Diagnostic Imaging Unit 3 Exam Material
1/266
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
267 Terms
Clinical Significance of Incomplete Segmentation of Transitional Vertebrae
— MAY be associated with back pain
— MAY be associated with disc herniation at the adjacent superior segment
— accessory articulation degeneration may occur
Sacralization vs Lumbarization
Sacralization = L5 doesn't fully segment from the sacrum (looks S1-like)
Lumbarization = S1 does not fully segment from L5 (looks L6-like)
What are some variable features associated with incomplete segmentation?
— hyperplasia of the transverse process
— non-segmentation or partial segmentation (MC)
— accessory joint formation
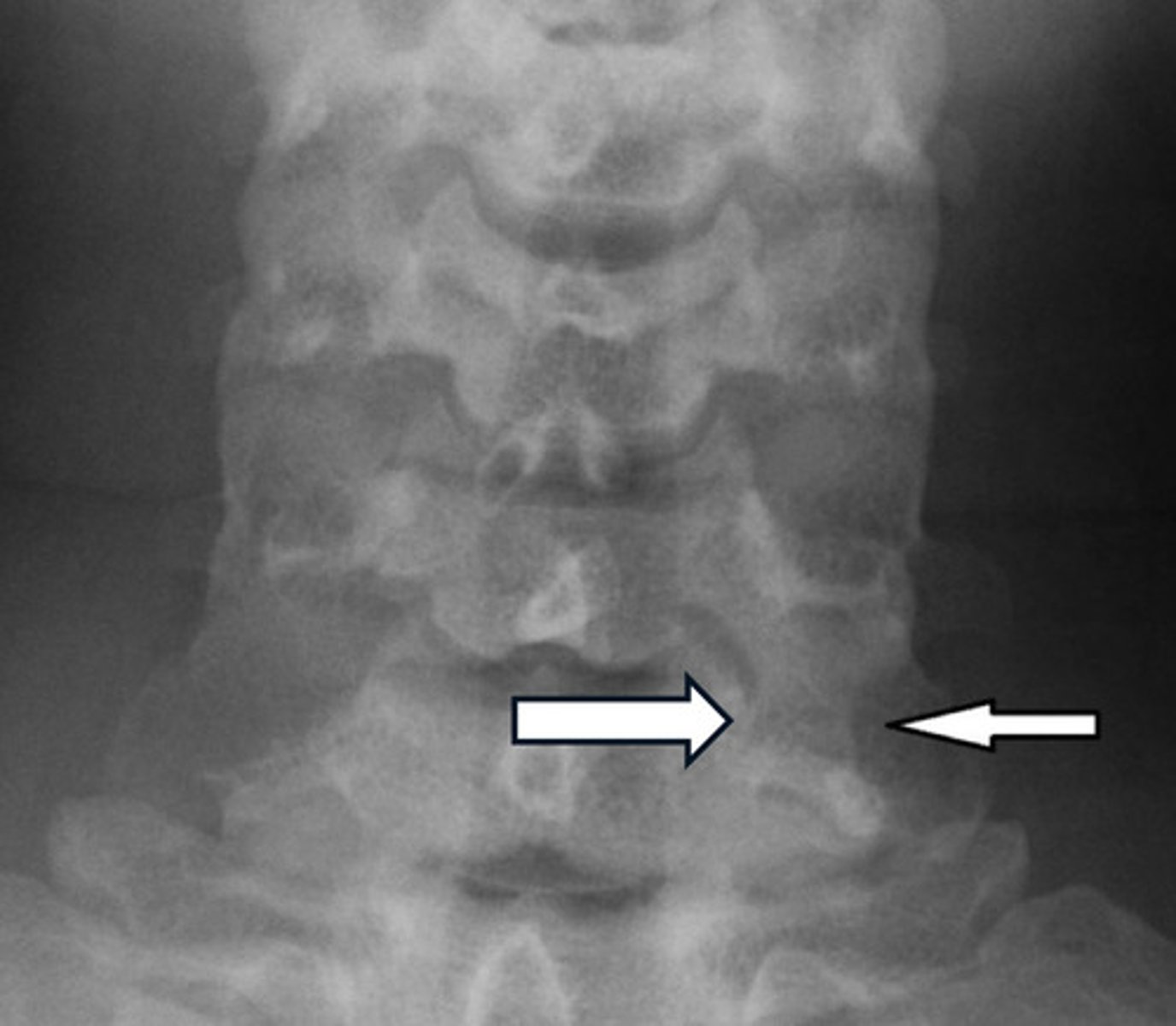
Imaging Findings of Incomplete Segmentation
— Hyperplastic transverse process ("batwing" appearance)
— Hypoplastic disc
— Possible accesory joint formation
— Occasional accessory joint degeneration

If you cannot use T1 for an accurate assessment of the transitional segment, what do you name it?
Generic term = lumbosacral transitional segment
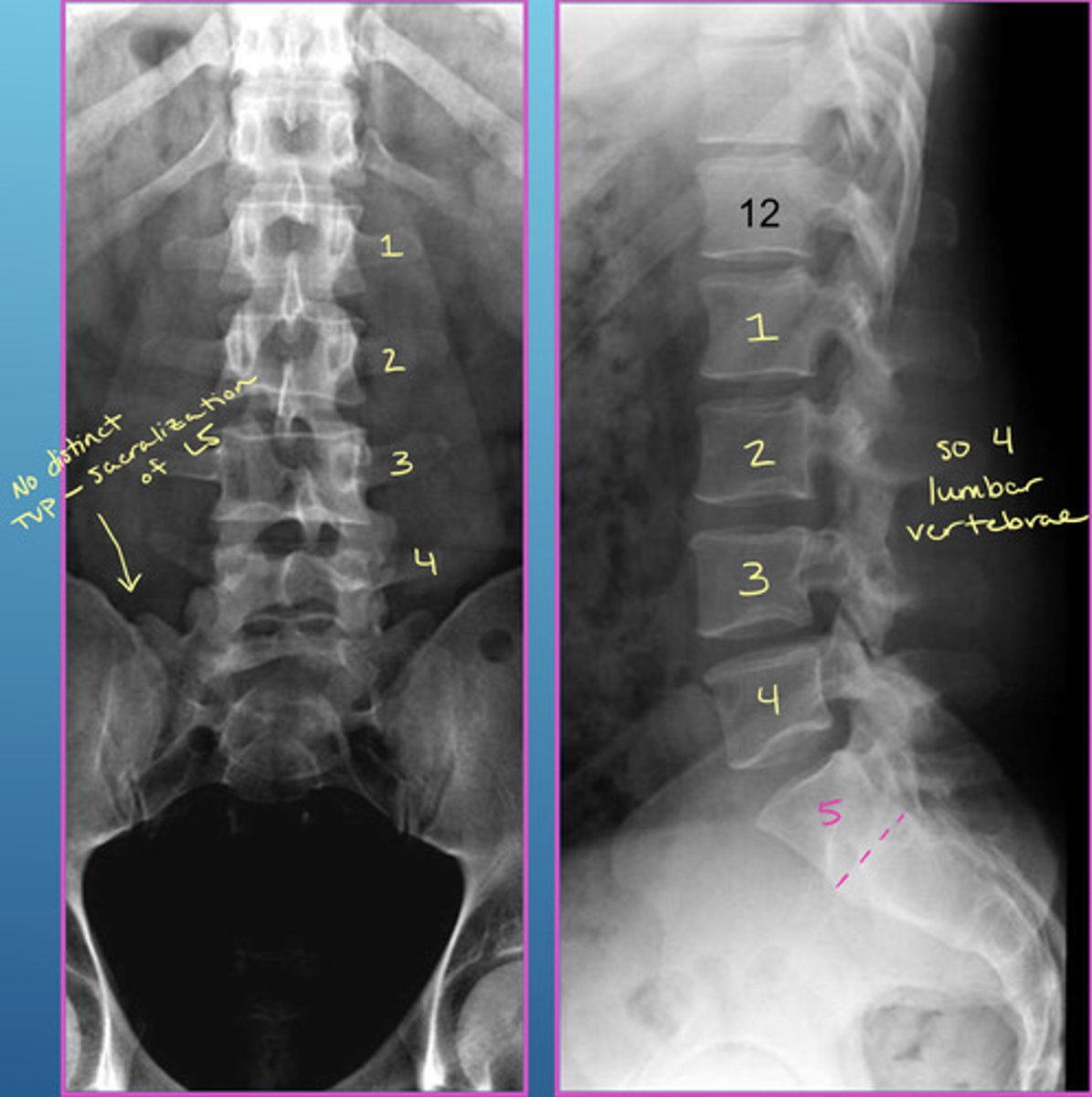
COMPLETE lumbarization vs sacralization
Complete lumbarization = 6 lumbar segments (S1 separated from sacrum)
Complete sacralization = only 4 lumbars (L5 fused with sacrum)
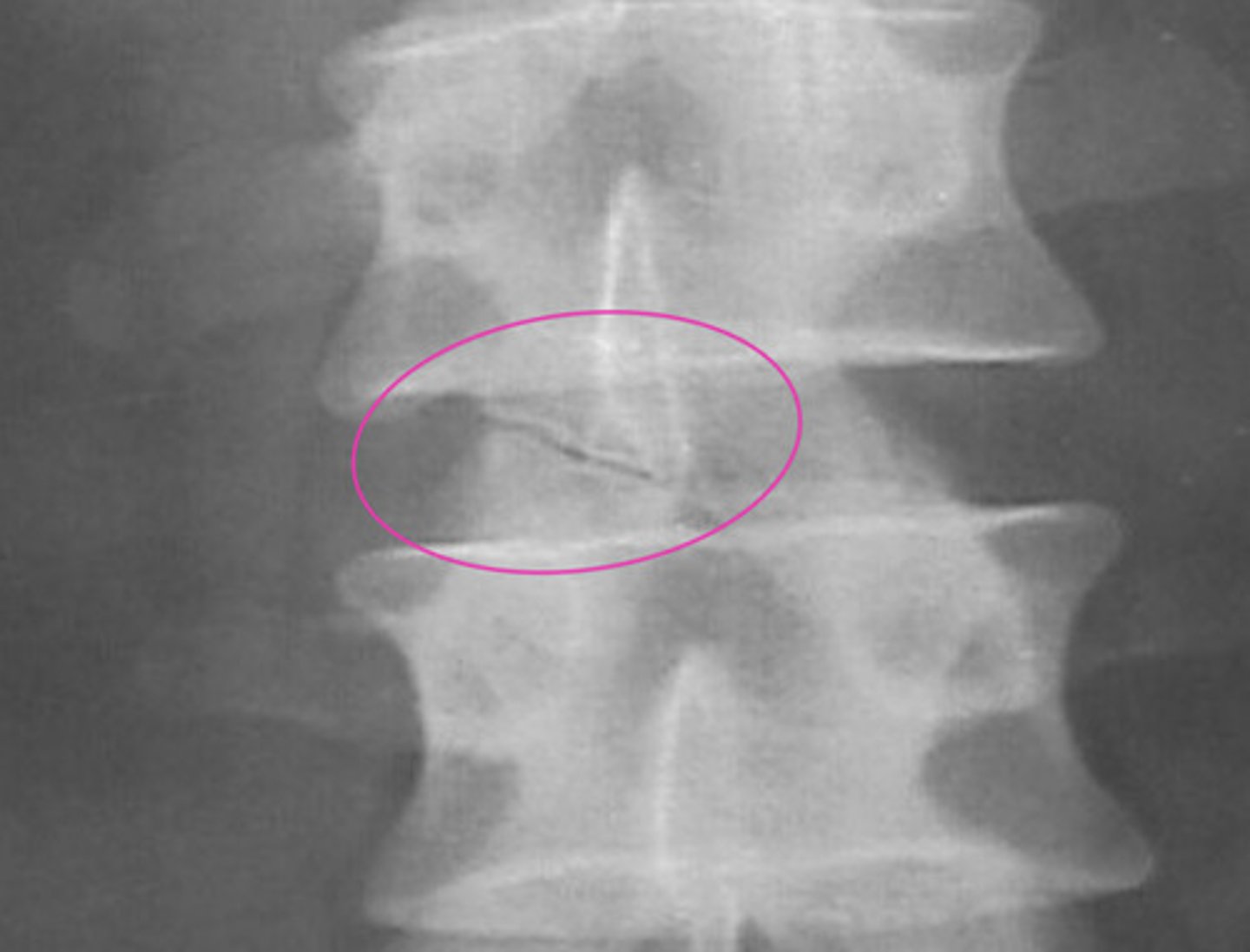
Image example of sacralization of L5
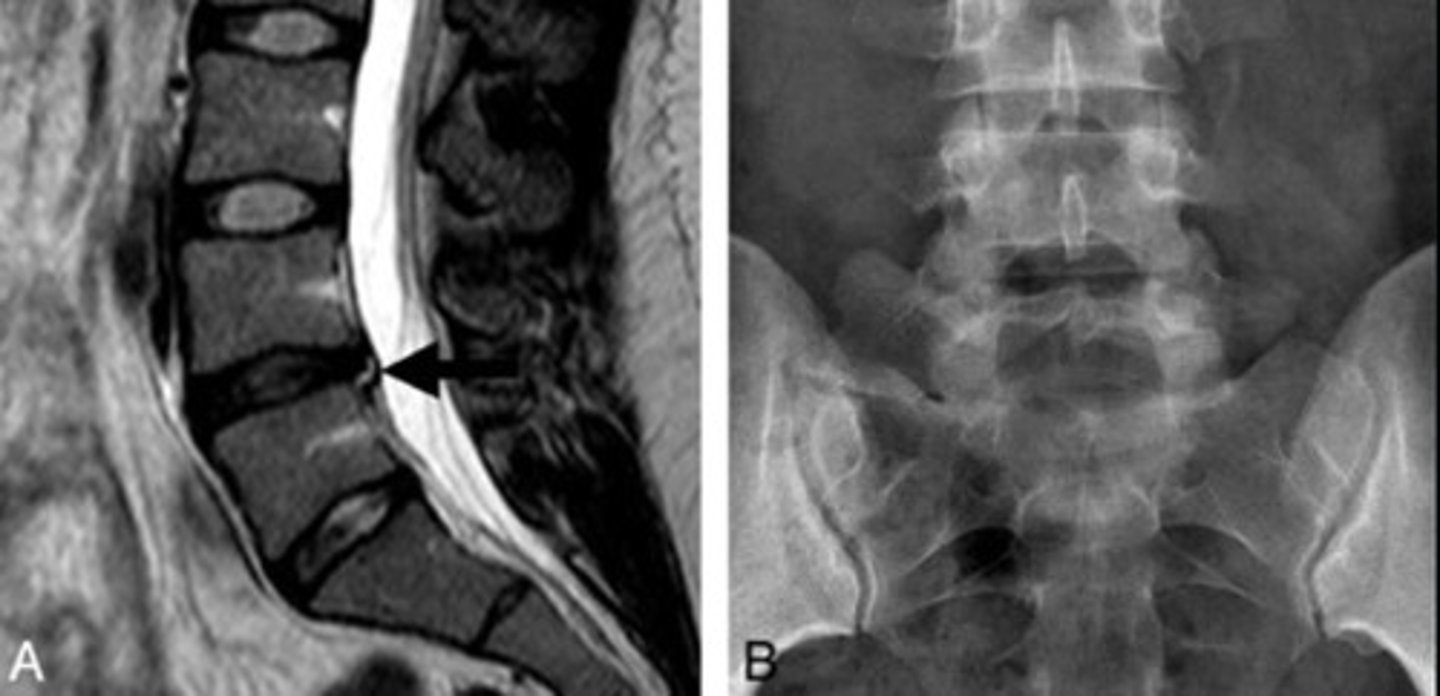
What is Bertolotti Syndrome?
Disc herniation with sacralization
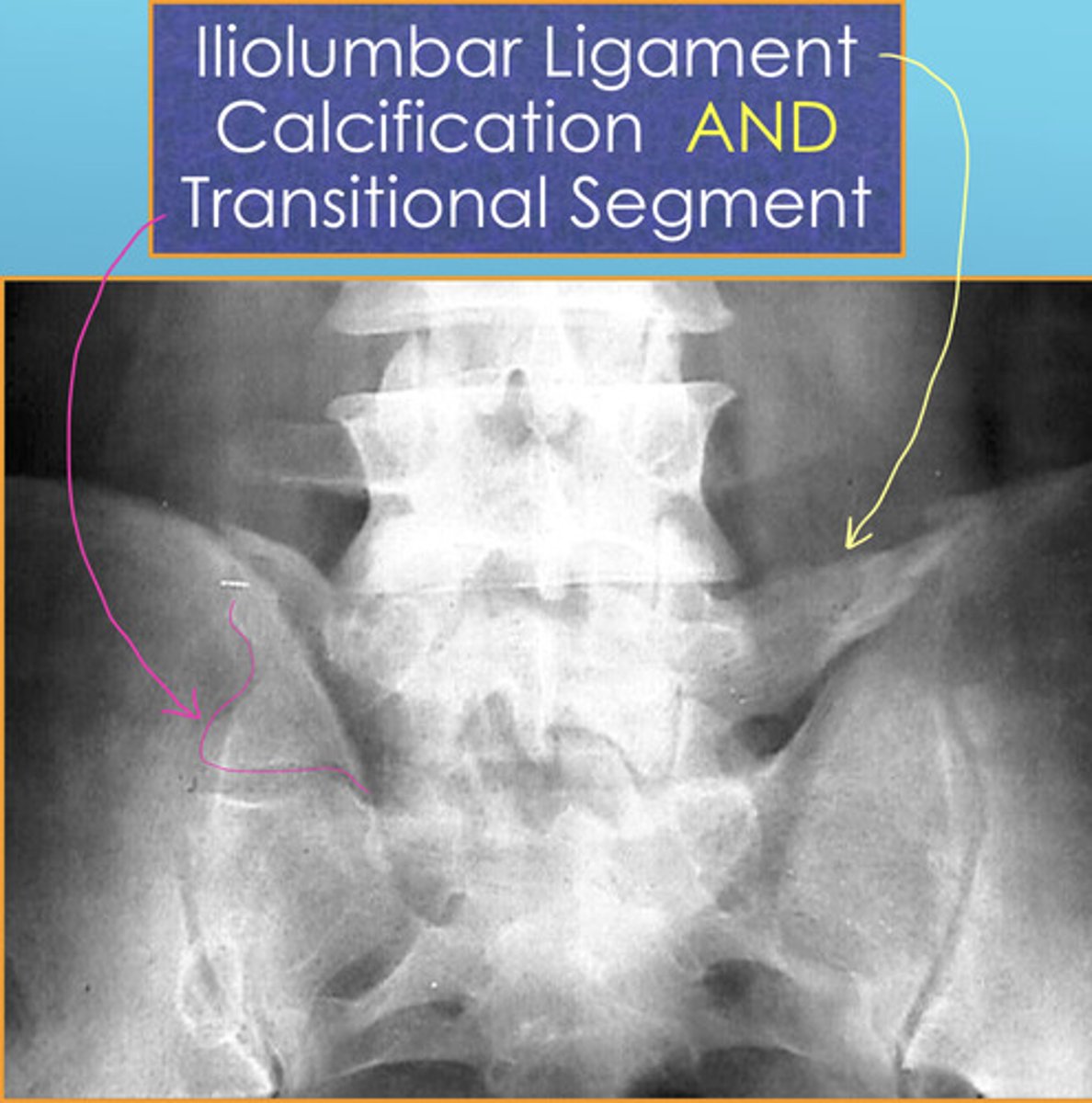
Iliolumbar Ligament Calcification

Iliolumbar Ligament Calcification AND a Transitional Segment
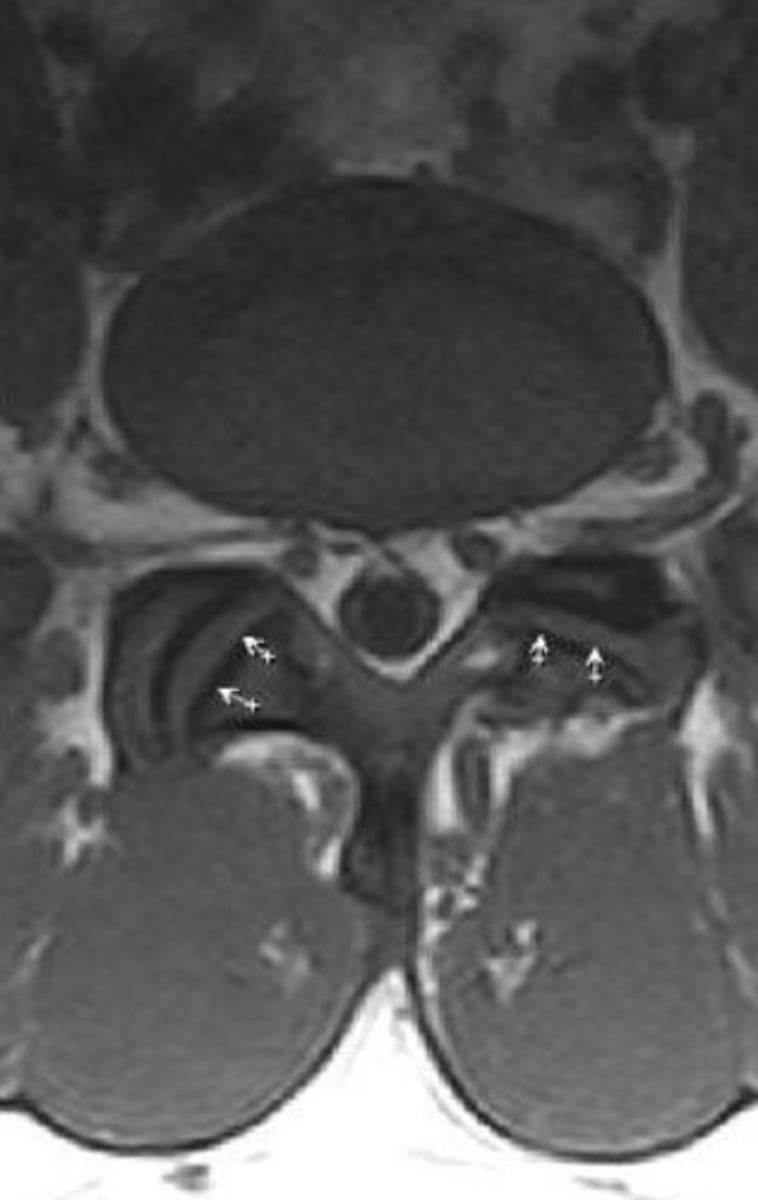
Facet Tropism
"Trop" = to turn
Asymmetric orientation of the facets = coronal AND sagittal facets at one level

Clinical Significance of Facet Tropism
Usually NOT clinically significant for most BUT may affect your adjustment
COULD be a predisposing factor for some pathological changes in the lumbar spine (disc degeneration, facet degeneration, and degenerative spondylolisthesis)
What is the most sensitive study to see facet tropism? What is the necessary difference in angulation of the facet joints to be considered facet tropism?
CT studies
8 degrees or more difference = facet tropism
Accessory Articulation at the Transverse Process

What is the clinical significance of an accessory articulation at the transverse process?
No clinical association known (rare finding)
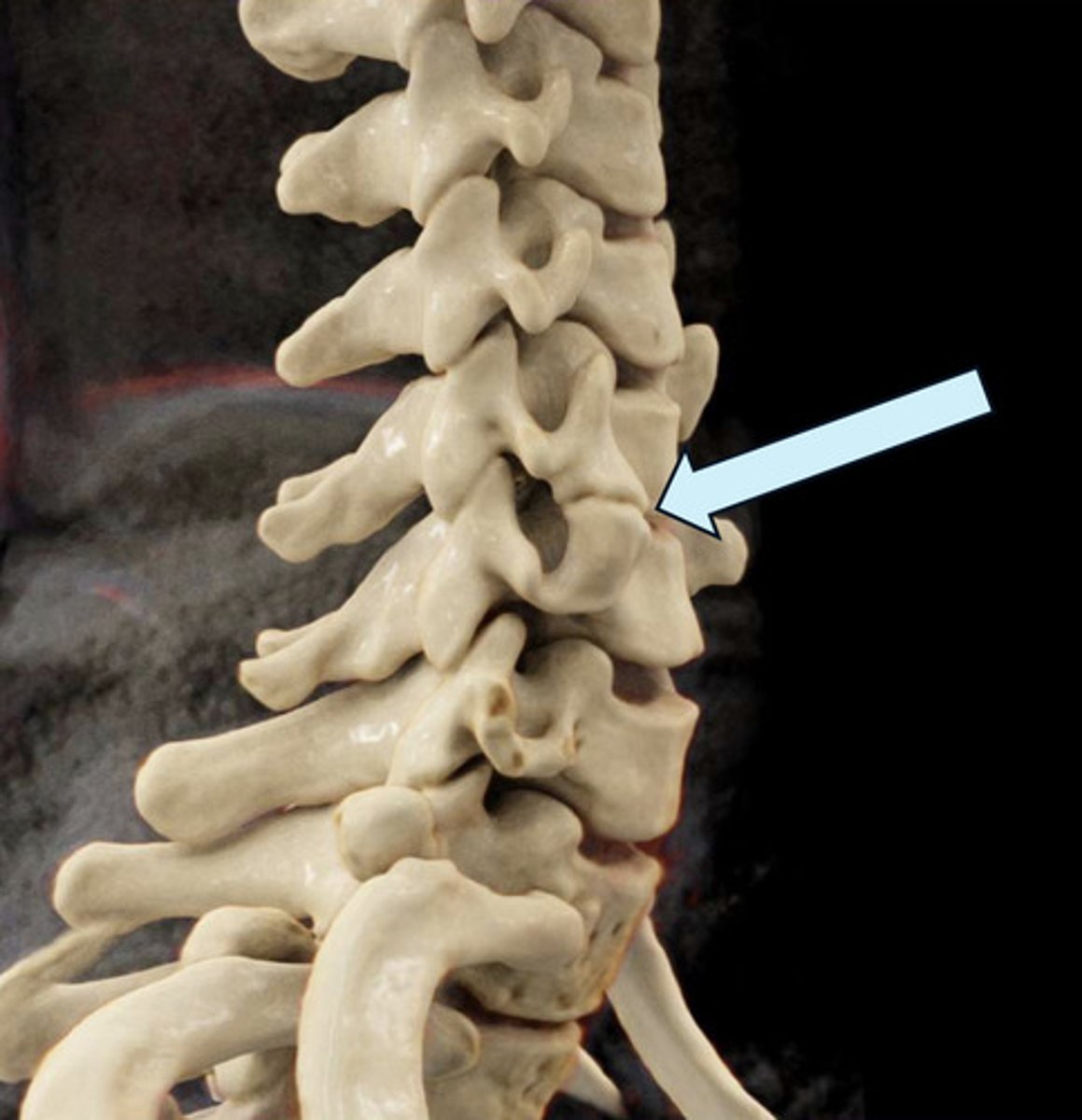
How does an accessory articulation at the transverse process occur?
Each cervical vertebrae transverse processes are formed by the lateral extension of the center of the neural arches
The costal portion of the transverse process may enlarge and elongate the anterior tubercle to articulate with the vertebrae below, giving rise to an unusual variant that could simulate a fracture
Persistent Apophysis
Reminder: apophysis = normal secondary ossification center that is located in the non-weight bearing part of the bone and eventually fuses over time
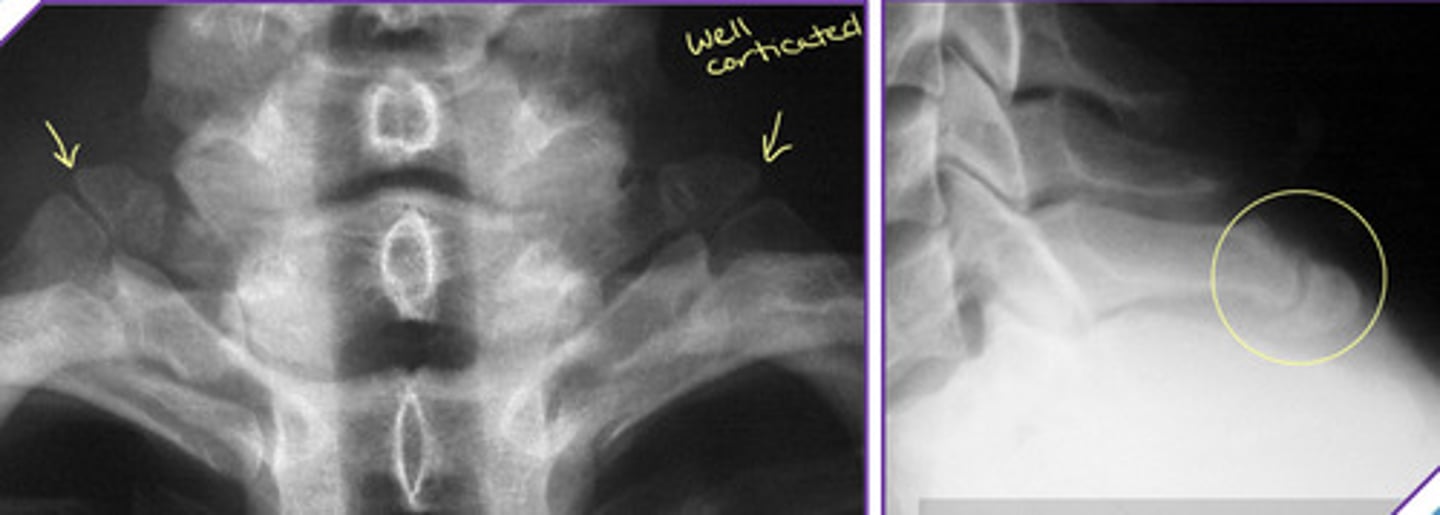
Hahn Vascular Cleft/Groove/Canal
Embryonic vascular channel = vertebral vascular foramina (Hahn Canal)
Do not mistake for a fracture
NO clinical significance
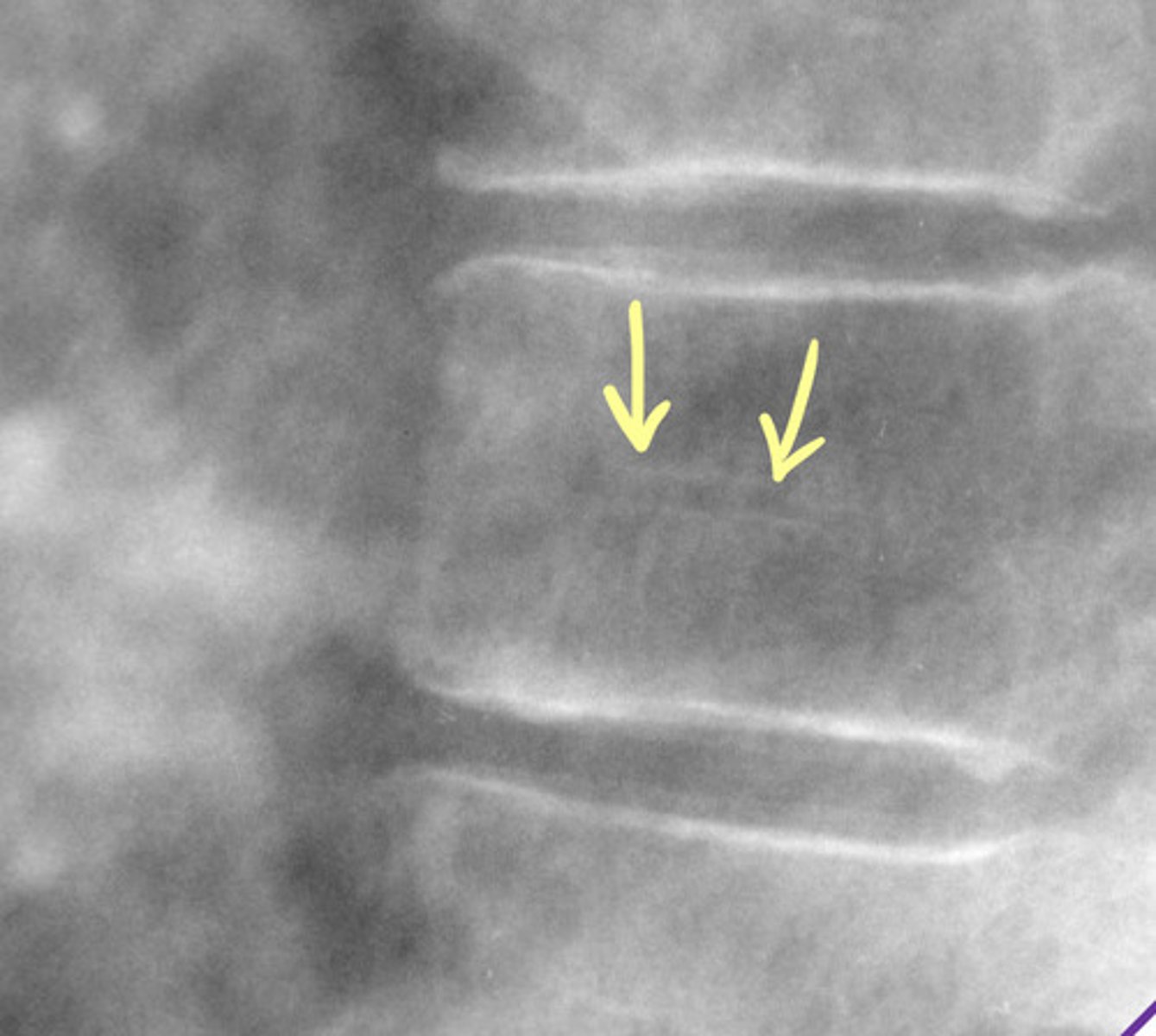
What does the Hahn Canal transmit?
— basivertebral veins
— intraosseous nutrient arteries
— basivertebral nerve
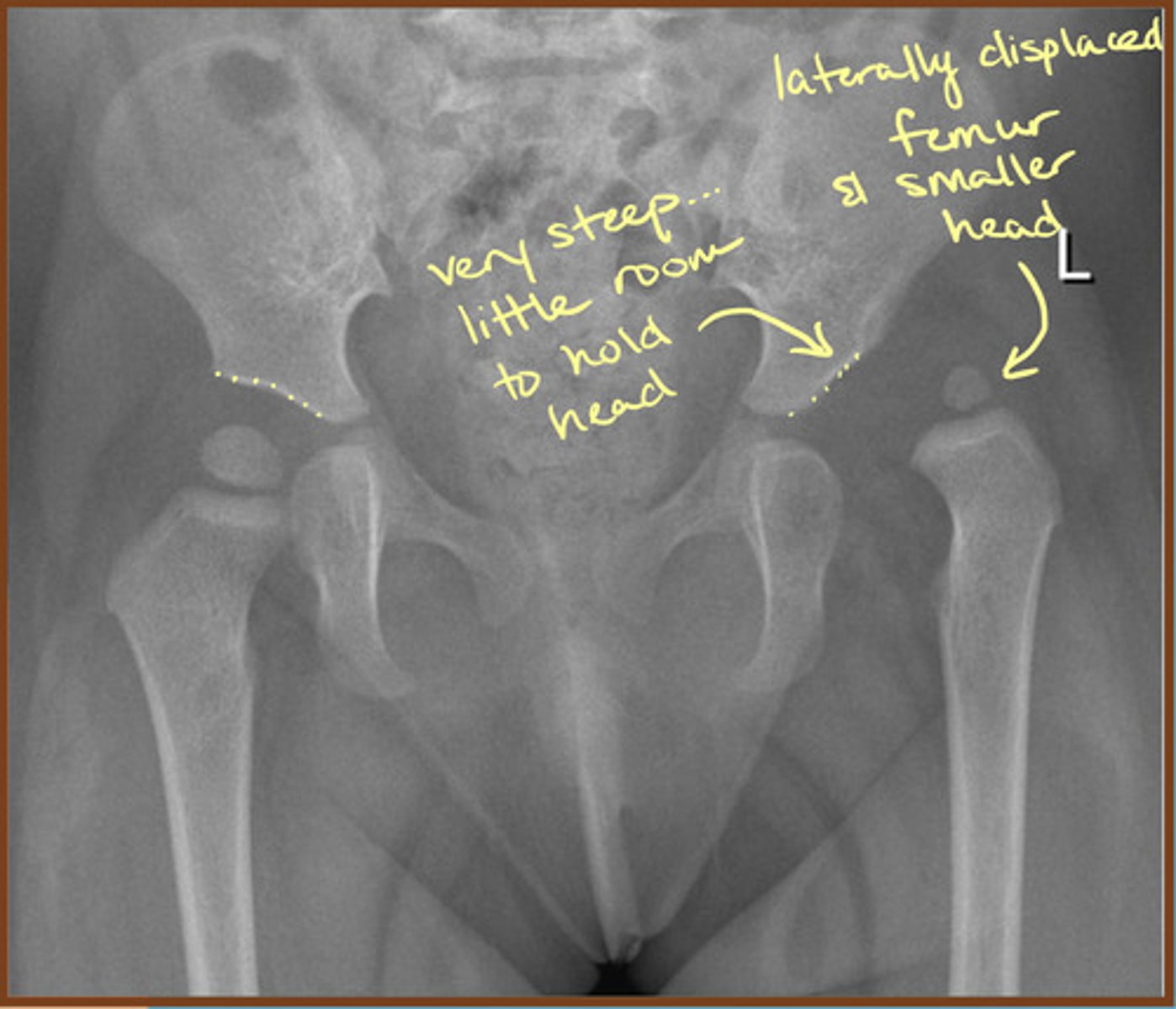
Developmental Dysplasia of the Hip (DDH)
Aberrant development of the hip joint, resulting from an abnormal relationship of the femoral head to the acetabulum
Usually occurs from ligamentous laxity and abnormal position in utero
Negative Ulnar Variance
Relative shortness of the ulna compared to the radius
Measured by comparing the distal ends of each bone

DDH Risk Factors
— females
— firstborn baby
— family history
— breech position
— oligohydramnios
— metatarsus adductus
— spina bifida
DDH commonly causes early onset of what?
Osteoarthrosis of the hip joint (sometimes even in the teens)
Orthopedic exams for DDH
Ortolani and Barlow
DDH more frequently affects which hip?
Left hip is more frequently affected
1/3 of cases are bilateral
Imaging Modality for DDH
Ultrasound is the modality of choice prior to ossification
Once significant ossification (>6 months) = X-ray is appropriate
What is the alpha angle on ultrasound to classify DDH?
Greater than or equal to 60 degrees
Hilgenreiner's Line
Used for assessment of DDH
Line drawn horizontally, connecting the inferior aspect of the tri-radiate cartilages bilaterally >> femoral head should be below this line

Perkin's Line
Line drawn vertically through the lateral most aspect of the acetabular roof perpendicular to Hilgenreiner's line
The ossified femoral head should be located in the inferomedial quadrant created
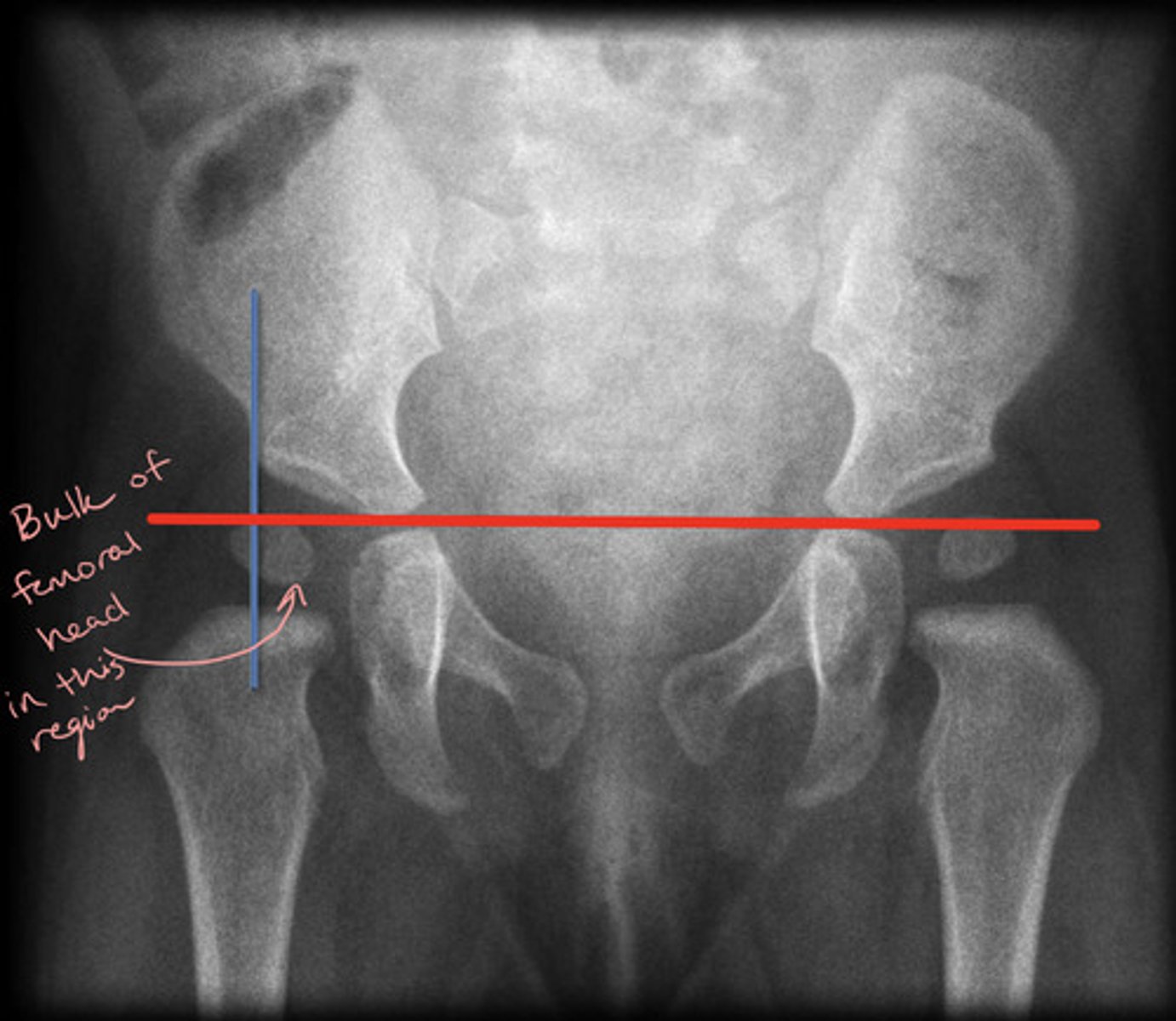
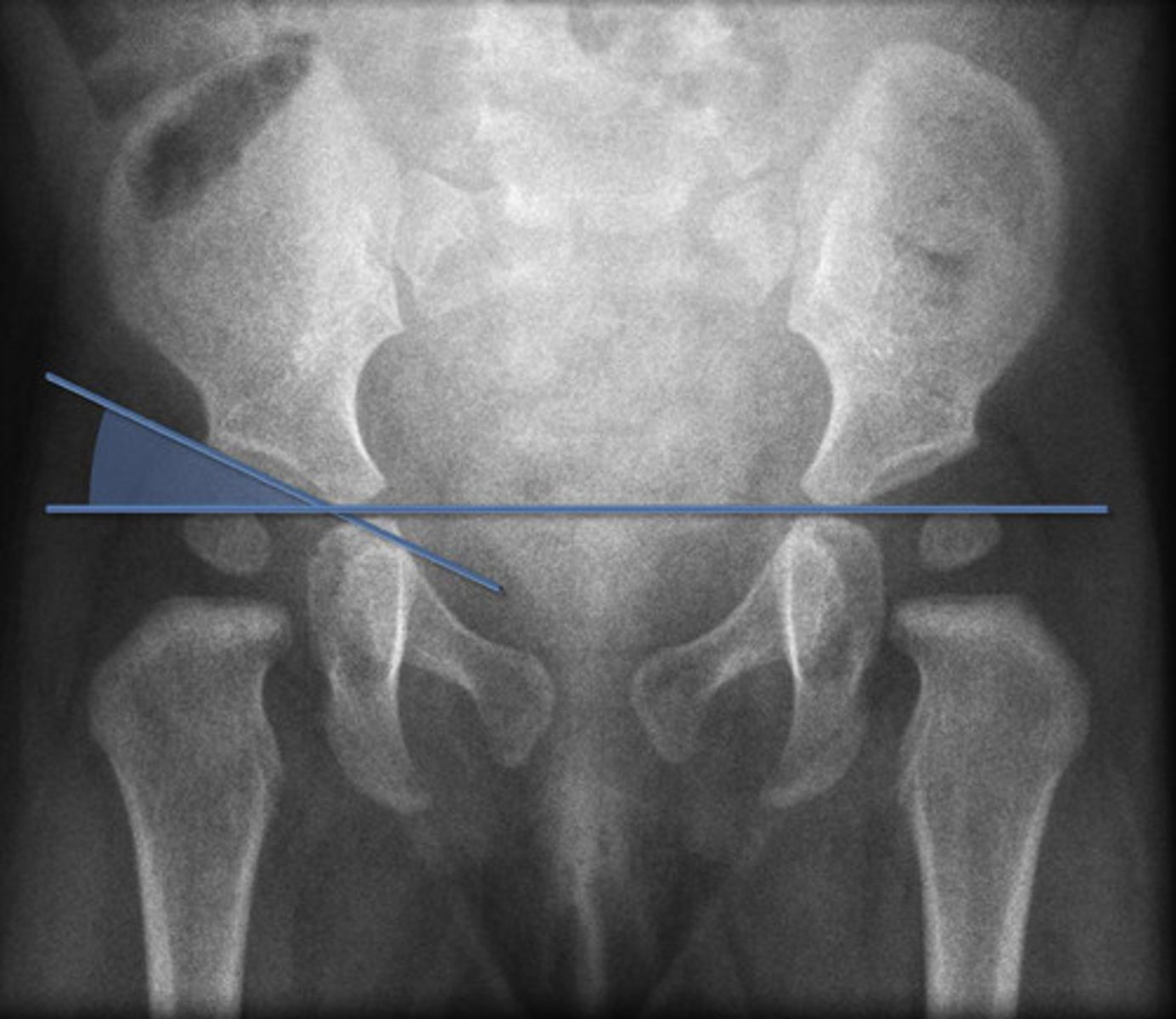
Acetabular Angle
Angle measured between Hilgenreiner's line and a line parallel to the acetabular roof
What is the normal bony coverage of the femoral epiphysis by the acetabular roof?
Greater than or equal to 50% coverage
What is the clinical significance of ulnar variance?
May lead to lunate avascular necrosis
Lunate avascular necrosis = Keinbock Disease
Positive Ulnar Variance
Relative lengthening of the ulna compared to the radius
Measured by comparing the distal ends of each bone
Clinical significance of positive ulnar variance
May lead to ulnar abutment (impaction) of the lunate and TFCC (triangular fibrocartilage complex) degeneration
May be associated with triangular fibrocartilage tear

What is the normal value for the acetabular angle at birth? What should it be later in life?
At birth should be less than 28 degrees
Should progressively reduce with maturation of the hip to less than 22 degrees after the age of 1
Adults = between 33 and 38
Imaging findings of Acetabular Protrusion
— Center-edge angle (Wiberg Angle) greater than 40 degrees and medialization of the medial wall of the acetabulum past the ilioischial line (Kohler's Line)
— Acetabular fossa greater than 3 mm beyond the ilioischial line in men and 6 mm in women
— Projection of the femoral head medial to the ilioischial line
Femoral Herniation Pits
Notice denser, cortical bone around the pit

Clinical Significance of Femoral Herniation Pits
Incidental findings with no clinical significance = "leave it alone lesion"
Pits may enlarge over time
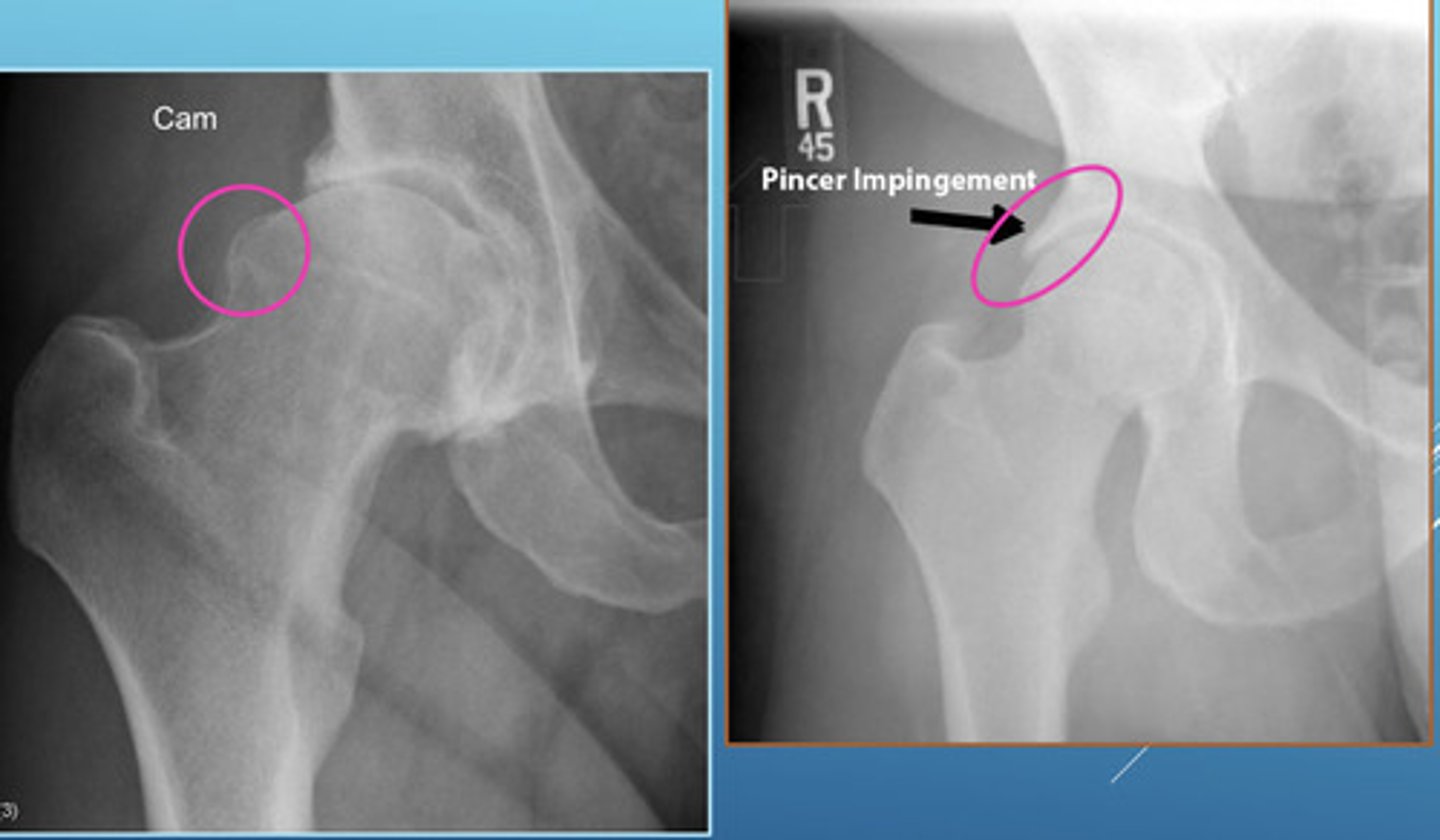
Femoral Acetabular Impingement (FAI)
Condition that characteristically presents with hip pain secondary to mechanical impingement from abnormal hip morphology involving the proximal femur and/or acetabulum
2 Types of FAI Joint Deformities
(1) Pincer Morphology = overcoverage of the femoral head
(2) Cam Morphology = bump formation at the femoral neck and asphericity
Both can co-occur and can lead to FAI and predispose to early OA
What is the acetabular angle that defines acetabular dysplasia?
Greater than 42 or 45 degrees (varies between authors)
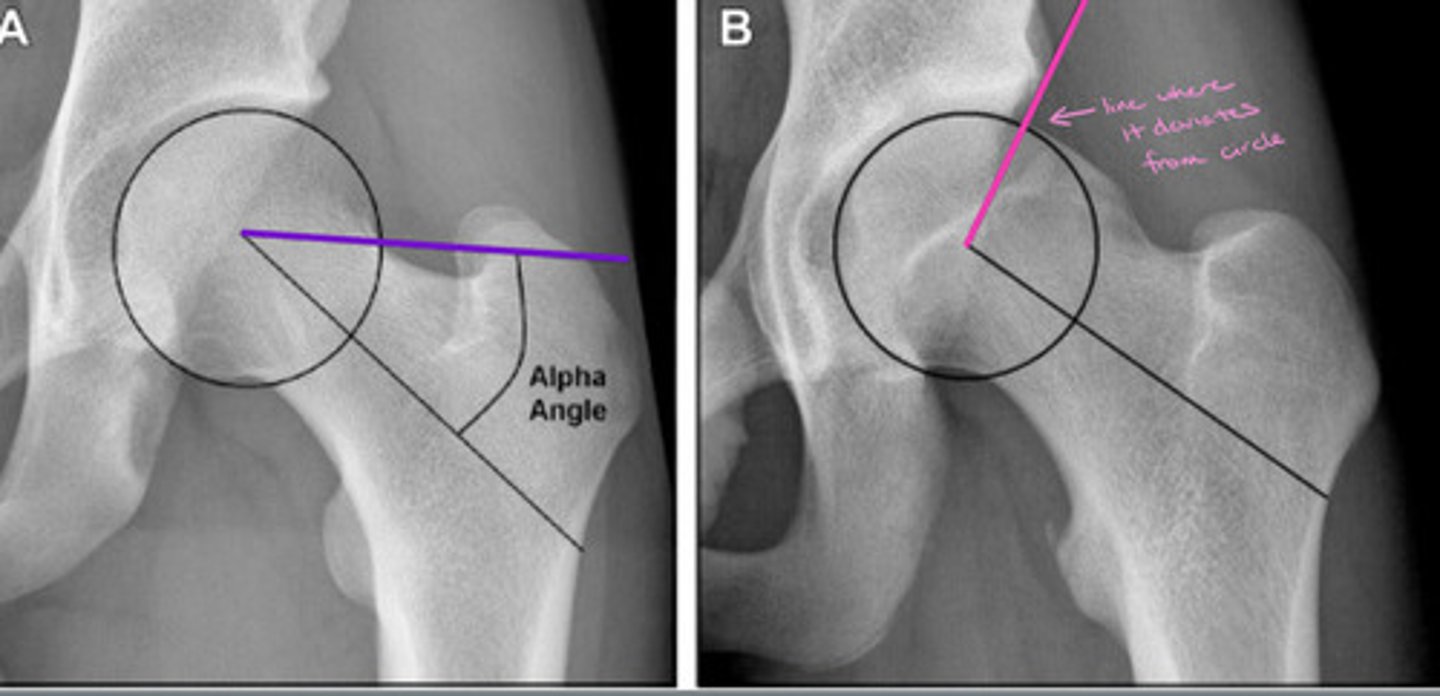
Alpha Angle
Measures the extent to which the femoral head deviates from spherical
Normal = <50 degrees
FAI = >50 degrees
Ischiopubic Synchondrosis

Paraglenoid Sulcus/Sulci
Note: nearly exclusively seen in females

Imaging Findings of FAI
— Cam or Pincer morphology
— Pistol grip deformity (Cam)
— Acetabular overcoverage (Pincer)
— Ilioischial line violation (protrusio acetabuli)

Putti's Triad
Sign of DDH
(1) Absent or small proximal femoral epiphysis
(2) Superolateral or lateral displacement of the femur
(3) Increased acetabular angle
What is the term for when there is stylohyoideus ossification with clinical symptoms like neck pain?
Eagle Syndrome (rare to have clinical symptoms)

Costal Cartilage Calcification
More common in lower ribs

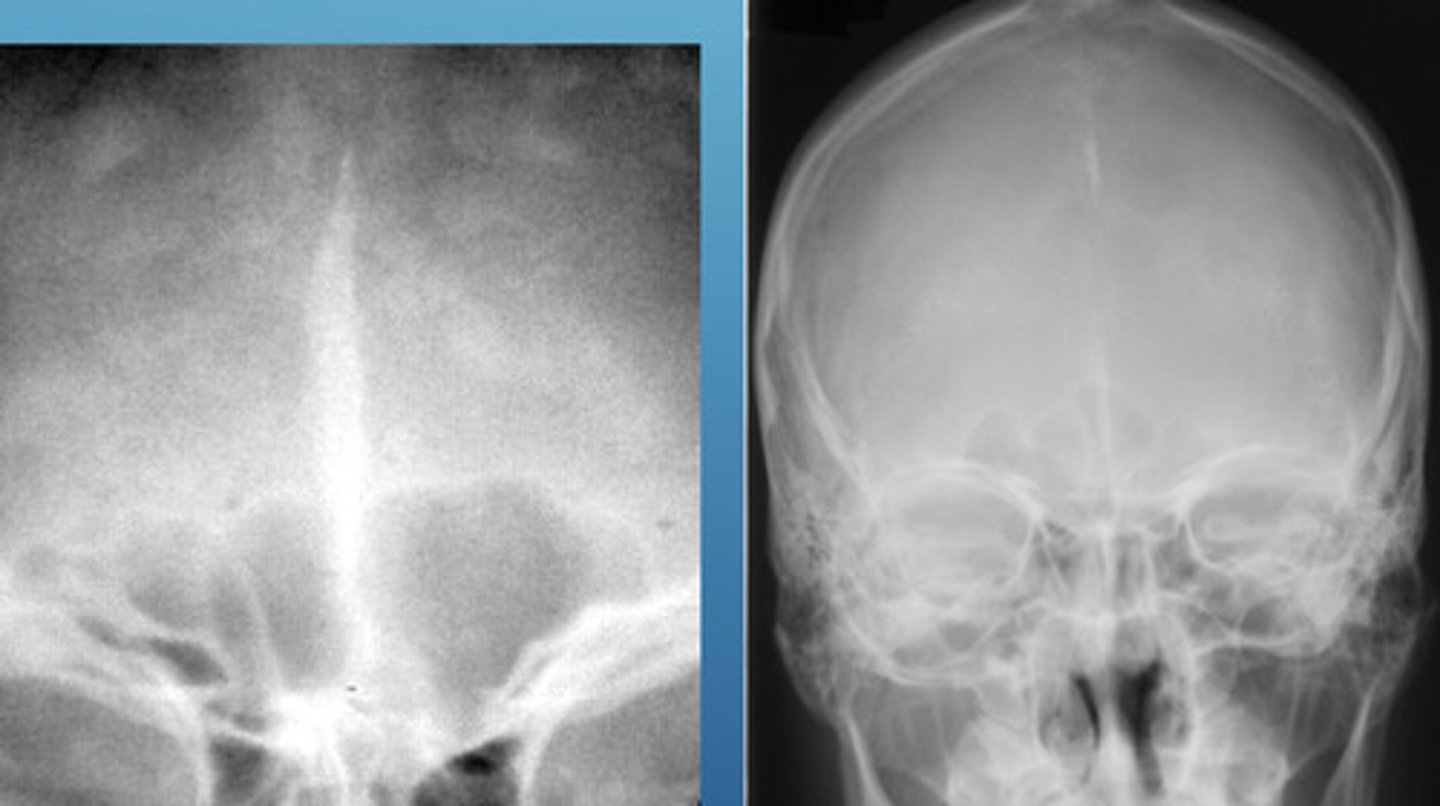
Falx Cerebri Calcification
Physiological calcification of the dura at the frontal bone
no clinical significance
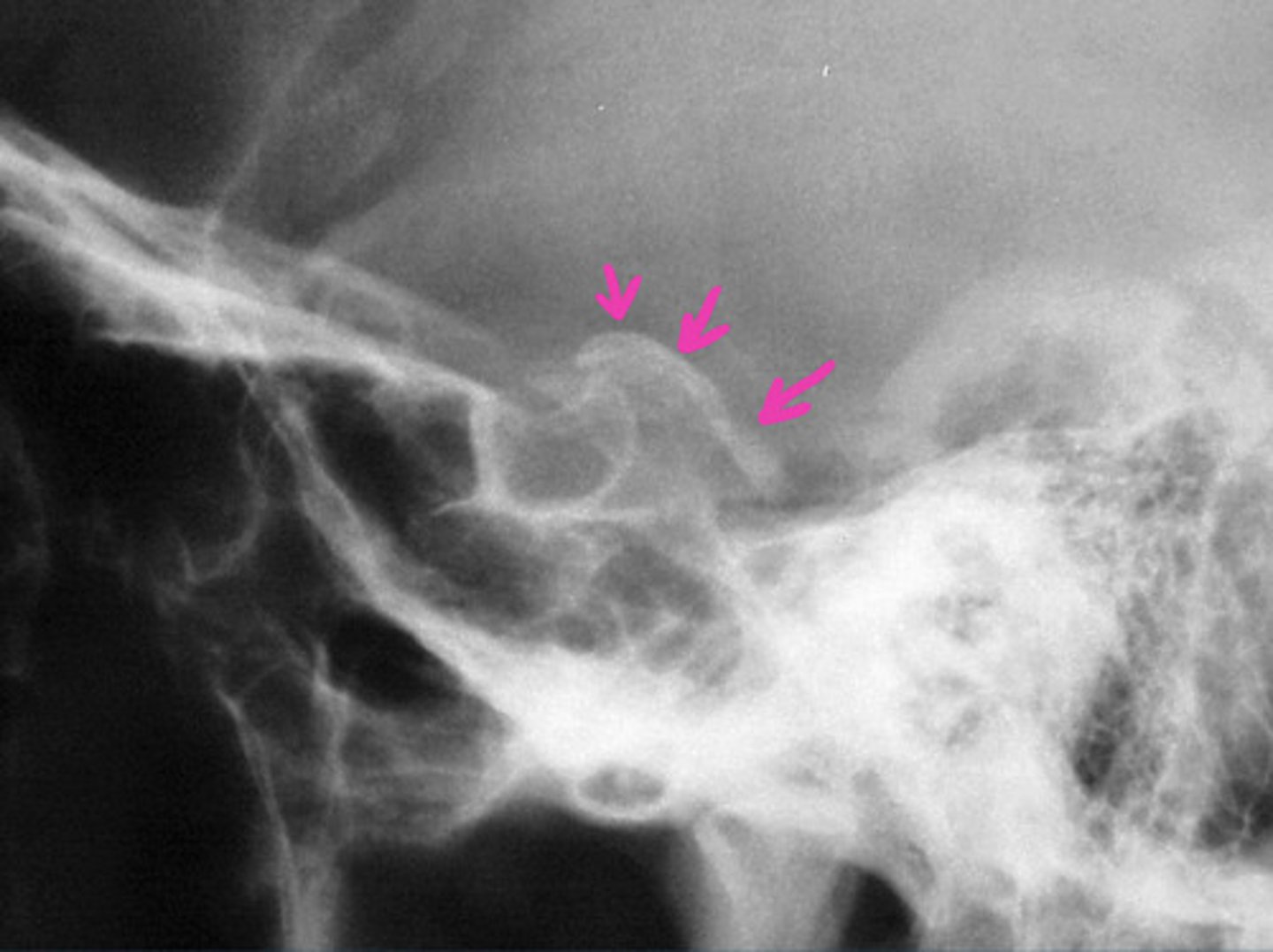
Petroclinoid Ligament Calcification
Physiological calcification of the dura
No clinical significance
Pineal Gland Calcification
Physiological calcification in about 50% of the population

Acetabular Protrusion (aka Protrusio Acetabuli)
Intrapelvic displacement of the acetabulum and femoral head, resulting in the femoral head projecting medial to the ilioischial line
What age should we suspect a neoplasm instead of pineal gland calcification?
< 6 years it is very rare so suspect a neoplasm (pinealoma)
Calcification of the thyroid cartilage
No clinical significance

Phleboliths
Calcified venous thrombi
Perirectal veins (not midline)

Causes of Acetabular Protrusion
Primary (developmental)
Secondary (pretty much anything that soften's bones)
— Paget's
— Psoriatic arthropathy
— RA
— osteomalacia and Rickett's
— Marfan Syndrome
— Osteogenesis imperfecta
— Hemophilia
Categories of Soft Tissue Calcifications
(1) Dystrophic (trauma, including infection)
(2) Metabolic/metastatic
(3) Physiological (normal, usually cartilaginous tissue)
Stylohyoideus Ossification
Physiological calcification with minimal clinical impact
Clinical Significance of Scoliosis
— cardiopulmonary complications
— altered biomechanics
— degenerative changes
— curvature progression
— cosmetic concerns
What is scoliosis defined as?
Coronal curvature(s)/lateral deviation(s) greater than or equal to 15 degrees
May include rotation at one or more segments
Note: less than 15 degrees is a “curve”
How to measure scoliosis on AP Film
(1) Draw a line along the endplates of the uppermost and lowermost involved vertebrae that tilt significantly toward the concavity
(2) Draw perpendicular lines through those two lines
(3) Measure the resulting intersecting angle
What is the apex of a scoliosis?
The "peak" of curvature = the vertebra furthest from midline
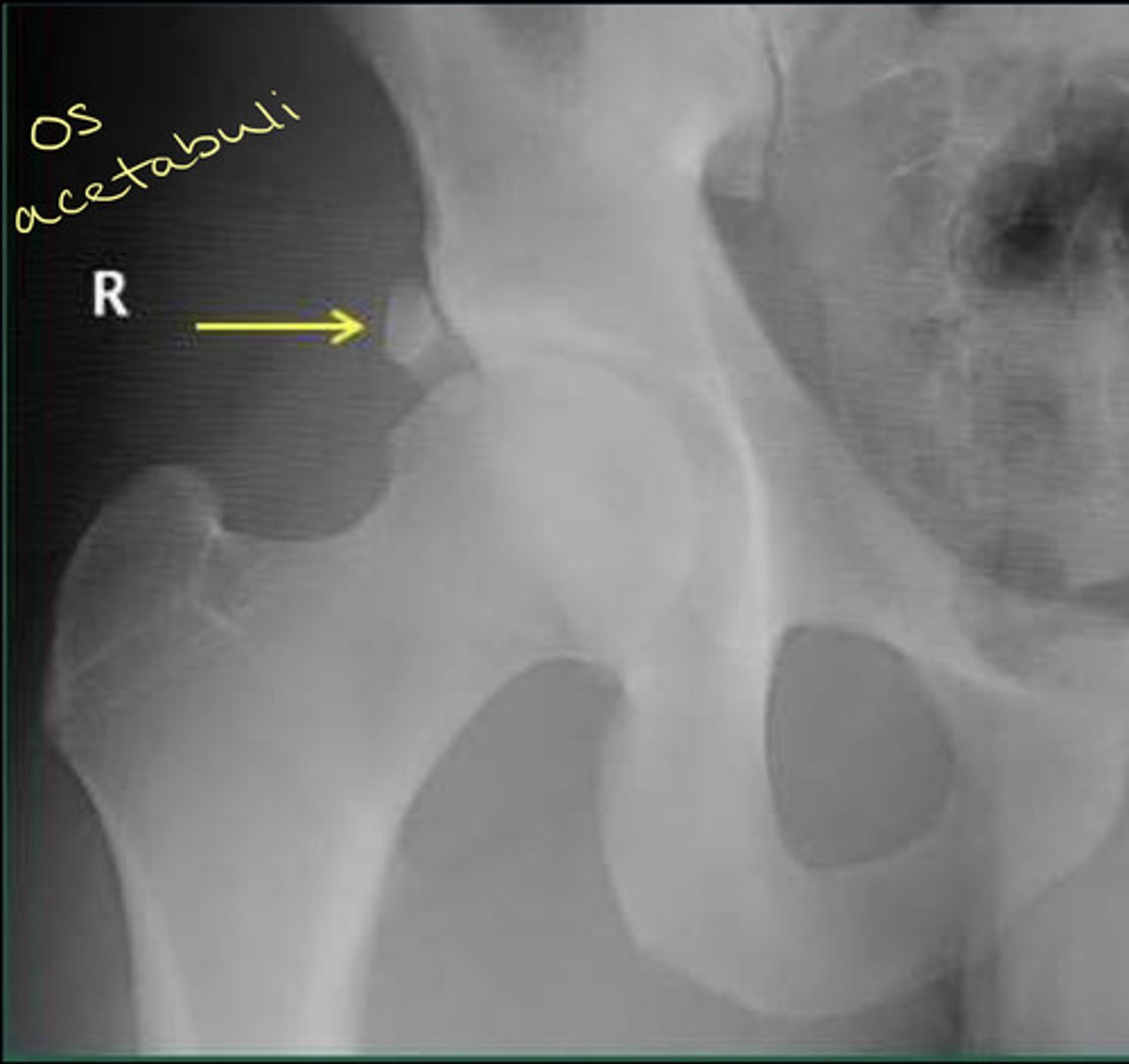
Persistent ulnar styloid process
Another persistent apophysis

Os Acetabuli
Another persistent apophysis
Oppenheimer Ossicles
Accessory ossicles of the facet joints (another example of a persistent apophysis)
Mainly in the lumbar spine (rarely in T or C spine) — about 4% of lumbar spines
Predominately a single, unilateral ossicle of the inferior articular process (but can occur at superior process too)

What is believed to be the cause of Oppenheimer Ossicles?
Thought to arise as a result of the non-union of an articular process secondary ossification center (typically fuses between ages 17 and 25)
Age Classifications of scoliosis
Infantile = 1-3 years
Juvenile = 3-10 years (more common in females)
Adolescent = > 10 years (more common in females)
Absent Pedicle and its clinical significance
Congenital Absence of a spine pedicle is rare, but important to avoid misdiagnosis >> if not congenital, could be an osteolytic pathology
"Winking Owl Sign"

Imaging Findings of an Absent Pedicle
— MAY have stress hypertrophy (enlargement, cortical thickening, and sclerosis) of the contralateral pedicle)
— MAY have accessory transverse process sign (small inferiorly directed transverse process with a small joint space separating it from pedicle or vertebral body)
— MAY have spinous deviation towards the contralateral side (away from the side of pedicle missing
Absent Pedicle Etiologies
(1) Congenital
(2) Destructive (tumor or infection)
(3) Surgical
What does coalition mean?
A joining together
A connection between two bones without indicating etiology
What are the most common carpal bones involved in carpal coalition?
(1) Lunotriquetral coalition (more common in females)
(2) Capitohamate coalition (~5%)
Less common = hamate-pisiform coalition
But many other reported combinations
Carpal Coalition etiology
(1) Congenital (Mendelian inheritance)
(2) Acquired (inflammatory arthropathy or due to intentional surgical arthrodesis)
Lunotriquetral Coalition

De Villier's Lunotriquetral Coalition Classification
(1) Incomplete (or fibrocartilaginous) fusion
(2) Incomplete osseous fusion
(3) Complete osseous fusion
(4) Complete osseous fusion with other carpal abnormalities
Lunotriquetral Coalition management and prognosis
Most commonly an incidental finding and does not require treatment if not symptomatic
May occasionally cause chronic wrist pain and can be fractured
What must be determined in EVERY case of scoliosis?
Etiology (cause)
Prognosis ands management are highly dependent on the cause
What are the two types of scoliosis?
(1) Functional
(2) Structural
What is the maximum size of pineal gland calcification?
Should not exceed 10 mm
What is the measurement to consider positive or negative ulnar variance?
Positive = level of the ulna is > 2.5 mm beyond the radius margin
Negative = ulna is less than or equal to 2.5 mm than the radius margin
What are the features of a functional scoliosis?
Curve is sufficiently mobile to resolve with a change in posture
— non-progressive
— leg length discrepancy
— asymmetrical activities
— pain/antalgia
What is structural scoliosis? What is a good indicator of this?
Fixed and nonflexible curve that fails to correct on recumbent lateral bending radiographs
If laterally bends to the convex side, you would expect that curve angle to open BUT...if structural, that would not happen and the curve would not change with lateral bending
What is the most common cause of scoliosis? (Overwhelmingly)
Idiopathic
Other causes of scoliosis
(1) Arthritic
(2) Congenital
(3) Neuromuscular
(4) Tumors
(5) Post-irradiation
Idiopathic Scoliosis
By far the most common form
— thought to be related to defects in proprioception and vibratory sense
— girls are more frequently affected than boys (7:1) and they are more likely to progress and require treatment
— patterns may be thoracic (usually convex to the right), thoraco-lumbar, lumbar, or double major
Degenerative Scoliosis
Scoliosis is secondary to degeneration of the ligaments (like the IVD!)
Congenital Scoliosis
Secondary to hemivertebra(e) or congenital non-segmentation
— the curvatures are usually seen in short segments
— bracing is ineffective
— high risk for progressive curves (usually surgically fused early in life to limit progression)
What is the most common tumor causing painful scoliosis?
Osteoid osteoma (usually located in the posterior elements)
Characteristics of scoliosis caused by a tumor
— scoliosis is usually long with concavity on the side of the lesion
— tumor is best detected and evaluated with a bone scan and CT
What neuromuscular conditions can cause scoliosis?
(1) Cerebral palsy
(2) Syrinx
(3) Poliomyelitis
(4) Muscular dystrophy
(5) Spinal cord tumor
What are the usual characteristics of scoliosis caused by a neuromuscular condition?
Curves are often long, single, LEFT C curves
"Wrong way scoliosis"
Note: not required to be left curve, but most common
Idiopathic scoliosis with early onset should cause suspicion of which other etiology?
Neuromuscular etiology
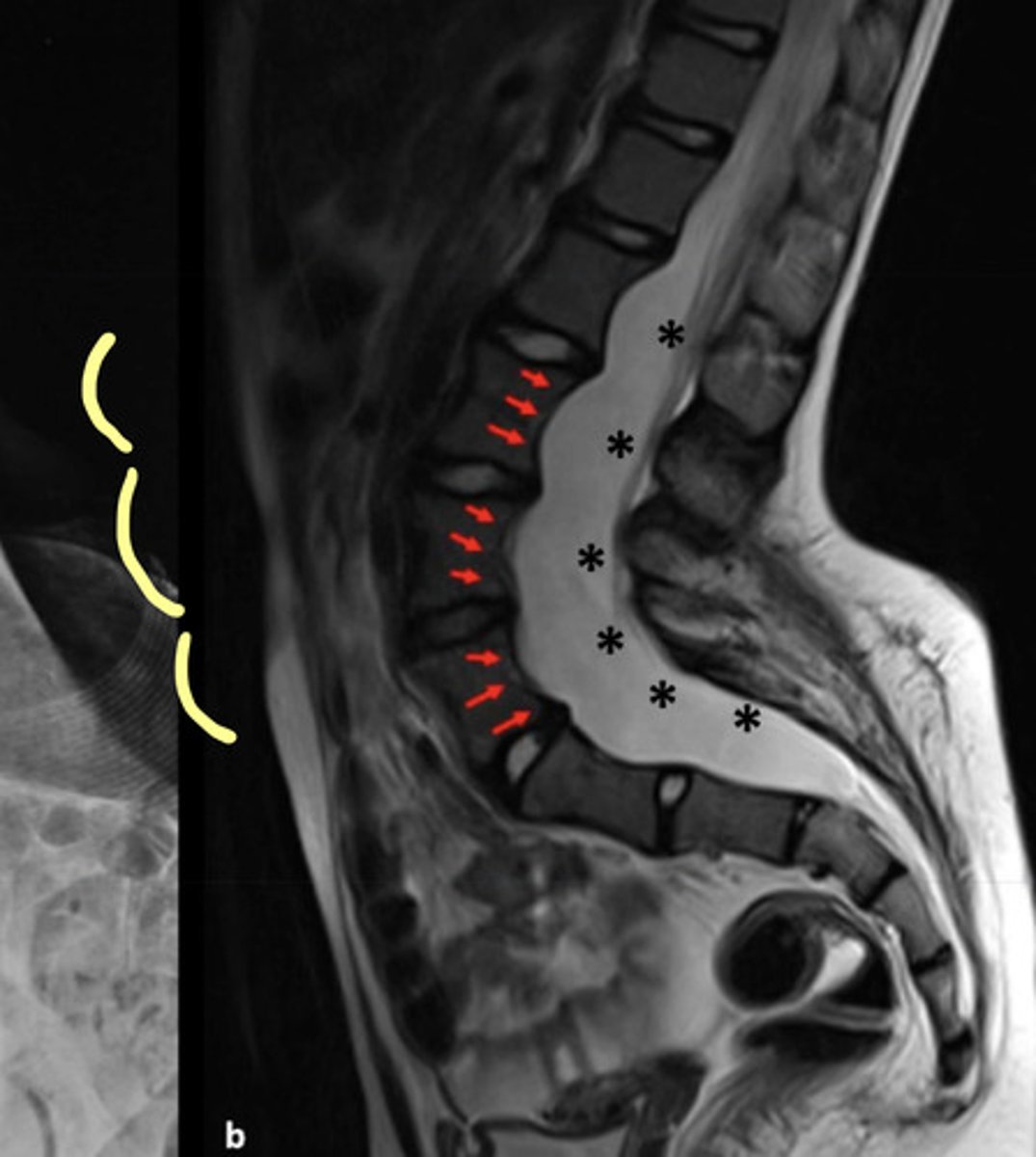
Scoliosis is commonly associated with what other condition?
Neurofibromatosis (NF) I and II = autosomal dominant disorder with skin, endocrine, nervous system, and bone manifestations
What are some clinical signs of NF I and II?
— cafe au lait spots that appear prior to age 3
— skin nodules that occur in late adolescents
What is a common sign of NF in the spine on an X-ray?
Ribbon-shaped ribs and posterior vertebral body scalloping
Curves must be monitored carefully since they can collapse and rapidly produce paralysis
Radiation Etiology of Scoliosis
Exposure of the skeletally immature spine within the radiation port will delay or stop growth of the spine, potentially resulting in scoliosis
Note: today radiation is delivered more precisely with small radiation ports
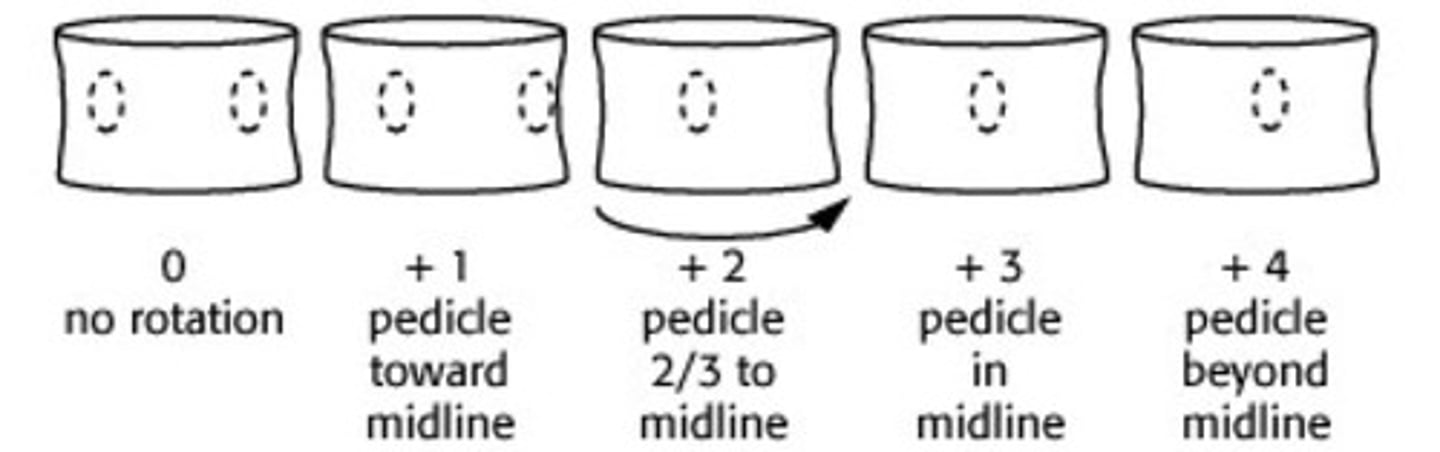
Pedicle Rotation: Nash-Moe Method
Pedicle movement on the CONVEX side
Graded 0-4 at the apex of the curve
What is an imaging technique to help analyze the curve flexibility of a spine with scoliosis?
Lateral Bending Radiographs
How do lateral bending radiographs help you analyze a curve?
If not much change with lateral bending = structural scoliosis
If the curve changes with lateral bending = non-structural
Who is at risk for curve progression?
A spine that is still growing!!