Introduction to Viruses & HIV/AIDS (Lecture 10)
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
What was the first discovered virus to affect humans and in what year?
Yellow Fever Virus; 1901
In nm, what is the size of HIV?
120 nm
Viruses are not “living things” but “_ of _”
“forms of life”
According to Kooning et al (2021), viruses are…
non-organismal mobile genetic elements, “replicators that encode structural protein encasing their own genomes”
What is the Nucleocapsid if the HIV virus made up of?
Caspid (capsomers) - the envelop/ external layer
Nucleic acid (DNA or RNA) - can be single or double stranded
Name the 6 steps of the life cycle of a virus.
1 attachment, 2 penetration, 3 uncoating, 4 gene expression and replication, 5 assembly, 6 release
The life cycle of a virus steps:
Entry involves attachment, in which a virus particle encounters the host cell and attaches to the cell surface, penetration, in which a virus particle reaches the cytoplasm, and uncoating, in which the virus sheds its caspid
Following the uncoating, the naked viral genome is utilized for gene expression and viral genome replication
Finally, when the viral proteins and viral genomes are accumulated, they are assembled to form a progeny virion particle and then released extracellularly
Virion assembly and the release from the cell constitute the exit
T/F The life cycle of the virus can occur slowly or quickly depending on the sort of virus it is?
True
Does HIV specifically target CD4 or CD8?
CD4
HIV is _virus
retrovirus
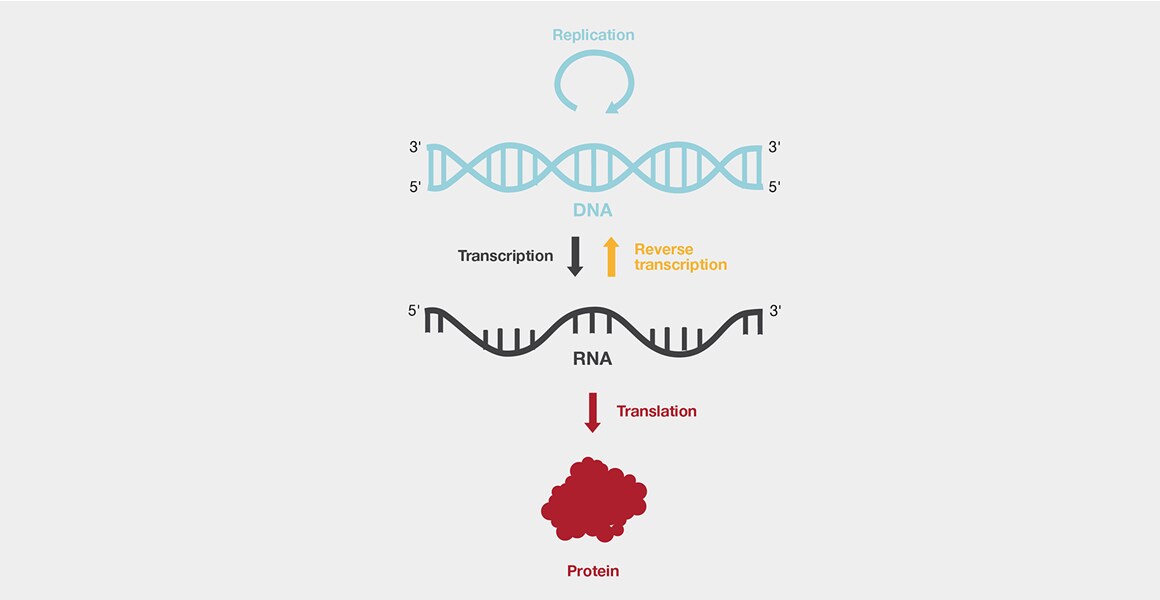
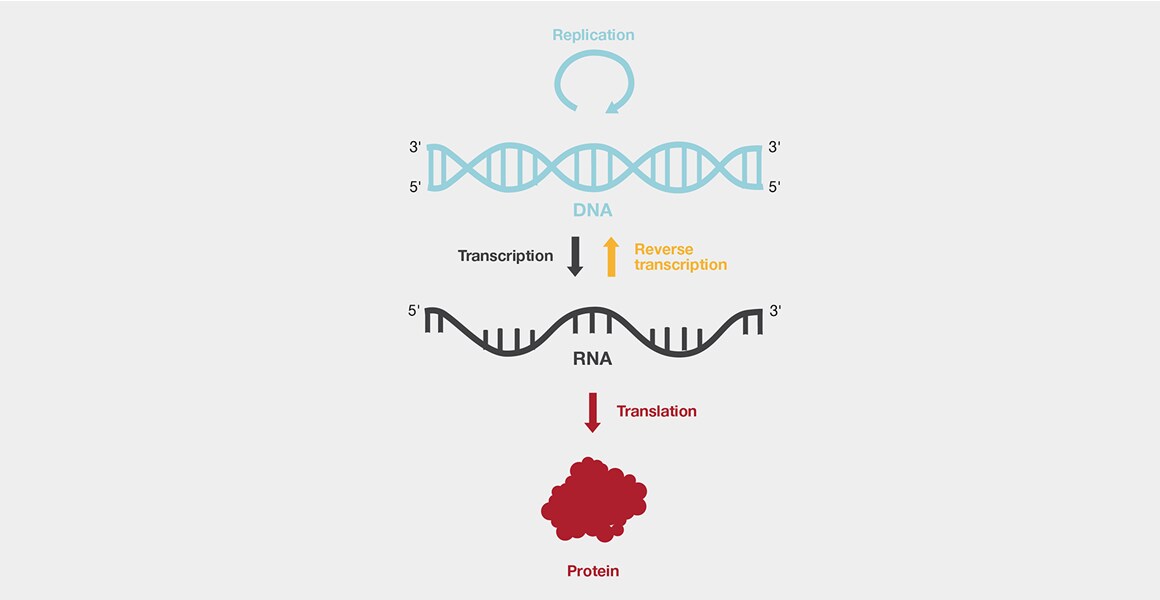
What does it mean when something is in the retrovirus family?
a family of RNA enveloped viruses that replicate in a host cell through the process of reverse transcription. It is also an oncogenic virus. (retro=reverse transcription)
What genus does HIV belong to?
“Lentivirus”
Was it HIV1 or HIV2 that’s is most common and cause of the HIV pandemic?
HIV1
HIV originated in what animal. Which then turned into a spillover event. Thus, transferring to humans.
Chimpanzees
humans kill for food
blood infects humans causing the spread
HIV1 viruses are categorized into 4 groups/ sub-types:
Main (M), Outlier (O), Non-M(N), and group P viruses
Each group originates from an independent cross-species transmission event (spillover) between non-human primates and humans
HIV1 is the most _ HIV type.
Cased recognized in
Virus identified in
Presents many sub-types (4)
common; 1981; 1983
HIV2 was discovered in 19_ and distributed mainly in _ . it is also less common and less _ than HIV1
1985; West Africa; virulent
The first human known to be infected with HIV was a man from _ (now the Democratic Republic of Congo) who had his blood stored in 1959 as part of a medical study.
Kinshasa
HIV was originally called what?
Lymphadenopathy associated virus (LAV)
Who termed the name Lymphadenopathy associated virus (LAV)?
Luc Montaginer (1983)
Human T cell leukemia virus types III was termed by who in 1984.
Robert Gallo
The human immunodeficiency virus was discovered at the Institute Pasteur by who
Francoise Barre-Sinoussi and Luc Mantagnier
In 2023, how many people were living with HIV
almost 40 million (39.9 million)
Which GP is needed to attach to the host cell and which GP is critical for the cell fusion process
gp 120 and gp 41
The primary targets of HIV are …
activated and memory CD4+ T helper lymphocytes of any subpopulation: Th1, Th2, Th17, Tregs, and Tfh (follicular T helper) cells
Th17, located primarily at barrier surfaces in the gastrointestinal tract, lung, and skin, and participating in mucosal, immunity are _ susceptible to HIV infection and became viral reservoirs
HIGHLY
To complete entry, HIV1 requires what kind of receptors?
co-receptors
What are the co-receptors that HIV1 need to enter the cell surface?
The C-C chemokine receptor type 5 (CCR5) or R5 and the C-X-C chemokine receptor type 4 (CXCR4) or X4
What are the Dendritic cells responsible for in terms of HIV transmission?
DC accumulate virus particles on their surfaces but usually do not internalize them They transport HIV to regions containing large numbers of its target cells
Modes of transmission of HIV are not considered infectious unless visibly blood?
feces, nasal secretions, sputuum, sweat, vomitus, saliva, tears, and urine
HIV must be transmitted through _ cells, (Macrophages, Lymphocytes) from an infected person. Infected cells are present in bodily fluids including (3).
infected; genital, rectal, blood
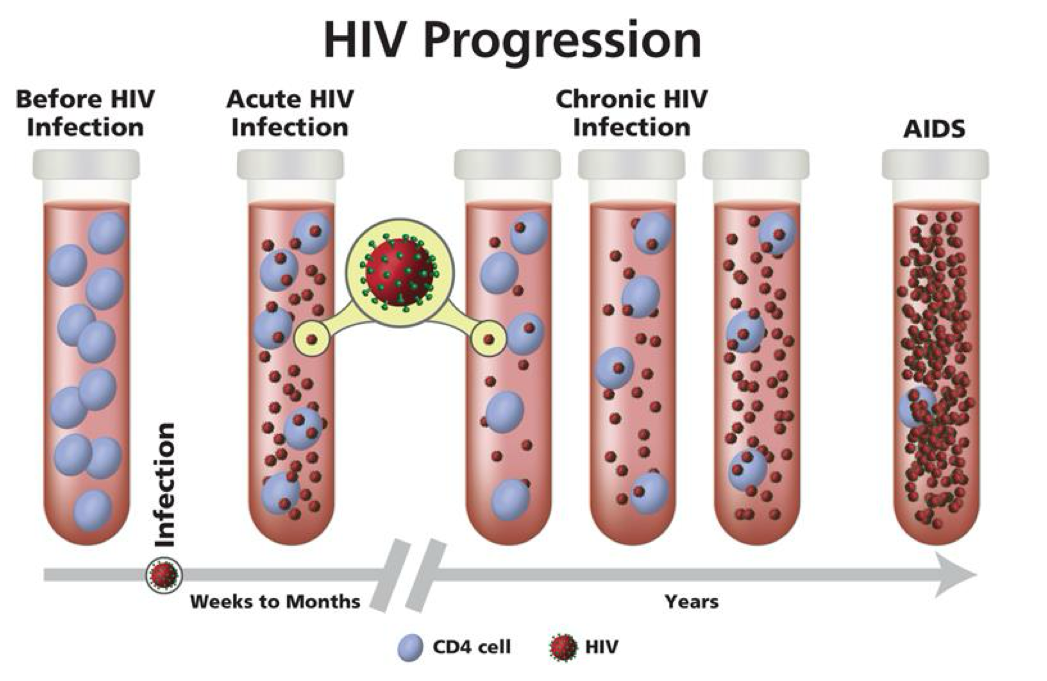
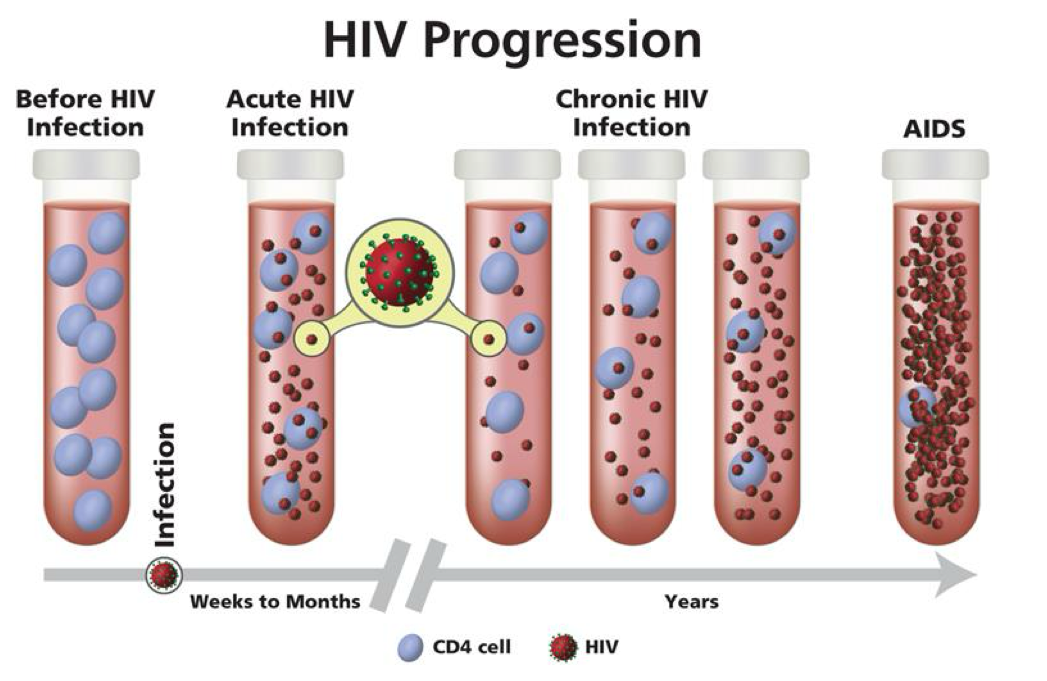
Stages of Infection: (1) Acute HIV Infection
2-4 weeks post infection
30% asymptomatic (1/3)
Symptoms, if any, are transient, mononucleus (fever, headache, rash)
Most infectious (high blood conc)
Strong immune response
Stages of Infection: (2) Chronic HIV Infection (Chronic lymphadenopathy, Sub-clinical immune dsyfunction, Skin and mucous membrane immune defects)
Strong immune response
HIV is detectable in blood, semen, and cervical secretions
Person enters clinical latency which is completely asymptomatic
Stage II lasts for >6yrs in 65-85% of cases
clinical latency = dormant
asymptomatic = still replicating but really slowly because of how few are left/ was only able infect a few CD4 cells
Stages of Infection: (3) Acquired Immunodeficiency Syndrome (AIDS) (Systemic immune deficiency)
W/O treatment will be be the result! (AIDS)
Diagnosis occurs when CD4 count is less than 200 cells/ uL
Most severe stage of infection: virus can no longer be controlled (CD4+, dendritic cells & CD8+ cells are all destroyed/ dysfunction)
DCs can’t present antigens
so other parts of the immune system r being compromised as well, thus causing the next 3 points.
CD4+ cells are impaired and cannot stimulate CD8+
CD4+ cells decline
Opportunistic infections, cancers, etc. set in
Average 3 year survival
Without treatment, later in the infection course, there's widespread inflammation, virus mutation, cellular impairment causing, “ _ _”.
immunological exhaustion
What does immunological exhaustion?
Means the immune system can’t keep up with what needs to be done.
Monocytes lose phagocytic activity, chemotaxis and cytokine secretion
DCs no longer function properly
B cells become dysfunctional
CD4+ are massively killed and cannot be replenished
CD8+ T cells start dying off because they do not get appropriate signals from CD4+ T helper cells resulting in less viral killing
Complete collapse of immune system
Without treatment at how many months does it take for HIV to platoe?
2 months
What is Viral load monitoring?
the number of bloodstream HIV particles, as after the initial peak, the virus reaches a “set point” during latency
viral load is a better marker for predict disease progression early, before CD4 are too low
<200 copies/mL: Disease will probably never occur
<1000 copies/mL: Disease in probably >10 years
>=100,000 copies/mL: <10 years
Most patients with >100,00 copies/mL, lose their CD4+ cells more rapidly and progress to AIDS before 10 years
Most patients have between 10,000 and 100,000 copies per mL are in the clinical latency phase
Combination antiretroviral therapy (cART)
Affluent countries have seen a >7-% decline in HIV/ADIS deaths
Reduces overall health care cost and restore quality of life
Reduces transmission
interferes with capacity for virus to be able to highjack the DNA of cells!
Standard treatment: combination of at least 3 drugs (:highly active antiviral therapy” or HAART) that suppress HIV replication
First-line ART consists of 3 drugs (reducing the likelihood of resistance)
teo nucleoside reverse transcriptase inhibits (NRTIs) plus a non-nucleoside reverse-transcriptase inhibitor (NNTRI)
want to cover all bases for whatever stage the virus is in!
BUT virus mutations arise due to the high error rates of reverse transcriptase and RNA polymerase II whose function is replicate the viral genome. Many of these mutations confer RESISTANCE to ARTs
What is the goal of someone taking cART?
to slow down after infection so it cannot turn into AIDS