L12 GI Tract
1/252
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
253 Terms
What are the parts of the oral cavity?
lips, teeth, tongue
What are the parts of the stomach?
Cardia, fundus, body, pylorus
What are the parts of the small intestine?
duodenum
jejenum
ileum
Accessories of the GI system
salivary glands, live, gallbladder, pancreas
Digestive system function:
ingest food and water
absorb water and nutritive substances
expel solid wastes
mucosa: secretion, barrier, immunologic protection
Oral cavity structures function
Structures: lips, teeth, gingiva, gum, palate, tongue, salvary glands, lymphoid tissue
Function
receives, chews and moistens food
enzymes begin the digestion process (process food in mouth)
Oral mucosa
lining mucosa: nonkeratinized stratified squamous
masticatory mucosa: keratinized stratified squamous (resist abrasion)
specialized mucosa: nonkeratinized stratified squamous with taste buds
oral cavity components
epithelium
lamina propria → minor salivary glands (always secrete)
muscle → voluntary manipulation
secretory products
lymphatic tissue - diffuse, nodules, tonsils
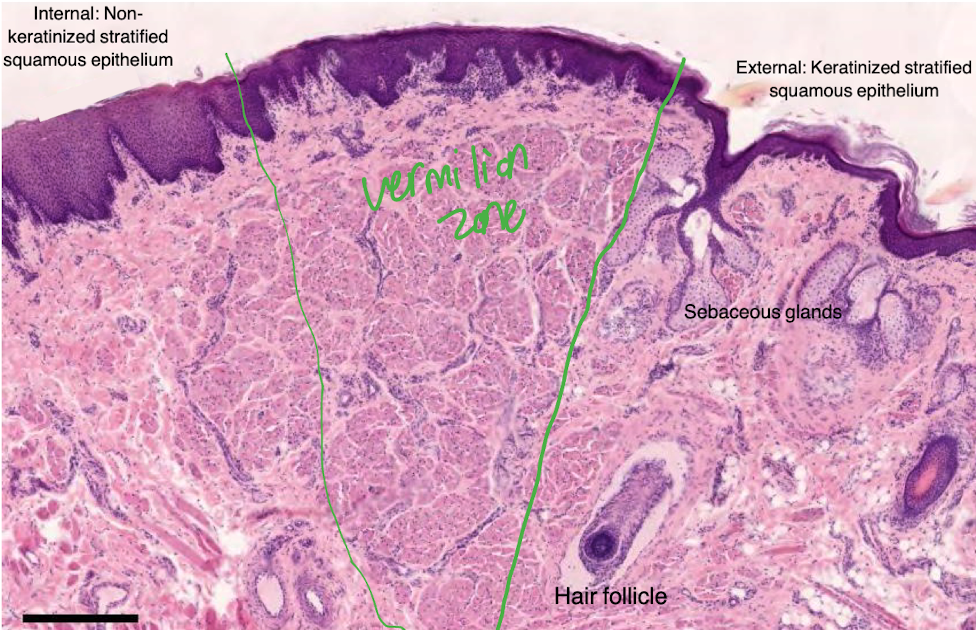
The lip
Internal region: stratified squamous nonkeritinized (has minor salivary glands)
Vermilion zone: stratified squamous, slightly keritinized (has blood vessels)
External region: stratified squamous, keritinized (has hair follicles and sebaceous glands)
Vermilion zone of lip
no sweat or sebaceous glands (need moisturizer)
underlying CT is rich in sensory innervation and capillaries (pink colour)
Can enamel be recplaced?
no
Enamel
96-98% calcium hydroxyapatite
integrity maintained by saliva
secreted by ameloblasts
acellular mineralized material
Dentin
dense, calcified tissue, forms bulk of tooth
secreted by odontoblasts
70% calcified hydroxyapatite, 30% collagen type 1
harder than bone
support enamel
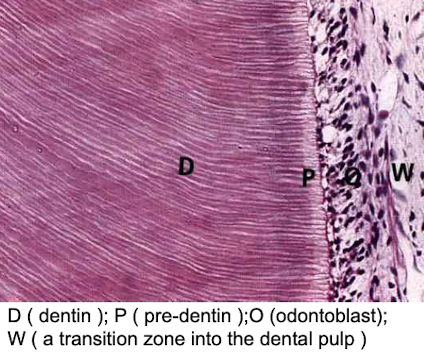
Pulp cavity
consists of delicate connective/supportive tissues
highly vascular
rich nerve supply (myelinated pain fibers get unmyelinated in pulp, extend into dentinal tubules, contact odontoblastic processes - sensory receptors for dentin
Cementum
65% mineralized, similar to bone
covers root, secreted by cementoblasts
reacts to compressive forces against alveolar bone and reacts by reabsorbing old bone and depositing new bone
keeps root in close contact with socket and alveolar bone
site of attachment for periodontal ligament/membrane to alveolar bone
What is the function of the periodontal ligament?
permits limited amounts of movement → shock absorber
derived by mesenchyme
dense collagenous tissues (collagen fibers called sharpey’s fibers → run obliquely down from cementum to alveolar bone)
What happens if there is a problem with the periodontal ligament?
issues = tooth exfoliation
What type of gland is a salivary gland?
exocrine gland
retain connection with surface epithelium by ducts that have glandular secretions reach the surface
Major salivary glands
pair of parotid, submandibular, and sublingual glands
regulated secretion in response to neural stimulus
parasympathetic activity (rest and digest)
Minor salivary glands
numerous in mucosa of oral cavity, in tongue, cheeks, lip, soft palate
continuous secretion
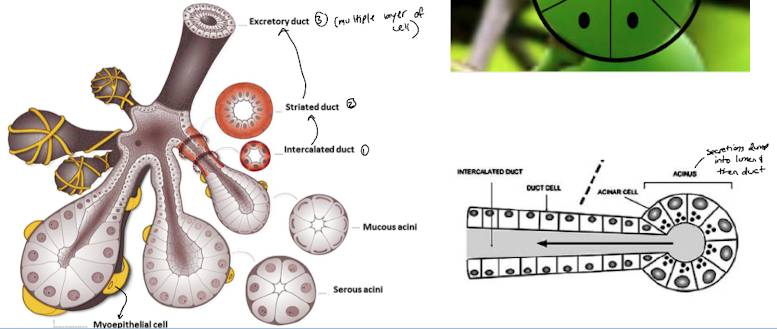
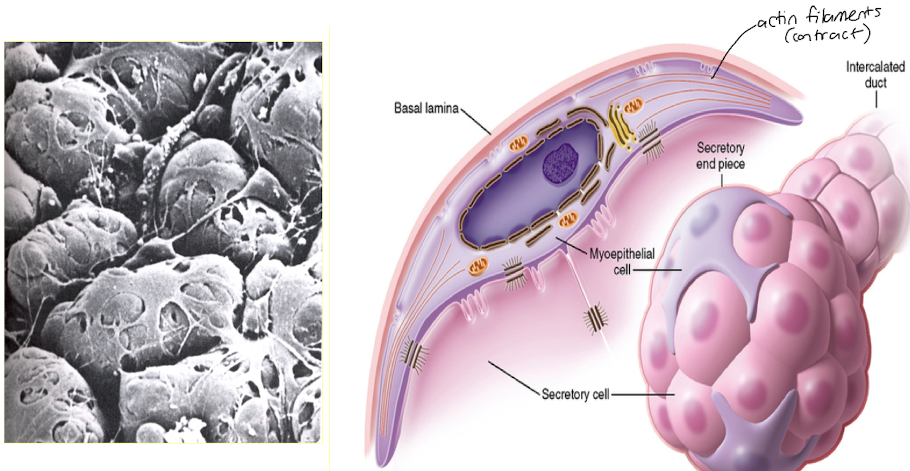
How are salivary glands organized?
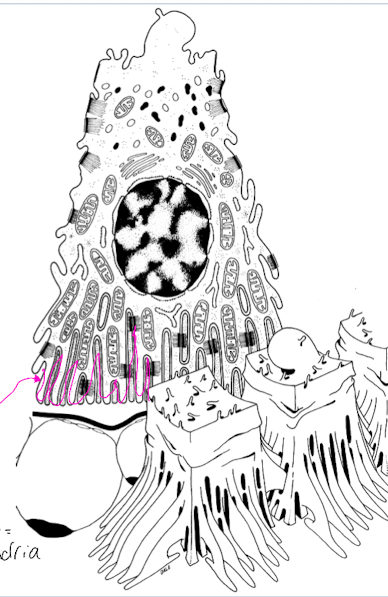
acinus (sac of cells) → make secretions
myoeptihelial cell → can contract, squeeze contraction into duct
intercalated duct, striated duct, excretory duct
Gland development
epithelium sits on a basement membrane supported by mesenchyme
basement membrane breakdown and epithelial cells migrate to underlying mesenchyme (mesenchyme cells and epithelial cells communicate with eachother)
epithelial cells de-differentiate into duct and secretory cells
lumen is constructed and differentiation continues
Secretory portion of gland structure
either sac like (acinar/alveolar) or tube-like (tubular)
also intermediate configurations (tubuloacinar or tubuloalveolar)
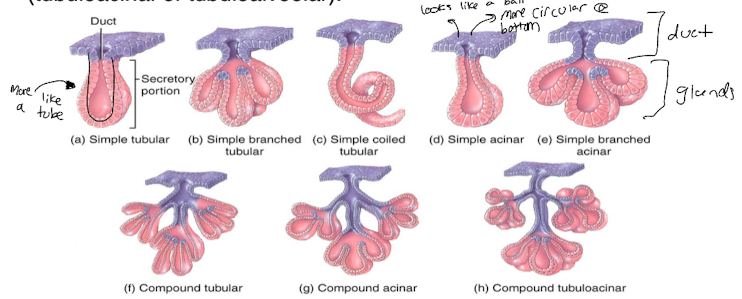
Structure of excretory duct
Simple: unbranched duct system (ex: sweat gland)
Compound: branched duct system (ex: salivary glands and pancreas)
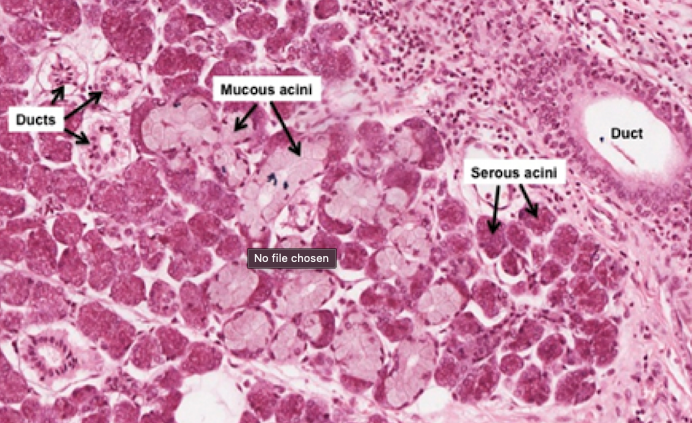
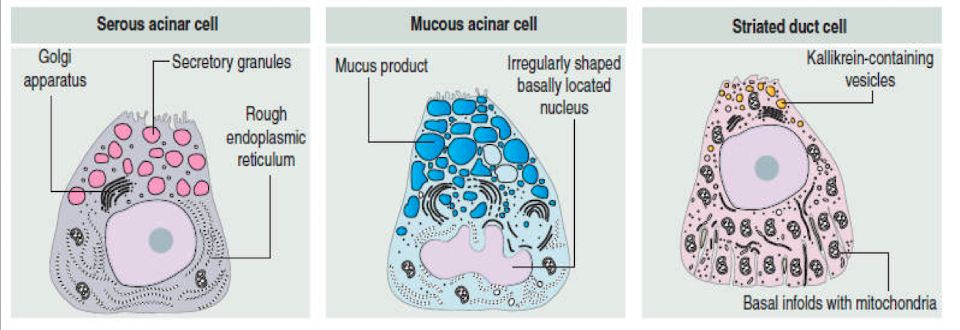
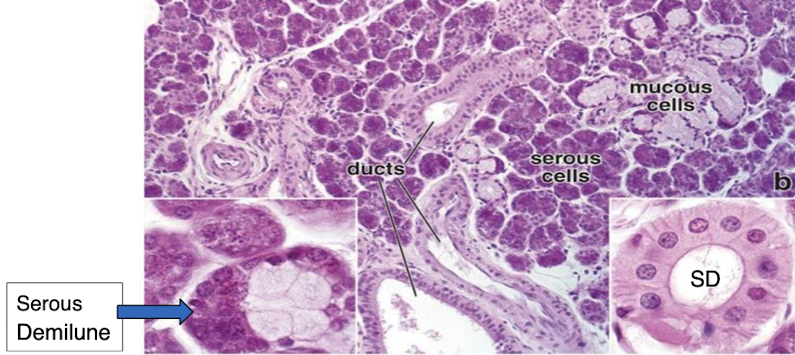
Classification of acinar glands
serous cells: protein rich secretory granules, pyramidal shape, round nuclei, eosinophilic
mucous cells: synthesize and store mucinogen granules, cuboidal to columnar, flattened nuclei, pale colour washed out stain
Mix of serous and mucous cells → serous demilune
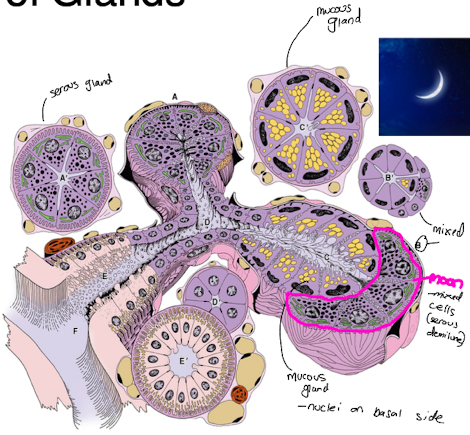
Organization of ducts in glands
lobe → salivary glands surrounded in a capsule of CT and divided into lobes
lobules → CT divides lobes into lobules
intercalated discs → join ducts together to form larger ducts, connect to acinar
striated duct → cuboidal to columnar epithelium
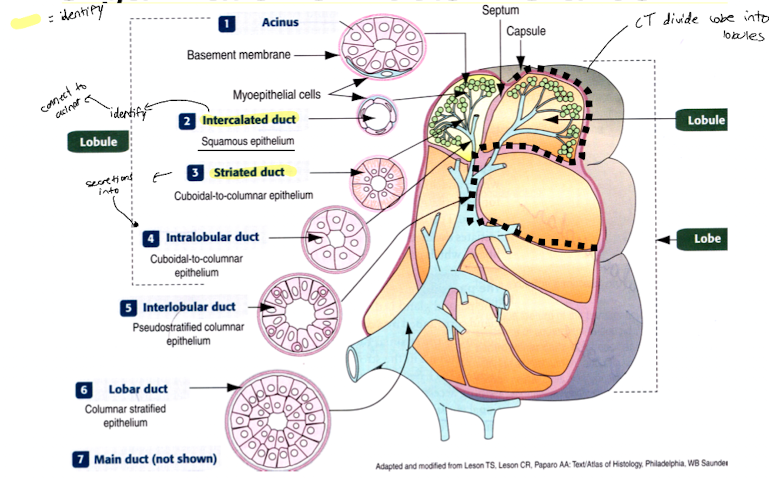
Intercalated ducts
secretion of the acinus enters the intercalated duct, lined by simple squamous to low cuboidal epithelium
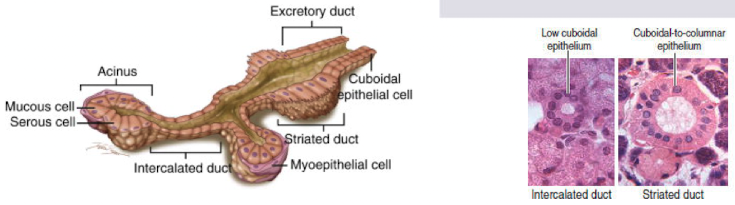
Striated duct
lined with tall cuboidal or low columnar cells
nuclei towards the center of the cell
basal portion present cell membrane interdigitations (foldings) and mitochondria in between the foldings
increase SA of pumps and mitochondria
Production of hypo-osmotic saliva
acinar cell makes saliva and dumps it into the lumen continuous with the intercalated duct and it goes to striated duct
acinar cell actively pumps Na+ and Cl- which are resorbed in the striated duct
Kallikrein is a protease released into striated duct that modifies proteins in saliva
bicarbonate is released into striated duct to neutralize the acid and create buffering capacity
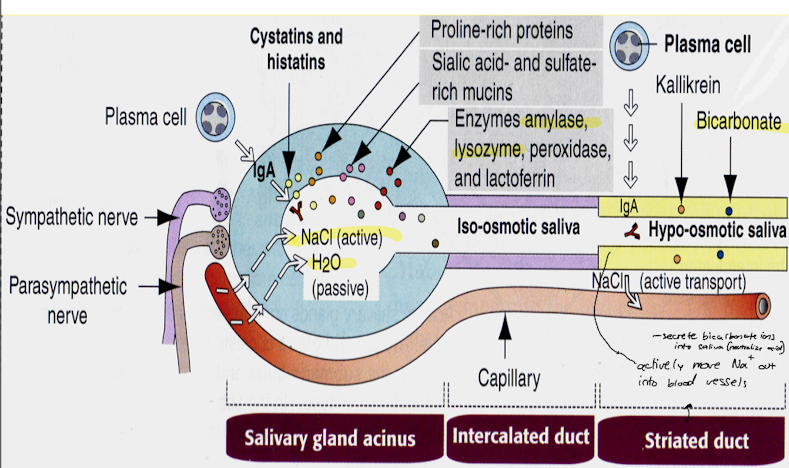
Striated (intralobular) duct
striations at basal portion
sodium ions are reabsorbed from raw saliva to produce hypotonic saliva (less sodium and chloride, more potassium and bicarbonate)
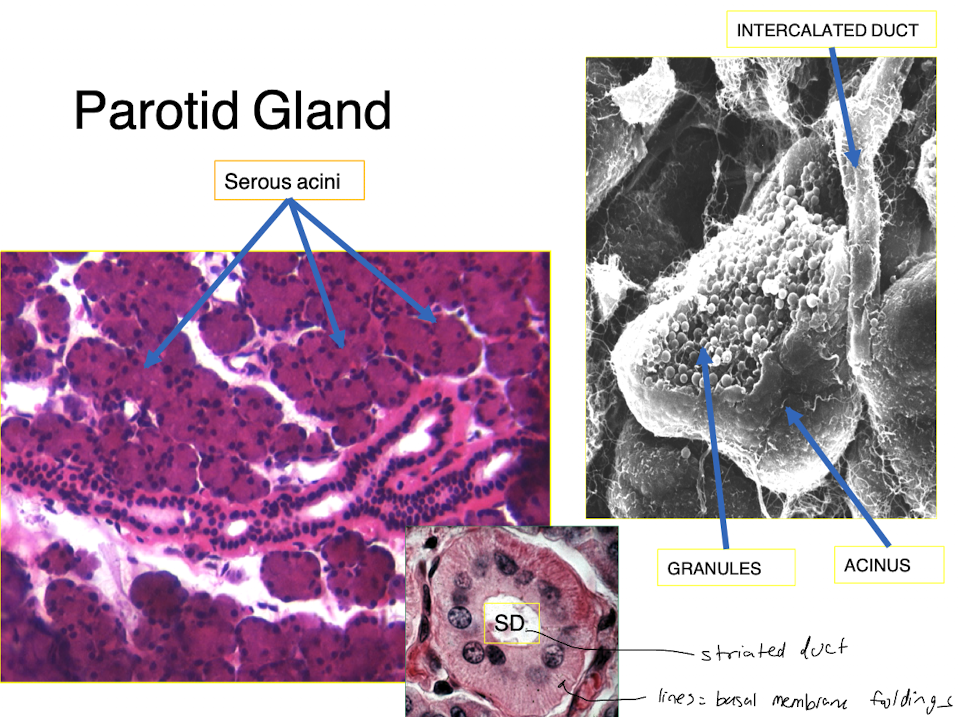
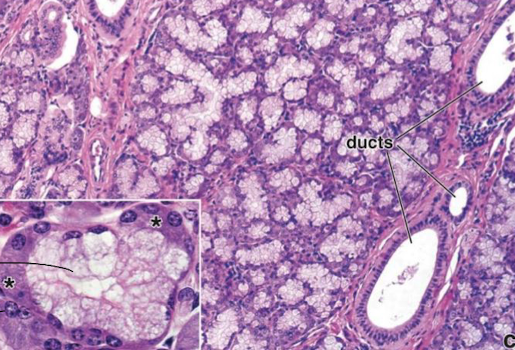
Parotid gland
tubuloalveolar gland
serous acini produce thin water secretion rich in enzymes and antibodies
25% of alkaline salivary volume is secreted by parotid gland
Sublingual gland
branched compound tubulo-acinar gland
mixed, MOSTLY mucous
secrete lysozymes to hydrolyze cell walls of bacteria
sublingual gland
Submandibular gland
branched compound tubolaracinar gland
mixed, mostly serous
mucous acini with serous demilune in a mixed gland
submandibular gland
What is Waldeyer’s ring?
in tonsils (first organ of defense in oral cavity)
an interrupted circle of protective lymphoid tissue at the upper ends of the respiratory and alimentary tracts
Taste buds structure
specialized epithelial structure
pale staining, barrel shaped, lie perpendicular to epithelium
each taste bud has receptors for all 5 tastes
Where are taste buds found?
mainly on dorsal surface of tongue

Neuroepithelial/sensory cells in taste buds
elongated cells, microvilli
tight junctions with neighbouring cells
at bases, they form synpases with CN VII, IX, and X (7, 9, 10)
Sustentacular/supporting cells of taste buds
slender, microvilli
do not synapse with nerve cells
Basal cells of taste buds
small cells located near basal lamina
stem cells for the supporting and sensory cells
How do we taste?
tastant binds with a TR1 or TR2 receptor
G proteins and secondary messengers are activated and bind to G complex
depolarization
calcium is released and triggers neurotransmitters from taste cell
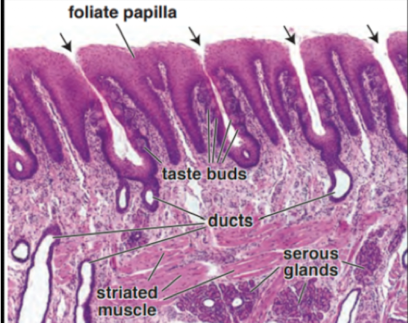
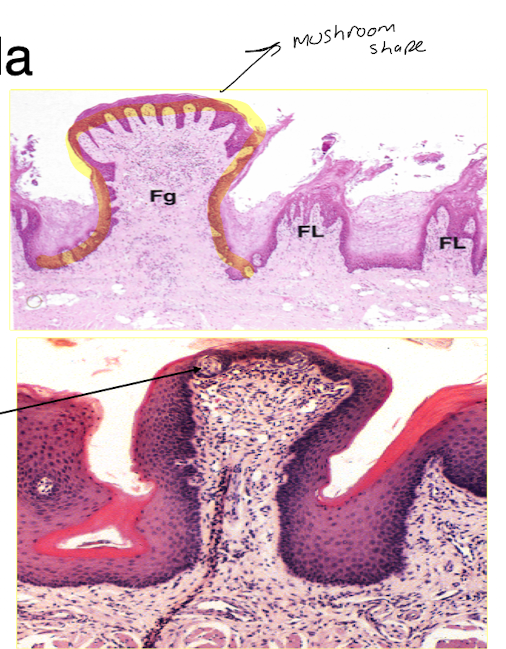
Foliate papillae
disappear as we get older (may be vestigial), well defined in infants and youth
occur on lateral edge of tongue
taste buds found along lateral wall of furrows
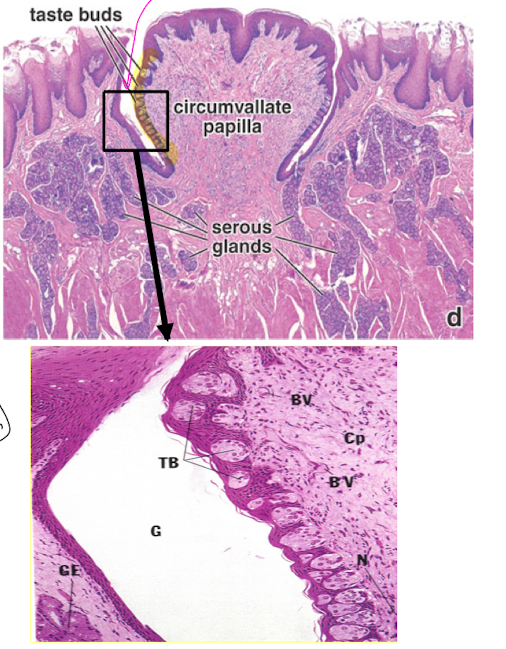
Circumvallate papillae
largest, 8-12 found anterior to sulcus terminalis
each is surrounded by a gutter/moat/rampart
taste buds on lateral wall (about 250 on each)
serous glands of Von Ebner found in CT around papillae
Fungiform papilla
look like mushrooms
concentrated in anterior portion of tongue
narrow stem, broad round top that projects above surface, red colour
taste buds are on stratified squamous on dorsal surface
only a few taste buds on dorsal
Filiform papillae
most numerous, conical structures on anterior 2/3 of tongue
NO taste buds
keritinized simple squamous
mechanical function (ex: licking)
white in colour
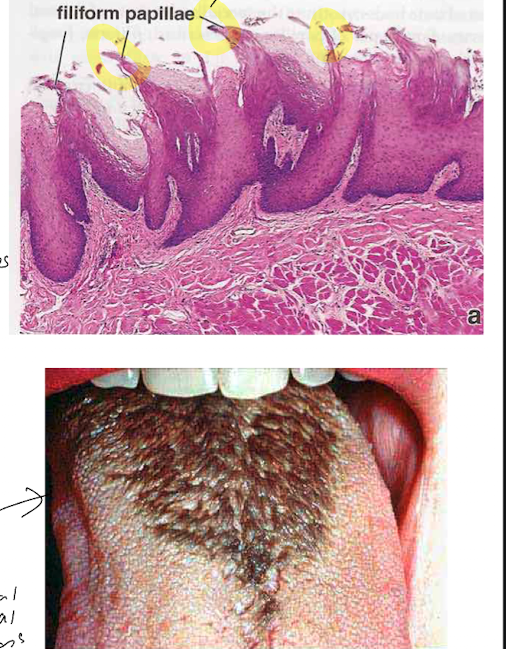
Hairy tongue
patient has dark hypertrophied filiform papilla with bacterial colonies on it
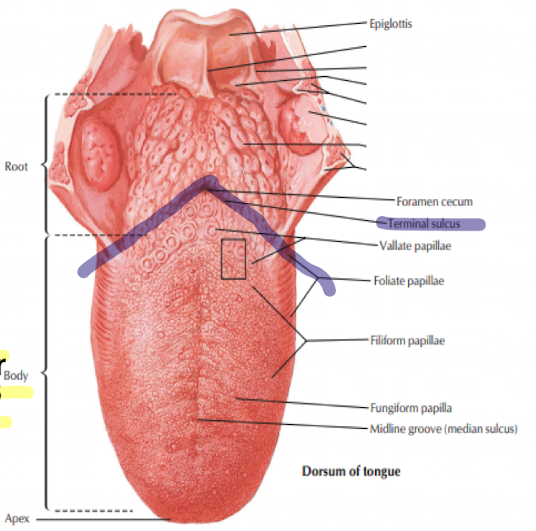
Dorsal surface of tongue
bottom of tongue
circumvallate papillae (on v-shaped teminal, Ebner’s glands)
foliate papillae (not lot in human)
fungiform papillae (on margin of tongue)
filiform papillae (no taste buds, increase friction between tongue and food)
The tongue
skeletal muscle
helps in mastication, swallowing, speech, taste, temp, pain and touch perception
dorsal and ventral surface
How is the tongue divided?
Dorsal surface: anterior 2/3 and posterior 1/3
V-shaped sulcus terminalis
Tongue histological features
Core: formed by intrinsic, very vascularized skeletal muscle
Mucosa: stratified squamous on doral and ventral
Lamina propria: CT, many blood vessels, lymphatics and nerves, lingual salivary glands

Mumps
swollen, painful salivary glands
fever and sometimes orchitis, pancreatitis, etc.
1/3 infected people do not show symptoms
effective vaccine since 1967
Salivary duct cysts
Epithelial lined cavity filled with mucus and fluids
Sialolithhiasis
salivary stones
calcium salts deposited around debris
Sialodentitis
inflammation of salivary glands because of mumps, influenza, coxacki virus, or systemic disease (Sjogren’s)
Pleomorphic adenoma
large tumour from salivary gland

Saliva functions
protection (fluid lubricant with imunoglobulins and calcium binding proteins))
antimicrobial (lysozymes, antibodies, lactoferrin)
Buffering (HCO3 and PO4 and saline maintain pH and neutrolize)
Tooth integrity: source of calcium and phosphate → increases enamel hardness in new erupted tooth
Digestion: moisten bolus of food, amylase, lingual lipase
Taste: solubilizes molecules sensed by taste buds
Myoepithelial cells
at base of acinar cells
between acinar cells and their basal lamina
have actin filaments that contract
What is the main cell type in the parotid gland?
serous
has myoepithelial cells
numerous intercalated discs
moderate striated ducts
What is the main cell type in the submandibular gland?
serous mainly (some mucous)
has myoepithelial cells
medium intercalated discs
abundant striated ducts
What is the main cell type in the sublingual gland?
mixed, mostly mucous
has myoepithelial cells
not many intercalated discs
not many striated ducts
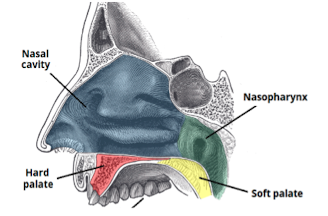
Does the palate have an oral and nasal surface?
Yes
What structure shuts food off from going into the air tract pathway?
epiglottis
What type of palate is at the roof of the oral cavity
Hard palate
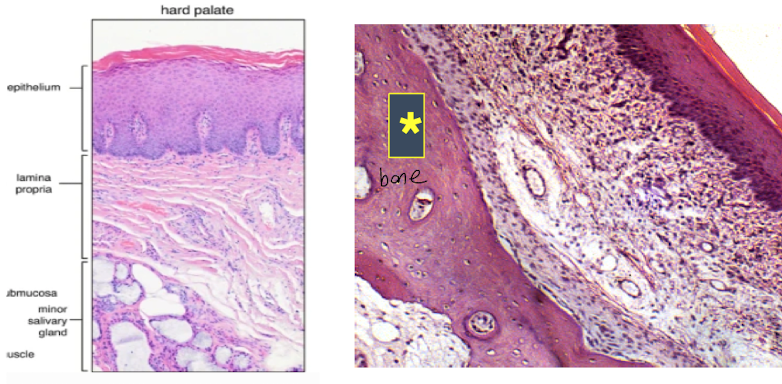
Hard palate tissue
keritinized stratified squamous supported by LP
Upper layers supported by spicular bone
Soft palate structure and function
nasal and oral surface
involved in talking, breathing and swallowing
Soft palate support tissue
supported by skeletal muscle
houses many secretory mucous glands
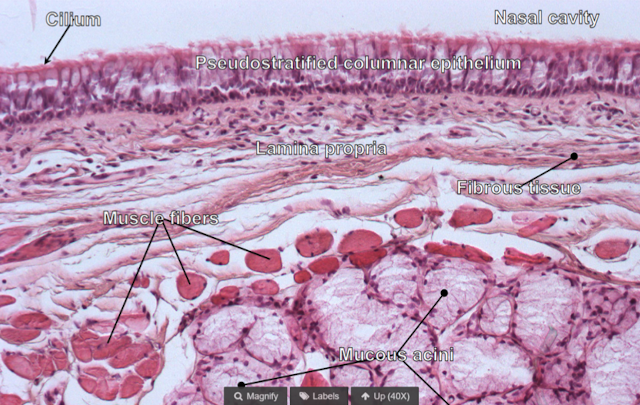
What type of epithelium is in the nasal surface of the soft palate?
pseudostratified ciliated columnar epithelium with mixed glands
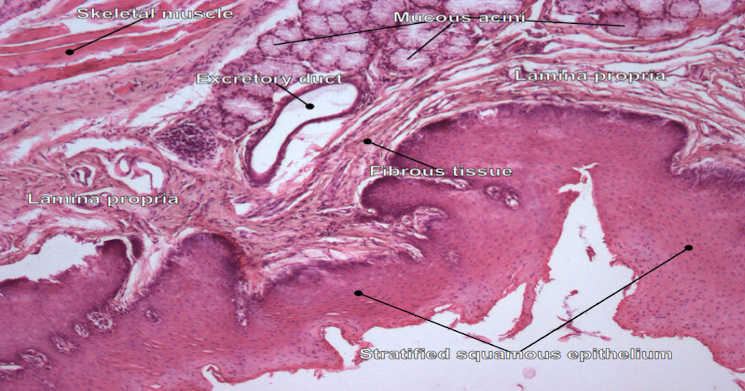
What type of epithelium is in the oral surface of the soft palate?
nonkeratinized stratified squamous
wet kind
interdigitated with LP under
Pharynx location and function
extends back from oral cavity
passage for food that goes through pharynx to esophagus
nasopharynx, oropharynx, hypopharynx
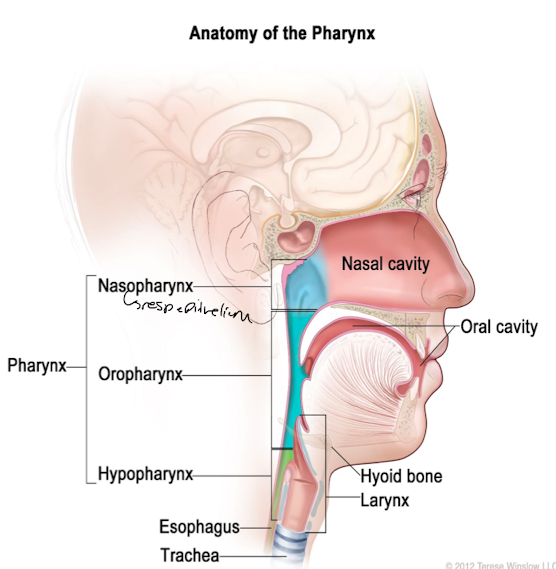
Pharynx mucosa and submucosa tissue
MUCOSA: wet nonkeratinized stratified squamous epithelium with LP rich in elastic fibers
SUBMUCOSA: CT between LP and underlying skeletal muscle, occasional seromucous glands that can extend into muscle
What structure does stroke affect if issue in coordination of swallowing muscles?
Pharynx
What are the 4 layers of the GI tract?
mucosa
submucosa
muscularis externa
serosa/adventitia
What tissues are in the mucosa? (GI tract)
epithelium lining
lamina propria (CT)
muscularis mucosae (smooth muscle)
What tissues are in the submucosa? (GI tract)
glands
vessels with nerve plexus
What tissues are in the muscularis externa? (GI tract)
inner circular layer and outer longitudinal layers of smooth muscle
nerve plexus in between
What tissues are in the adventitia/serosa (GI tract)?
loose CT on outside
simple squamous epithelium (mesothelium)
adventitia - secures organs to surrounding tissue
serosa - cover organs
Mucosa functoins
epithelium → barrier + absorptive functions
mucosa → secretory function (enzymes, hormones) and contains glands, BV, lymphatic tissue
muscularis mucosa → allows fine adjustments in mucosa by making ridges and valleys (make longitudinal folds → elastic fibers recoil and move food)
Submucosa functions
within CT there are nerves (enteric nervous system), blood vessels, glands and lymphatics
loose CT allows folding of overlying mucosa to form folds
Muscularis externa function
contracts, mixes, and propels contents
can cause bowel movements
Esophagus function
strong muscular tube, conveys food from oropharynx to stomach
How does swallowing work?
initiation is a voluntary act with skeletal muscle of oropharynx
followed by strong peristaltic reflex in upper part of esophagus → convey bolus of food and fluid to stomach
What are the diff muscles in each third of the esophagus?
upper 1/3 = skeletal muscle
middle 1/3 = smooth + skeletal
lower 1/3 = smooth involuntary muscle
Esophagus lumen tissues
thick, protective, non-keratinized stratified squamous epithelium
lamina propria
muscular mucosa under lp
Esophagus submucosa tissue
very loose, fair amounts of elastic fibers, has seromucous glands
Esophagus muscularis externa tissue
outer longitudinal and inner circular layer
smooth muscle
Esophagus submucosa layer tissue
peripheral ganglia between layers of muscularis
very thin, hard to see
How does epithelium change from esophagus to stomach?
drastic change from stratified squamous in esophagus to simple columnar in stomach
withstands acidity
seromucous glands into stomach for short distance, then disappear
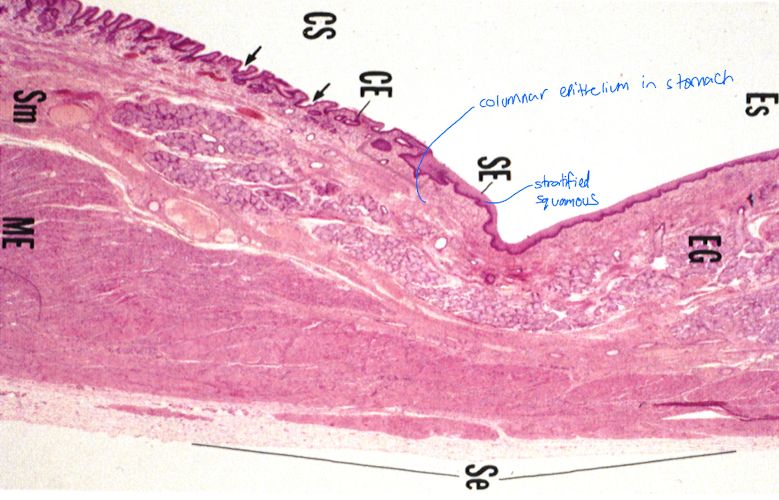
Barrett esophagus
intestinal metaplasia (columnar replace squamous) of distal esophagus
patches of red, velvety mucosa extending up from gastroesophageal junction
increases risk of esophageal adenocarcinoma (cancer)
What are the 3/4 regions of the stomach?
cardiac region (superior opening of stomach)
fundus and body (major part of stomach)
combine bc same tissues histologically
pyloric part (funnel-shaped outflow)
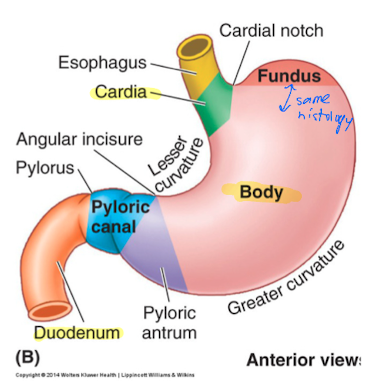
What are rugae?
folding of mucosa in wall of stomach body
folds when stomach is empty and disappears when stomach is full
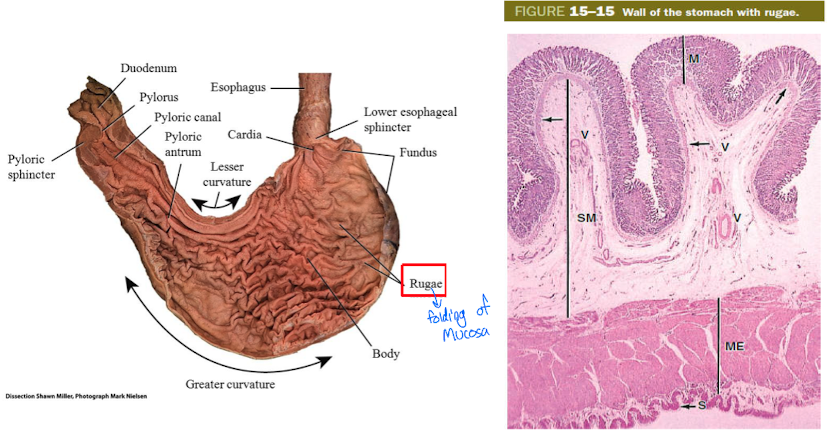
What makes rugae possible?
The contractions of muscularis externa and loose submucosa
What kind of organ is the stomach?
exocrine-endocrine organ
Stomach function
mechanically churn food and make chyme
digestion
some absorption in stomach (water, ions, alcohol, aspirin, caffeine)
produces pepsin, HCL, and gastic lipase to help digest proteins, triglycerides
What does the stomach produce?
pepsin
mucous
lysozyme
gastrin
somatostatin
Which structure has 3 layers in the muscularis externa?
The stomach, has additional oblique muscle layer
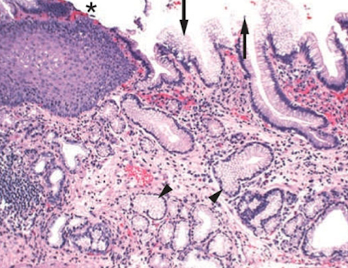
Gastric pits
in the stomach and connect to gastric glands in mucosa
lined by surface mucous cells
What makes up the gastric mucosa?
gastric pits
gastric gland isthmus
gastric gland neck
gastric gland base
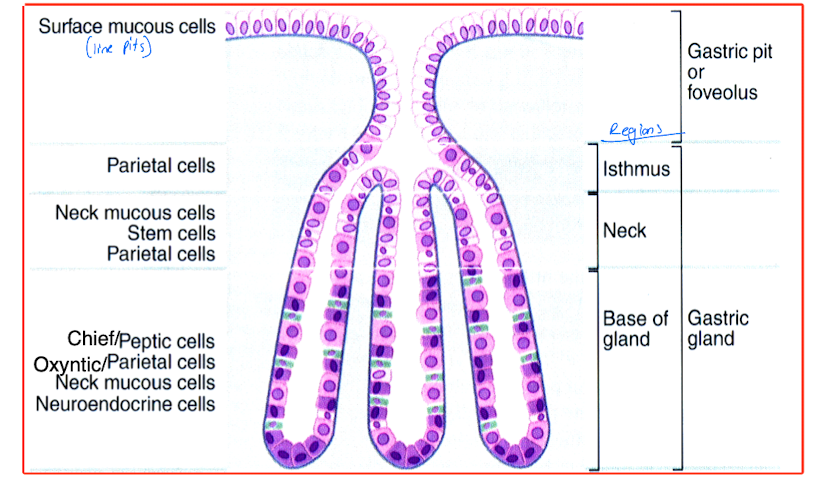
What cells are in the gastric gland isthmus?
parietal cells
What cells are in the gastric gland neck?
neck mucous cells
parietal cells
stem cells (replenish cells at surface constantly exposed to stomach acid)