Urology
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
68 Terms
Define pollakiuria, hematuria, stranguria, and urinary incontinence
Pollakiuria = ↑ frequency
Hematuria = blood in urine
Stranguria = difficulty urinating
Incontinence = leaking urine/puddles
What key physical exam components are needed in dysuria cases?
Bladder palpation, perineal exam, rectal exam, penis/prepuce exam, vulvar palpation
What are the major differentials for dysuria in dogs?
Bacterial cystitis, urinary stones, and neoplasia(urithelial cell carcinoma - used to be called TCC)
How common is bacterial cystitis in dogs and cats?
Common in dogs, especially females(short & wide urethra)
Rare in intact males unless prostatitis
Very rare in cats (<2% LUTD), except older cats with CKD
What organisms commonly cause UTIs in dogs?
Most common: E. coli
Others: Staph, Strep, Enterococcus, Enterobacter, Proteus, Klebsiella, Pseudomonas
Usually one organism; 20–30% mixed infections
Normal source = intestinal or skin flora
What are the updated diagnostic highlights?
Need clinical signs + pyuria
Culture recommended for all suspected bacterial cases
Define bacteriuria, subclinical bacteriuria, and bacterial cystitis
Bacteriuria: bacteria present in urine
Subclinical bacteriuria: bacteria without clinical signs
Bacterial cystitis: bacteria + clinical signs of LUTD
How are bacterial cystitis types classified?
Sporadic: <3 UTIs/year
Recurrent: ≥4 UTIs/year
Is UA necessary?
This slide prompts the question—later slides elaborate. Answer: yes, UA is part of standard workup
How reliable is a urine dipstick in dogs?
Cheap & available
Only reliable for ketones & protein
NOT reliable for USG, pH, neutrophils
Not reliable to detect infection
What does urine sediment tell us?
Pyuria = inflammation can be bacteria, stones, or cancer
Pyuria + bacteriuria → infection likely
Bacteriuria alone ≠ cystitis
Epithelial cells ≠ tumor
When is urine culture recommended?
Recurrent suspected UTI
Multiple recent antibiotic courses
Multiple hospitalizations
Raw food diet (higher resistant organism risk)
What can radiographs detect in dysuria cases?
Bladder size
Radio-opaque stones (CaOx & struvite)
90% visible on digital radiography
Pull forelimbs forward → better urethra view
What are radiograph limitations, and when do we use contrast?
Limitations:
Can't determine stone type
Urethra obscured by bone
Tumors not seen unless mineralized
Contrast studies: Urethrocystogram under GA with catheterization
What can ultrasound evaluate?
Bladder stones, mass, wall, Upper urinary tract
Limitations:Urethra obscured by bone
Overestimates stone size
When do you need imaging?
High suspicion of stones
Possible obstruction
Systemic illness
When is bloodwork needed?
Only if:
Systemic signs (fever, pyelonephritis, obstruction)
Low USG suggesting kidney disease
What human evidence supports NSAIDs alone?
RCT: ibuprofen vs ciprofloxacin in women
2/3 recovered without antibiotics
No difference in relapse or symptom resolution
→ UTIs often self-limiting in women; symptom control sometimes enough
When can we consider NSAIDs instead of antibiotics in dogs?
Extremely reliable owners
Dogs that cannot tolerate antibiotics
What are first-line antibiotics for cystitis?
Amoxicillin 11–15 mg/kg q12h, less likely to cause D
Amoxicillin-clavulanate 12.5–25 mg/kg q12h
TMS 15–30 mg/kg q12h (risk of side effects but acceptable short-term) can get KCS, or acquired endocrine problems
When are fluoroquinolones or 3rd gen cephalosporins appropriate?
When first-line drugs not options → for Gram -
When PO or q12h dosing not possible
If concurrent tissue infection(like prostate)
IMPORTANT → differentiate need vs convenience
When is empirical treatment reasonable?
Reasonable: 1st episode
NOT recommended:
2nd episode
Multiple antibiotics
Multiple hospitalizations
Raw food diet
How long should cystitis be treated?
Sporadic: 3–7 days
Recurrent: longer, individualized
Stop when: clinical signs resolve, sediment normal, negative culture (if performed)
What determines when to stop antibiotics?
Symptom resolution
Sediment normalization
Negative culture (if used)
How fast should improvement occur on correct antibiotics?
Within 1–2 days
What questions should be asked on recurrence?
Did bacteria evade treatment?
Did bacteria easily enter?
Did we treat long enough?
Could it be stones or tumor instead?
What are pros and cons of cystocentesis?
Pros: avoids contamination
Contraindications: bladder tumor, thrombocytopenia, coagulopathy
What colony counts indicate infection per collection method for urine culture?
Cystocentesis: ≥1000 CFU/mL
Catheter (male/female): ≥100,000 CFU/mL
Voided: not recommended
Are voided samples reliable for urine culture?
Only if no other option—must evaluate growth level, species, purity, cytology, and clinical signs
How should urine samples be stored?
Cysto: process <24h refrigerated
Voided: <12h refrigerated
How to treat the 2nd episode of UTI?
Start antibiotics
Often same drug until results
Duration usually longer
What interpretation questions should be asked after culture?
Does organism fit with patient?
Does result match clinical response?
What drugs are appropriate?
Do we need systemic therapy?
What if culture shows intermediate, resistant, or sensitive bacteria?
Intermediate:
Clinical response → continue
No response → switch drug
Resistant:
Clinical response → continue
No response → reconsider compliance/diagnosis
Sensitive:
If no clinical response → check compliance first
Should subclinical bacteriuria be treated?
No, even in systemic disease or immunosuppression
Should multidrug-resistant bacteriuria be treated?
Not if asymptomatic — resistance alone is not an indication
How should recurrent UTIs be approached?
Incomplete response → investigate underlying cause
Reinfection (new pathogen) → look for predisposing factors
Relapse (same pathogen) → reevaluate dose, regimen, compliance
Treatment:
Reinfection: short course 3–5 days
Relapse/persistent: 14+ days, choose tissue-penetrating antibiotics
When should intra-therapy or post-therapy cultures be done?
Only for long treatments >2 weeks
Intra: day 5–7
Post: 5–7 days after stopping antibiotics
Sporadic cystitis with resolved signs → no post-culture needed
Should asymptomatic bacteriuria be treated before elective surgery (e.g., CCL repair)?
No.
Study showed:
SBU 6.5% prevalence
No difference in surgical site infections
SSI organisms differed from urine isolates
→ Screening and treating SBU is not beneficial
What are the most common canine urolith types and their proportions?
85–91% are struvite(can dissolve with diet) + calcium oxalate(will not dissolve, need sx)
CaOx: 42–45% (98% of feline and 50% of canine upper-tract calculi)
Struvite: 43–44%
Purine: ~5%
Ca phosphate: 1%
Cystine: ~1% (increasing)
Silicate: <1%
What factors help estimate urolith type?
Age/sex
struvite → young animals, females due to infection
calcium oxylate → older animals, males
crystals, urine pH, stone shape, breed, underlying disease, and presence of infection
Which stones show strong sex predispositions?
CaOx much more common in males
Struvite far more common in females
Urate more male-associated
Cystine overwhelmingly male
Does finding crystals on UA mean the dog has stones?
No. Crystals do not reliably indicate stones
Why are urinary crystals unreliable diagnostically?
They vary with diet, infection, storage time, temperature, pH, contaminants, and iatrogenic causes (contrast, allopurinol). Fresh, unrefrigerated urine is needed; crystals are rarely clinically significant
Which stones form in acidic vs alkaline urine?
Alkaline (>7): Struvite, Ca phosphate (rare)
Acidic (<7): CaOx, ammonium urate, cystine, silicate, uric acid
Also note: urine pH at stone formation may differ from pH at time of exam
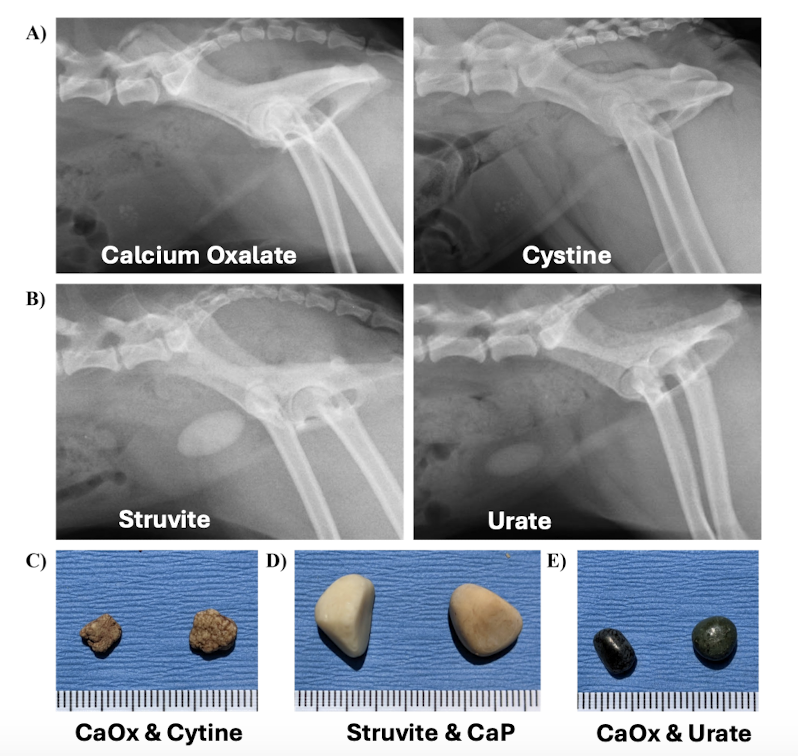
What are typical appearances of CaOx, cystine, struvite, and urate stones on imaging?
Images show:
CaOx: highly radiopaque, irregular
Cystine: moderately opaque, smoother
Struvite: opaque, smooth
Urate: less radiopaque/variable
Which breeds are predisposed to which stones?
Urate: Dalmatian, Bulldog, Pitbull, Russian terrier, Giant Schnauzer
Struvite: Yorkie, Lab, Dachshund, Shih Tzu, Mini Schnauzer
CaOx: Yorkie, Lhasa Apso, Mini Poodle, Shih Tzu, Schnauzer, Bichon
Cystine: Bulldog, Dachshund, Newfoundland, Mastiff, Lab
Silicate: Australian cattle dog, Chihuahua, Corgi, GSD, Collie
What important genetic mutations are linked to urate and cystine stones?
Urate: SLC2A9 mutation (Dalmatians; autosomal recessive).
Cystine: SLC3A1 or SLC7A9 mutations depending on breed.
Type III cystinuria: androgen-dependent, only males, improved by castration, no gene mutation identified.
Testing available via PennGen
What systemic diseases predispose dogs to specific uroliths?
Cushing → CaOx
Hyperparathyroidism → Ca phosphate
Portosystemic shunt → urate
Renal hematuria → dried blood “stones”
Bacterial cystitis → struvite
What non-disease factors influence stone formation?
Prior surgery (≈9.5% recurrent stones are suture-induced; increased to 18.5% in 2018, stones grow on sutures in bladder), obesity (not proven), water mineral content, lack of Oxalobacter formigenes
What is required for struvite formation in dogs?
Usually secondary to urease-producing UTIs (Staph pseudintermedius, Pseudomonas, Klebsiella, Ureoplasma, Proteus, Corynebacterium). E. coli UTIs have low struvite risk so don’t treat subclinical bacteremia
How does location and suspected type guide treatment?
Bladder + likely struvite → dissolution first
Bladder + NOT struvite → removal
Urethral obstruction → urgent removal
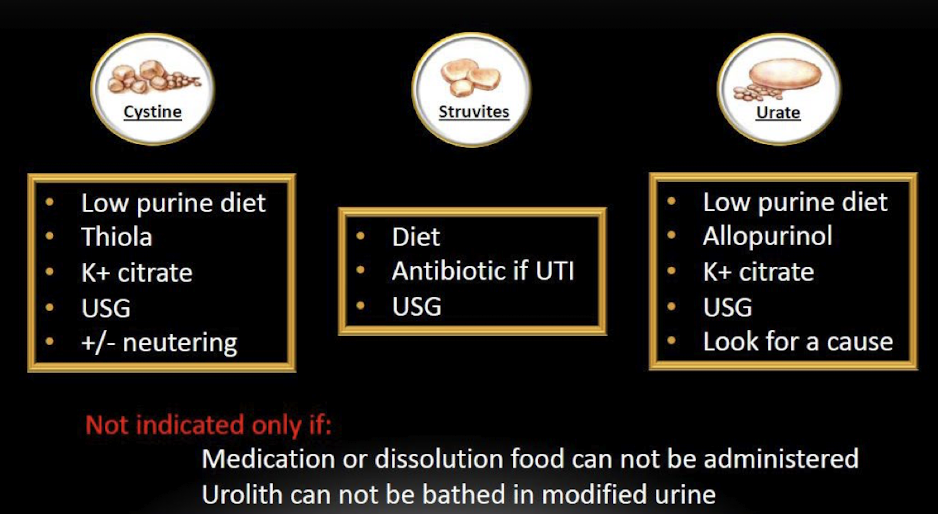
For which stones is medical dissolution effective, and what are the goals?
Very effective for struvite
Moderate for urate and cystine
Goals: reduce calculogenic salts, increase urine volume.
Requirements vary by type (low purine diet, thiola, antibiotics if infected, K-citrate etc.)
What are the key decision points in struvite dissolution flowchart?
Sex → infection status → presence of urease-producing bacteria → contraindications → dissolution vs removal → rechecks every 4–6 weeks
Does size affect dissolution success?
No
Should all stones be submitted for analysis?
Yes—always submit, even recurrences; results in ≤2 weeks
What are the main removal techniques and their pros/cons?
Surgery: invasive, long anesthesia, risk of incomplete removal (14%), suture-induced stones.
Non-invasive (preferred): voiding urohydropropulsion, endoscopic removal, lithotripsy → shorter stay, less pain
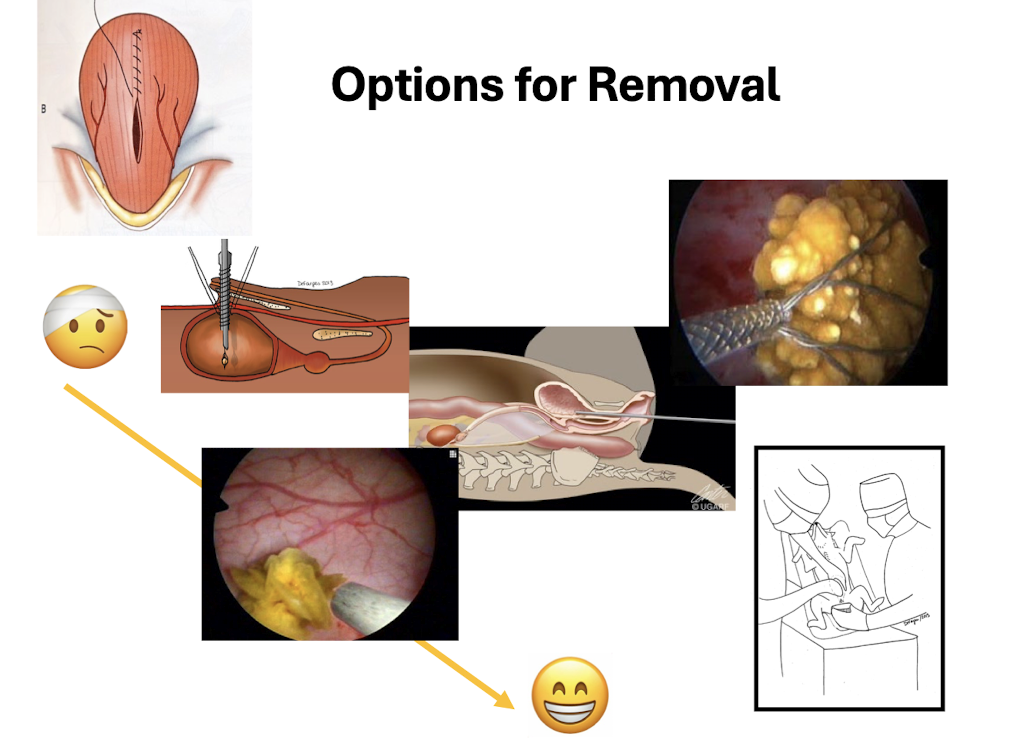
When is voiding urohydropropulsion indicated/contraindicated?
Indications: stones < urethral diameter, mainly females.
Contra: large or jack-shaped stones, male cats
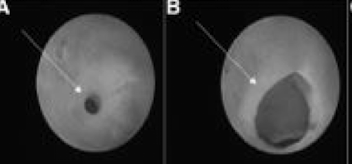
What are advantages and limitations of cystoscopy and lithotripsy?
Diagnoses strictures, bleeding sources, ectopic ureters; can remove/fragment stones.
Not feasible in male cats; >3kg females OK.
Laser lithotripsy effective in all females and most males; best in female dogs >4kg and male dogs >7kg
What is typical lithotripsy postoperative care?
5 days NSAIDs, same-day discharge, send stones for analysis
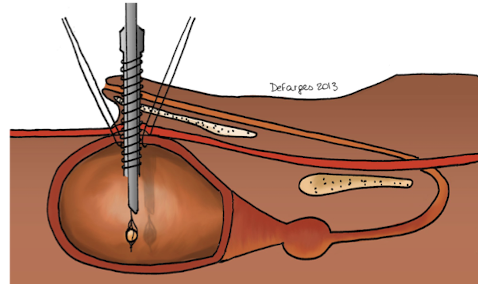
What is Percutaneous Cystolithotomy (PCCL) used for?
Minimally invasive percutaneous cystolithotomy for male dogs & cats under GA via small incision at bladder apex
What are differentials when dysuria persists with normal imaging & culture?
Urethral diseases: infiltrative disease, inflammation, or stricture; imaging may miss these; urethrogram or cystoscopy needed. Biopsy essential to differentiate TCC/SCC/leiomyoma vs proliferative urethritis
What is the role of Liquid Biopsy & BRAF testing in urinary tract tumors?
Detects cfDNA mutations in free-catch urine; >85% sensitivity, 100% specificity for urothelial & prostatic carcinoma; mutation present in 43–87% of UC cases
needs lots of urine, very good for diagnosing carcinoma, can do in general practice
Does BRAF mutation status affect survival?
In a 79-dog retrospective study, BRAF status did not significantly influence overall survival, though treatment type and tumor location did
What are features of proliferative urethritis in dogs?
Uncommon, mainly female dogs, presents as obstruction; 73% have UTI history; treatments include piroxicam/steroids; recurrence common; balloon dilation/stenting prolongs time to recurrence.
Can dx by vaginal or rectal exam, may be able to feel abnormal structure of urethral papilla.
Why might a male dog still obstruct after complete stone removal?
Possible urethral stricture—catheter won’t pass despite no stones
What can cause overflow incontinence following dysuria?
Male dog with urinary incontinence → Partial obstruction → enlarged bladder → detrusor atony(extreme) → overflow; requires imaging/cystoscopy
What are differentials for acute hematuria with a bladder mass on ultrasound?
Bladder tumor vs bladder hematoma
What are the major differential categories for dysuria?
Urethral disease: stones, stricture, tumor, proliferative urethritis
Bladder disease: cystitis, stones, mass/infiltration, hematoma