MD-2 Influenza and Vaccination
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
51 Terms
What family is the influenza virus part of?
Orthomyxovirus
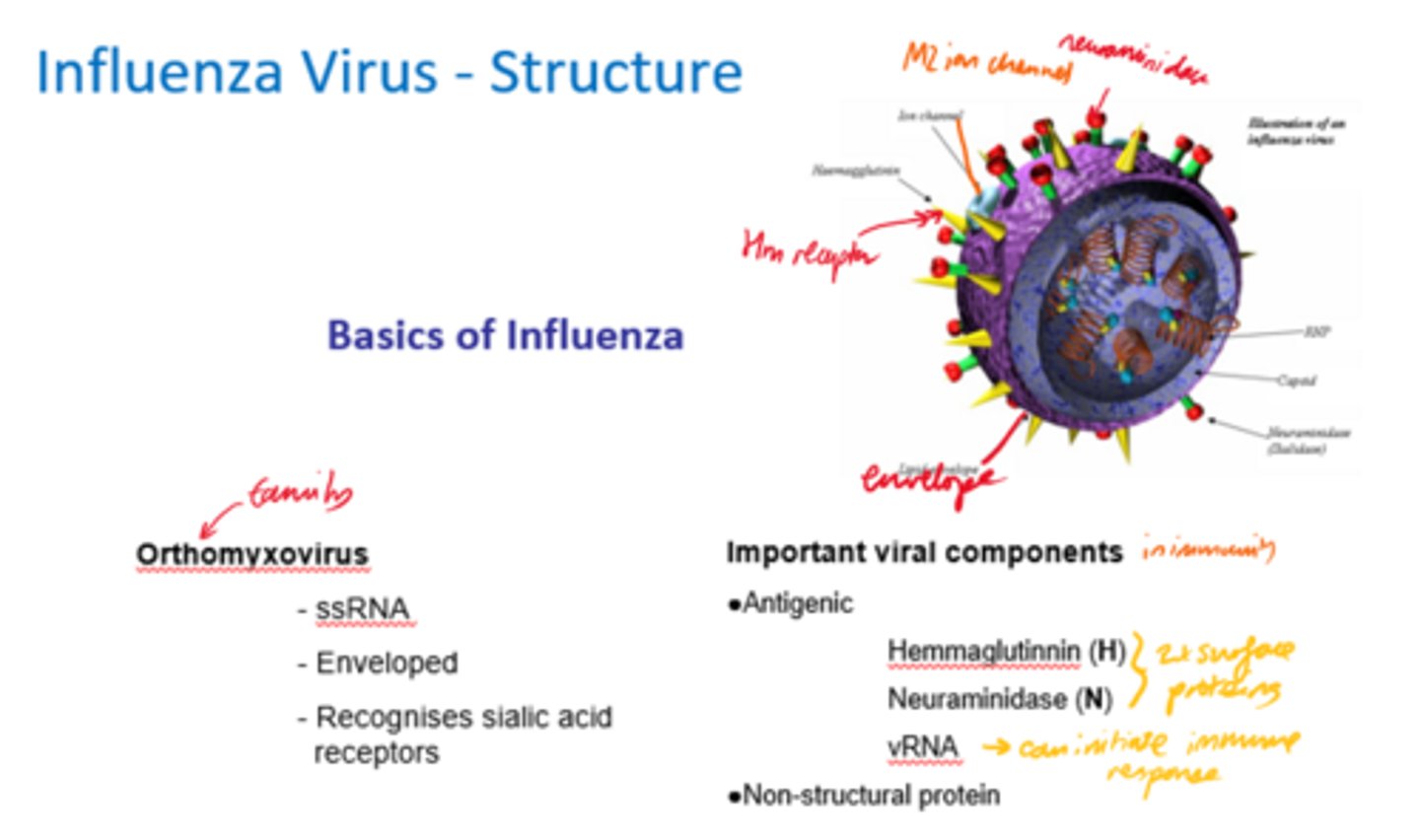
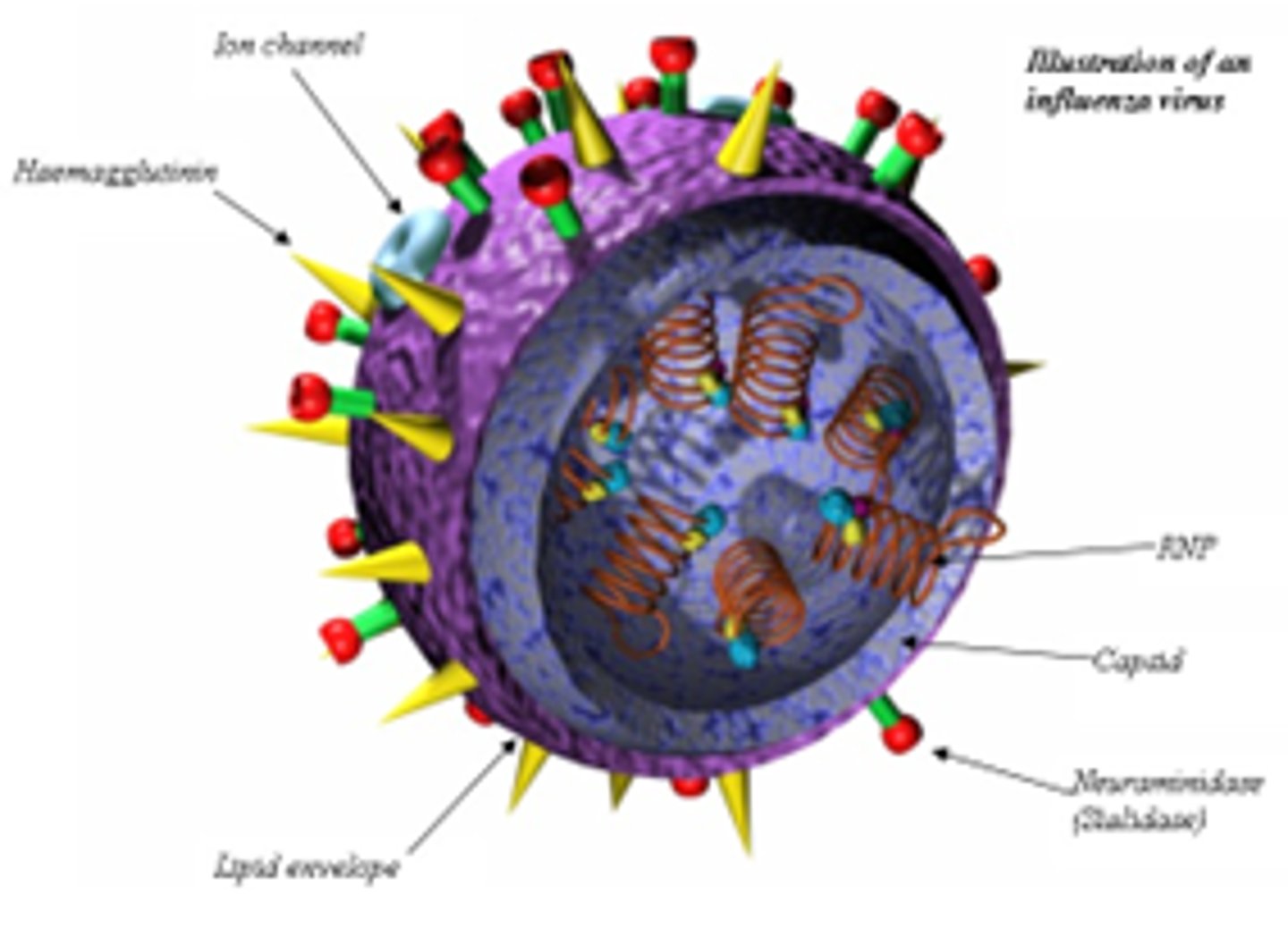
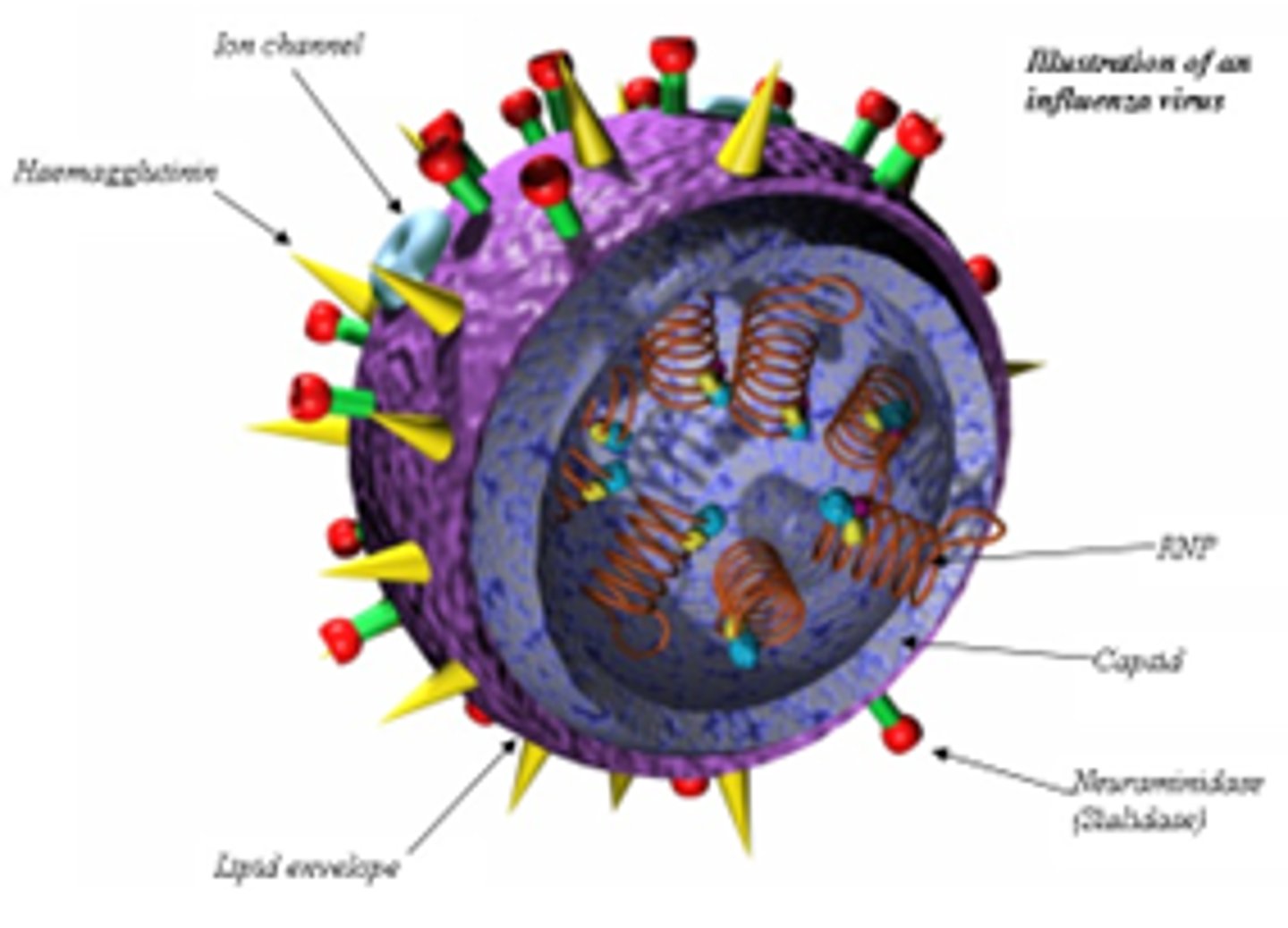
Describe the structure of orthomyxovirus.
What receptors does it recognise?
- ssRNA.
- Envelope.
- Recognises sialic acid receptors.
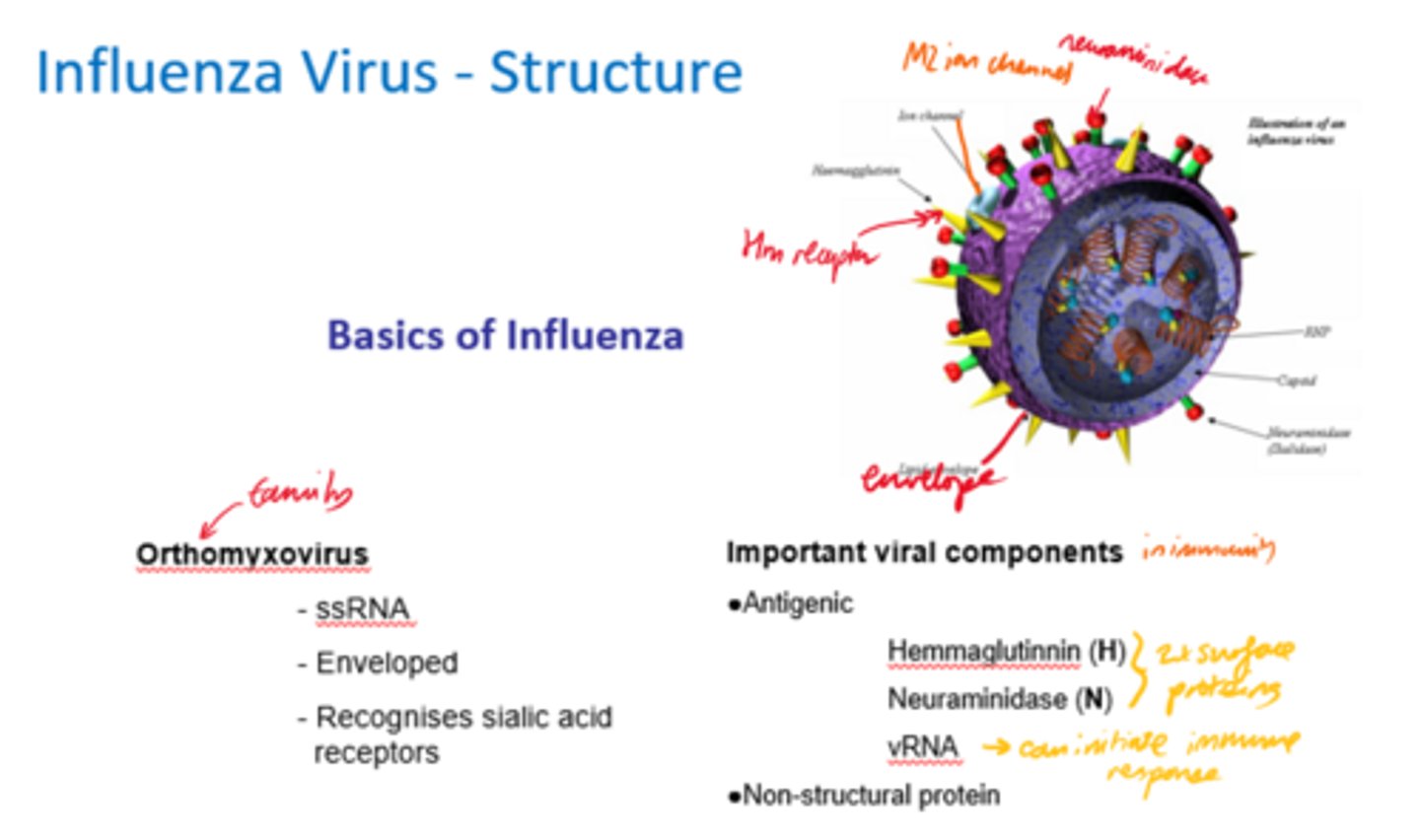
What are the important viral components of influenza for immunity?
- Haemaglutinin (H).
- Neuraminidase (N).
- vRNA.
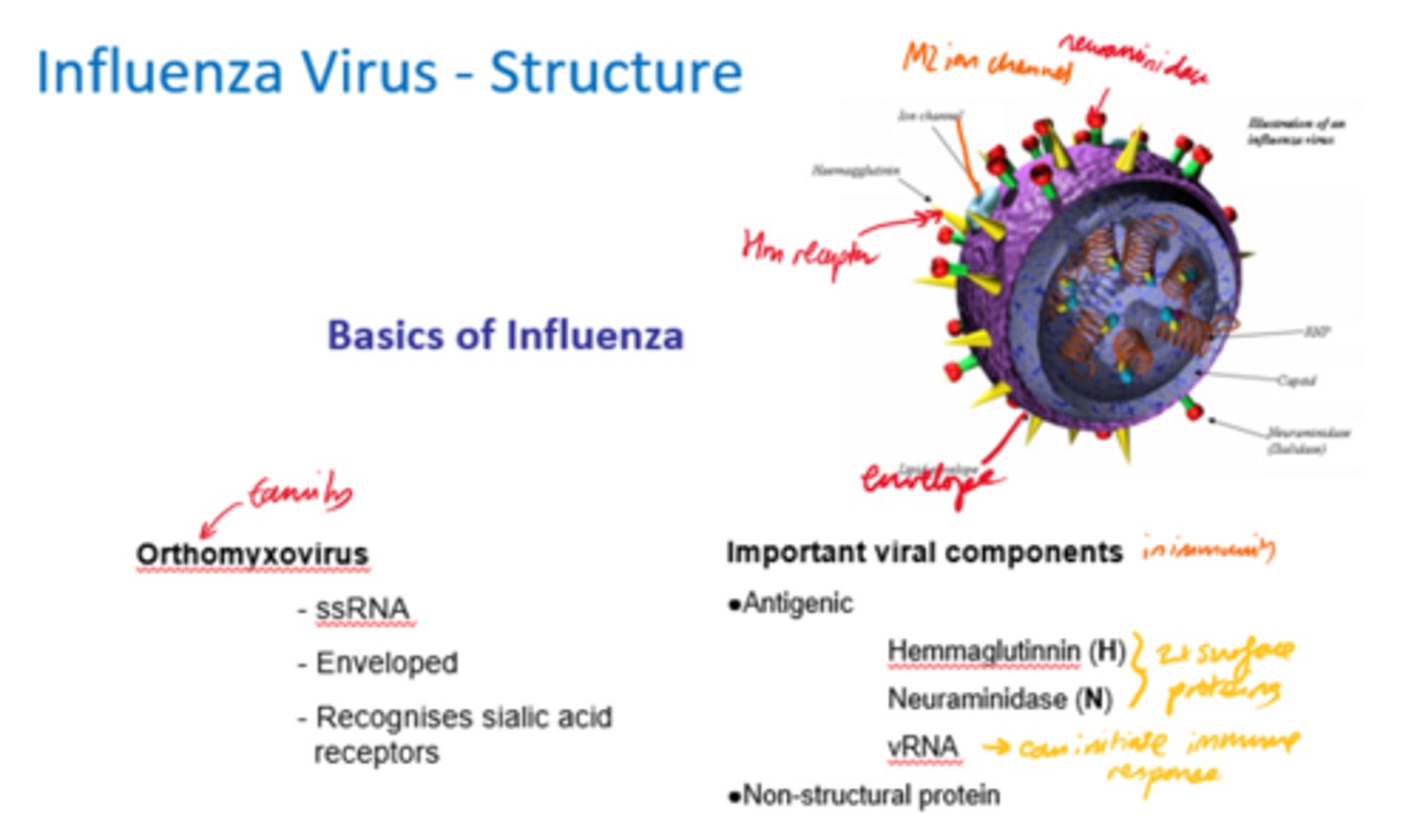
What are the 3x main surface proteins in influenza viruses?
- Haemagglutinin (HA).
- Neuraminidase (NA).
- M2.
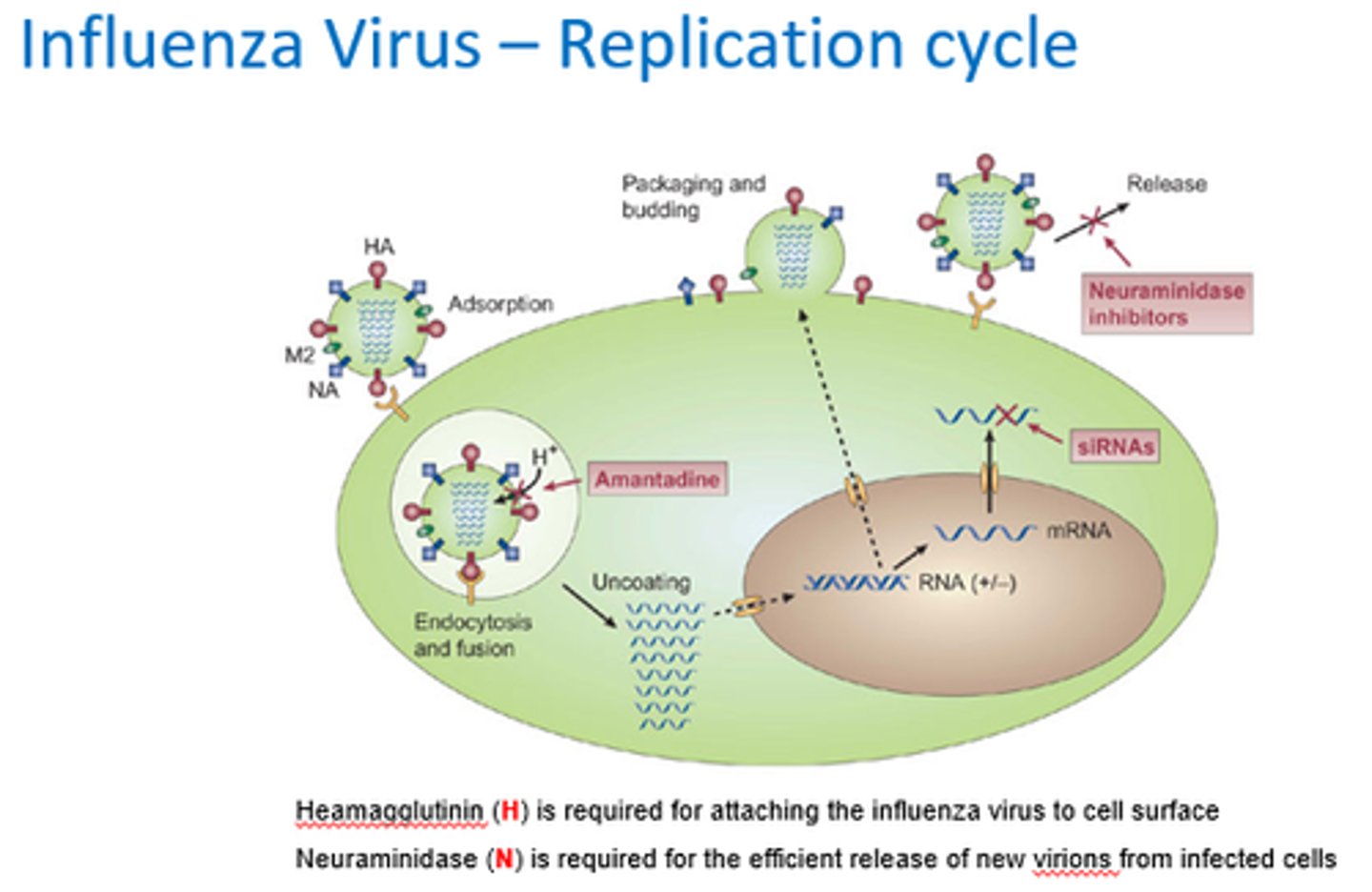
What is the function of haemagglutinin?
Functions in attachment and penetration at start of replication cycle.
What is the receptor for haemagglutinin?
Siaclic acid receptor - terminal carb on cell glycoproteins, so can be recognised by HA.
What is neuraminidase (NA)?
- Enzyme that cleaves sialic acid from glycoconjugates.
What does neuraminidase enzyme do?
- Cleaves receptor off cell surface allowing new particle to be released.
- Facilitates elution of pyrogeny virions from infected cells.
- Works at end of replication cycle.
What does M2 channel protein do?
- Uncoating and virus maturation.
- Allows pH drop (protons migrate in).
- Allows ssRNA to be released into cytoplasm (passed into nucleus and prcessed).
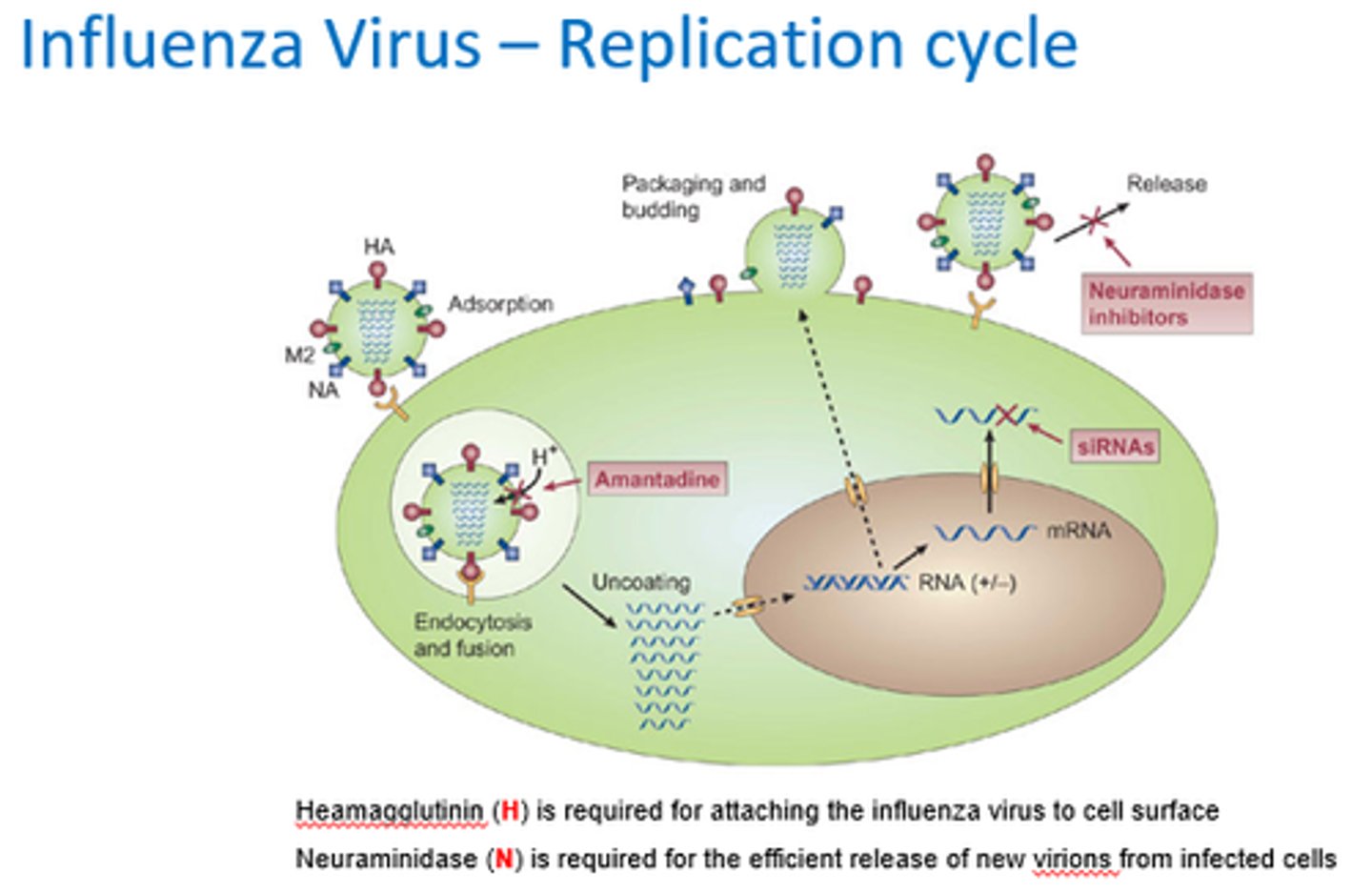
What is Haemagglutinin required for?
Attaching influenza virus to cell surface.
What is neuraminidase required for?
Release of new virions from infected cells.
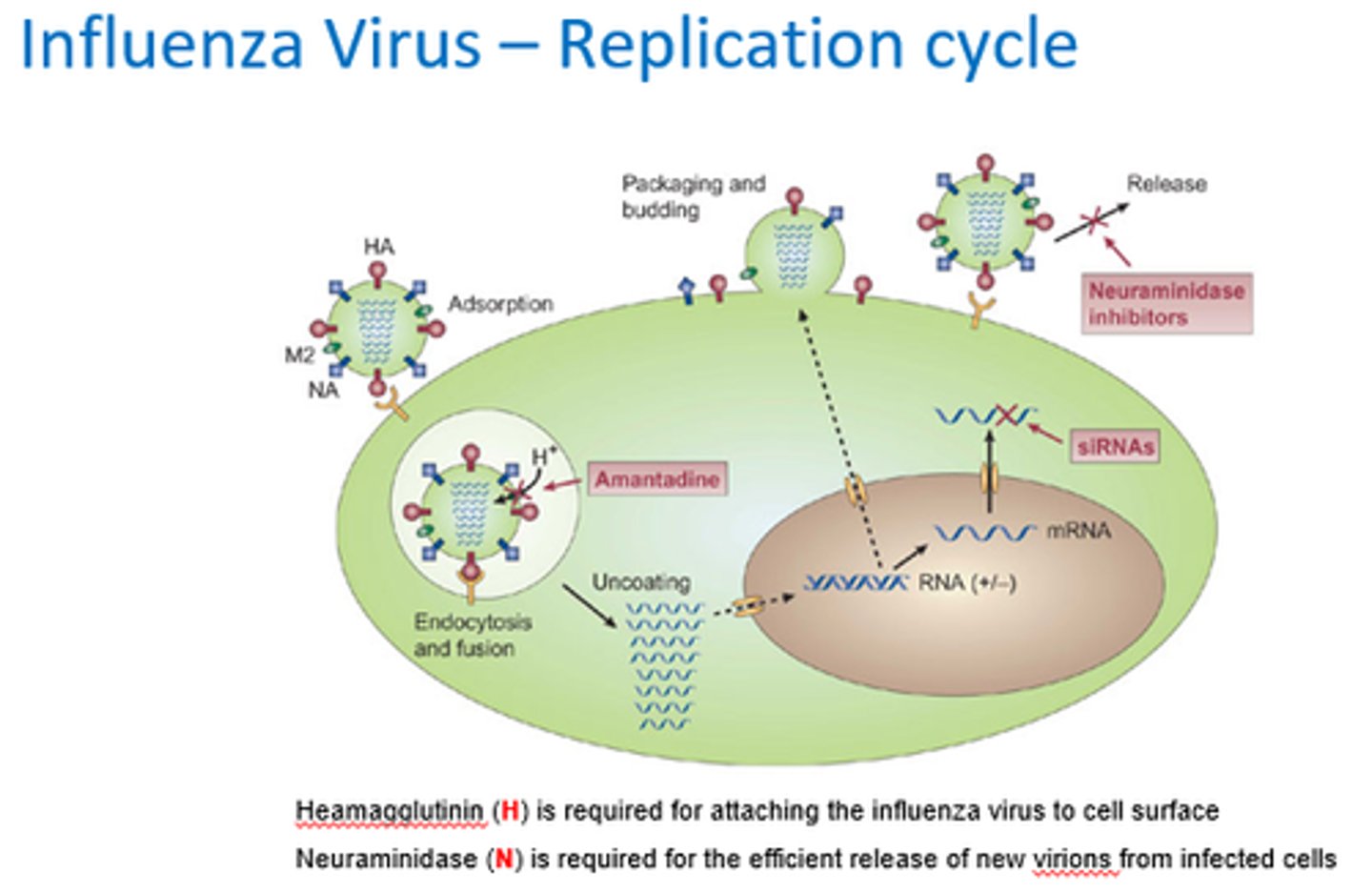
When is haemagglutinin required in the replication cycle?
At the beginning to promote binding an internalisation
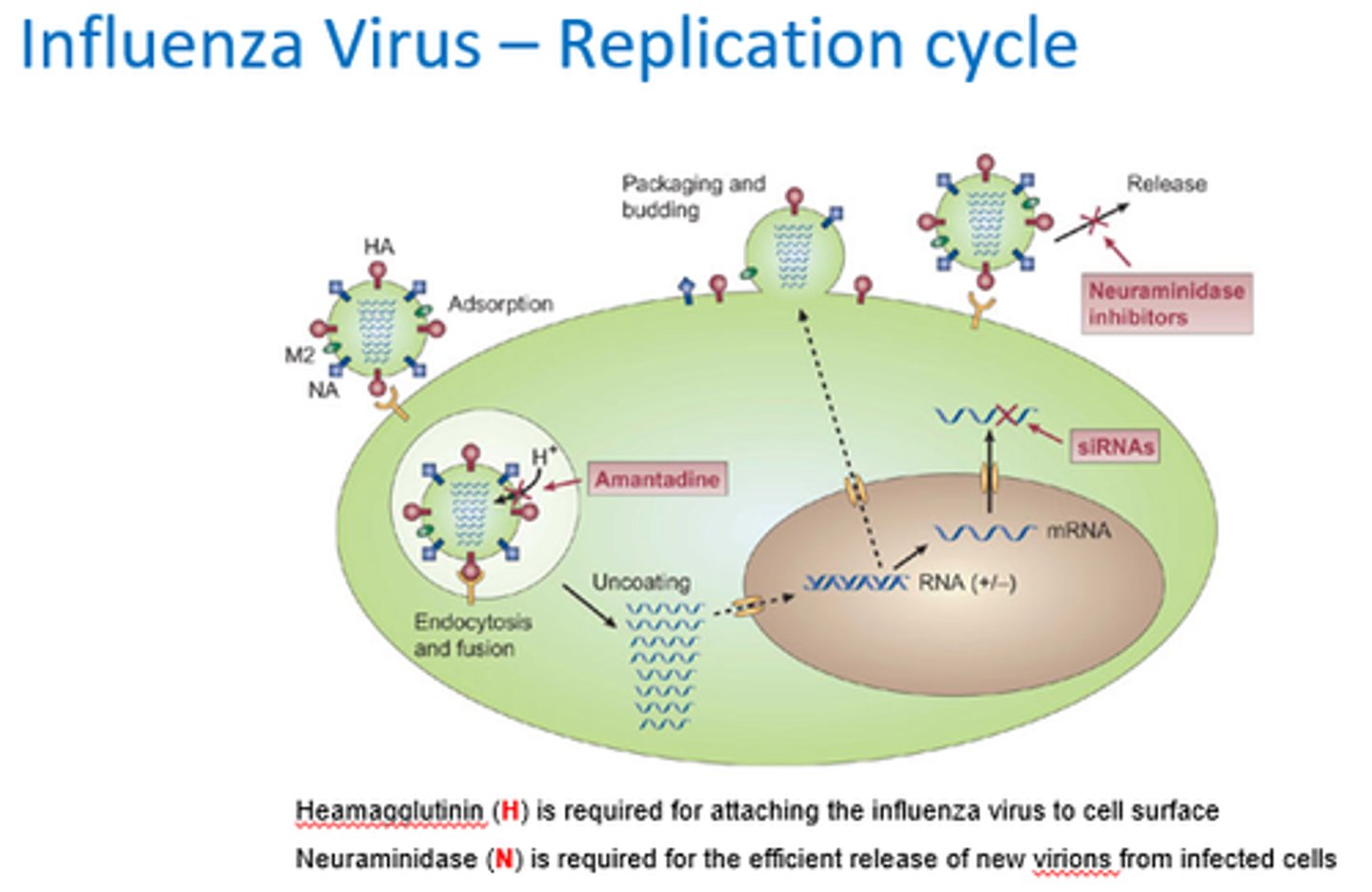
When is neuraminidase required in the replication cycle?
At the end to allow new particles to be released into circulation.
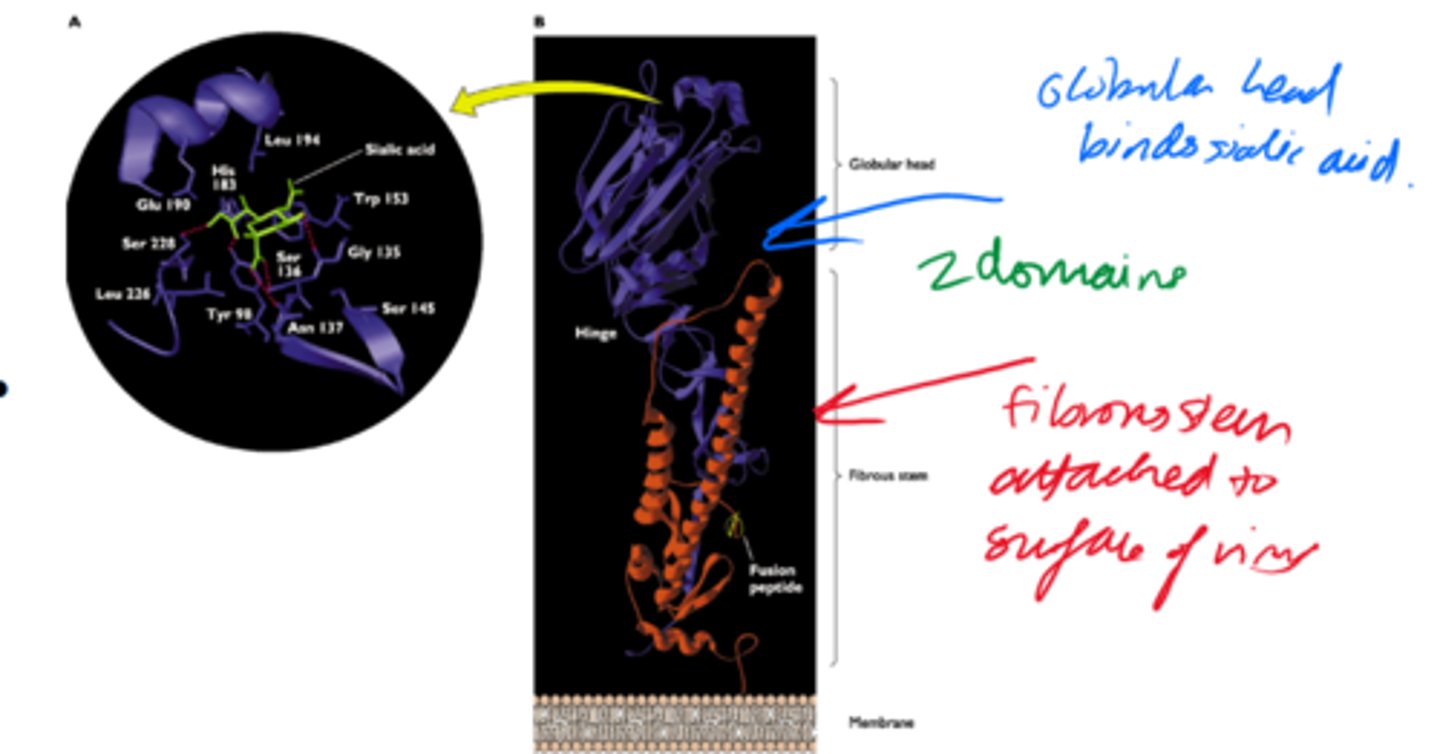
Describe the structure of Haemagglutinin protein.
2x domains:
- Globular head.
- Fibrous stem.
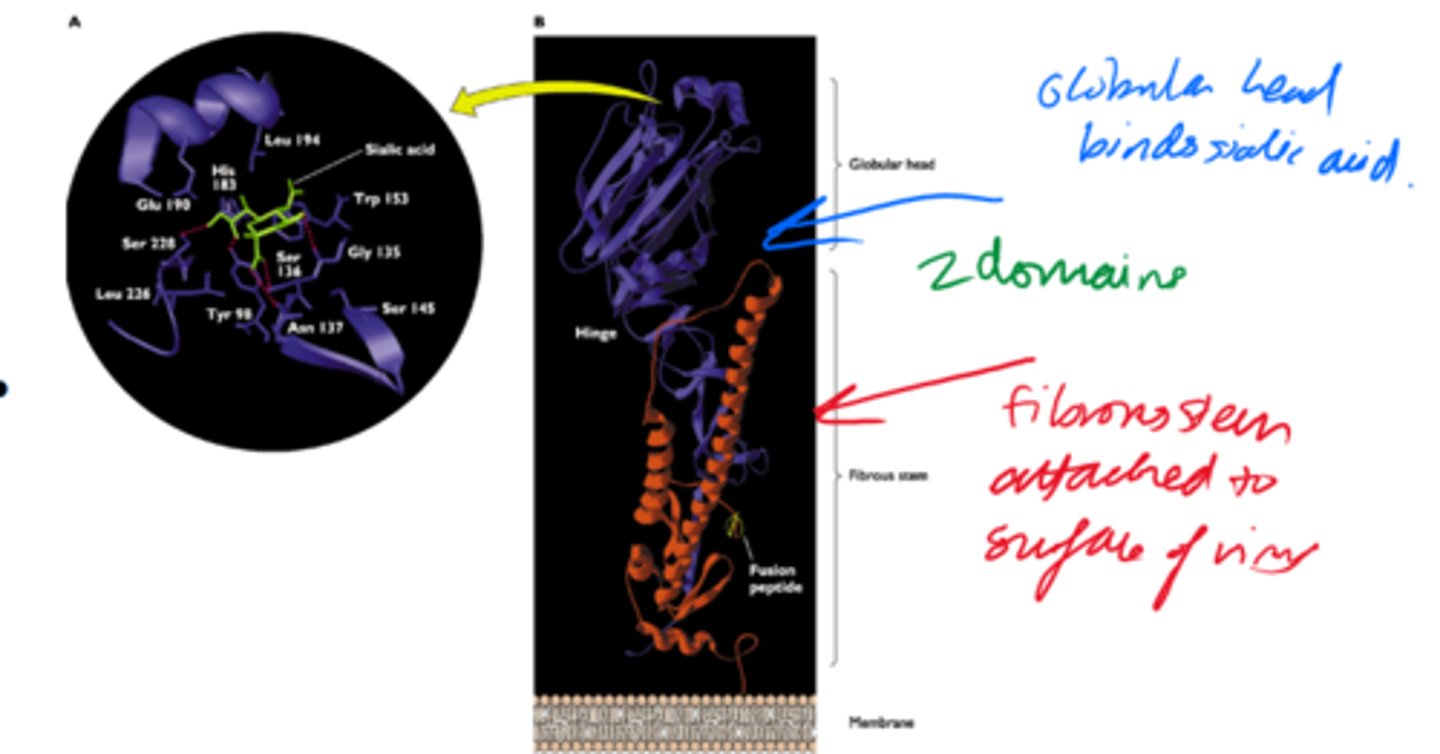
What is the role of the globular head of haemagglutinin?
- Binds to cell surface receptor sialic acid.
- Changes its shape to promote endocytosis into host cell.
What is neuraminidase?
An enzyme that acts at the end of replication to hydrolyses the sialic acid receptor on the cell surface.
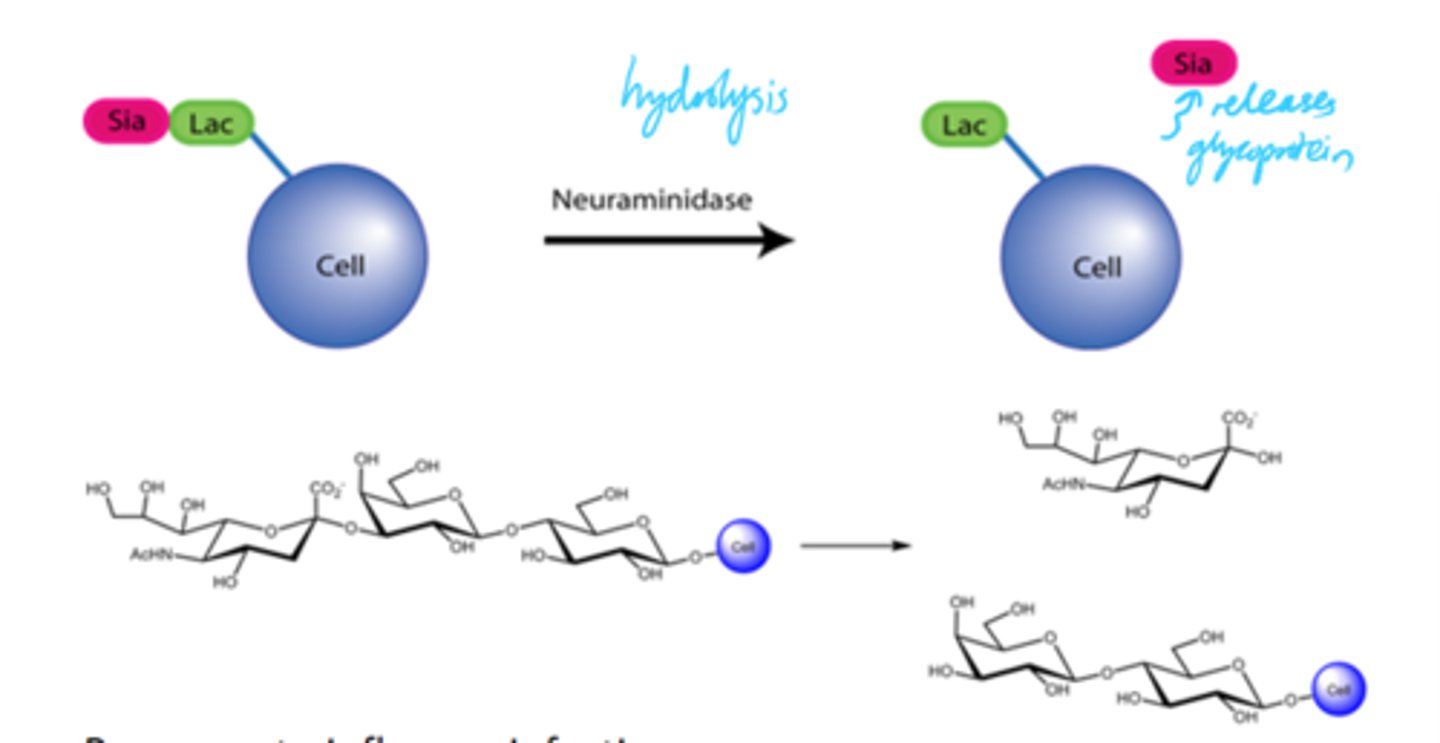
What does it mean when the sialic acid is removed from the receptor by neuraminidase?
The haemagglutinin protein no longer binds.
What is the inital response of the body to an influenza infection?
Non-specific, pro-inflammatory innate response.
What does NFKB transcription lead to?
Pro-inflammatory cytokine gene expression of TNFa, IFNb and IL-8
How do chemokines and cytokines produced increase inflammatory response?
By attracting NK, B and T cells to infection site.
Describe the long term response to influenza infection.
- IFNy boosts chemokine gene expression, macrophage activation, antigen presentation and specific cell-mediated immunity.
- Th2 response.
- T cell stimulation.
- Antigen presentation.
- B cell maturation.
- Antigen-specific IgG production.
What gives long term protection against similar strains of influenza?
Antigen-specific IgG production
How many types of influenza viruses are there and how are they referred to?
4 - A,B,C,D
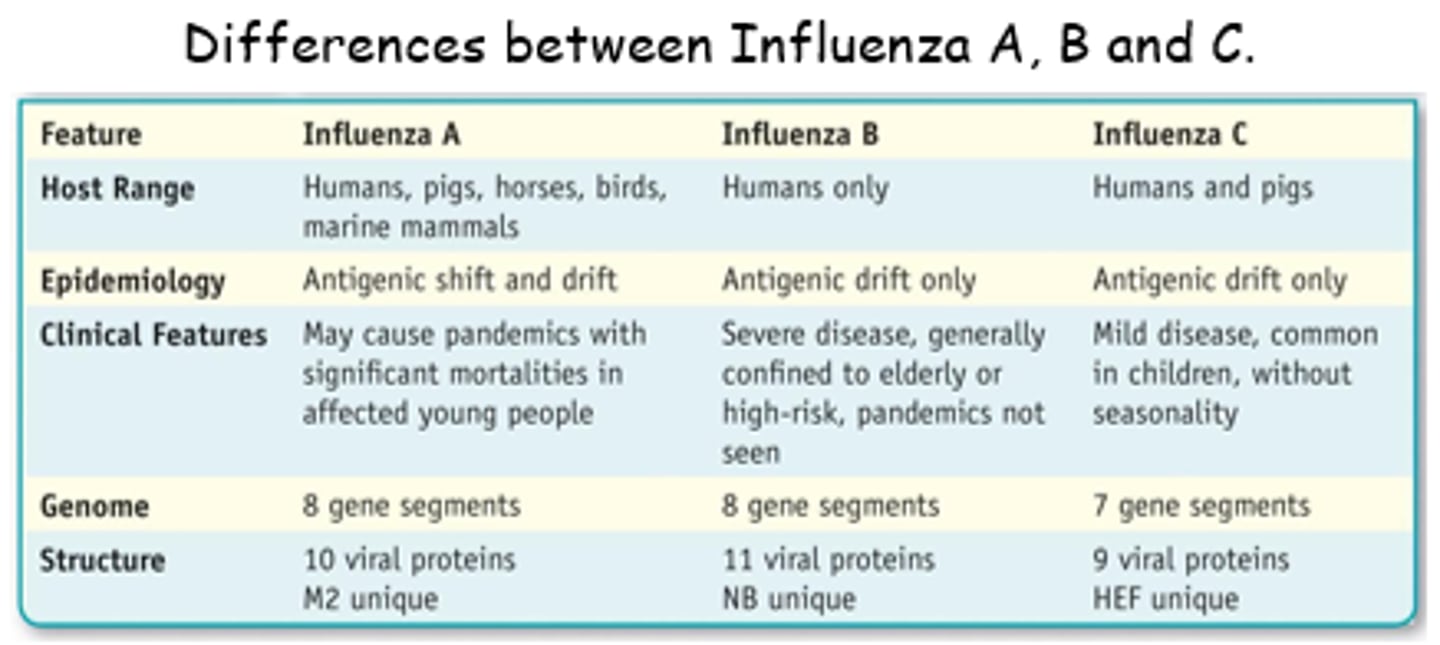
Which types of influenza viruses cause seasonal epidemics?
Human influenza A and B viruses
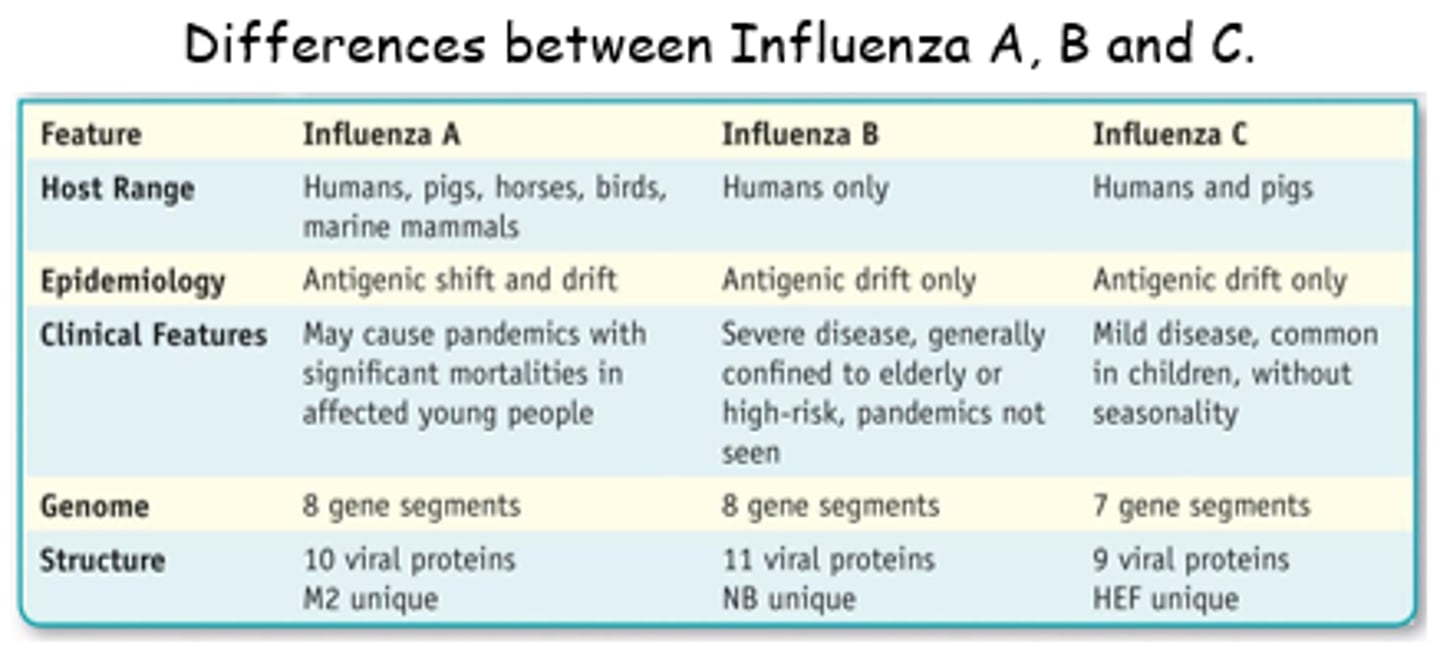
What do influenza C viruses do?
- Cause mild respiratory illness.
- Not thought to cause epidemics.
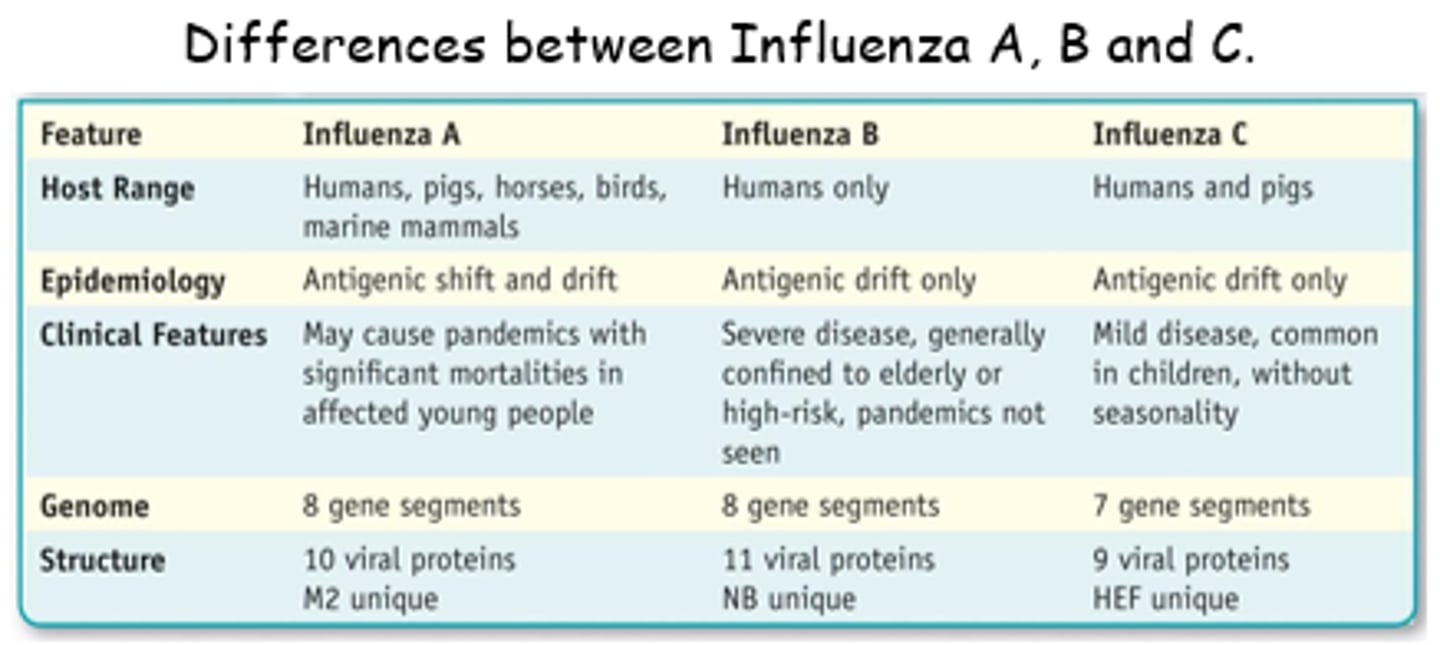
What do influenza D viruses affect?
Cattle - not know to infect people.
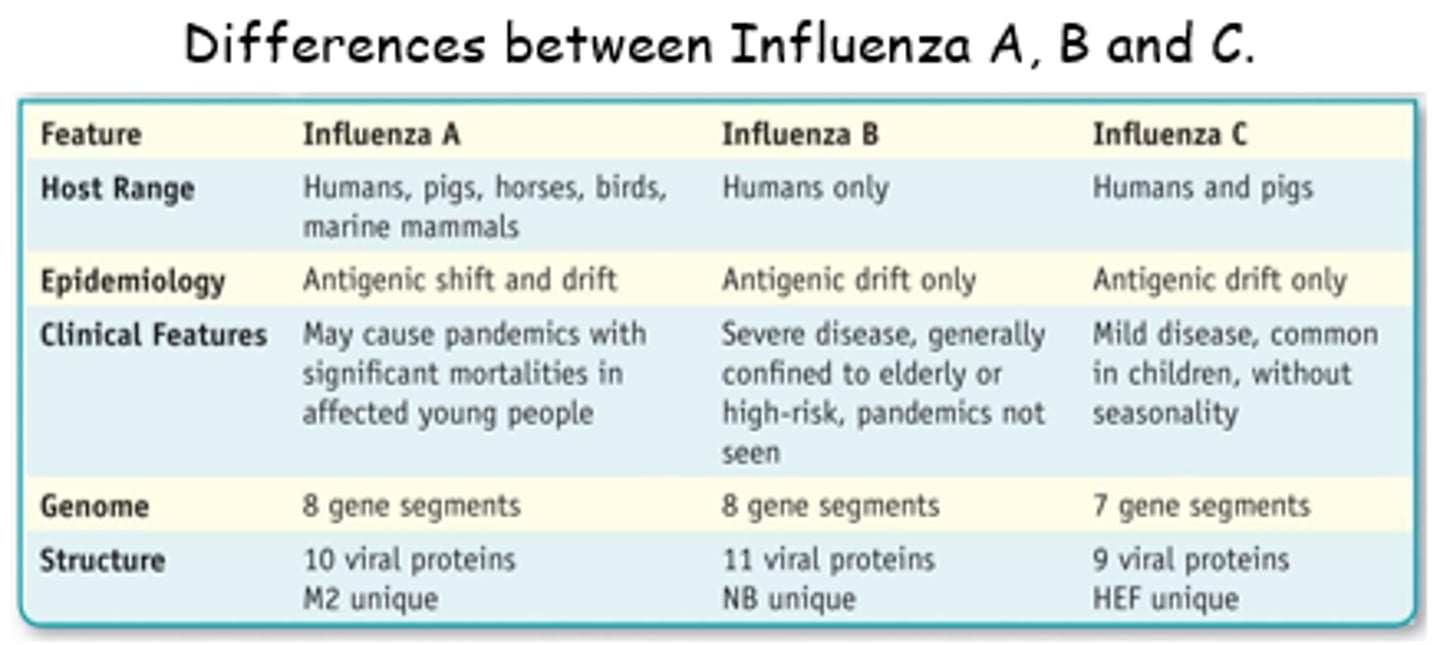
How are influenza A subtypes divided?
Based on 2x surface proteins on the virus - haemagglutinin and neuraminidase.
How many different subtypes of haemagglutinin and neuraminidase subtypes are there?
Haemagglutinin - 18 subtypes (H1-H18).
Neuraminidase - 11 subtypes (N1-N11).
What will an IgG antibody only recognise?
IgG antibodies will only recognise the ONE sub-type of H or N it was generated agianst.
What are the current subtypes of influenza A viruses found in people?
Influenza A (H1N1) and influenza A (H3N2) viruses.
What is Antigenic drift?
Gradual accumulation of amino acid mutations that allow haemagglutinin to escape neutralising antibodies.
What happens if a mutation (from antigenic drift) is close to an antibody binding site?
IgG antibodies won't bind as tightly/strongly
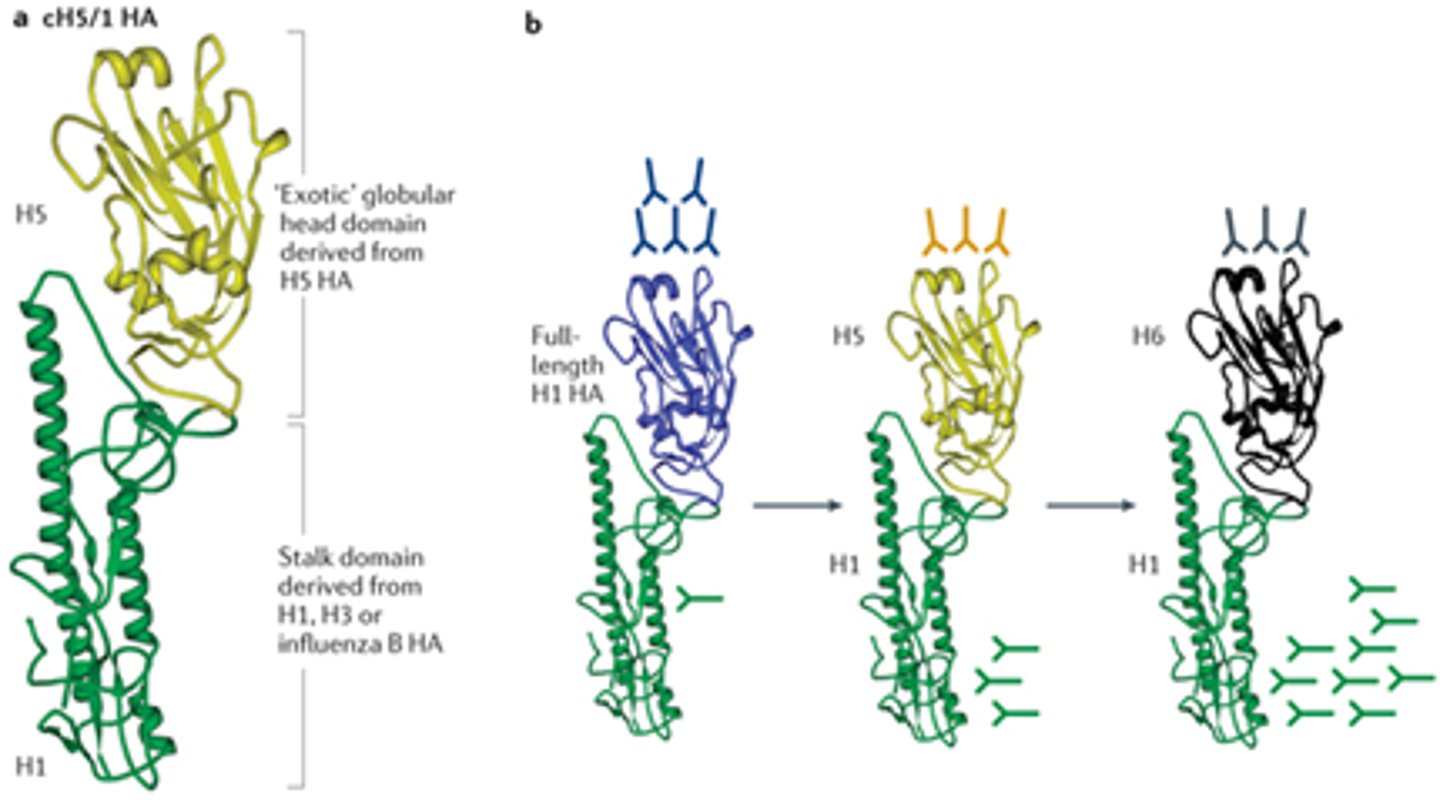
What are epidemic strains of influenza thought to have changes in?
Three or more antigenic sites
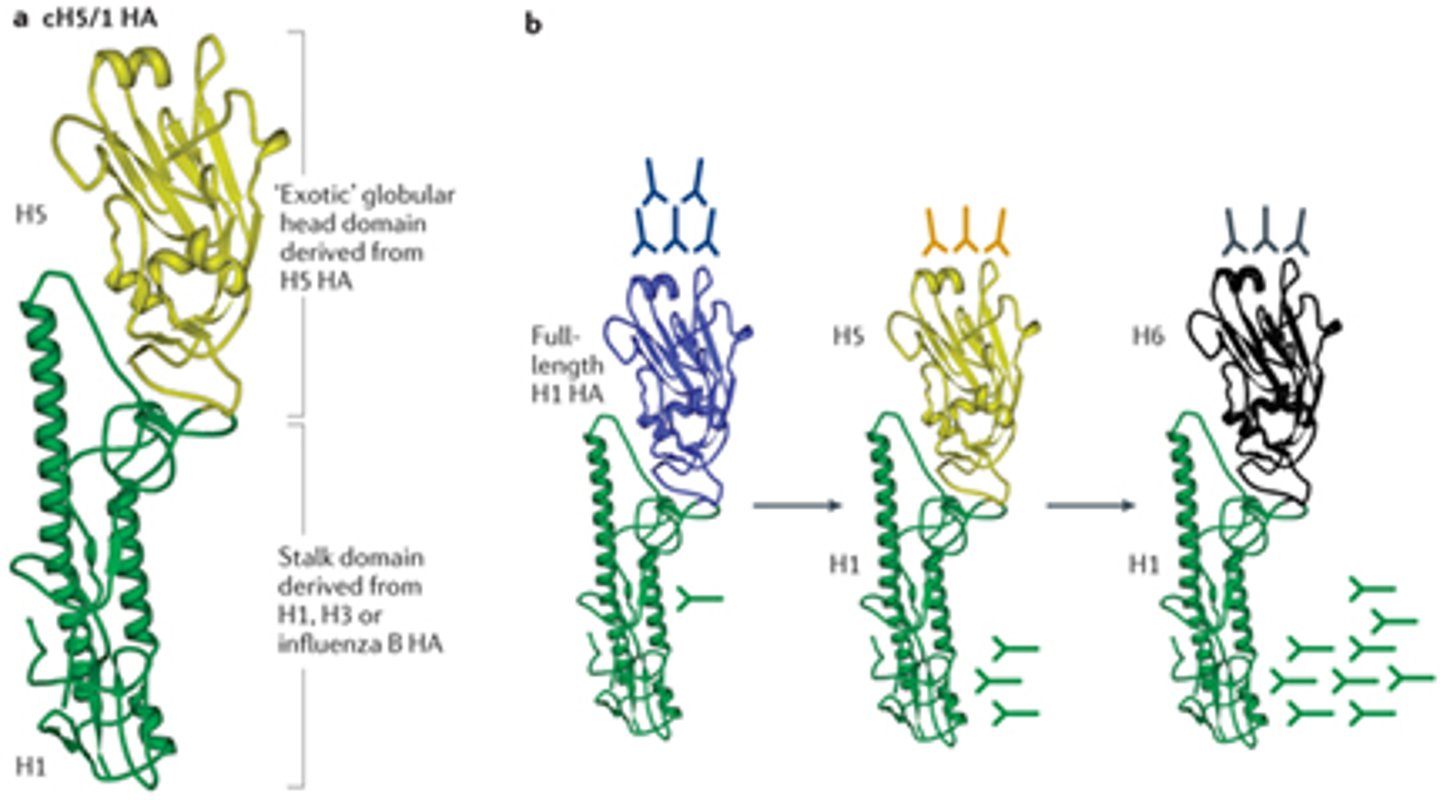
What does antigenic drift result in?
Reduced ability of circulating antibodies to recognise the 'new' virus.
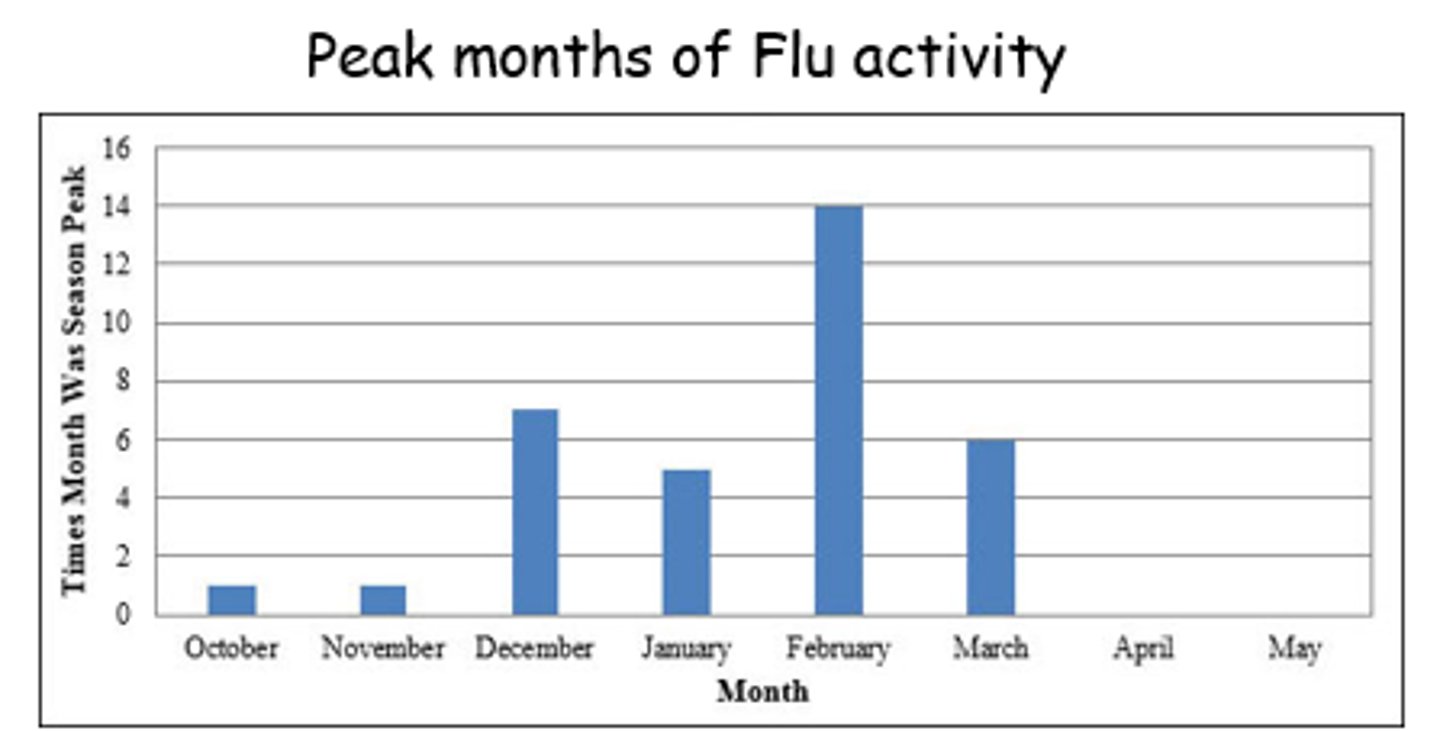
What are the peak months of flu activity?
October to Feb
What type of vaccines are influenza vaccines normally?
Inactivated
How are influenza vaccines produced?
- Grow virus in culture media.
- Inactivate it with heat/chemicals (eg formalin).
What are some pros of inactivated flu vaccines?
- Not alive and can't replicate.
- Entire dose given in one injection.
- Can't cause disease.
- Generally safer.
- Improved stability so easier to rapidly distribute.
What are some disadvantages to inactivated flu vaccines?
- Can be costly.
- Hypersensitivity.
- 1st dose doesn't give protective immunity, but only primes the immune system.
- Needs 2nd/3rd dose for protective immune response.
What does valency refer to?
The no of strains in the vaccine.
What is a standard influenza vaccine (how many strains)?
Trivaleted Inactivated Vaccine (TIV).
How is a flu jab normally administered?
As an intramuscular (IM) injection.
What are some challenges to flu vaccine production techniques (egg propagation)?
- Time consuming.
- Expensive.
- Incompatible w/propagating high pathogenic avian influenza strains.

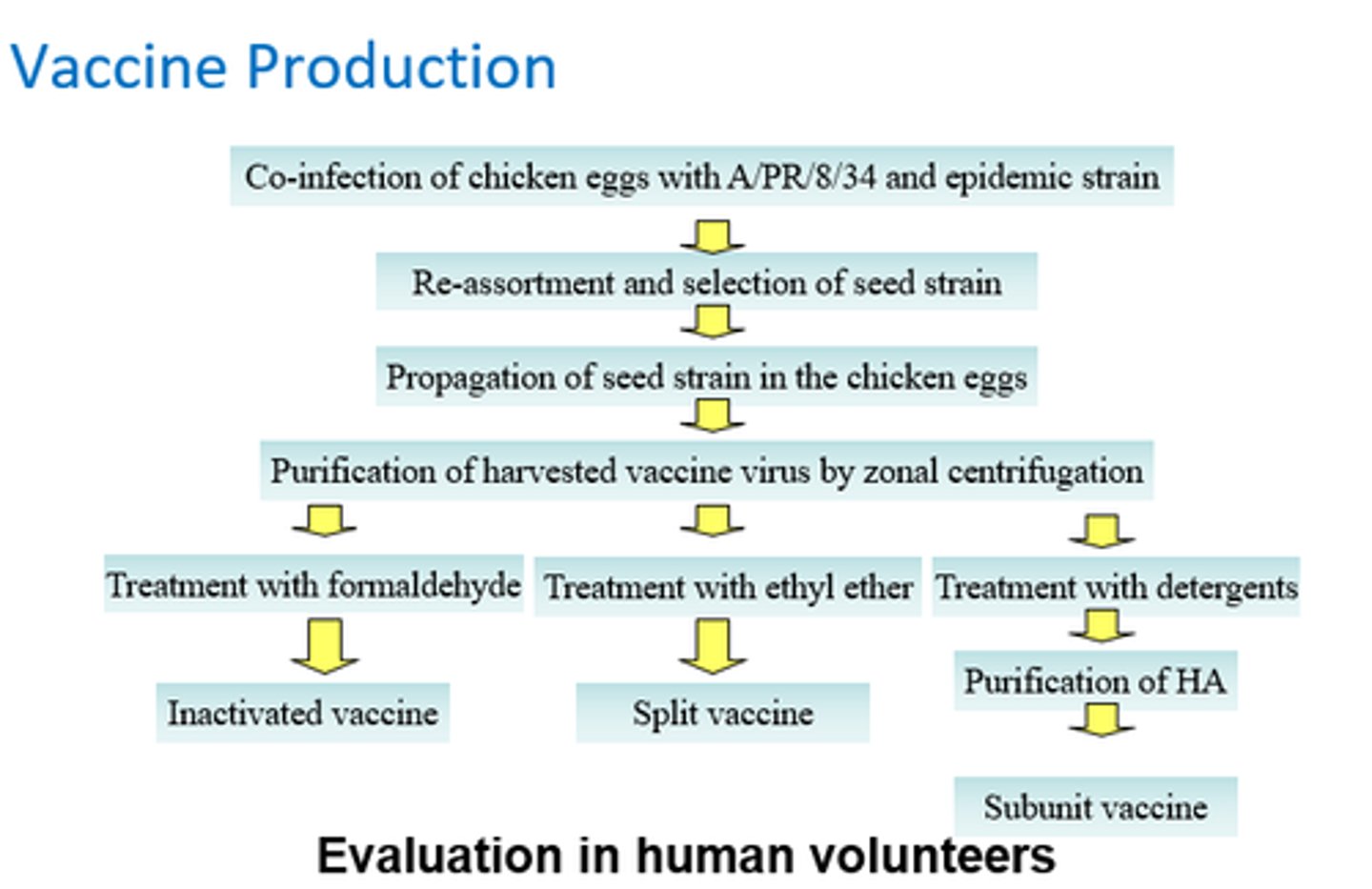
Describe vaccine production stages for an inactivated vaccine.
- Co-infection of chicken eggs w/ strains.
- Reassortment and selection of seed strain.
- Propagation of seed strain in chicken eggs.
- Purification of vaccine virus by zonal centrifugation.
- Tx w/ formaldehyde.
= inactivated vaccine!
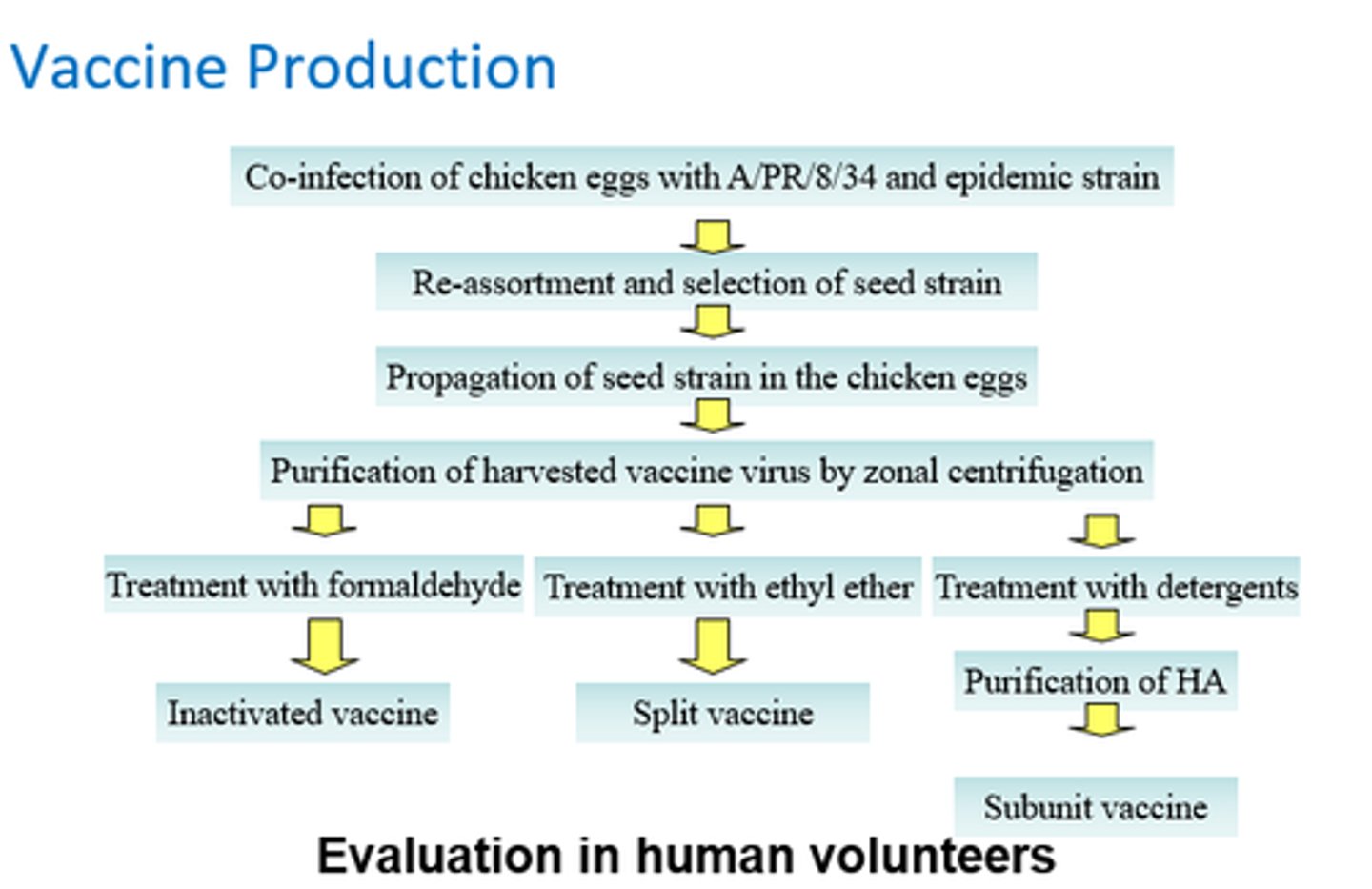
Simply describe the vaccine production process for flu.
- Co-infect egg w/standard and epidemic strains of flu virus.
- vRNA can mix up between 2x strains, so we can create a new combination strain.
- Seed virus is used to infect other eggs and grow larger amounts.
- Complete process for each of 3/4 new strains predicted.
What are the critical factors for influenza vaccine production?
- Growth potential of seed virus.
- Timing of strain selection.
- Potency test reagents.
- Timing of annual license supplement approval.
Growth potential of seed virus:
What is the quantity of Trivalent Influenza Vaccine that can be produced limited by?
The least productive monovalent strain
Why is timing of strain selection tricky when trying to make the annual fla vaccine?
- Production time limited due to necessity of distribution of vaccine prior to flu season.
- Don't want to guess the wrong strain, so we hold off as poss to get enough data.
- Working seeds need at least 4 weeks for development.
Why are potency test reagents required in flu vaccine production?
- To determine potency of monovalent compounds before vaccine formulation.
- Test potency of each strain.
- Must be standardised for new strains.
Why is an annual license supplement approval needed?
- Bypasses MHRA licensing agreement as needed annually, so quick production essential. (*)
- Required to begin packaging process.
Give an example of an alternative influenza vaccine.
- Flu-Mist - nasal spray vaccine.
- Live-attenuated.
- Propagated by infection of cells in culture and then manufactured in eggs.
