ID exam 3
0.0(0)
Card Sorting
1/101
Last updated 5:03 AM on 1/27/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
102 Terms
1
New cards
What are the 5 major ways SSTI are precipitated?
Open wounds
Trauma
entrapment
compromiSed skin integrity
HematogEnous spread (RaRe)
Trauma
entrapment
compromiSed skin integrity
HematogEnous spread (RaRe)
2
New cards
In what type of situations do SSTI’s occur and what do they generally entale as to pathogens
SSTI’s generally occur in patients with complicated infections already and they may be polymicrobial depending on the patient case
3
New cards
What are the 3 consequences of SSTI’s that occur in complicated infections
Morbidity (can be loss of mobility or limbs, pain)
Physical or emotional stress
Increased healthcare costs
Physical or emotional stress
Increased healthcare costs
4
New cards
Define the characteristics of: (specify purulence and other key characteristics)
Erysipelas
Erysipelas
Non-purulent inflection of dermis
Results in a RED, Raised area that is WARM and tender
Preferably occurs in the lower extremities
Results in a RED, Raised area that is WARM and tender
Preferably occurs in the lower extremities
5
New cards
Define the characteristics of: (specify purulence and other key characteristics)
Cellulitis
Cellulitis
Non-purulent infection of dermis AND subcutaneous tissues
Diffuse RED, swollen area, warm and tender
Preferably in the lower extremities
Diffuse RED, swollen area, warm and tender
Preferably in the lower extremities
6
New cards
Define the characteristics of: (specify purulence and other key characteristics)
Impetigo
Impetigo
Most commonly occurs in children
Purulent! red sores that may burst and develop HONEY-COLORED CRUSTS
Can exist in bullous and nonbullous appearances.
most common during hot, humid weather on hands, face, and feet
Purulent! red sores that may burst and develop HONEY-COLORED CRUSTS
Can exist in bullous and nonbullous appearances.
most common during hot, humid weather on hands, face, and feet
7
New cards
Define the characteristics of: (specify purulence and other key characteristics and CAUSED BY) Furuncle
Purulent infection of a singular hair follicle
Focal area of redness, warmths, swelling, and tenderness
Caused by Staph aureus
Focal area of redness, warmths, swelling, and tenderness
Caused by Staph aureus
8
New cards
Define the characteristics of: (specify purulence and other key characteristics and caused by): Carbuncles
Purulent infection of multiple adjacent hair follicles
Focal area of redness, warmths, swelling, and tenderness
Primarily caused by staph aureus
Focal area of redness, warmths, swelling, and tenderness
Primarily caused by staph aureus
9
New cards
Define the characteristics of: (specify purulence and other key characteristics and caused by)
Abscesses
Abscesses
Purulent infection of dermal tissue
Focal area of redness, warmths, swelling, and tenderness
primarily caused by staph aureus
Focal area of redness, warmths, swelling, and tenderness
primarily caused by staph aureus
10
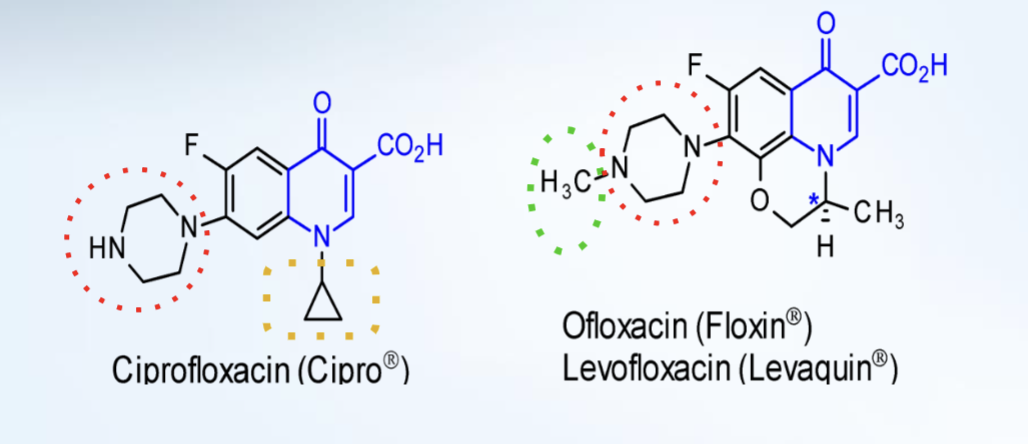
New cards
What are the 4 primarily signs of a necrotic infection?
Marked fever, chills, leukocytosis, and pain in affected area that may be disproportionate to initial presentation
11
New cards
What are the 3 signs of a necrotic infection?
Affected area initially resembles cellulitis without demarcated margins
Rapid, progressive infection with frequent development of a maroon/violet color
Affected area often shiny, exquisitely tender, and VERY painful
Rapid, progressive infection with frequent development of a maroon/violet color
Affected area often shiny, exquisitely tender, and VERY painful
12
New cards
Necrotizing fasciitis typically effects what?
What is a key characteristics of the necrotizing area?
How many types are there and what are their prevalences?
What is a key characteristics of the necrotizing area?
How many types are there and what are their prevalences?
NF is a rapidly-advancing necrotic infection that affects fascia
The affected fascia begins to have an almost wooden induration
There are 3 types
Type 1 occurs most often at \~80%
Type 2 occurs second most often at 15%
Type 3 (gas gangrene) is the most rare at only 5% occurrence
The affected fascia begins to have an almost wooden induration
There are 3 types
Type 1 occurs most often at \~80%
Type 2 occurs second most often at 15%
Type 3 (gas gangrene) is the most rare at only 5% occurrence
13
New cards
Type 3 of necrotizing fasciitis is gas gangrene which is also called?
How is it characterized?
How is it characterized?
clostridial myonecrosis
It is a rapidly advancing necrotic infection with PROMINENT GAS PRODUCTION that involves muscle. Typically occurs after surgery or trauma
It is a rapidly advancing necrotic infection with PROMINENT GAS PRODUCTION that involves muscle. Typically occurs after surgery or trauma
14
New cards
There are a lot of bacteria that can cause SSTI’s. What are the 2 most common gram + bacteria?
Staphylococcus aerus
Streptococcus pyogenes (group A streptococcus)
Streptococcus pyogenes (group A streptococcus)
15
New cards
What empiric coverage needs to be done for: Cellulitis
Strep pyogenes, MSSA
16
New cards
What empiric coverage needs to be done for: Erysipelas
Steprococcus pyogenes and MSSA
17
New cards
What empiric coverage needs to be done for: Impetigo
MSSA and MRSA
18
New cards
What empiric coverage needs to be done for: human/animal bites?
pyogenes, MSSA, anaerobes, and enteric gram negatives (widely varies based on bite)
19
New cards
What empiric coverage needs to be done for: Purulent infections
Pyogenes MSSA MRSA and others
20
New cards
What empiric coverage needs to be done for: Necrotizing fasciitis
look for broad empiric coverage that will cover everything especially pyogenes, enteric gram negatives, and anaerobes
21
New cards
In the case of human bite wounds, what is the primary bacteria involved and what else should be empirically covered?
What are the common human oral anaerobes that need covered?
What are the common human oral anaerobes that need covered?
streptococcus pyogenes and anaerobes primarily need to be covered.
\
Eikenella corrodens and peptostreptococcus are the most common oral human anaerobes
\
Eikenella corrodens and peptostreptococcus are the most common oral human anaerobes
22
New cards
What pathogens are primarily present in animal bites that differ from human bites? What is present in cats that aren’t present in humans/dogs?
Pasturella canis and pasturella cultocida are found in animal bites
\
Pasturella multocida is found in cats but not dogs/humans
\
Pasturella multocida is found in cats but not dogs/humans
23
New cards
What types of cultures should be done for animal/human bites?
Wound aspirations
secretions (exudate or pus)
Wound Swab
Surgical Cultures (like a debridement)
secretions (exudate or pus)
Wound Swab
Surgical Cultures (like a debridement)
24
New cards
In the case of necrotizing fasciitis, symptoms can GREATLY vary on a case to case basis. Classic symptoms like fevers and cutaneous manifestations may be not be present and imaging may not be helpful. What is characteristically almost always present?
Severe attributing pain to injury or procedure
Some systemic manifestations like NVD may occur as is present with any group A streptococcal infection
Some systemic manifestations like NVD may occur as is present with any group A streptococcal infection
25
New cards
When triaging patients with SSTI’s, what do we define as mild, moderate, and severe and when should they be hospitalized?
Mild: Local infection with NO systemic signs of illness
Moderate: Local infection with systemic signs of illness +/- hospital admission
Severe: Sepsis, failed incision & drainage attempt, deeper infection, or immunocompromised status
Moderate: Local infection with systemic signs of illness +/- hospital admission
Severe: Sepsis, failed incision & drainage attempt, deeper infection, or immunocompromised status
26
New cards
What nonpharm option can be done for furuncles?
A warm, moist compress
27
New cards
Treatment options for a nonpurulent (necrotizing infection/cellulitis/erysipelas)
MILD or MODERATE SSTI
MILD or MODERATE SSTI
Mild: oral Rx of penicillin VK or cephalosporin or dicloxacillin or clindamycin
\
Moderate: IV Rx of Penicillin or ceftriaxone or cefazolin or clindamycin
\
Moderate: IV Rx of Penicillin or ceftriaxone or cefazolin or clindamycin
28
New cards
Treatment options for a nonpurulent (necrotizing infection/cellulitis/erysipelas)
Severe (3 steps)
\
What if you find:
Pyogenes
clostridial sp
Vibrio vulnificus
Aeromonas hydrophila
Severe (3 steps)
\
What if you find:
Pyogenes
clostridial sp
Vibrio vulnificus
Aeromonas hydrophila
1. surgical exploration if needed
2. Empiric Rx of Vanco and Zosyn
3. culture/swab and narrow therapy
\
Pyogenes --- Penicillin + Clindamycin
clostridial sp --- Penicillin + Clindamycin
Vibrio vulnificus --- Doxy +ceftazidime
Aeromonas hydrophila --- Doxy + cipro
29
New cards
Treatment options for purulent (furuncle/carbuncle/abscess):
\
Mild
\
Mild
inspect and debridement
30
New cards
Treatment options for purulent (furuncle/carbuncle/abscess):
Moderate
3 steps
Moderate
3 steps
1. incision/debridement + Culture/swab
2. Empiric therapy of **bactrim or doxy**
3. Narrow therapy:
* MRSA: Bactrim
* MSSA: dicloxacillin OR Cephalexin
31
New cards
Treatment options for purulent (furuncle/carbuncle/abscess):
Severe
3 steps
Severe
3 steps
1. incision/debridement + Culture/swab
2. Empiric therapy of
1. vanco
2. or linezolid
3. or televancin
4. or ceftaroline
5. or televancin
3. Narrow therapy:
* MRSA: vanco/linezolid/etc.
* MSSA:
* nafcillin, cefazolin, clindamycin
32
New cards
For any form of group A streptococcal necrotizing fasciitis how long must empiric therapy run for?
48-72 hours
33
New cards
What drug that we use is a potent suppressor of toxins produced by staphylococcal and streptococcal pathogens in addition to cytokines produced in infections
Clindamycin
34
New cards
Though there is low quality of evidence may linezolid do to endotoxins?
inhibit toxin production
35
New cards
What is the minimum treatment durations for SSTI’s and what is the acception?
5 days with the acception of necrotizing infections which must be 4-6 weeks
36
New cards
What are neurological sequelae?
neurological deficits that result from neurological damage
37
New cards
What are the 4 steps as to how meningitis occurs within a patient?
Mucosal colonization and bacterial invasion
Bacterial replication in the subarachnoid space
Progressive inflammation
Increased intracranial pressure and cerebral edema
Bacterial replication in the subarachnoid space
Progressive inflammation
Increased intracranial pressure and cerebral edema
38
New cards
What are NORMAL lab findings for the following?
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
* WBCs ---
39
New cards
What are lab findings for Bacterial meningitis?
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
\
* WBCs --- 1000-5000
* Differential --- neutrophils
* protein --- elevated
* glucose --- low
* CSF/blood glucose ratio --- decreased
* WBCs --- 1000-5000
* Differential --- neutrophils
* protein --- elevated
* glucose --- low
* CSF/blood glucose ratio --- decreased
40
New cards
What are lab findings for viral meningitis?
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
\
* WBCs --- 50-1000
* Differential: lymphocytes
* protein: mild elevation
* glucose: NORMAL
* CSF/blood glucose ratio: Normal
* WBCs --- 50-1000
* Differential: lymphocytes
* protein: mild elevation
* glucose: NORMAL
* CSF/blood glucose ratio: Normal
41
New cards
What are the lab findings for fungal meningitis?
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
* WBCs
* Differential
* protein
* glucose
* CSF/blood glucose ratio
\
* WBCs: 20-500
* Differential: lymphocytes
* protein: elevated
* glucose: low
* CSF/blood glucose ratio: low
* WBCs: 20-500
* Differential: lymphocytes
* protein: elevated
* glucose: low
* CSF/blood glucose ratio: low
42
New cards
What’s the leading cause of Meningitis? How should it never be treated? What is it predisposed to cause if not taken care of quickly?
Leading cause is streptococcus pneumoniae
NEVER use vanco as monotherapy
High rates of neurologic sequelae
NEVER use vanco as monotherapy
High rates of neurologic sequelae
43
New cards
Neisseria meningitidis is generally associated with crowding and is spread through droplets. What are the characteristics of the immune reactions related with this bug?
Fever, arthritis, and pericarditis
44
New cards
Haemophilus influenzae can cause meningitis but rates have decreased recently due to immunization rates. What characteristic symptoms occur?
Ear infection, sinus infections, CSF leaks are risk factors
45
New cards
What is the leading cause of Meningitis in patients > 2 months old?
Streptococcus pneumoniae
46
New cards
When is comes to Listeria monocytogenes:
What populations are we concerned about?
Where can it come from?
Why do we care?
Whats the best way to treat it?
What populations are we concerned about?
Where can it come from?
Why do we care?
Whats the best way to treat it?
Elderly, neonates, immune compromised, alcoholic
Obtained from the GI tract
High fatality rates makes it concerning
Ampicillin +/- Gentamicin
Obtained from the GI tract
High fatality rates makes it concerning
Ampicillin +/- Gentamicin
47
New cards
What is the leading cause of neonatal meningitis?
Streptococcus agalactiae
48
New cards
When approaching treatment, what are the best 5 steps to do in order?
Identify
Lumbar puncture or CT
Empiric antibiotics
adjust per gram stain
adjust per C&S
Lumbar puncture or CT
Empiric antibiotics
adjust per gram stain
adjust per C&S
49
New cards
When should you initial antibiotic coverage begin for patients presenting with meningitis like symptoms?
start them as soon as possible after the diagnosis is considered likely. Even if lumbar puncture has not occurred yet
50
New cards
Empiric therapy for the following age ranges with meningitis:
< 1 mo
1-23 mo
2-50 yo
>50 yo
< 1 mo
1-23 mo
2-50 yo
>50 yo
< 1 mo :: Ampicillin + cefotaxime OR amp + aminoglycoside
1-23 mo :: Vanco + third gen cephalosporin
2-50 yo :: Vanco + third gen ceph
>50 yo :: Amp, vanco, third gen ceph
51
New cards
What are the pros of using dexamethasone and when MUST it be given
decreases inflammation, decreases neurologic sequelae in adults with S. pneumoniae meningitis, and decreases neurologic sequelae in children with H. influenzae meningitis
\
IT MUST be given with or before the first dose of antibiotics
\
IT MUST be given with or before the first dose of antibiotics
52
New cards
When considering a medication to be used in a patient with meningitis, what types of medications will most likely not be most effective?
Drugs like Augmentin and Bactrim that have an extra inhibitor will most likely not reach therapeutic levels within the CSF making them weak
53
New cards
What 6 drugs can you NOT use in CSF with or without inflammation?
Aminoglycosides
Amphotericin B
Beta-lactamase inhibitors
Cephalosporins (1st and 2nd gen)
Doxycycline
Itraconazole
Amphotericin B
Beta-lactamase inhibitors
Cephalosporins (1st and 2nd gen)
Doxycycline
Itraconazole
54
New cards
Ideal antibiotic properties for treating meningitis
LMW
non-ionized
Lipid soluble
low protein binding
high blood concentration
non-ionized
Lipid soluble
low protein binding
high blood concentration
55
New cards
What two bugs that can cause meningitis should be reported to the local health department?
Neisseria meningitidis
H. Influenzae
H. Influenzae
56
New cards
What is essential for viral encephalitis treatment?
Supportive care is essential
57
New cards
For HSV what type effects adults and which effects newborns?
\
What should be started immediately in coordination with hydration therapy?
\
What should be started immediately in coordination with hydration therapy?
Type 1 HSV primarily effects adults
Type 2 HSV primarily effects newborns
\
Acyclovir should be started quickly in both adults and newborns with suspected encephalitis even with pending diagnostic tests
Type 2 HSV primarily effects newborns
\
Acyclovir should be started quickly in both adults and newborns with suspected encephalitis even with pending diagnostic tests
58
New cards
When doing empiric coverage for patients with brain abscesses what should be covered and for how long?
Broad spectrum +/-/anaerobes
\
Vanco can be added for MRSA
Voriconazole and bactrim can be added in immunocompromised patients
\
6-8 weeks
\
Vanco can be added for MRSA
Voriconazole and bactrim can be added in immunocompromised patients
\
6-8 weeks
59
New cards
Any form of administration that is not within normal IV administrations must be:
Preservative free
60
New cards
Durations of therapy for the following meningitis causing bugs:
* Neisseria meningitidis
* haemophilus influenzae
* Strep pneumoniae
* strep agalactiae
* Aerobic gram negative stuff
* Listeria monocytogenes
* Neisseria meningitidis
* haemophilus influenzae
* Strep pneumoniae
* strep agalactiae
* Aerobic gram negative stuff
* Listeria monocytogenes
* Neisseria meningitidis - 7 days
* haemophilus influenzae - 7 days
* Strep pneumoniae - 10-14
* strep agalactiae - 14-21 days
* Aerobic gram negative stuff - 21 days
* Listeria monocytogenes - 21+ days
* haemophilus influenzae - 7 days
* Strep pneumoniae - 10-14
* strep agalactiae - 14-21 days
* Aerobic gram negative stuff - 21 days
* Listeria monocytogenes - 21+ days
61
New cards
Cryptococcus neoformans is the most common form of fungal CNS infection in the US. How is it gotten
What is it frequently treated with?
What is it frequently treated with?
inhalation of spore that generally takes over immunosuppressed patients
\
Amphotericin B + flucytosine
\
Amphotericin B + flucytosine
62
New cards
Amphotericin B
How does it work
Common side effects
How does it work
Common side effects
Binds to ergosterol altering cell membrane permeabilities and cell death
\
Nephrotoxicity, infusion-related reactions, and others
\
Nephrotoxicity, infusion-related reactions, and others
63
New cards
Women are predisposed to be more likely get a UTI over men. What are some causative factors for women? What are some causative factors for men?
Risk factors for everyone?
Risk factors for everyone?
Women: Sex, cervical diaphragms, spermicidal jellies, pregnancy
\
Men: Prostate hyperplasia, uncircumcised
\
All patients: Diabetes, physical abnormalities, catheters, or obstructions
\
Men: Prostate hyperplasia, uncircumcised
\
All patients: Diabetes, physical abnormalities, catheters, or obstructions
64
New cards
Signs of a lower UTI
\
Signs of an upper UTI
\
Signs of an upper UTI
Lower: Frequency, dysuria/nocturia, hematuria, suprapubic heaviness
\
Upper: Fever, chills, flank pain, N/V, malaise, fatigue, pelvic pain, + any lower symptoms
\
Upper: Fever, chills, flank pain, N/V, malaise, fatigue, pelvic pain, + any lower symptoms
65
New cards
What is a complicated UTI?
Any UTI known to be caused by structural or functional abnormalities. OR any UTI occurring in male patients
66
New cards
What are the most common bugs to cause UTIs
E. coli (always most common)
enterococcus spp.
k. pneumonia
Proteus spp.
enterococcus spp.
k. pneumonia
Proteus spp.
67
New cards
What 5 things should you watch for in UTIs
Presence of bacteria… AT ALL
Pyuria (WBCs)… should always be less than 5. Pyuria is considered when WBCs are >10 in the urine
\
nitrites
\
RBCs (should normally be
Pyuria (WBCs)… should always be less than 5. Pyuria is considered when WBCs are >10 in the urine
\
nitrites
\
RBCs (should normally be
68
New cards
What is the difference between sensitivity and specificity?
Sensitivity: proportion of tests that read positive that are actually positive patients
\
Specificity: proportion of tests that are read negative that are actually negative patients
\
Specificity: proportion of tests that are read negative that are actually negative patients
69
New cards
What are the 3 main drugs we used to treat uncomplicated UTI’s, Dose, duration, and pearls
Nitrofurantoin 100 mg BID for 5 days -- only for patients with a lower UTI
\
Bactrim 800/160 mg BID for 3 days -- sulfa allergies
\
Fosfomycin 3 grams for 1 dose -- covers GNRs, ESBL, VRE
\
Bactrim 800/160 mg BID for 3 days -- sulfa allergies
\
Fosfomycin 3 grams for 1 dose -- covers GNRs, ESBL, VRE
70
New cards
Treating complicated UTI’s, Durations, and pearls
Levofloxacin, ciprofloxacin, ceftriaxone - 7-10 days
\
3rd or 4th generation cephalosporins - 7-14 days - ORAL option: cefdinir
\
3rd or 4th generation cephalosporins - 7-14 days - ORAL option: cefdinir
71
New cards
Treatment for Catheter associated UTI’s
* old catheter of 2+ weeks
* if symptoms resolve when can treatment stop at the earliest? but they may last up to?
* What if we’re using fluoroquinolones?
* old catheter of 2+ weeks
* if symptoms resolve when can treatment stop at the earliest? but they may last up to?
* What if we’re using fluoroquinolones?
Old catheters should be removed or replaced.
\
7 day treatments may be enough if symptoms resolve but can go as long as 14 days
\
Fluoroquinolone regimens can go only 3-5 days
\
7 day treatments may be enough if symptoms resolve but can go as long as 14 days
\
Fluoroquinolone regimens can go only 3-5 days
72
New cards
What are the differences between the following terms:
* Neuropathy
* Impaired microvascular circulation
* Immunological defects
* Neuropathy
* Impaired microvascular circulation
* Immunological defects
* Neuropathy - decreased feeling in a limb that can cause improper wound care
* Impaired microvascular circulation - causing impaired healing and antibiotic distribution to infected areas
* Immunological defects
* Impaired microvascular circulation - causing impaired healing and antibiotic distribution to infected areas
* Immunological defects
73
New cards
What most commonly cause diabetic foot infections?
Gram-positive staphylococcus
74
New cards
When considering diabetic foot infections what diagnostic tests should be done?
Do cultures from deep tissues after wound is cleanset/debrided and BEFORE antibiotics
\
X-ray should also be done to rule out osteomyelitis
\
X-ray should also be done to rule out osteomyelitis
75
New cards
In treating Diabetic foot infections, what is the go to and what needs to be closely monitored?
IV antibiotics are the GO TO treatment course and glycemic control is incredibly important
76
New cards
What drugs traditionally cover MRSA and which are considered Oral?
Doxy, bactrim, clindamycin, linezolid, Vanco, dapto, ceftaroline
\
Orals: Doxy, bactrim, clindamycin, linezolid
\
Orals: Doxy, bactrim, clindamycin, linezolid
77
New cards
What drugs traditionally cover pseudomonas?
Zosyn, cefepime, carbapenems, cipro, levo
78
New cards
What drugs traditionally cover anaerobes?
Zosyn, augmentin, Unasyn, carbapenems, metronidazole
79
New cards
Mild-moderate diabetic infection without recent antibiotic use?
B-lactam allergy?
MRSA suspected?
B-lactam allergy?
MRSA suspected?
1. cephalexin or dicloxacillin
2. Clindamycin or a fluoroquinolone
3. Doxycycline or Bactrim
\
80
New cards
What type of symptoms suggest the presence of anaerobes?
foul odor, necrosis, gas, or significant ischemia
81
New cards
Severe diabetic foot infection… the CLASSIC FUCKIN GO TO DUO:
\-minor penicillin allergy:
\-severe penicillin allergy or ESBL infections
\-minor penicillin allergy:
\-severe penicillin allergy or ESBL infections
Vanco and Zosyn
Vanco, cefepime, and metronidazole
\
vanco + meropenem
Vanco, cefepime, and metronidazole
\
vanco + meropenem
82
New cards
How long should you treat a diabetic foot infection that is:
Mild-moderate?
Extensive, slow healing infections?
Osteomyelitis?
Mild-moderate?
Extensive, slow healing infections?
Osteomyelitis?
1-2 weeks
3-4 weeks
4-6 weeks
3-4 weeks
4-6 weeks
83
New cards
How do we define acute and chronic osteomyelitis?
Acute: days-weeks
Chronic: Months-years
Chronic: Months-years
84
New cards
What are the two ways that osteomyelitis begins
bacteremia spread from the blood into the bone
\
spreads from nearby soft tissue/joints or from bone exposure to environment
\
spreads from nearby soft tissue/joints or from bone exposure to environment
85
New cards
What is the primary pathogen that can cause osteomyelitis?
Staphylococcus
86
New cards
Clinical presentation of osteomyelitis:
Acute:
Chronic
Acute:
Chronic
pain, redness, and edema
\
acute: fever, systemic signs of infection
\
Chronic: bone necrosis, non-healing ulcers or fractures, and sinus tracts from skin to bone
\
acute: fever, systemic signs of infection
\
Chronic: bone necrosis, non-healing ulcers or fractures, and sinus tracts from skin to bone
87
New cards
What is the preferred method of imaging a bone that is suspected to have osteomyelitis
MRI is preferred due to high sensitivity
88
New cards
When using antibiotics to treat osteomyelitis what should absolutely be targetted?
MRSA and GNRs
Examples: Vanco + ceftriaxone
Doxy+Cefdinir
Examples: Vanco + ceftriaxone
Doxy+Cefdinir
89
New cards
What drugs are generally good at penetrating the bone?
Clindamycin, tetracyclines, fluoroquinolones, linezolid, trimethoprim
90
New cards
Generally how long do we treat osteomyelitis?
4-6 weeks
91
New cards
How do fluoroquinolones work?
bactericidal and inhibit DNA gyrase and topoisomerase 4
92
New cards
What is the benefit of a 6-F group on the CARBOXY-4-PYRIDONE structure?
increases lipophilicity and improves penetration of the bacterial cell wall
93
New cards
What is the relationship of Levofloxacin and Ofloxacin?
They are enantiomers of each other.
94
New cards
How is Ofloxacin prepared compared to its enantiomer levofloxacin?
Ofloxacin is sold as a racemic mixture
Levo is the 1S enantiomer only.
Levo is the 1S enantiomer only.
95
New cards
Which is stronger Levo or ofloxacin?
Levo is twice as active and 128 times more active than the R-enantiomer
96
New cards
Describe the fluoroquinolone SAR
A piperazine ring is present at C-7 that increases binding to CNS GABA receptors causing side effects
\
An alkyl group on the piperazine ring decreases GABA binding.
\
A cyclopropyl group on N-1 broadens the activity of the quinolone to include atypical bacteria
\
Addition of a methoxy group on C-8 decreases the photosensitivity
\
An alkyl group on the piperazine ring decreases GABA binding.
\
A cyclopropyl group on N-1 broadens the activity of the quinolone to include atypical bacteria
\
Addition of a methoxy group on C-8 decreases the photosensitivity
97
New cards
What is mandatory for fluoroquinolone activity to occur?
The carboxy-4-pyridone pharmacophore is essential for activity
98
New cards
What does a fluoro group at C-6 of a fluoroquinolone do to activity?
\
What if we add another at c-8?
\
What if we add another at c-8?
It increases activity by increasing the lipophilicity of the molecule. the C-6 F group also increases DNA gyrase/topo 4 inhibition
\
It improves drug absorption and half-life but ALSO increases drug-induced photosensitivity
\
It improves drug absorption and half-life but ALSO increases drug-induced photosensitivity
99
New cards
Why should Fluoroquinolones NEVER be taken with any form of polyvalent metal ions
They can chelate with the C3-carboxylic acid and 4-keto group drastically decreasing their absorption and solubility
100
New cards
Tetracyclines must has a C6 hydroxyl group or else what?
They will not undergo dehydration and be destroyed