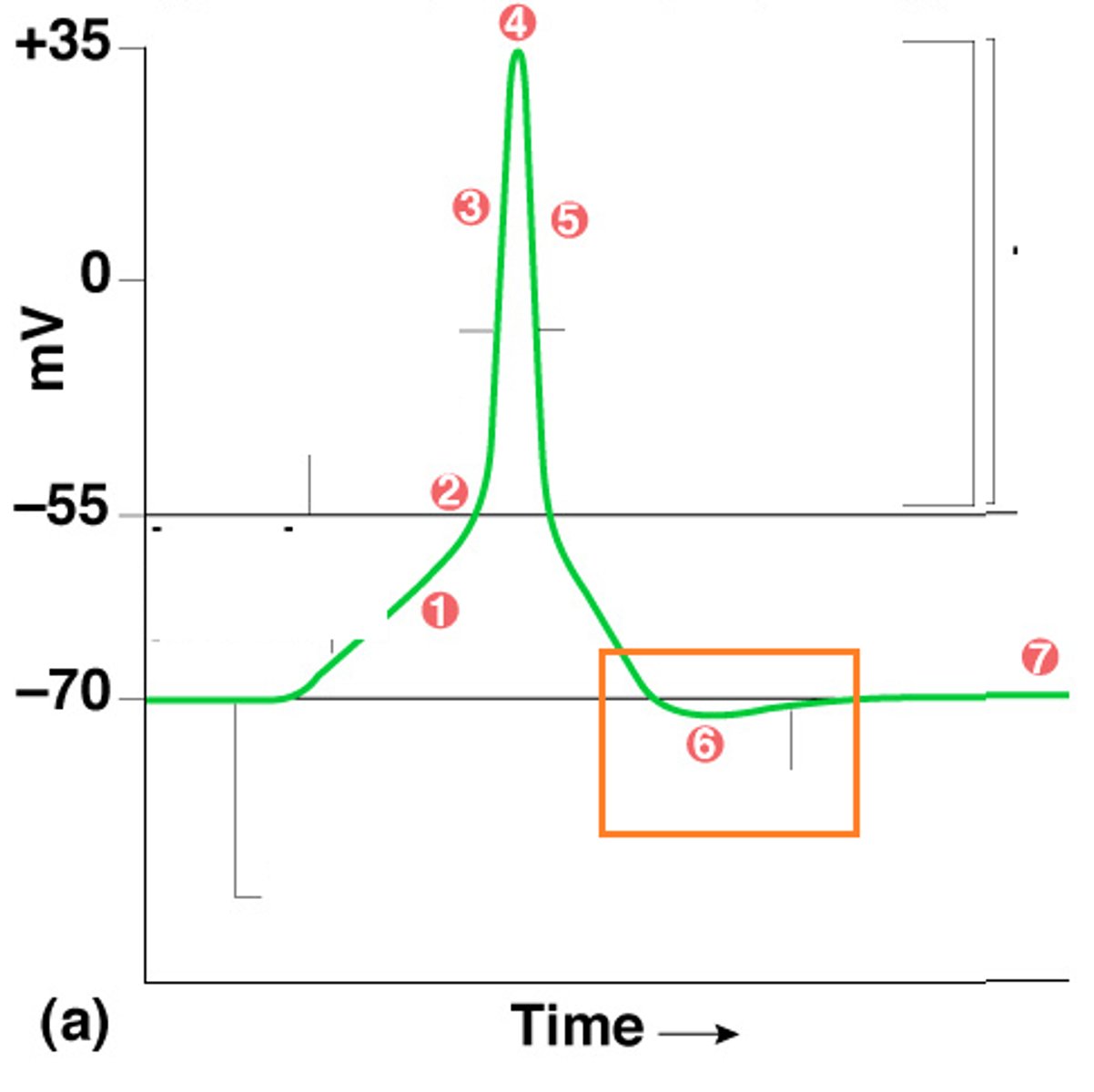
Increasing or decreasing ion permeability can cause changes in the membrane potential difference (Vm)
Entry of Ca2+ or Na+ into the cell will depolarize the cell (membrane potential becomes more positive)
Entry of Cl- into the cell hyperpolarizes the cell (makes the membrane potential more negative)
making the cell less permeable to K+ will make the membrane depolarize
produce and store insulin in cytoplasmic secretory vesicles
they secrete insulin when blood glucose levels exceed homeostatic range (after a meal) - 120 mg/dL
- insulin serves as the signal to other cells to take up glucose, bringing blood conc. down to pre-meal levels
they must be able to respond to blood glucose levels that are higher than acceptable range
must be able to translate the change in glucose conc. into cell action
coordination between membrane function and overall cell function
Pancreatic beta islet cells do what?
1. low blood glucose 60-120 mg/dL
2. metabolism slows (low cell. resp.)
- low facilitated diffusion w/GLUT
3. ATP decreases
4. Katp channels open
5. cell at resting membrane potential. no insulin released...voltage gated Ca2+ channel closed
no insulin secretion
Beta cell at rest. what is happening?
1. high blood glucose > 120 mg/dL
2. metabolism increases (high cell resp.)
- high facilitated diffusion w/GLUT
3. ATP increases
4. Katp channels close
5. cell depolarizes and calcium channels open
6. Ca2+ entry acts as an intracellular signal
7. Ca2+ signal triggers exocytosis and insulin is secreted
Beta cell secretes insulin. what is happening?