The Immune System | BIOL117
1/184
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
185 Terms
infectious agents can ________ or ________ a host
damage; kill
six major categories of infectious agent
bacteria
viruses
fungi
protozoans
multicellular parasites
prions
virulent
ability of microorganisms to cause serious diseases/side effects
what are the different shapes of bacteria?
rod (bacilli)
spherical (cocci)
coiled (spirilla)
virulent bacteria may have __________, __________, or release _________, or ____________
pilli; capsule, toxins; damaging enzymes
how does prion cause diseases?
prion mess with the structure of protein and make them nonfunctional
bacteria (prokaryotes/eukaryotes, cell membrane/cell wall, virulence factors, common examples)
prokaryotes
BOTH cell membrane and cell wall
VF: have either pili that allow it to attach to a cell or a capsule to give it extra protection from the body defense, or releases toxins or damaging enzymes
e.g., clostridium tetani, bacillus anthracis, clostridium c difficiles, etc
virus (prokaryotes/eukaryotes, cell membrane/cell wall, virulence factors, common examples)
no alive (neither prokaryotes/eukaryotes)
no cell wall/cell membrane - have a shell, capsid
VF: insert viral DNA to instruct the nuclei to protein viral RNA
e.g., common cold, influenza, herpes zoster
fungi (prokaryotes/eukaryotes, cell membrane/cell wall, virulence factors, common examples)
eukaryotes
cell membrane AND cell wall
VF: spores releasing proteolytic enzymes that causes inflammation
examples (three type)
—> superficial: athletes’s foot, ring worm, onychomycosis
—> mucosalL yeast infection, thrush
—> internal: Aspergillosis, candidiasis
protozoan (prokaryotes/eukaryotes, cell membrane/cell wall, virulence factors, common examples)
eukaryotes
cell membrane (no cell wall)
VF: inherent parasites (can work in or outside of cell)
examples
—> malara
—> giardiasis
—> trichomoniasis
helminth (prokaryotes/eukaryotes, cell membrane/cell wall, virulence factors, common examples)
eukaryotes
cell membrane (without cell wall)
VF: take nourishment from the host and eating their way through cell
examples:
—> tapeworm, pinworm, roundworm
prion (prokaryotes/eukaryotes, cell membrane/cell wall, virulence factors, common examples)
neither eukaryotes or prokaryotes (fragment of infectious protein - misfolded proteins) - all the same amino acids but assembled differently
no cell membrane or cell wall
VF: the misfolded properties cause the protein to act haywire and cause diseases
examples:
—> Mad Cow Disease
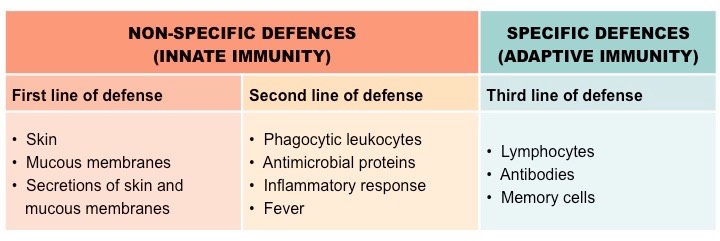
when does monocytes become macrophages?
when it leave the blood and enter the tissues
characteristics of innate immunity
prevent entry of any potential harmful substances
responds nonspecifically
two lines of defense (external —> internal)
no memory of the response (generalized and does not remember the pathogens)
characteristics of adaptive immunity
destroy potential harmful substances
respond specifically (to what the body know) with T & B lymphocytes replication and response
one line of defense (the third line of defense)
keep memory of the response (specific and remember the pathogens)
what cells in the body release antibody and where does that cell come from?
plasma cells, which come from B-lymphocytes when activated (basically B-lymphocyte differentiate when activated)
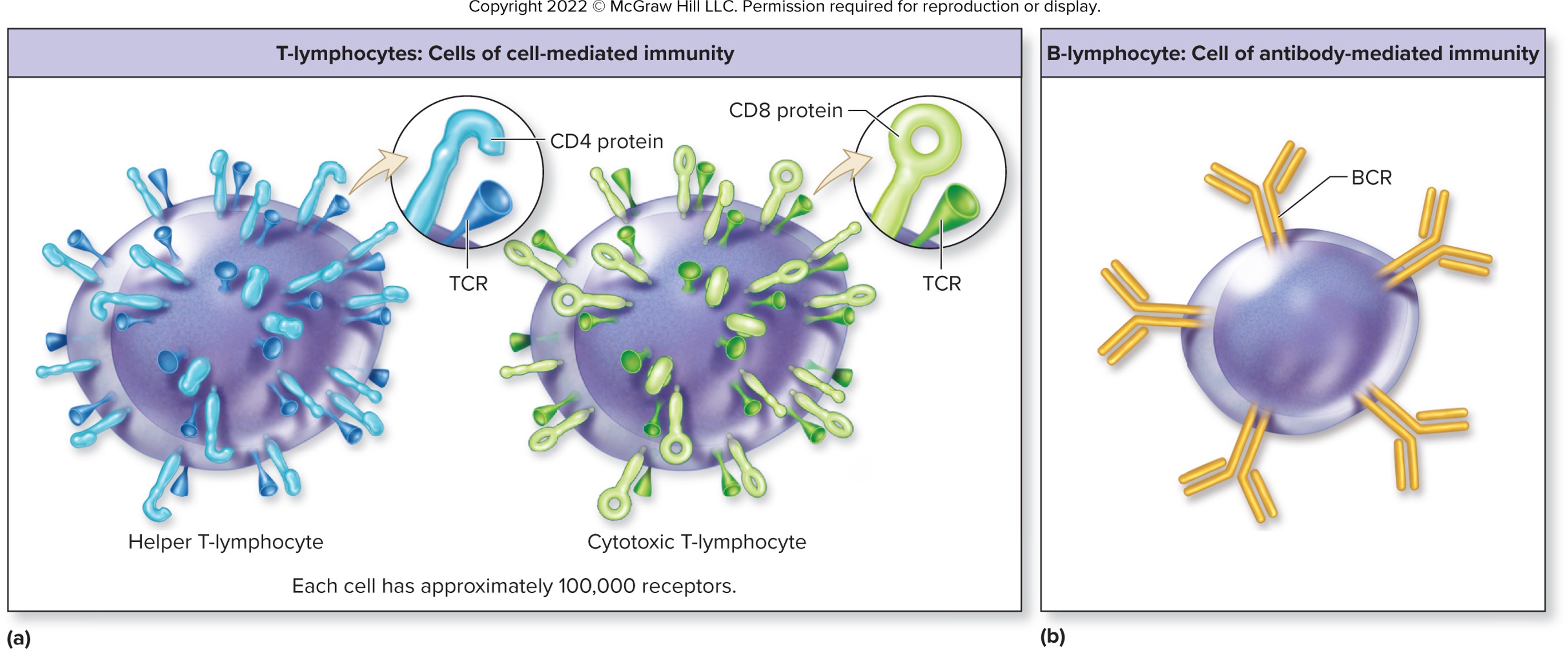
differences between T & B lymphocytes in mediated immunity
T - cell-mediated immunity
B - antibody-mediate immunity
what is the body first line of defense
skin and mucosal membrane (and their secretion)
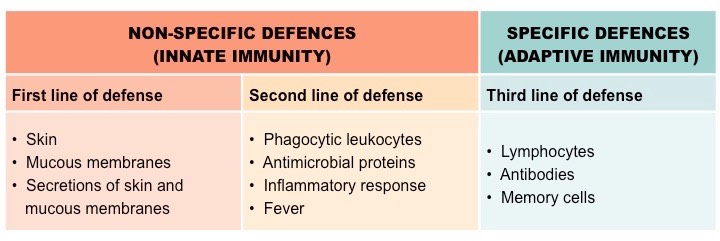
what is the body second line of defense
internal processes: inflammation, fever, and granulocytes (neutrophils, macrophages, dendritic cells, eosinophils, basophils, and NK cells - NOT agranulocyte)
cytokines
small proteins that regulate immune activity through chemotaxis, controlling development and behavior of immune cells, regulating inflammatory response, and destroying cells
innate immune respond _________ while adaptive immunity __________ to be effect
immediately; takes several days
differences between autocrine, paracrine, and endocrine cytokines
autocrine - act on on the cells that released it (influence one’s own activity)
paracrine - act on local cells (influence local activity)
endocrine - act on distant cells after circulating through the blood (influence elsewhere activity)
true or false: cytokines is produce by both the innate and adaptive immune system
true
interferon
a type of cytokines made by virus-infected cell to protect nearby cells from the viruses by basically signalling that it is infected so neighboring cells can response by making antiviral proteins to block virus replication and activate immune cells (e.g., NK cells)
interferon (IFN) alpha and beta (secreted by, function)
produced by virus infected cell to signal that the cell is infected and for neighboring cells to start producing antiviral proteins to protect themselves
also activate NK cells and T-lymphocyte
interferon (IFN) gamma (secreted by, functions)
produced by T-lymphocutes and natural killer cells to stimulate macrophages to destroy virus-infected cells to phagocytize infected cells)
complement (secreted by, functions)
a group of inactive protein secreted by the liver until trigger - destroy bacteria and mark pathogens for elimination
activated through infection
forms the Membrane Attack Complex (MAC) to punch holes (cytolysis) in bacteria cell walls, leading to cell death
helps with opsonization (marking pathogens for phagocytosis) and triggering inflammation
elimination of immune complexes
cytolysis
destruction of a cell
how are proteins in the complement system recognized naming wise?
letter “C”
(DO NOT NEED) what are the three pathway of complement proteins?
classical pathway - antibody attaches to foreign substance then complement binds to the antibody
alternative pathway - complement binds to PAMPs (pathogen-associated molecular pattern) of bacterial or fungal cell wall
lectin pathway - complement binds to lectins on bacterial or fungal cell wall
opsonization
a process done by complement proteins to mark pathogens for phagocytosis
true or false: few microbes can penetrate the intact skin
true
dermcidin (secreted by, function)
secreted by: sweat glands
functions: antimicrobial peptide that kills bacteria and fungi on the skin surface
lysozyme (secreted by, function)
secreted by: saliva, tears, mucus, and sweat
functiona: breaks down bacterial cells walls, killing bacteria
sebum (secreted by, function)
secreted by: sebaceous (oil) gland
function: lubricates the skin and hair and has antimicrobial properties to inhibit bacterial growth
defensins (secreted by, function)
secreted by: skin, mucous membranes, and neutrophils
function: antimicrobial peptides that poke holes in bacterial cells membranes
skin releases antimicrobial substances from ________ glands and ________ glands
sweat; sebaceous
function of mucous membrane as part of the immune system
produce mucus to prevent entry of microbes and release antimicrobial substances (e.g., defensin, lysozymes, IgA)
IgA (immunoglobin A - location & function)
an antibody that plays a key role in protecting mucosal surfaces (areas exposed to the external environment)
located mainly in mucus, saliva, tears, breast milk, and secretion from the respiratory, digestive, and urogenital tracts
neutralize pathogens before they can infect cells
commensal microflora
AKA normal microflora
microorganisms that reside on body surfaces (e.g., GI tract, skin)
nonpathogenic
interfere with attachment of potential pathogenic organisms
true or false: while the second line of defense include selected immune cell and antimicrobial proteins, they are still nonspecific and does not remember the pathogens that they kills, just kill any potentially harmful substance
true
function of neutrophils in the immune system
destroy engulfed particles
functions of dendritic cells and macrophages in the immune system
destroy particles and then present fragments so that the specific immune cells (e.g., T lymphocytes) can learn and kill that pathogens
basically the post office that show the FBI most wanted list
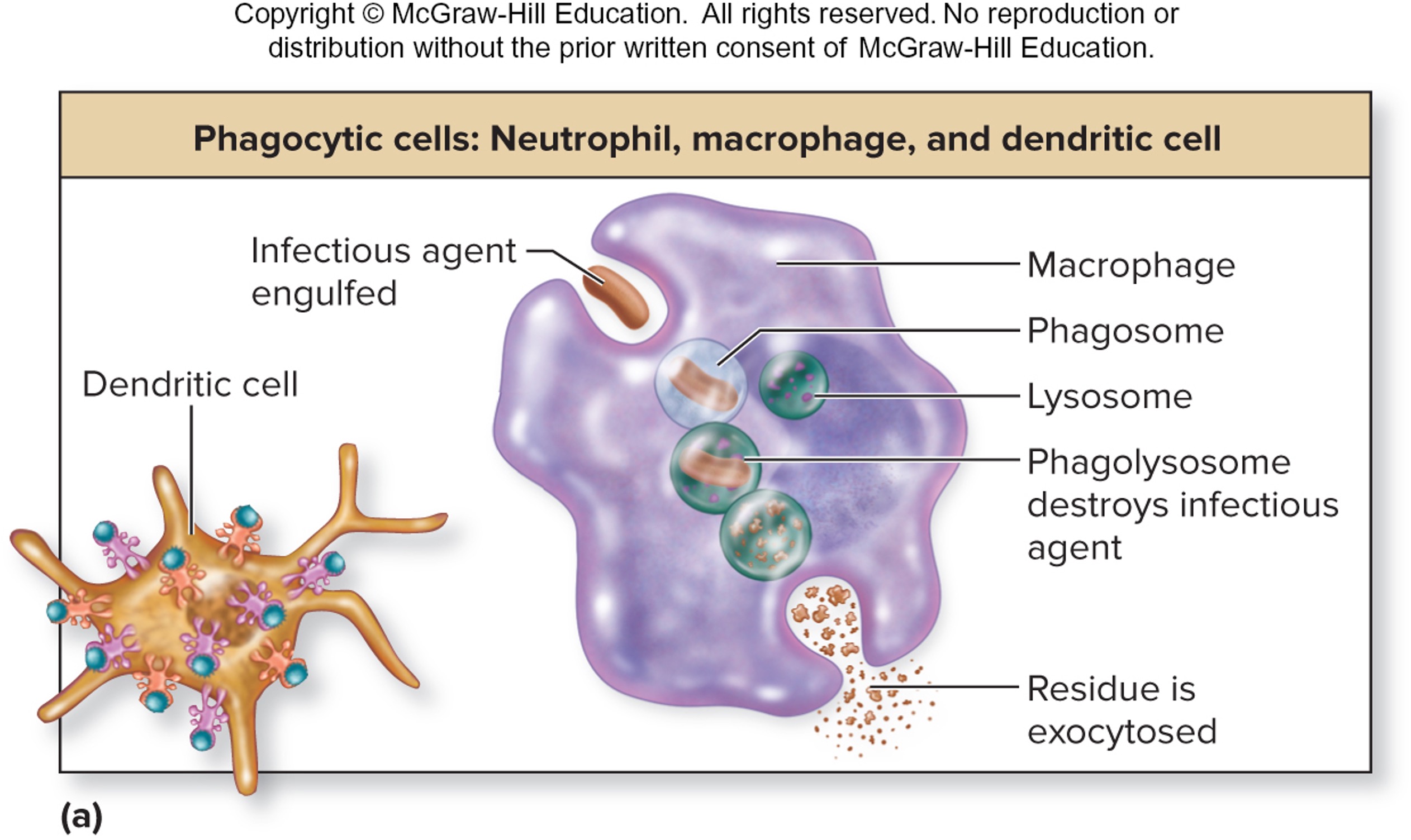
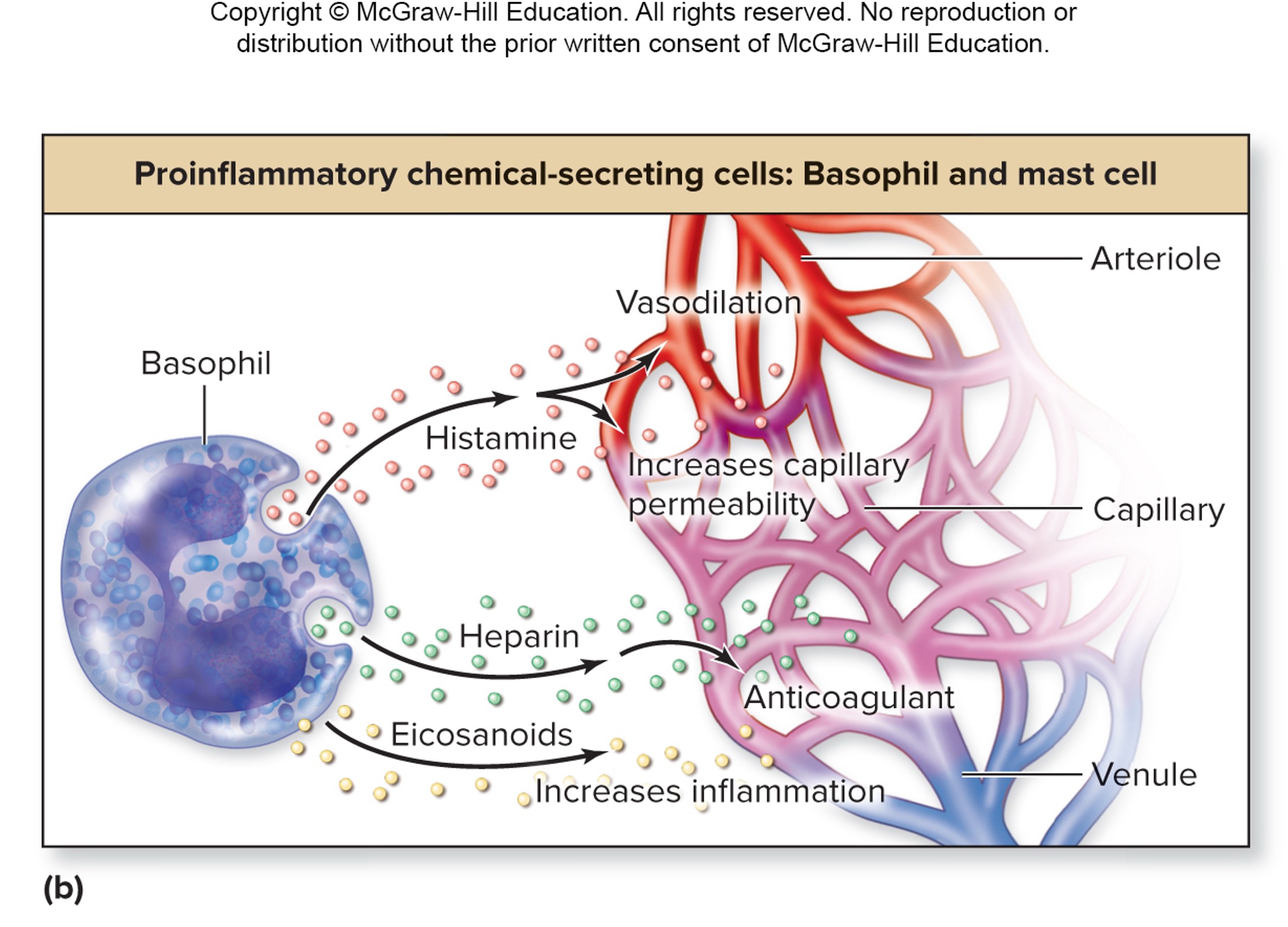
functions of basophils and mast cell in the immune system
promote inflammation
release granules containing chemicals (histamine, heparin, ecosanoids)
—> chemicals increase movement of fluid from blood to injured tissue
—> some induce chemotaxis (attract immune cells)
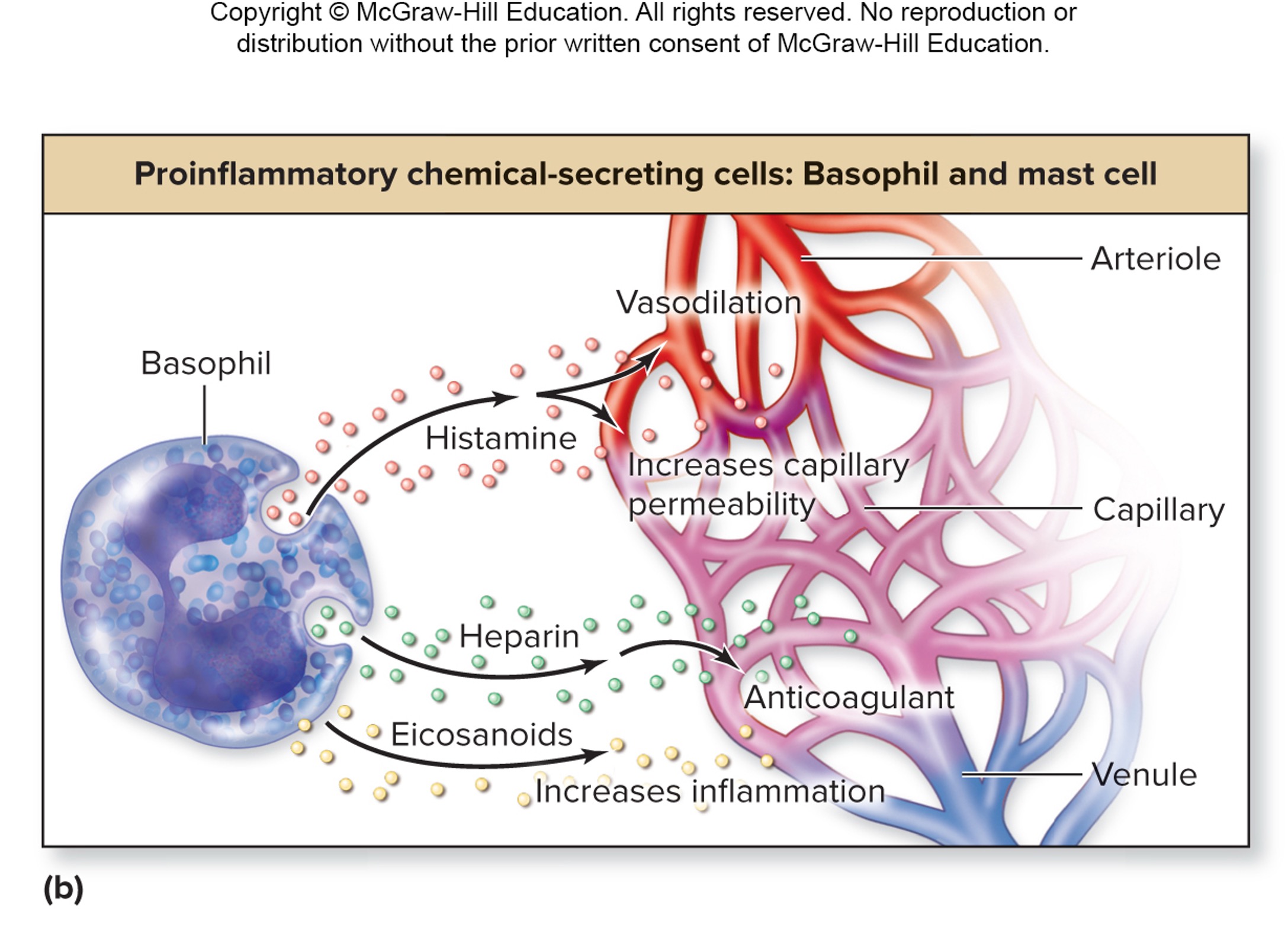
histamine (secreted by, function)
basophil and mast cells
increases vasodilation and capillary permeability (triggering inflammation)
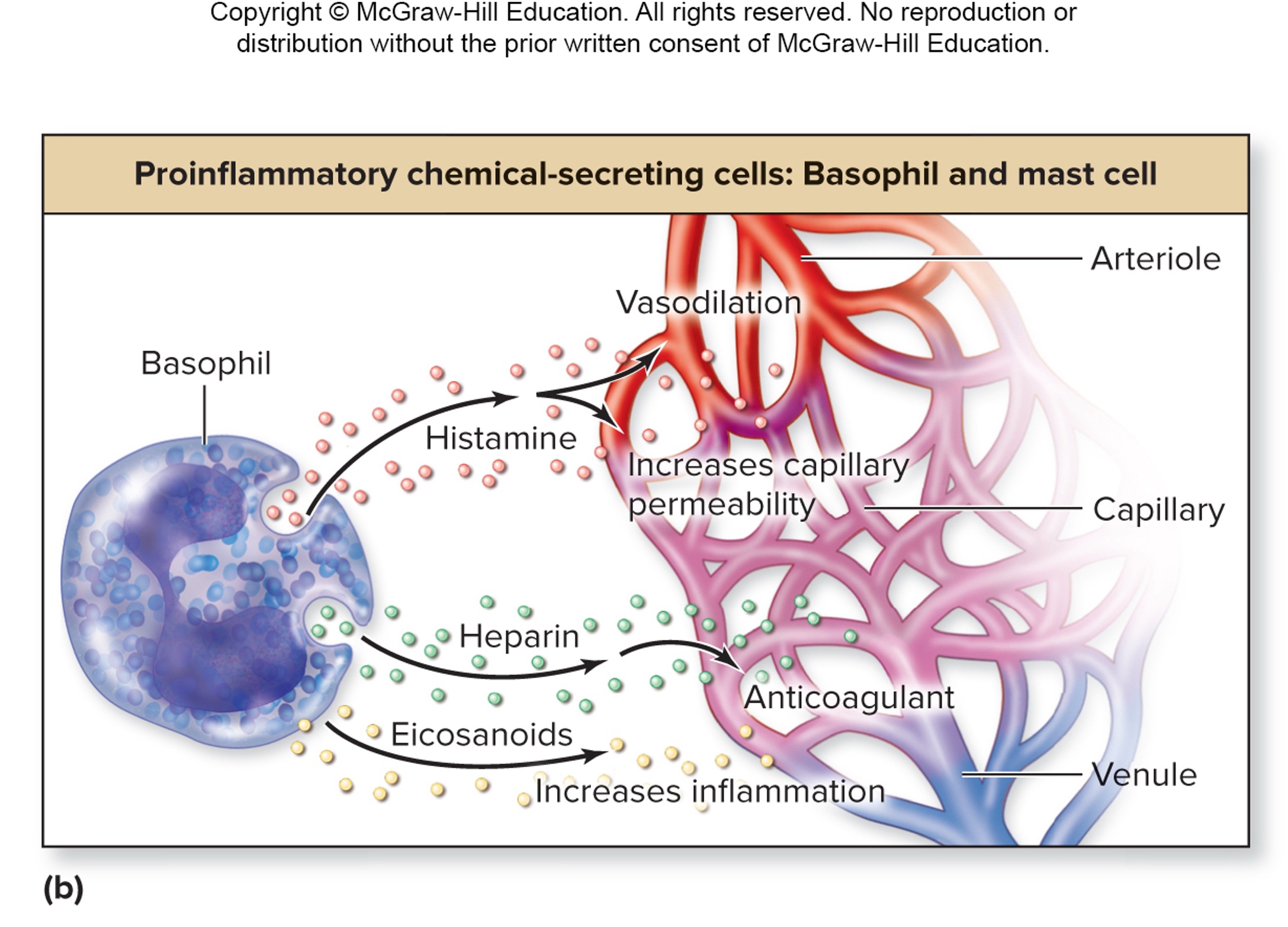
heparin (secreted by, function)
basophil and mast cells
acts as an anticoagulant
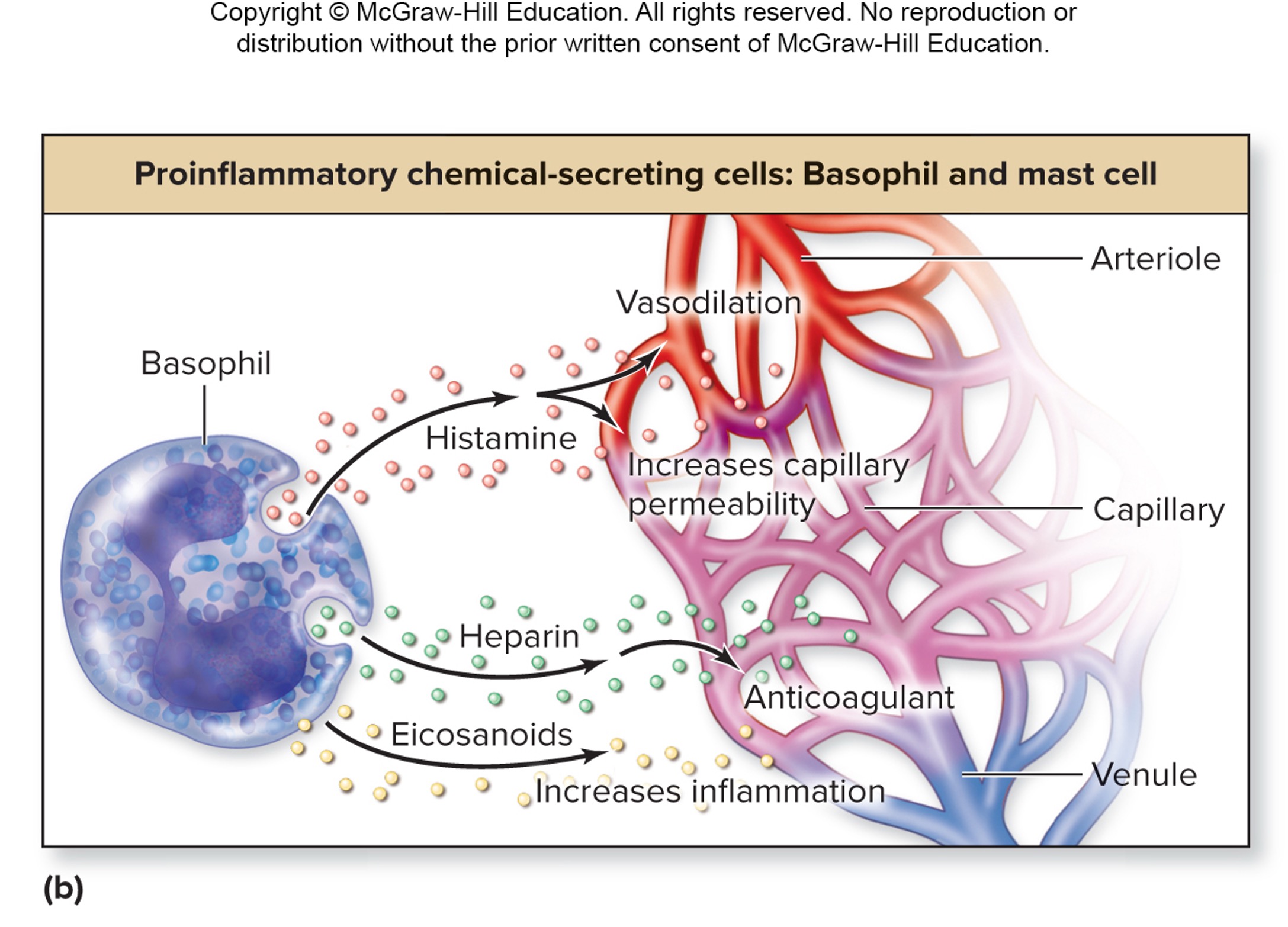
eicosanoids (secreted by, function)
basophils and mast cells
increases inflammation
how does phagocytosis of neutrophil destroy the pathogen?
respiratory burst - the pathogens will be destroy through reactive oxygen contain molecules - create a burst
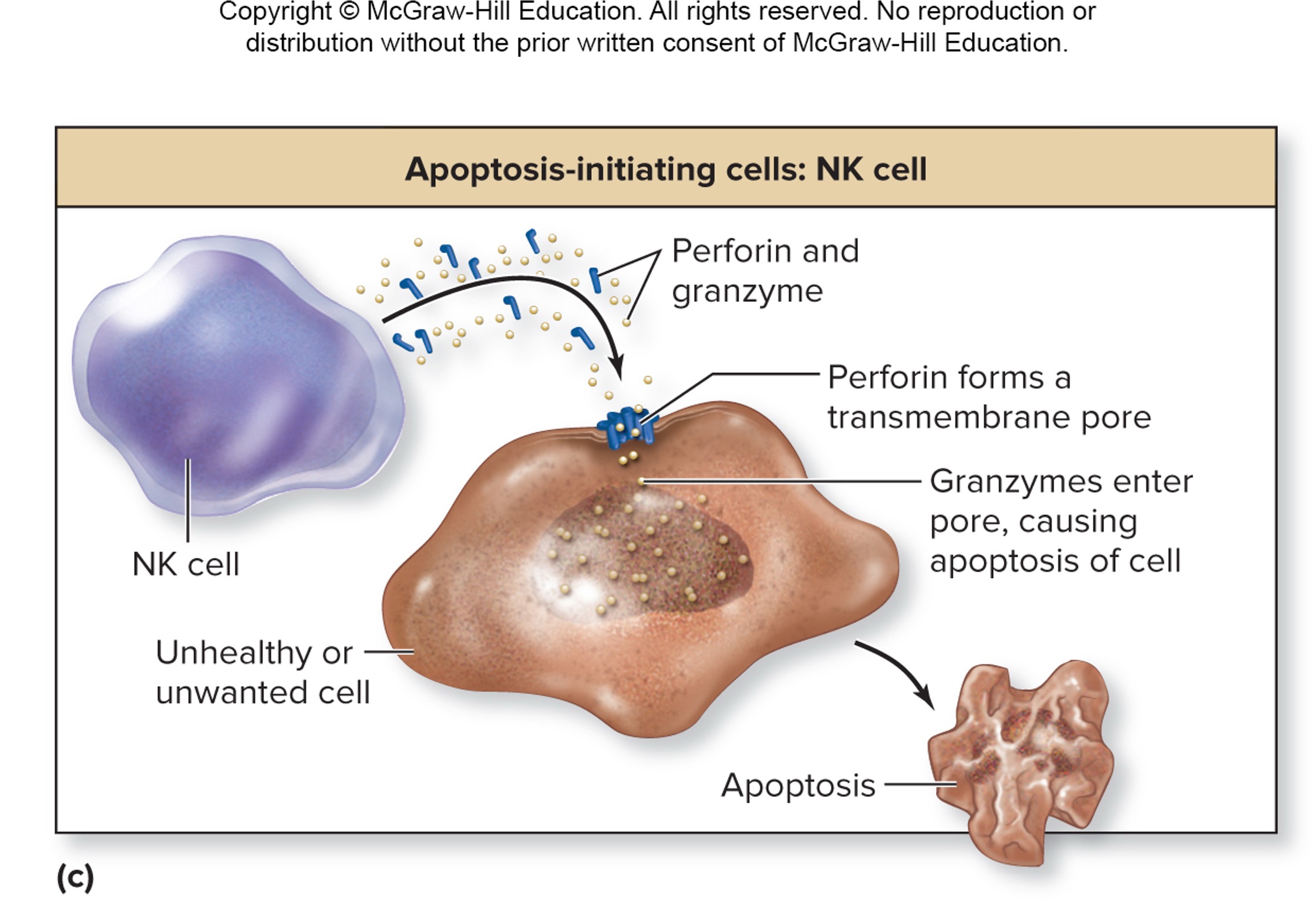
function of natural killer cells
destroy unhealthy/unwanted cells (e.g., virus/bacteria-infected cells, tumor cells, cells of transplanted tissue)
perform immune surveillance (patrol the body, detect unhealthy cells)
release perforin (creating pores on targeted cells)
release granzymes (cause apoptosis of cells)
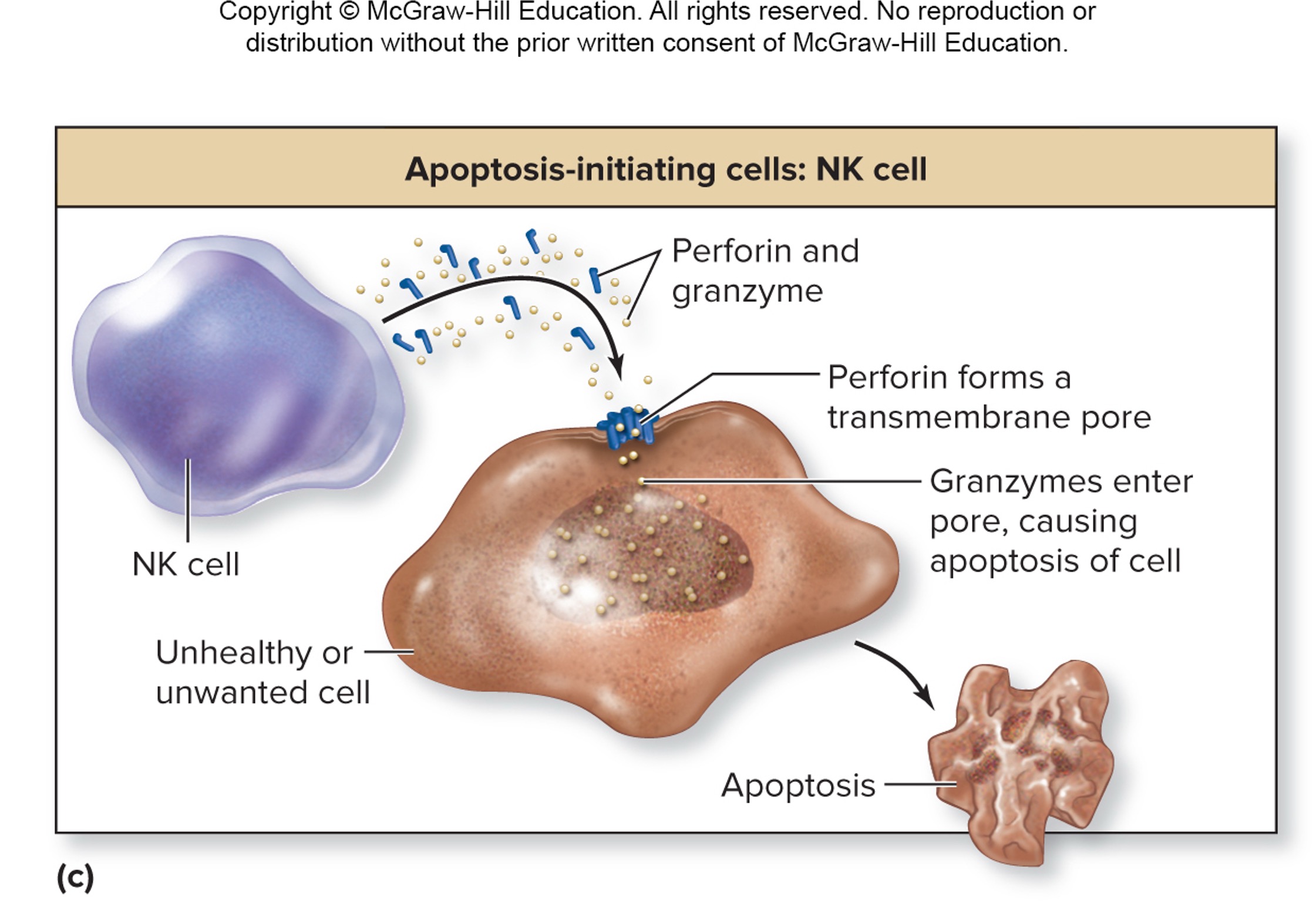
perforin (secreted by, function)
natural killer cells (NK cells)
create transmembrane pores in unwanted cells
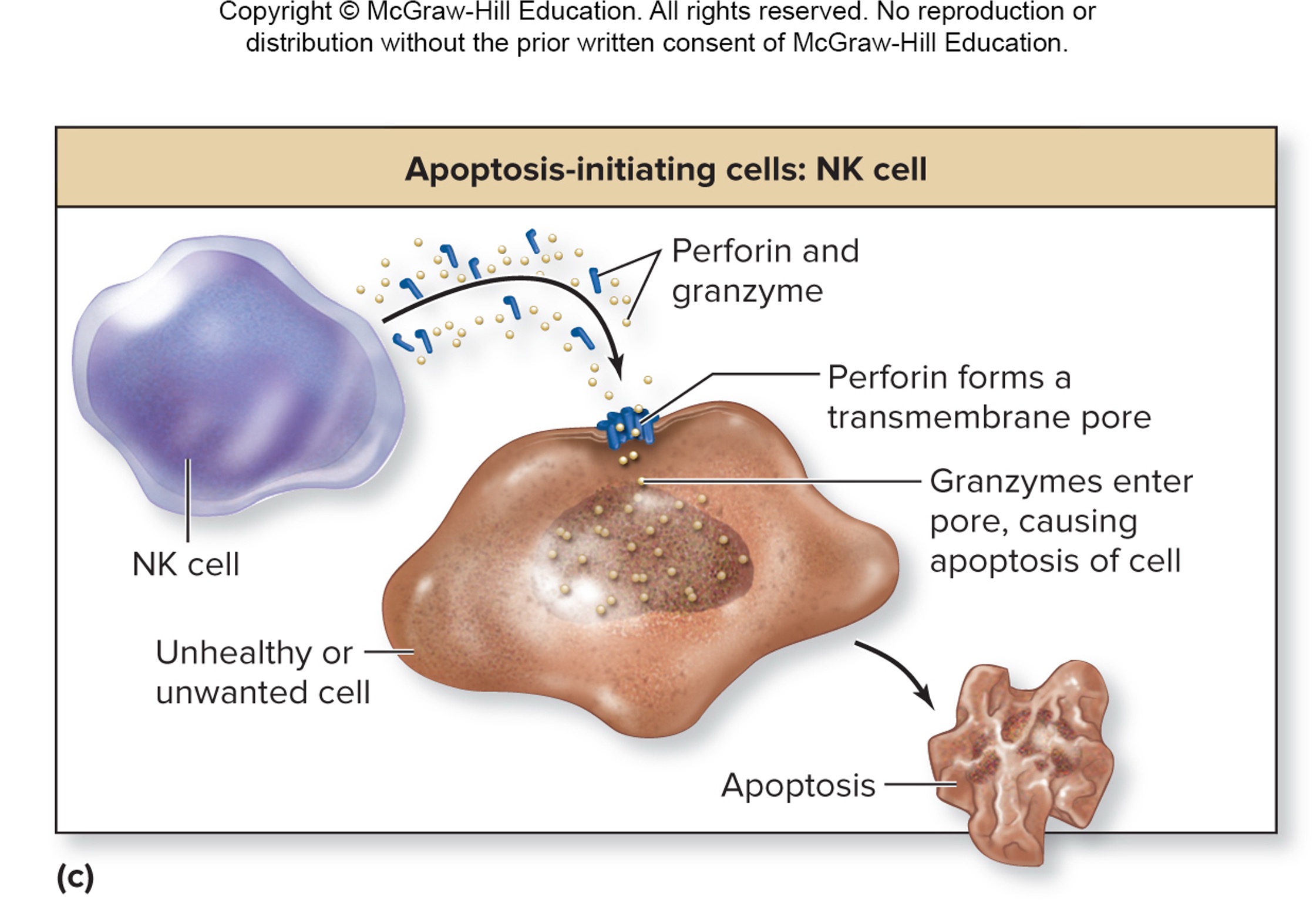
granzymes (secreted by, function)
natural killer cells (NK cells)
enter the pore created by perforin and cause apoptosis of cell
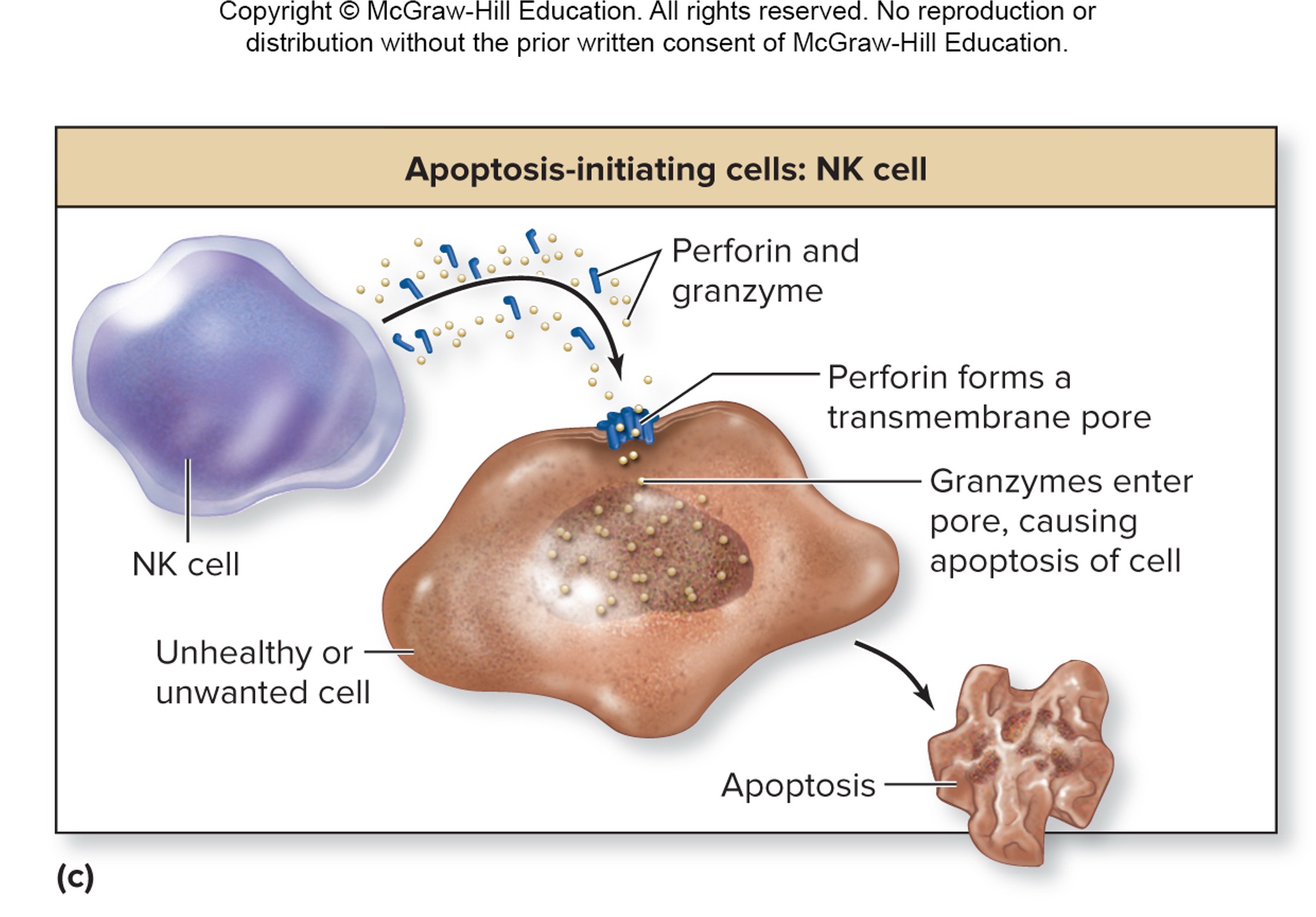
apoptosis
cell death cause by shriveling of cells
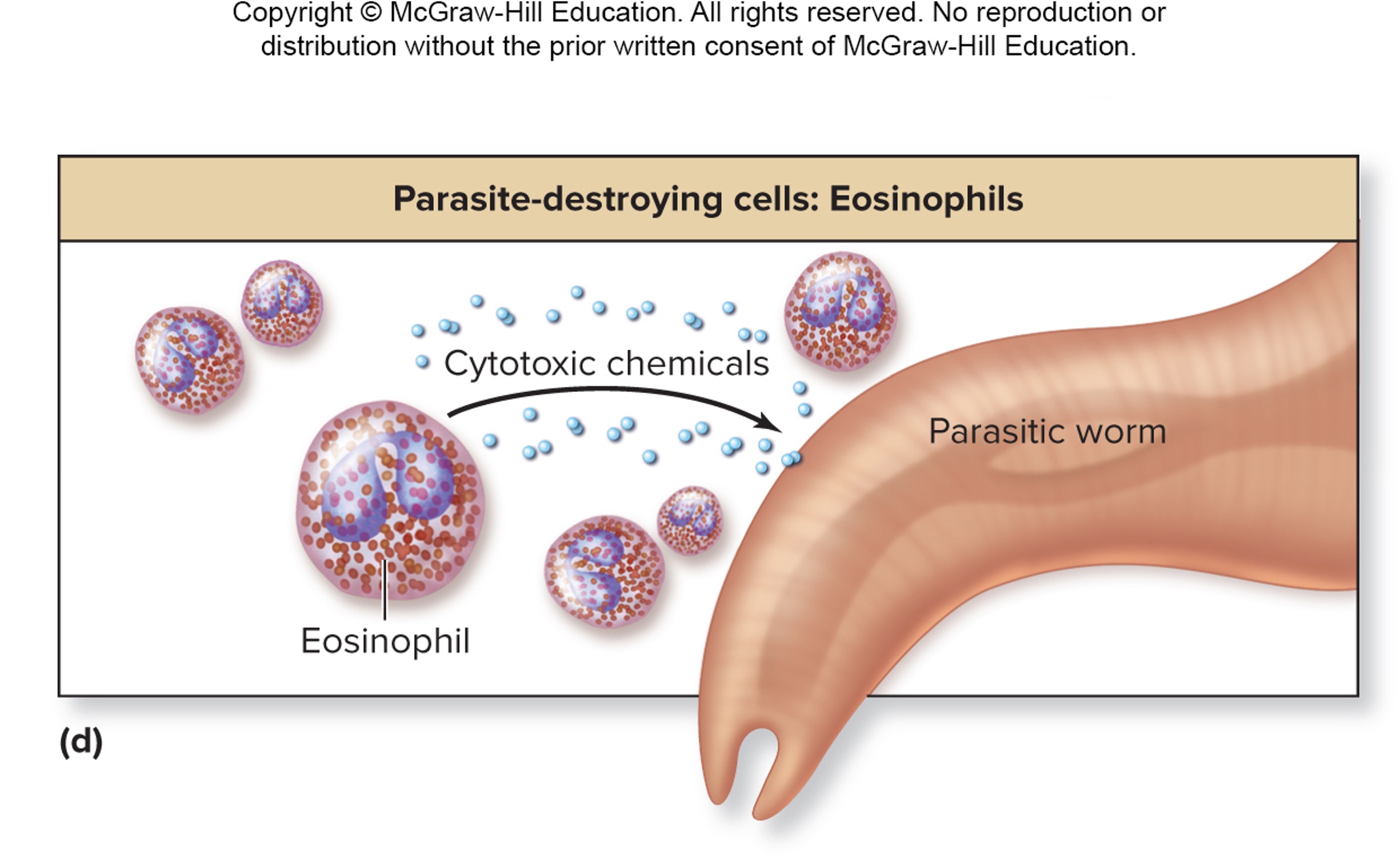
how does eosinophils attack multicellular parasites?
release proteins (enzymes and toxic substances) that form transmembrane pores in parasite’s cells
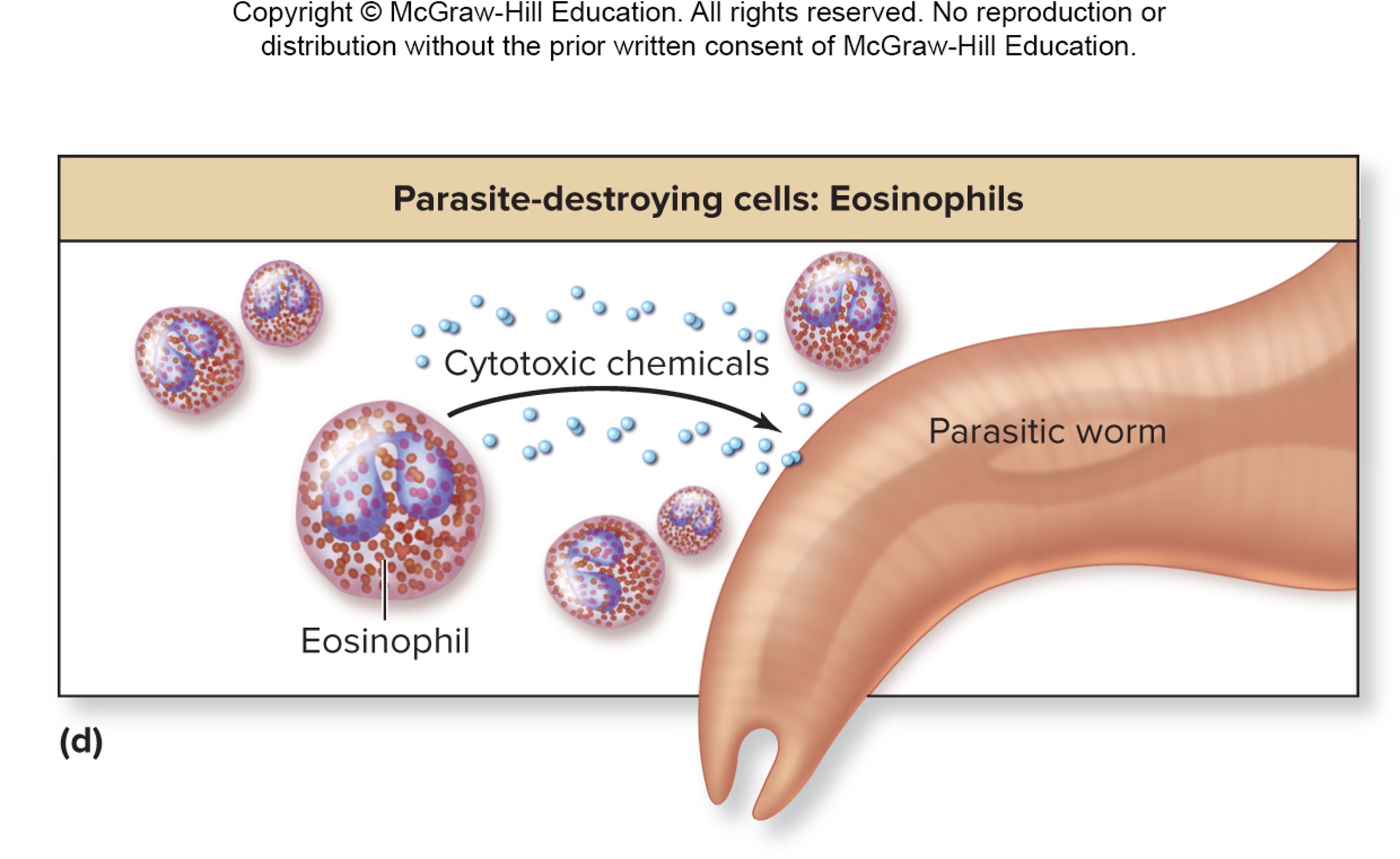
true or false: beside from killing parasites, eosinophil also participate in immune response of allergy, plasma and phagocytosis of antigen-antibody complexes
true
cell of innate immune system recognized microbes as foreign because of _________
receptors (toll-like receptors) - that either recognizes or do not recognizes the pattern on the microbes surface
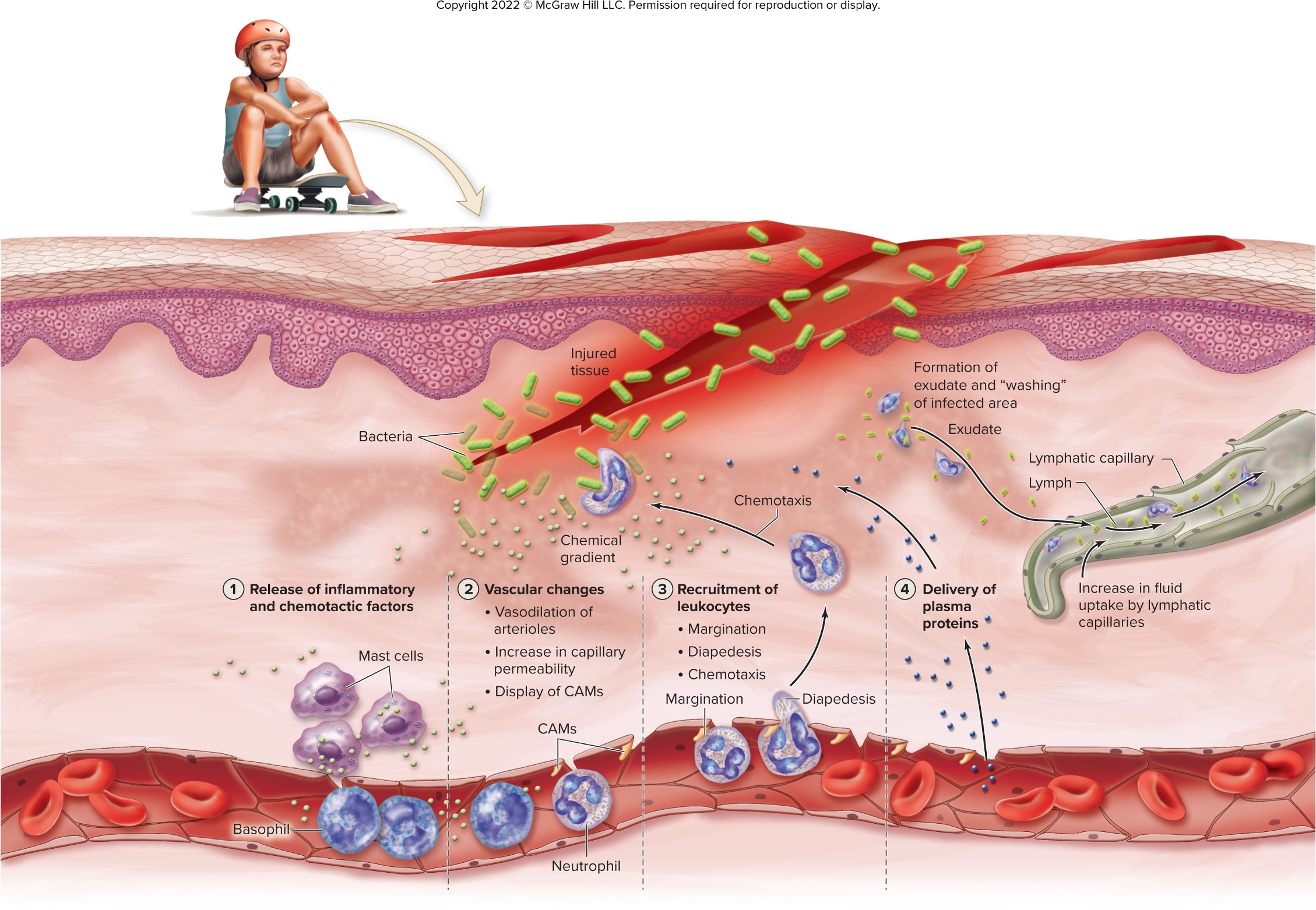
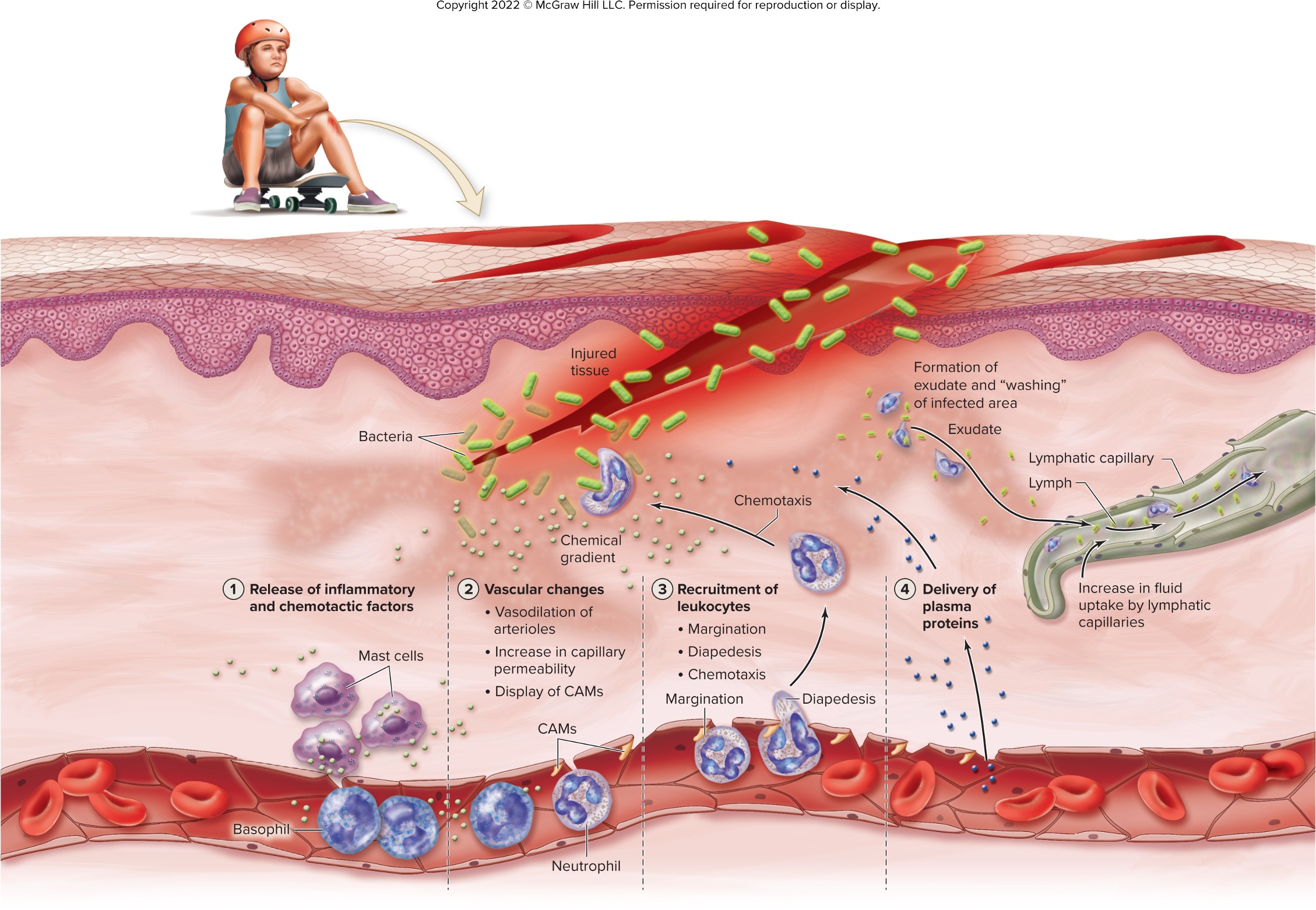
steps of inflammations
an immediate response to ward off unwanted substance (local/nonspecific)
release of chemical that initiate immune response
release of chemicals that cause vascular changes (vasodilation, increased capillary permeability, increased endothelial expression of molecules for leukocyte adhesion, CAMs)
recruitment of leukocytes through margination, diapedesis, and chemotaxis
delivery of plasma proteins - form clots, stimulate pain receptors (kinin), increase cpaillary permeability (kinin), increase production of CAMs by capillary cells (kinin)
kinin (secreted by, function)
liver and other cells (from inactive kininogens)
stimulate pain receptors, increase capillary permeability, increase production of CAMs by repillary cells
margination of leukocytes
more and more leukocytes adhere to the endothelial membrane of blood vessels through cell adhesion molecules
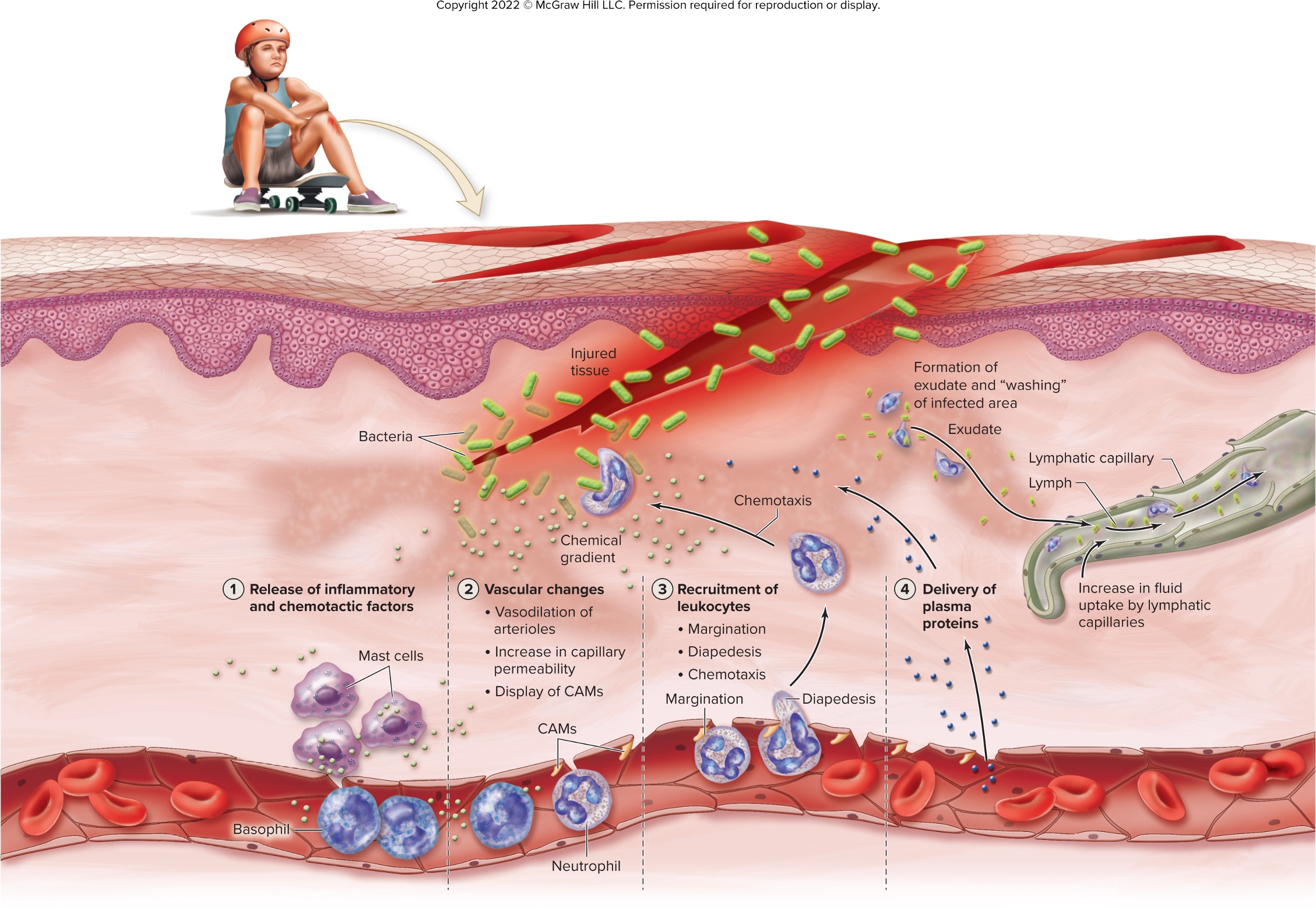
diapedesis of leukocytes
leukocytes squeeze out of the blood vessels wall and into the tissues where the infection site is location
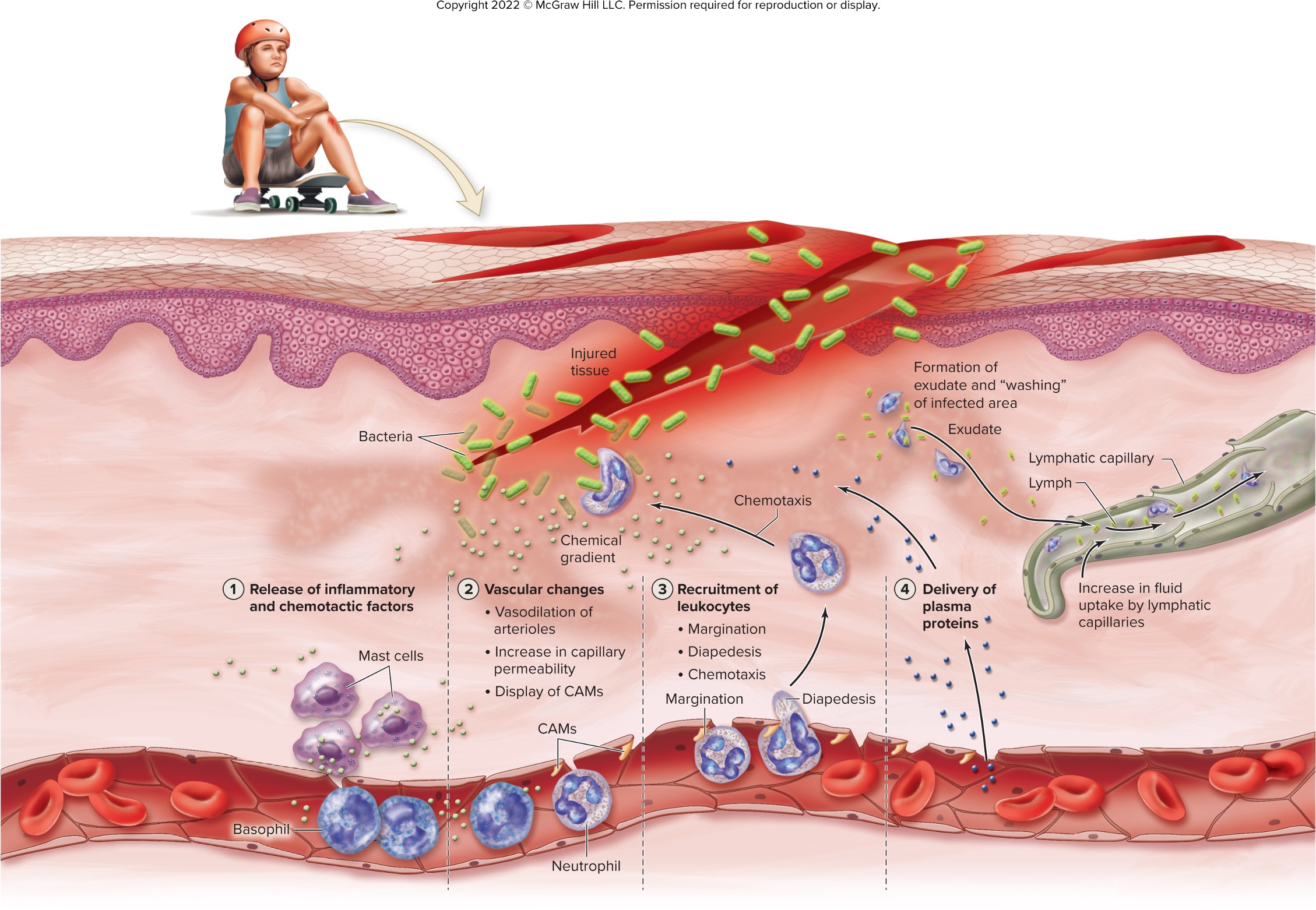
chemotaxis of leukocytes
leukocytes migrate toward chemicals released from damaged dead, or pathogenic cells
pyrogens (secreted by, function)
macrophages
fever-inducing
what are the chemicals involve with inflammation)?
histamine, leukotrienes, prostaglandins, chemotactic factors
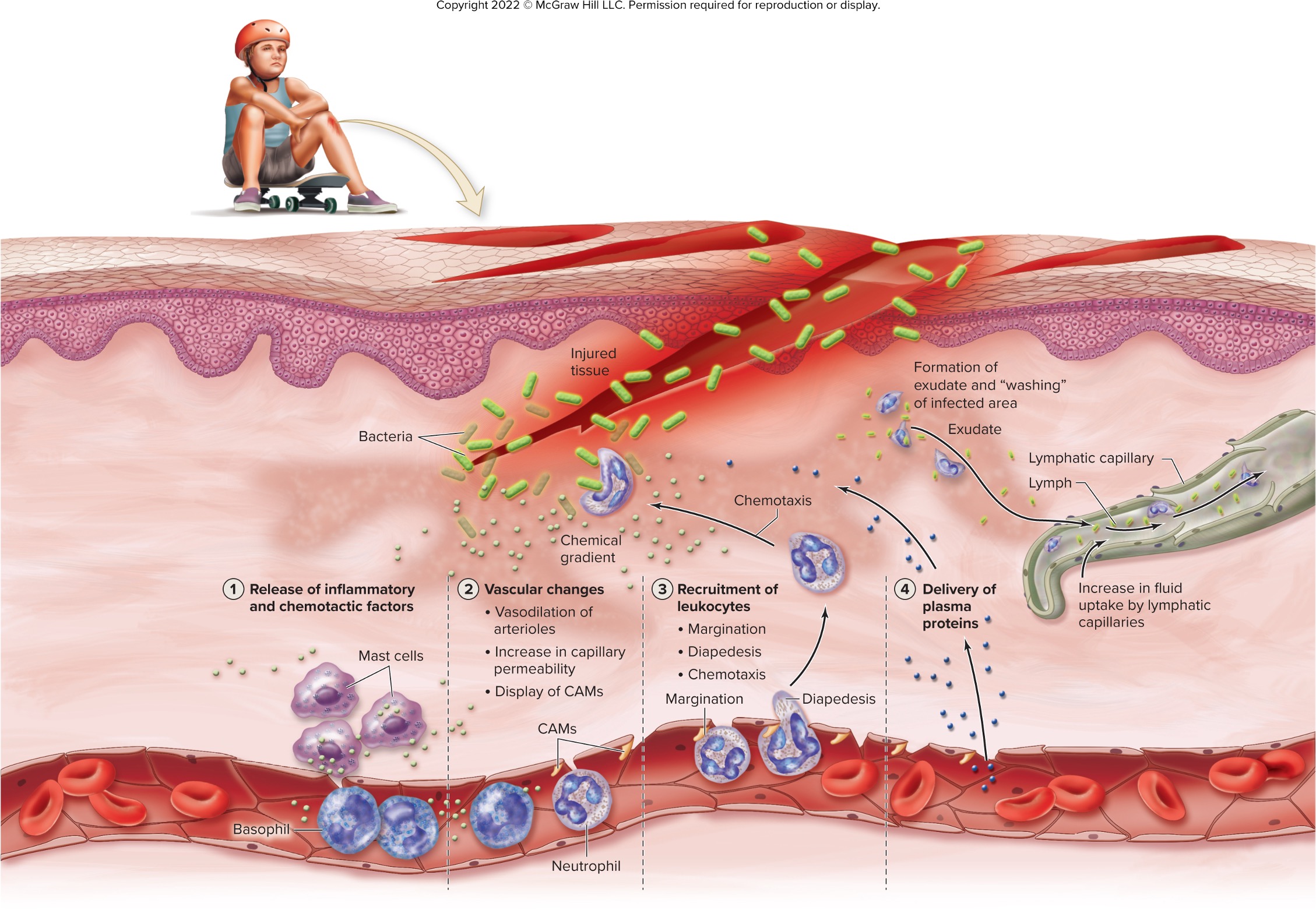
recall the effect of inflammation (how does it happens and what does it cause?)
fluid (exudate) moves from blood to injured or infected area in the tissues
—> increasing cpaillary permeability
vasodilation brings more blood to the area
loss of plasma proteins to decrease osmotic pressure, thus decreasing fluid reabsorption into the blood (swelling - extra fluid to “wash” infected through lymphatic capillaries) and proteins also help with immune response
macrophages eats bacteria, damaged host cells, and dying neutrophils
tissue repair begins as fibroblast form new CT
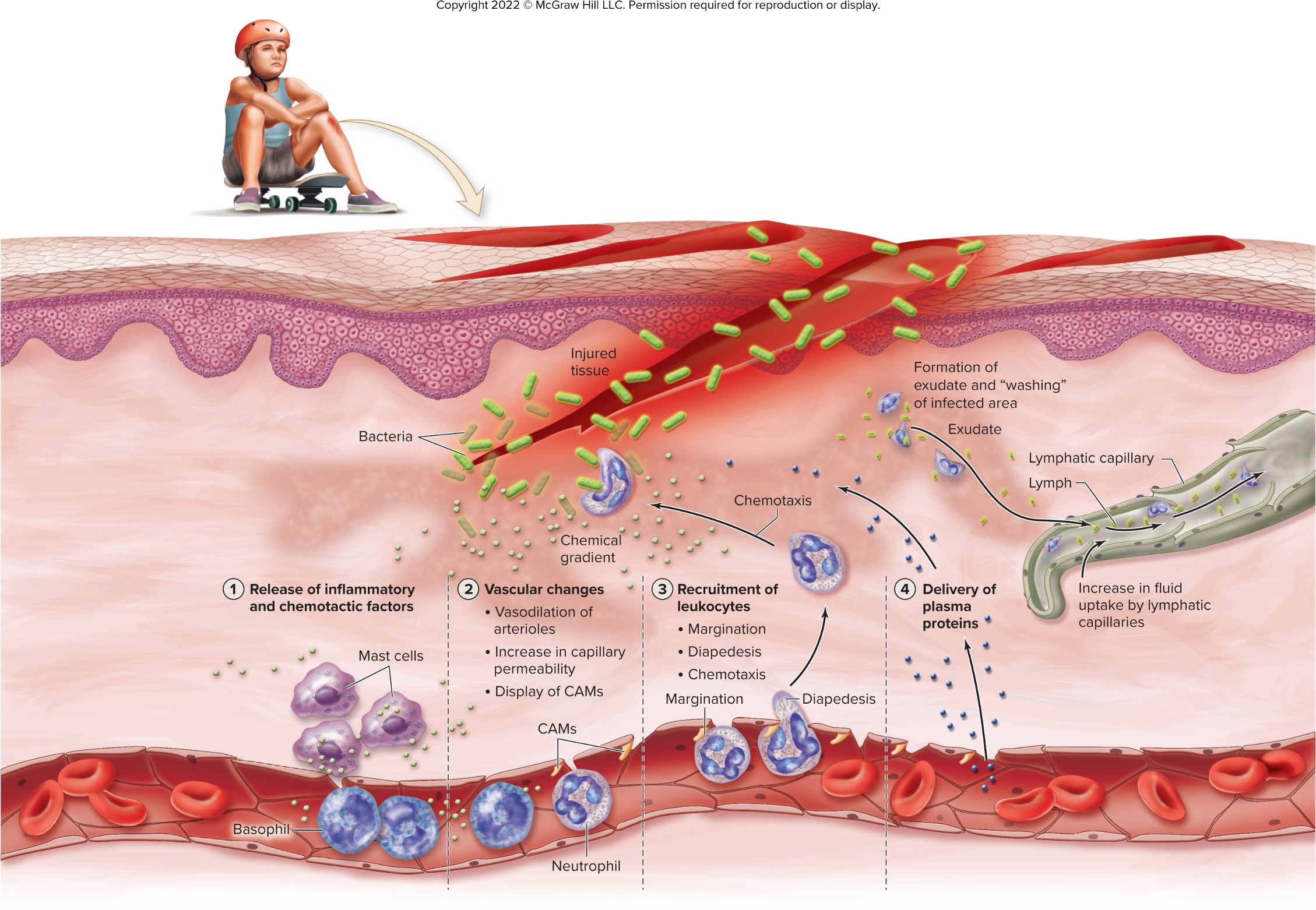
4 hallmarks (cardinal signs) of inflammation & its pathology
redness (increased blood flow)
heat (increased blood flow and increased metabolic activity)
swelling (increased in fluid loss from capillaries into the tissue)
pain (stimulation of pain receptors by kinin)
fever (pyrexia)
abnormal body temperature elevation (1 celcicus or more from normal of 37 celsius) due to release of pyrogens from macrophages or infectious agents
steps of fever
pyrogen circulate throughout the blood and target hypothalamus
once reached, hypothalamus releases prostaglandin E2
prostaglandin E2 signal the hypothalamus to raise temperature set point leading to fever
hypothalamus stimulate constriction of dermal blood vessels (preventing heat loss) & muscle shivering (generate heat)
bodily metabolic rate increases to promote elimination of harmful substances
liver and spleen bind zinc and iron to slow microbial reproduction
defervescence: body return to normal temperature
benefits of fever
inhibit reproduction of bacteria & viruses (higher body temp slow down replication)
promotes interferon activity (fever boosts interferon)
increases activity of adaptive immunity (elevated temperature speed up lymphocyte activation & proliferation)
accelerates tissue repair (heat increases metabolic rates)
increases CAMs (Cell Adhesion Molecules) on endothelium of capillaries in lymph nodes
additional immune cells migrating out of blood
true or false: If either CD4 or CD8 on a T cell matches with MHC Class I or II and binds with moderate strength, the cell survives positive selection because it can recognize self-MHC, which is necessary for proper immune function. However, if the T cell binds too strongly to a self-antigen during negative selection, it undergoes apoptosis to prevent it from attacking the body’s own tissues, helping avoid autoimmunity.
what is the temperature of low-grade, intermediate grade, and high-grade?
low grade: 100-101 F
intermediate grade: 102 F
high grade: 103-104 F
risk of intermediate/high fever or long term low -grade fever
changes in metabolic pathways and denaturation of proteins
possible seizures
irreversible brain damage (greater than 106 F)
death (greater than 108 F)
adaptive immunity involves specific lymphocytes responses to ____________
antigen
_______________ consist of lymphocytes and their products
immune response
since it takes days to develop, __________________ is considered the third line of body’s defense
adaptive immunity
what are the two branches of adaptive immunity and its component?
cell-mediated immunity (T-lymphocytes)
antibody-mediated immunity (B-lymphocytes, plasma cells, and antibodies)
antigens
substance that binds a T-lymphocytes or antibody and can trigger an immune response if foreign to the body
have many different type
what are the barrier that contain viruses as a form?
protein capsid
true or false: bacteria an fungi have capsid
false: bacteria and fungi have cell wall
antigen
any substance (e.g., proteins, carbohydrate, or other molecules) that triggers and immune response because it is recognized as foreign y the immune system
foreign antigen vs. self antigen
Foreign antigen: An antigen from outside the body that usually binds to immune components and triggers an immune response.
Self-antigen: An antigen produced by the body that normally doesn’t bind to immune components, preventing an immune response.
how does autoimmune disorders work?
when the immune system react to self-antigens and instead of ignoring the self-antigen cell, it starts attacking it
antigenic determinant
AKA epitope
specific site on antigen recognized by the immune system (determine if foreign or self)
each antigen can have many different epitopes, each with different shapes
true or false: pathogens tend to have more variety and complexity in their antigenic determinant than human
true; this diversity help them better evade the immune system
immunogen
antigent that induce an immune response
immunogenicity
the ability of an antigen to trigger an immune response
true or false: immunogenicity of an antigen increases with increase in the antigen’s degree of foreignness, size, complexity or quantity
true
haptens (what it is, function, and an example)
small molecules that can’t trigger an immune response on their own but become immunogenic when attached to a carrier molecules (usually a proteins)
can also cause hypersensitivity reactions (allergies)
e.g., the toxin in poison ivy becomes immunogenic when it bind to skin proteins
what happens when the immune system lack tolerance for specific self-antigent?
initiate an immune response as if the cells were foreign
cross-reactivity
forbidden clones
altered self-antigens
entering areas of sequestered antigen
cross reactivity
the immune system mistake self-antigens for foreign antigens because they share similar structures
forbidden clones
harmful cells that attacks the body own cells despite recognizing self-antigens
escaped the elimination process by chance (the body immune response is tasked with destroying all cell like this through negative selection)
altered self-antigens
mutation or damage altered self-antigens which make them look s unfamiliar to the immune system, promoting it to attack them as if foreign
receptor complexes (structure of lymphocytes) and the different type
site on T & B lymphocytes that binds one specific antigens
TCR (t-cell receptor) antigen receptor of T-lymphocytes
BCR (b-cell receptor) antigen receptor of T-lymphocytes
how do B-lymphocyte and T-lymphocyte interact with antigens?
B-lymphocytes: direct contact with the antigen without the need for processing
T-lymphocytes: don’t make direct contact with antigen - required other cells to process and present the antigen to the coreceptors of the T-cell (helper T-cell require APCs while cototix would require the nucleated cells to have antigen fragments)
function of helper T-cells (CD4+)
act as coaches to activate other immunes (e.g., NK cells, macrophages)
guide the immune response
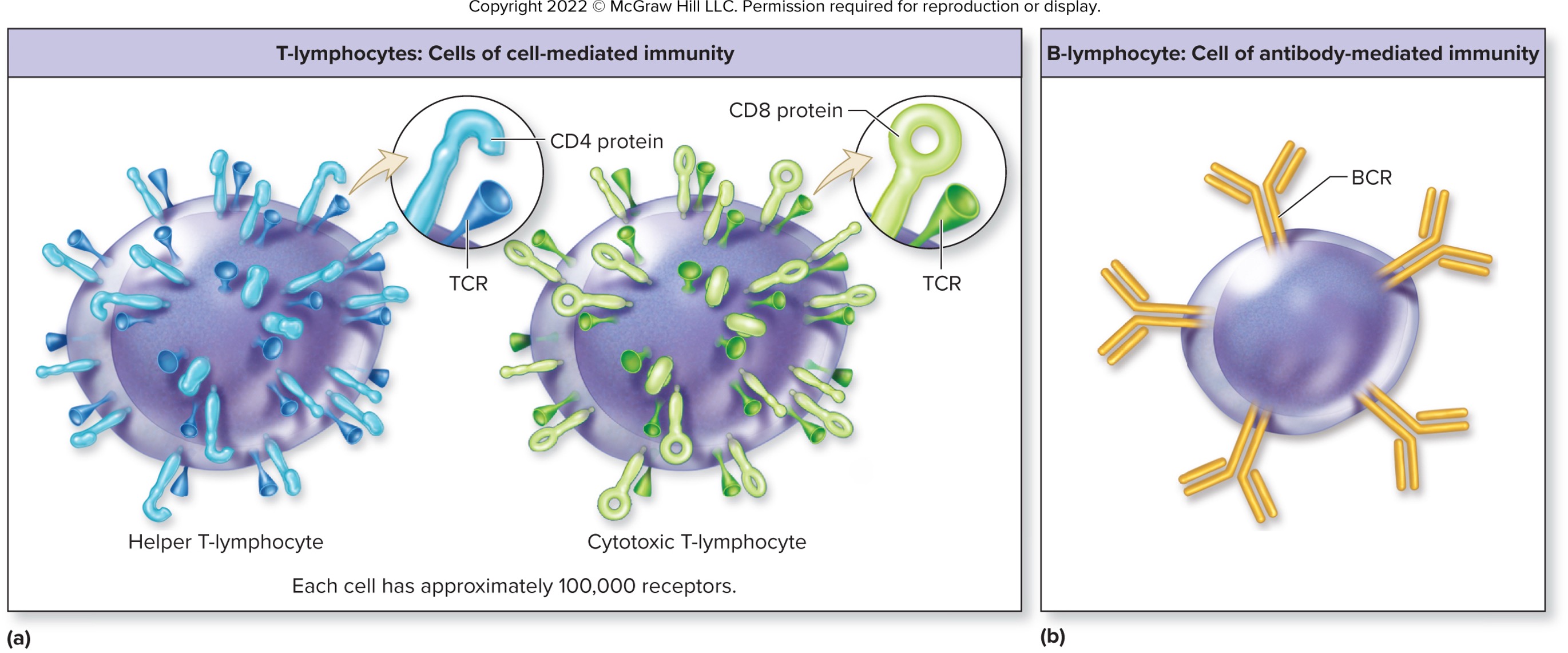
function of cytotoxic T-cells (CD8+)
act as “assassins” to destroy infected or harmful cells
target cells already presenting the antigen
function memory T-cells
remember past invader and respond (e.g., activating an immune response, clal in reinforcement) quickly if the same invader
function of regulatory T-cells
act as the “calm-down squad”
regulate and control the immune response to prevent overraction or autoimmunity
cluster of differentiation
specific surface markers or proteins found on immune cells - help identify and classify different types of immune cells
what is the difference between an antigen and a cluster differentiation (CD)?
• Antigen:
• A foreign substance (e.g., proteins, carbs) that triggers an immune response.
• Examples: Bacteria, viruses, pollen.
• Cluster of Differentiation (CD):
• Cell surface markers or proteins found on immune cells.
• Help identify and classify immune cells (e.g., CD4 on helper T-cells, CD8 on cytotoxic T-cells).
• Not foreign substances, but markers on cells involved in the immune system.
antigen presentation
cells display an antigen on their plasma membrane so T-cells can recognize it and mount an immune response
how does all nucleated cell of the body present antigen?
use MHC I (major histocompatibility complex) to show “self” antigens