Transfusion medicine
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
How do you know if a patient needs a blood transfusion?
Based on clinical signs
Signs suggestive of reduced oxygen provision to tissues —> tachycardia, tachypnoea, lethargy, weakness etc.
Ensure patients are normovolaemic before deciding whether to transfuse
Generally looking at PCV of 10-15% for cats and 15-20% for dogs
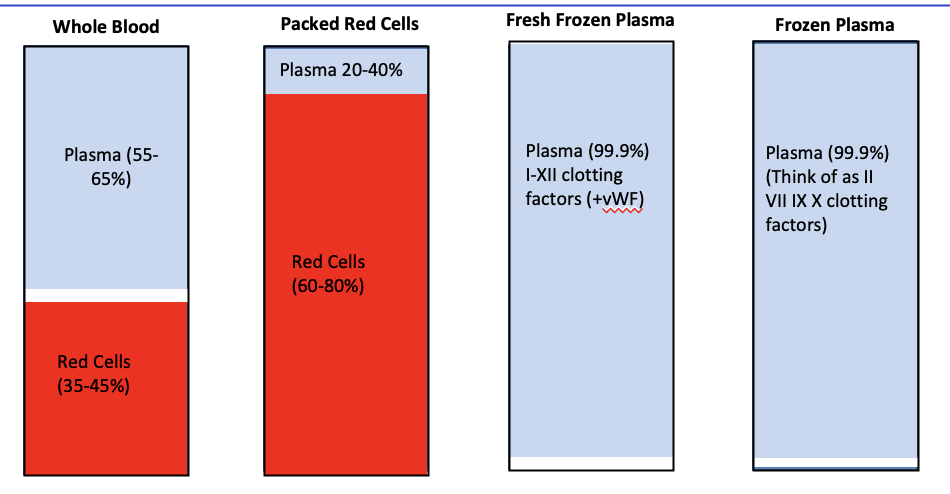
Which blood products can be used for blood transfusion?
Replace 'like with like'
Blood loss —> replace with whole blood or if not available, packed red cells e.g. crystalloid fluid therapy
Haemolysis —> Replace with packed red cells
Coagulopathy —> Replace with fresh frozen plasma, regular plasma or cryoprecipitate depending on cause
Why do we need to blood type patients?
Will influence blood type of blood product
Ideally give type-matched blood to dogs
If unable to blood type dog, administer DEA 1 negative blood to dogs
Imperative to give type-matched blood to cats
Not strictly necessary for admin of plasma products
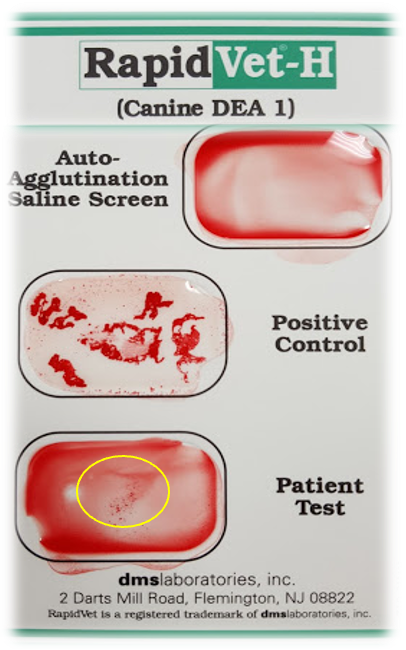
What system is used to classify dogs blood types
Based on Dog Erythrocyte Antigen system
One we care about most is DEA 1 blood type- most antigenic
So dog can either be DEA 1 -ve or DEA +ve
Dogs do not have naturally occurring antibodies only develop them following tranfusion- may have acute haemolytic reaction if exposed subsequently
What happens if we give a dog the wrong DEA 1 type blood?
A DEA 1 –ve dog receiving DEA 1 +ve blood will have a very mild, delayed reaction
A DEA 1 +ve dog receiving DEA 1-ve blood will not demonstrate any signs
First transfusion usually 'free'
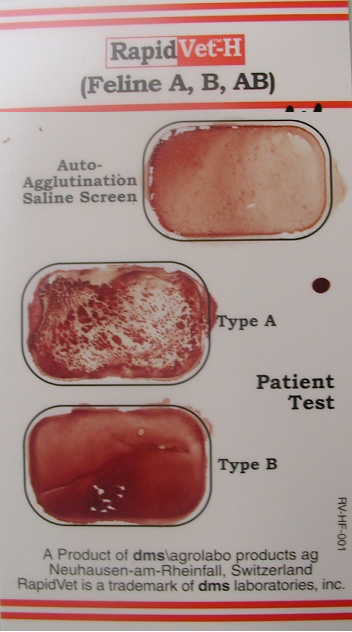
What is the feline blood type system?
Based on A/B system with A being dominant to B and AB being polygenic
Cats have naturally occurring antibodies
Imperative to give type-matched blood as can have fatal acute haemolytic reactions with wrong type
What happens if we give cats the wrong type of blood?
Giving B cats type A blood is BAD → severe acute haemolytic reaction
Giving A cats type B blood is not As Bad → milder, delayed reaction
How can you blood type a patient?
Gold standard is sending to external lab for confirmation
Otherwise use card/casette-based methods
Only available for DEA 1 and A/B
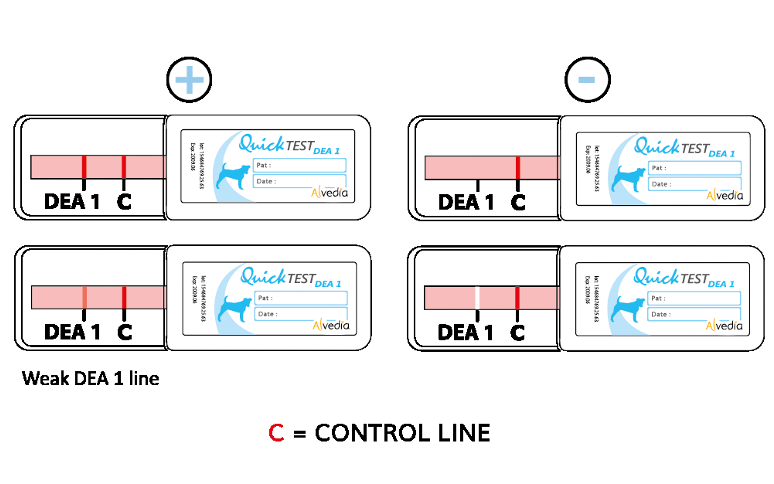
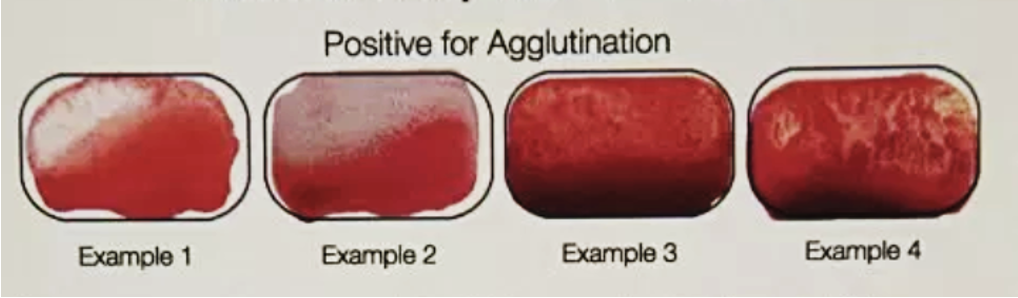
Imperative to rule out auto agglutination before using card based method
What is cross-matching?
Detects more haemotological (Type II HS) incompatabilities than blood typing alone
Will detect the majority of antigen-antibody incompatibilities
Will not detect non-antibody mediated incompatibilities
What are the different types of cross-matching?
Major crossmatch —> Recipient antibodies against donor red cells
Minor crossmatch —> Donor antibodies against recipient red cells
When is it necessary to cross-match patient?
If has had previous transfusion then imperative
Unless within 3-5 days of first transfusion as antibodies will not have formed
Grey area with need for crossmatch if have received plasma products
Similarly unclear with previous pregnancies
How do you cross match?
Laboratory is gold standard
Rarely get 100% compatible —> choose least risky
IDEXX and Pet blood bank will crossmatch and deliver bags to you (takes 24 hours)
In house gel-based methods are inaccurate and not recommended
How do you know how much blood you should give a placement via tranfusion?
Restrictive transfusion target —> aim for around PCV 21-25%
Use formulas as rough guide
Round up to nearest bag
How should a blood transfusion be administered?
IV admin
Transfusion set with an in line filer

Intra-osseous also acceptable
Slow rate initially and then building up thereafter —> generally dose dependent
Consider equipment, ability to monitor and maintaining sterility is vital
blood is growth medium for bacteria
How does the way of administering a blood transfusion differ in dogs and cats?
Dog —> better to administer drip by drip through a transfusion set rather than fluid pump
Cat —> better to administer via syringe driver
How fast should a transfusion be given?
0.5-1ml/kg/hr for first 15-30 mins
Increase to 4-6ml/kg/hr thereafter
Can be given as fast as possible in emergency situation
Ideally within 4 hours
Can slow down/take breaks if needed but ideally don't disconnect patient
How should you flush an IV in a blood transfusion?
Only with 0.9%NaCl as calcium containing fluids can form clots (interacts with anticoagulants)
What points should we note to do during a blood transfusion?
Administer medications in a separate line
Warming prior to admin not recommended (other than to room temp) → breakdown of RBCs in blood
Allow access to water but not food
What should you monitor in a patient receiving a blood transfusion?
Monitor for signs of transfusion reaction during and after admin
Monitor HR, RR & rectal temp (multiparameter machines)
Watch for signs of anaphylaxis e.g. swelling, urticaria, nausea, vomiting
Try and categorise to decide on underlying cause/appropriate tx
What are the types of transfusion reactions?
Haemolytic
Respiratory
Non-haemolytic
What are the different types of haemolytic transfusion reactions?
Acute
Delayed
What are the signs of an acute haemolytic transfusion reaction? What should we do?
Happens in minutes
Severe
Tachycardia/tachypnoea
Nausea/vomiting/pyrexia
Haemolysed serum
Haemoglobinuria
Can result in death
(expected with incompatible crossmatch)
STOP TRANSFUSION
What are the signs of a delayed haemolytic transfusion reaction?
Happens over days
Mild(er)
Slow removal of red blood cells
Mild antibody reaction OR new antibody formation
Jaundice/bilirubinaemia(uria)
Slower reduction in PCV
What are the types of respiratory trasnfusion reaction? When does each happen?
Transfusion associated circulatory overload (TACO)
Volume overload
Cats/small dogs/cardiac disease/renal disease
Transfusion associated reaction acute lung injury (TRALI)
Immune reaction
What should be done in a case of respiratory transfusion reaction?
Stop transfusion
Oxygen Support
Radiographs
Judicious fluids
?furosemide?
What are the types of non-haemolytic transfusion reactions?
Pyrexia/anaphylaxis
Citrate toxicity
Sepsis
What are the signs of pyrexia/anaphylaxis due to transfusion? What should be done?
Wbc/proteins/ microparticles
Vomiting/Nausea
Panting/pyrexia/tachycardia
Pause transfusion
Slower rate
Chlorphenamine
Maropitant
What are the signs of citrate activity due to transfusion reaction? What should you do?
Shaking/shivering
Check iCa2+
Administer calcium on separate line
What should you do if you can't differentiate between a mild transfusion reaction or stress/underlying condition?
If in doubt, 15-30 minute break, restart at slower rate
How much is the reccommended rate of fresh frozen plasma/frozen plasma or Cryo?
10-20ml/kg