Chapter 57: Obesity
1/16
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
17 Terms
Chapter 57: Obesity
Obesity is defined as a BMI ≥ 30.
Overweight is defined as a BMI 25–29.9.
Prevalence is increasing in adults and children.
Obesity is associated with reduced life span and increased morbidity.
Health risks increase with higher BMI and central fat distribution.
Management focuses on quality of life, long-term weight reduction, and prevention of complications.
Health Promotion and Disease Prevention
Lifestyle modification is the foundation of prevention and management:
Reduce calorie intake
Incorporate cultural food preferences
Increase aerobic and resistance exercise
Avoid dietary triggers
Set realistic goals
Manage stress
Use social support
Identify emotional eating patterns
Maintain a food diary
Healthy People 2030 Goals
Reduce the proportion of adults with obesity
Increase access to health care visits that include counseling on:
Weight loss
Physical activity
Dietary recommendations
Decrease consumption of added sugars
Obesity Risk Factors
Lifestyle factors (decreased physical activity)
Medications (corticosteroids, antidepressants)
Genetic predisposition
Cardiovascular disease
Hypertension
Stroke
Chronic stress
Mood disorders (depression)
Hyperlipidemia
Type 2 diabetes mellitus
Bone and joint disorders
Gallstones
Obesity Findings
Body Mass Index (BMI) Categories
Overweight: BMI 25–29.9
Class 1 obesity: BMI 30–34.9
Class 2 obesity: BMI 35–39.9
Class 3 obesity: BMI ≥ 40
Waist Circumference
Strong predictor of long-term complications (central obesity).
Increased risk if:
Female: > 88 cm (35 inches)
Male: > 102 cm (40 inches)
Obesity Care
Promote safe, respectful, nonjudgmental care
Monitor skin integrity and mobility
Encourage gradual lifestyle changes
Collaborate with interdisciplinary team
Considerations
Risks During Hospitalization
Poor wound healing and increased infection risk (reduced blood supply to adipose tissue)
Pressure injuries
Skin folds, moisture, increased friction
Limited mobility
Increased cardiac workload
Obstructive sleep apnea
Increased neck circumference
Reduced lung volume
Hypoventilation, hypoxemia, hypercapnia
Venous thromboembolism (VTE)
Inadequate pain management
May require higher medication doses
Increased risk of injury to client and staff during transfers
Therapeutic Management
Weight Management
Balance energy intake with energy expenditure
Combines diet modification, physical activity, and behavior changes
Lifestyle Modifications
Goal setting
Stimulus control
Cognitive restructuring (address negative thoughts)
Problem solving
Relapse prevention
Physical Activity
Moderate exercise at least 30 minutes daily
Example: walking 1.5 miles per day
Dietary Modifications
Individualized and balanced diet:
Adequate protein
Controlled carbohydrates
Decreased fat
Increased fiber
Calorie restriction as indicated
Limit alcohol intake
Limit refined sugars
Complementary and Alternative Therapies
Acupuncture
Hypnosis
Obesity Meds
Used for clients with elevated BMI and additional risk factors
Always combined with diet and exercise
Orlistat
Decreases fat absorption
Adverse effects: oily stools, flatulence, fecal urgency, vitamin deficiencies
Teach low-fat diet
Take multivitamin supplement
Phentermine
Appetite suppressant
Adverse effects: headache, dry mouth, insomnia, dizziness, constipation
Contraindicated in hyperthyroidism, glaucoma, MAOI use
Take early in the day
Naltrexone-bupropion
Decreases appetite and cravings
Adverse effects: nausea, constipation, headache, dry mouth
Contraindicated in seizure disorders, eating disorders, MAOI use
Monitor for suicidal ideation (antidepressant effect)
Liraglutide
Increases satiety, slows gastric emptying
Adverse effects: nausea, vomiting, diarrhea, tachycardia, hypoglycemia
Used in type 2 diabetes management
Administered subcutaneously
Can be taken with or without meals
A nurse is preparing to teach a newly licensed nurse about medications used for weight management. The nurse should include which of the following medications is administered subcutaneously?
a
Orlistat
b
Liraglutide
c
Naltrexone-bupropion
d
Phentermine-topiramate
b Liraglutide
It should be used with caution for clients who are taking anti-hyperglycemic medications. Liraglutide is also used to lower blood glucose for clients who have diabetes mellitus and can potentiate the effects of other anti-hyperglycemic medications.
Obesity Procedures
Hydrogel Pill
FDA-approved adjunct for BMI 25–40
Taken with meals
Absorbs water to increase gastric fullness
Excreted through GI tract
Adverse effects: constipation, obstruction, diarrhea, dehydration
Contraindicated in Crohn’s disease or prior GI surgery affecting motility
Intragastric Balloon Therapy
Gas- or saline-filled balloon placed endoscopically
Promotes satiety and delayed gastric emptying
Adverse effects:
Nausea and vomiting
Balloon rupture
Gastric or esophageal rupture
Pancreatitis if left in place longer than 6 months
Bariatric Surgeries
Surgical treatment for obesity when lifestyle and pharmacologic therapy fail.
Achieves weight loss by:
Restricting stomach capacity
Causing malabsorption via small intestine bypass
Combination of both mechanisms
Can be open or minimally invasive.
Some clients later undergo plastic surgery (abdominoplasty, breast reduction) for excess skin.
Preoperative: upper endoscopy to rule out GI disease.
Postoperative: barium X-ray to evaluate for anastomotic leaks.
Often improves comorbidities:
Hypertension
CAD
Hyperlipidemia
Asthma
Sleep apnea
Type 2 diabetes mellitus
Indications
BMI ≥ 40 without comorbidities
BMI ≥ 35 with at least one obesity-related condition (HTN, osteoarthritis, type 2 DM)
BMI 30–34.9 with poorly controlled glucose despite medications and lifestyle changes
Bariatric Surgeries Types
Restrictive Procedures
Decrease stomach capacity while maintaining normal digestion.
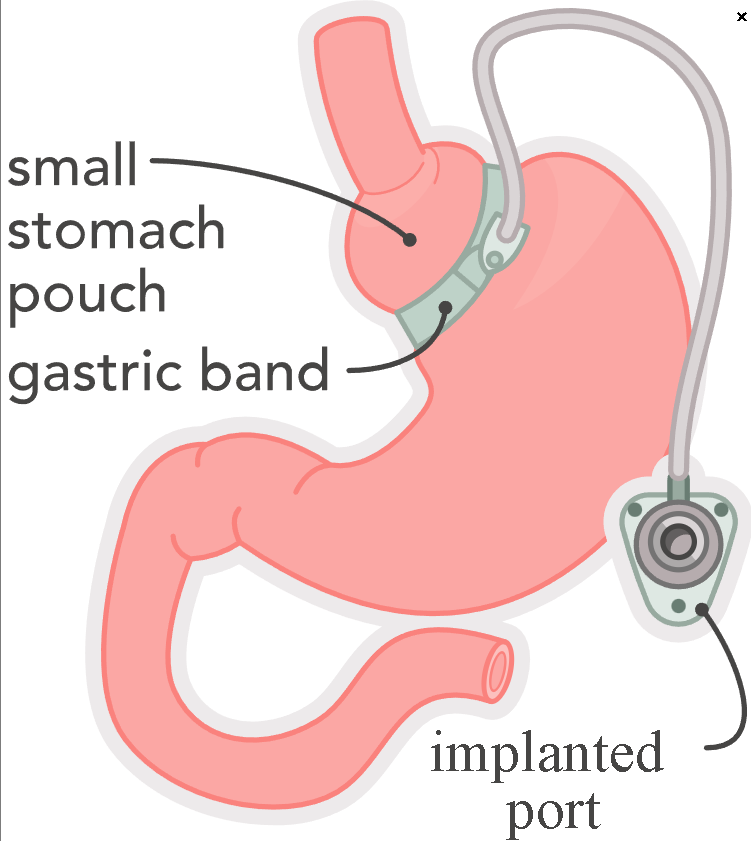
Gastric Banding
Adjustable band placed laparoscopically around upper stomach
Creates small pouch limiting food intake
Subcutaneous port allows band inflation or deflation
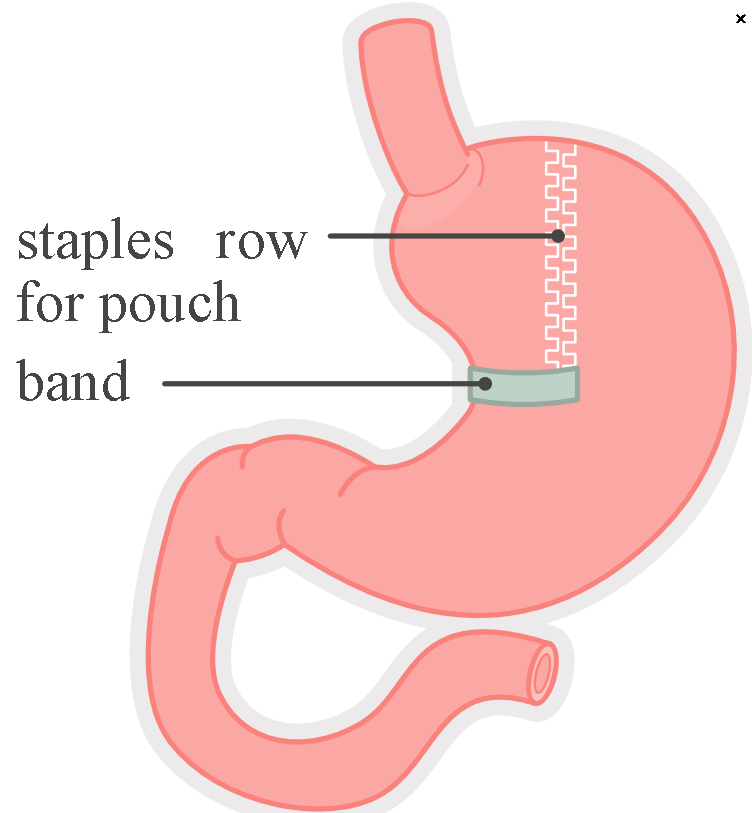
Vertical Banded Gastroplasty
Upper stomach stapled to form small pouch
Band slows gastric emptying
Sleeve Gastrectomy
Large portion of stomach removed
Creates narrow gastric sleeve
Performed open or laparoscopically
Malabsorptive Procedures
Combine restriction with bypass of small intestine.
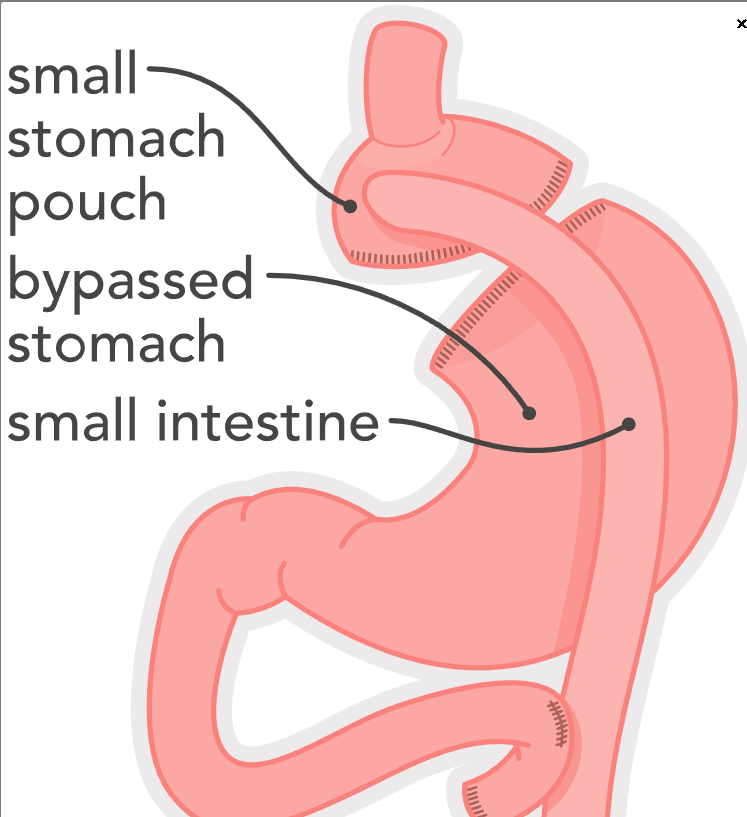
Gastric Bypass
Roux-en-Y (RYGB)
Small gastric pouch created
Jejunum attached directly to pouch
Food bypasses most of stomach and duodenum
Increased risk for dumping syndrome (loss of pyloric valve)
Often robotic-assisted or laparoscopic
Biliopancreatic Diversion with Duodenal Switch
Portion of stomach removed
Pouch attached directly to jejunum
High malabsorption risk
Bariatric Surgeries Care
Preprocedure Nursing Actions
Assess psychosocial factors and emotional relationship with food
Assess understanding of lifelong diet and lifestyle changes
Ensure bariatric equipment availability:
Proper bed, furniture, BP cuff size
Ensure adequate staff for transfers and ambulation
Use mechanical lift devices to prevent injury
Review labs:
CBC
Electrolytes
BUN, creatinine
HbA1c
Iron
Vitamin B12
Thiamine
Folate
Apply sequential compression devices (VTE prevention)
Postprocedure Nursing Actions
Monitor airway and oxygen saturation
Maintain semi-Fowler’s position (lung expansion)
NG tube care:
Do not reposition NG tube placed intraoperatively
Do not insert NG tube postoperatively
Monitor for complications:
Atelectasis
Thromboembolism
Skin breakdown
Incisional hernia
Peritonitis
Monitor bowel sounds and abdominal girth
Apply abdominal binder for open procedures
VTE prevention:
Early ambulation
Sequential compression devices
Low-molecular-weight heparin as prescribed
Fluid management:
Initially restricted, then gradually increased
Diet progression:
Clear liquids to full liquids
Discharge often on full liquid diet
Pureed foods after 1 week
Solid foods at 6–8 weeks
Four to six small meals per day
No liquids for 30 minutes after meals
Teach signs of dumping syndrome:
Cramping
Diarrhea
Tachycardia
Dizziness
Fatigue
Avoid empty-calorie, high-sugar foods
Coordinate long-term support with case management and mental health services
Client Education
Follow prescribed diet consistency and volume (often ≤ 240 mL per meal)
Avoid carbonated beverages
Walk daily at least 30 minutes
Use physical therapy guidance as needed
Remain in low-Fowler’s position for 20–30 minutes after meals (slows gastric emptying)
Bariatric Surgeries Complications
Anastomotic Leak
Common and life-threatening complication after gastric bypass
Report immediately if:
Increasing abdominal, back, or shoulder pain
Restlessness
Tachycardia
Oliguria
Dehydration
Indicators:
Excessive thirst
Concentrated urine
Goal fluid intake ≥ 1.5 L/day
Notify provider if signs present
Malabsorption and Malnutrition
Caused by reduced stomach size or intestinal bypass
Common deficiencies:
Vitamin B12
Vitamin D
Thiamine
Calcium
Iron
Folate
Nursing Actions for Malnutrition
Monitor tolerance of food and fluids
Refer to dietitian
Encourage low-Fowler’s position during and after meals
Client Education for Malnutrition
Protein intake often 60–80 g/day
Eat nutrient-dense foods only
Avoid empty calories and excess carbohydrates
Lifelong vitamin and mineral supplementation required
A nurse is reviewing the actions of bariatric medications and devices with a client who is obese and seeking information about weight loss. Match each action to the medication or device it describes.
Absorbs water to decrease stomach capacity
Suppresses appetite and decreases cravings
Increases satiety with placement of an expandable device filled with saline
Inhibits digestion of fats by blocking lipases
Intragastric balloon
Hydrogel pill device
Orlistat
Naltrexone-bupropion
Intragastric balloon
Increases satiety with placement of an expandable device filled with saline
Hydrogel pill device
Absorbs water to decrease stomach capacity
Orlistat
Inhibits digestion of fats by blocking lipases
Naltrexone-bupropion
Suppresses appetite and decreases cravings
Adjustable Band Gastroplasty (image)
Vertical Banded Gastroplasty (image)
Roux-en-Y Gastric Bypass
A nurse is planning care for clients who have had bariatric surgery. Sort the procedures by whether they are categorized as restrictive or malabsorptive surgeries.
Gastric banding
Roux-en-Y
Sleeve gastrectomy
Vertical banded gastroplasty
Biliopancreatic diversion with duodenal switch
Restrictive
Malabsorptive
Restrictive
Gastric banding
Sleeve gastrectomy
Vertical banded gastroplasty
Malabsorptive
Biliopancreatic diversion with duodenal switch
Roux-en-Y
Although Roux-en-y and biliopancreatic diversion with duodenal switch are surgeries that also create decreased capacity, they are considered malabsorptive because they bypass part of the small intestine to reduce absorption of nutrient
A nurse is providing discharge teaching to a client who had gastric bypass surgery. Which of the following statements by the client indicates understanding of the instructions?
Select all that apply.
a
“I should start to eat solid foods 2 weeks after surgery.”
b
“I should expect very little urine output for the first 2 weeks.”
c
“The most serious complication I can expect is vomiting.”
d
“The amount of refined carbohydrates in my diet should be limited.”
e
“I should drink at least 1.5 liters of water each day.”
f
“After a meal, I should wait for 30 minutes to drink liquids.”
d
“The amount of refined carbohydrates in my diet should be limited.”
e
“I should drink at least 1.5 liters of water each day.”
f
“After a meal, I should wait for 30 minutes to drink liquids.”
Following a gastric bypass surgery, high intake of refined carbohydrates increases the risk for dumping syndrome. Ensuring adequate water intake decreases the risks of dehydration that can be caused by vomiting or diarrhea. Delaying intake of liquids for at least 30 minutes following a meal of solid foods decreases the risk for dumping syndrome.