Lower GI Structural Pathologies
1/70
Earn XP
Description and Tags
These flashcards cover key concepts and details regarding lower GI structural pathologies, including diverticular disease, volvulus, intussusception, and imperforate anus.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
71 Terms
What are structural pathologies of the lower GI tract?
Conditions that affect the anatomy of the colon, disrupting normal bowel function due to physical or structural abnormalities.
Which pathologies are included in the structural submodule?
Diverticular disease, volvulus, intussusception, and imperforate anus.
Why are many structural GI pathologies considered emergencies?
Because they can cause bowel obstruction, compromised blood supply, necrosis, perforation, and peritonitis.
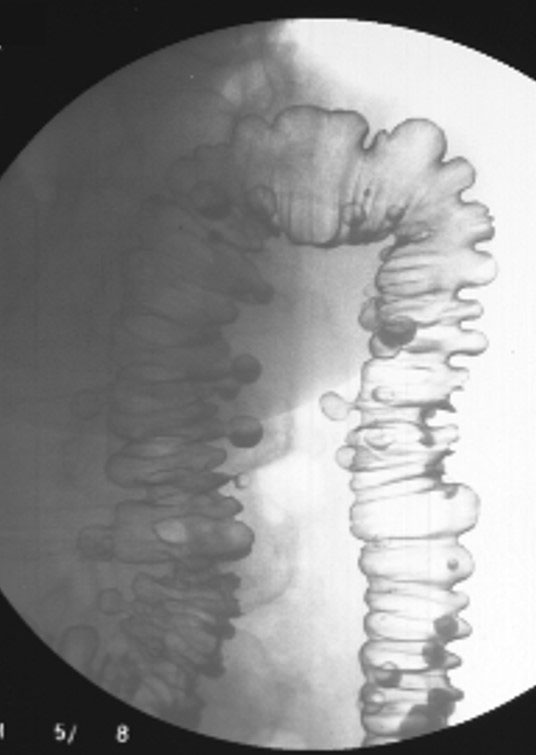
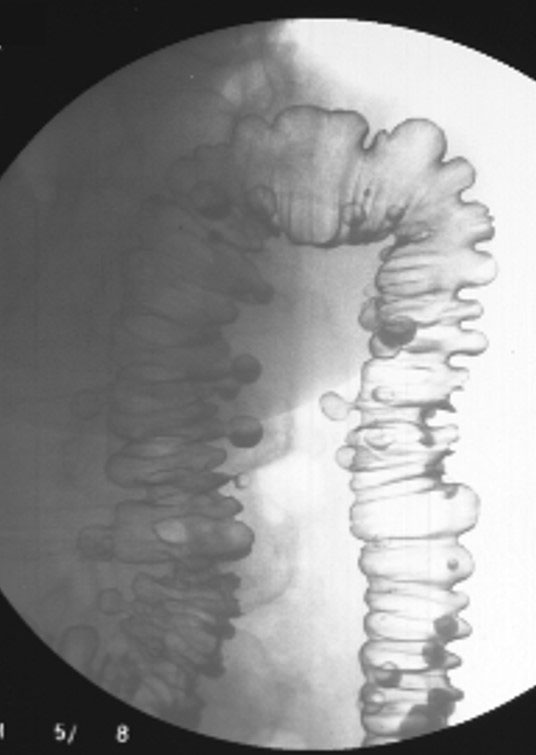
What are diverticula?
Outpouchings (herniations) of the mucosal layer through a weakened muscular layer of the bowel wall.
What is diverticulosis?
The presence of diverticula without inflammation.
What is diverticulitis?
The inflamed or infected form of diverticulosis, usually due to trapped fecal material.
How is diverticular disease classified?
As an inflammatory and degenerative pathology.

What causes diverticula to form?
Herniation of the mucosal layer through weak areas in the muscular wall of the colon.
What dietary pattern increases the risk of diverticulosis?
Low-fiber, low-bulk diets.

Why is diverticulosis common in Western countries?
Due to highly processed, low-fiber diets.

At what age is diverticulosis uncommon?
Under 30 years of age.

What percentage of people over 60 have diverticula?
More than 50%.
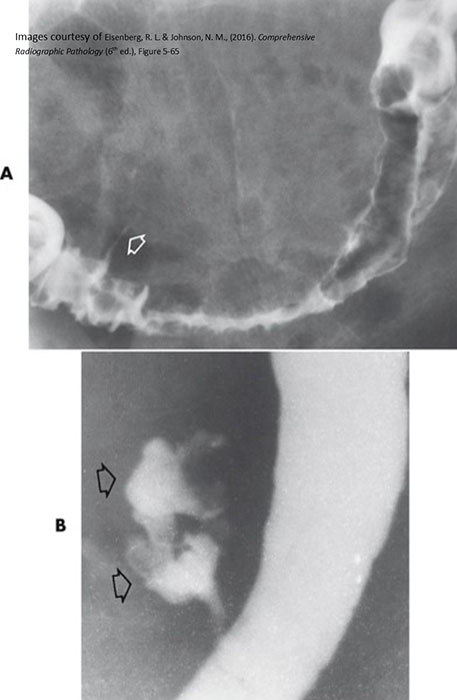
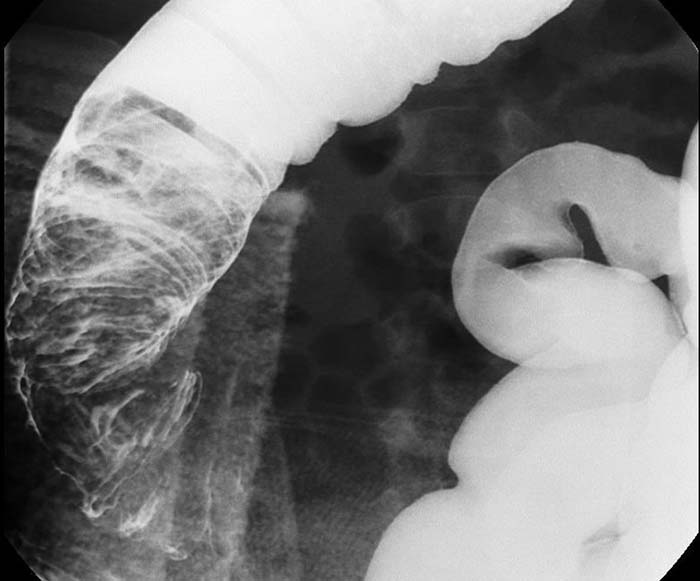
Where do diverticula most commonly occur?
The sigmoid colon.

Why is the sigmoid colon the most common site for diverticula?
It is narrow and experiences high pressure during stool movement toward the rectum.
What contributes to the formation of diverticula?
Straining during defecation and increased intraluminal pressure.

Where do diverticula usually form along the bowel wall?
At sites where mesenteric vessels penetrate the bowel wall, near the tenia coli.
Do diverticula usually occur singly or in groups?
In groups, not singly.

What complications can occur if fecal material becomes trapped in diverticula?
Diverticulitis, perforation, abscess, fistula formation, or bowel obstruction.
Is diverticulosis usually symptomatic?
No, it is usually asymptomatic.
What symptoms may occur with diverticulosis?
Intermittent lower abdominal pain, alternating diarrhea and constipation, and occasional bleeding.
What additional symptoms indicate diverticulitis?
Fever, localized tenderness, and increased white blood cell count.
How is diverticulosis managed?
High-fiber diet, increased exercise, and avoidance of seeds, nuts, and popcorn.
Why should seeds and nuts be avoided in diverticulosis management?
They can become trapped in diverticula and cause inflammation or infection.
How is diverticulitis treated?
Antibiotics and a fluid diet to reduce bowel strain.
When is surgery required for diverticular disease?
When perforation occurs.
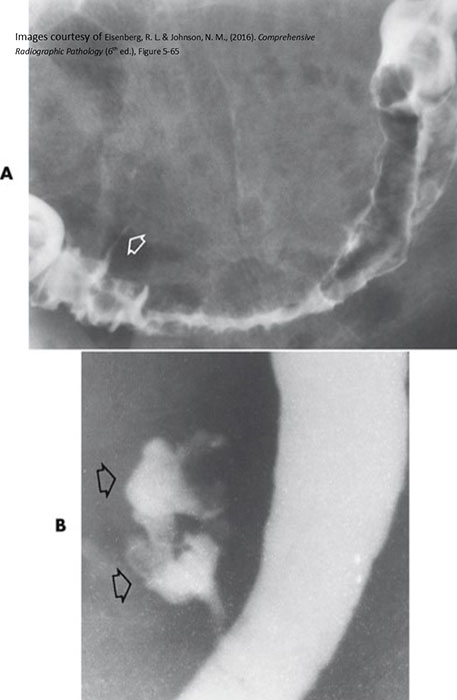
What is volvulus? (twist)
A twisting of a portion of the bowel that may cause obstruction and compromise blood supply.
How can you remember what volvulus means?
Volvulus → revolve → twist.
How is volvulus classified?
As congenital and degenerative.
What causes volvulus?
An abnormally long mesentery or redundant bowel loops that allow twisting.

What is the role of the mesentery?
It anchors the bowel and carries nerves, blood vessels, and lymphatics.
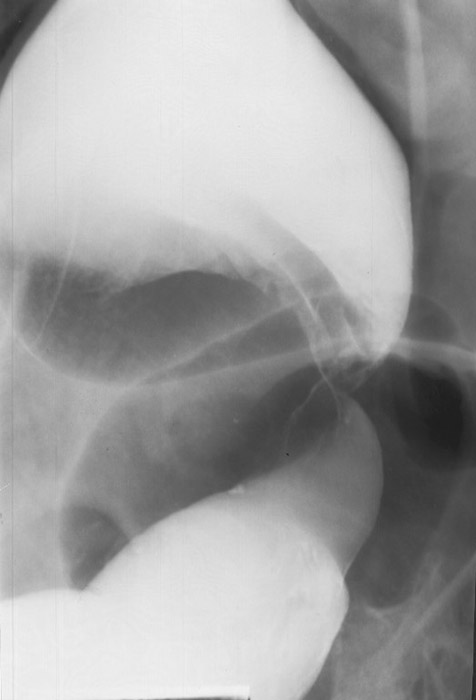
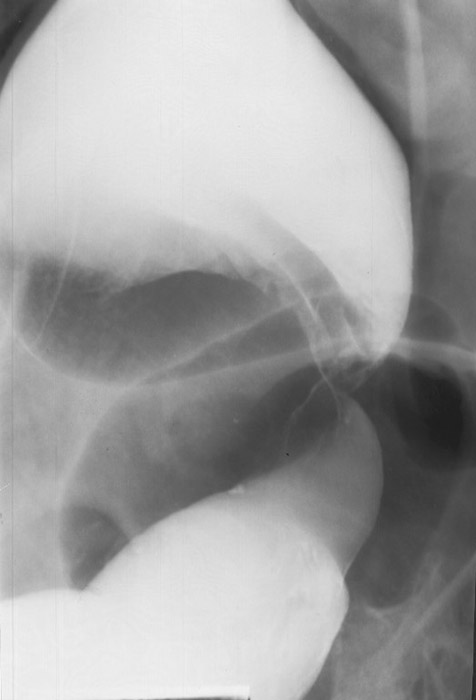
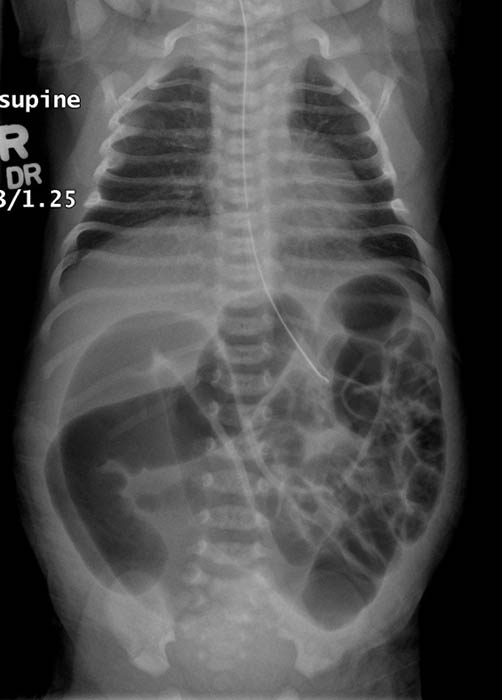
Where does volvulus most commonly occur?
In the cecum and sigmoid colon. (image shows cecal volvulvus)


Which age group commonly experiences cecal volvulus?
Younger individuals.

Which age group commonly experiences sigmoid volvulus?
Elderly individuals.
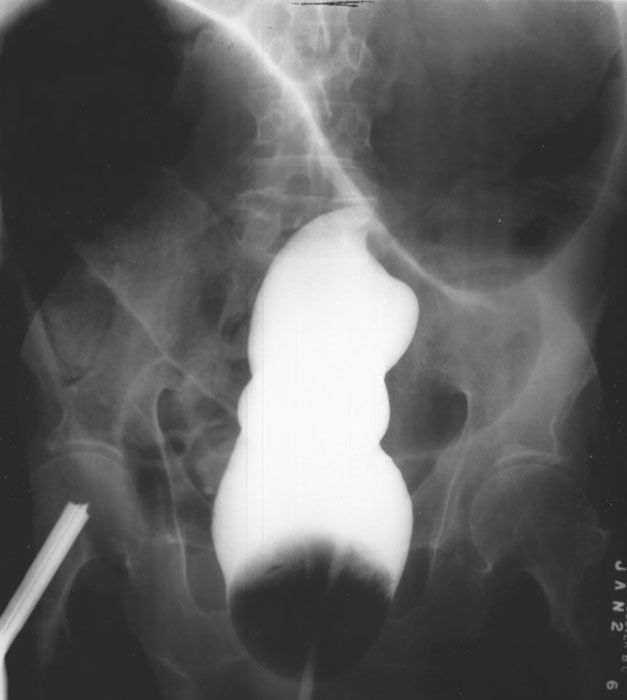
How does cecal volvulus occur?
The cecum twists on its long axis and often displaces upward and to the left.
How does sigmoid volvulus occur?
The sigmoid twists on its mesenteric axis, rotating left or right.

What are the two major dangers of volvulus?
Bowel obstruction and compromised blood supply.
What can compromised blood supply lead to in volvulus?
Necrosis and gangrene.
Why can volvulus cause peritonitis?
Obstruction can cause severe distension leading to bowel perforation.

What are common symptoms of volvulus?
Severe abdominal pain, vomiting, and abdominal distension.
How is volvulus treated?
Emergency surgery to untwist the bowel.
When is bowel resection required in volvulus?
If the bowel has become necrotic.
What surgical options may be required for volvulus?
Partial colectomy, ileum reattachment, or total colectomy with ostomy.
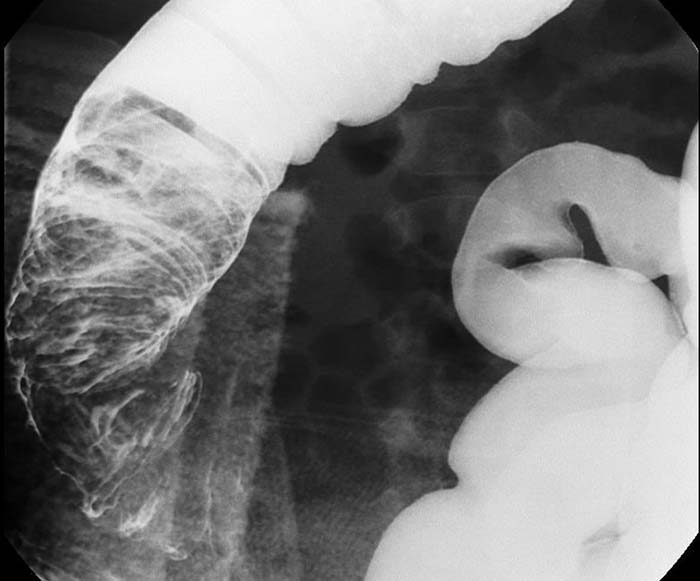
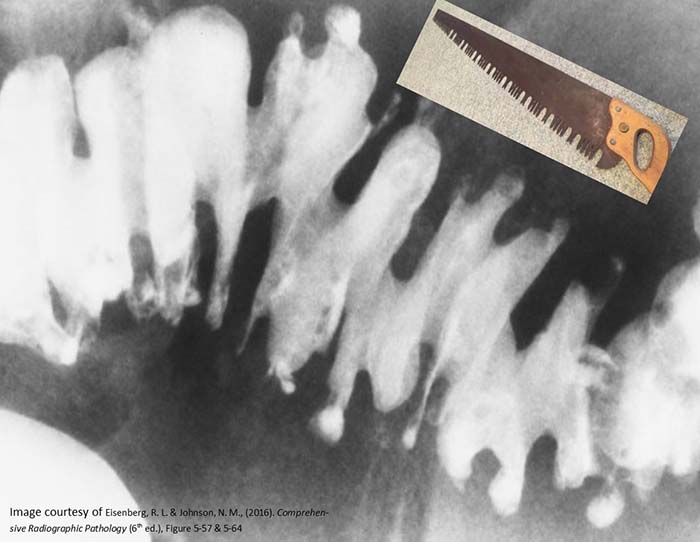
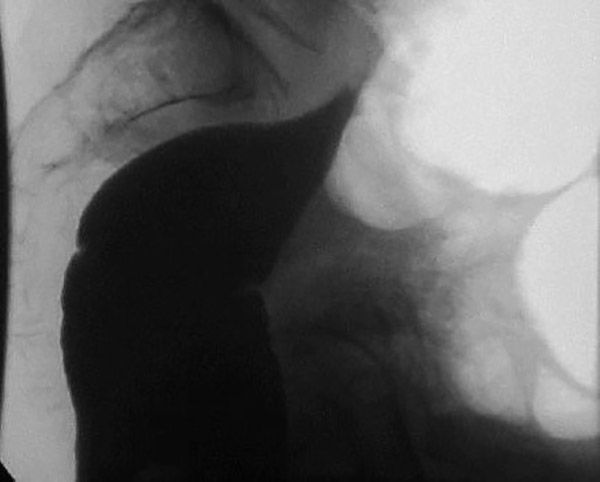
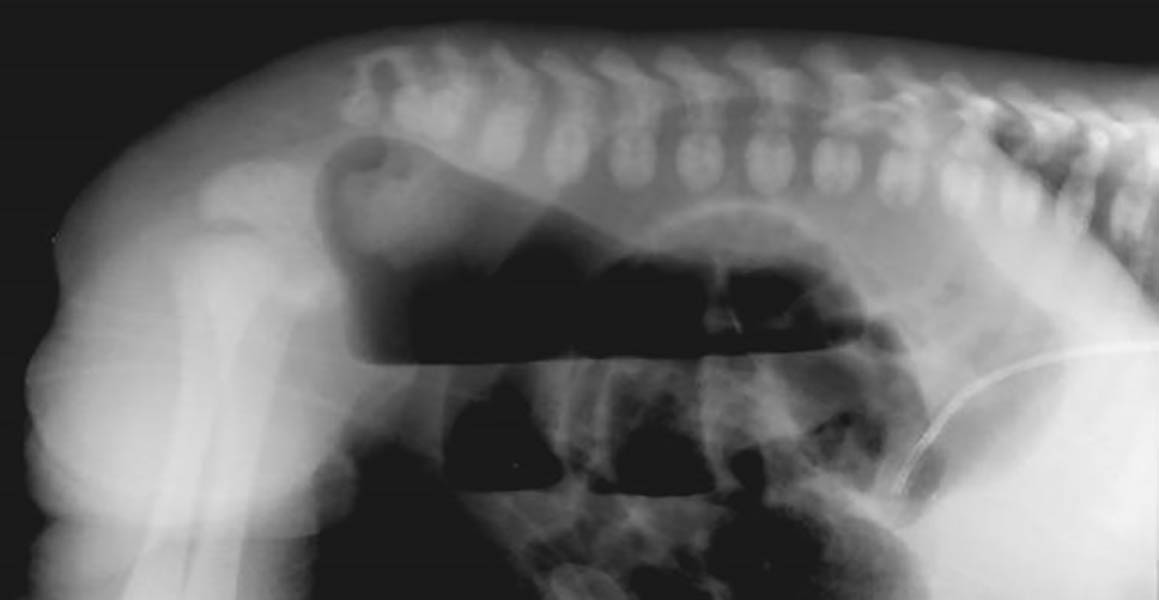
What is intussusception?
Telescoping of a proximal bowel segment into a distal segment, causing obstruction.

Why is intussusception dangerous?
It compresses the mesentery, cutting off blood supply and causing necrosis.

How is intussusception classified?
Idiopathic and degenerative.

In which age group does intussusception most commonly occur?
Infants and young children (>90% of cases).
What causes intussusception?
Peristalsis forcing bowel into itself.
Why does obstruction occur in intussusception?
Bowel contents cannot pass through the telescoped segment.

Where does intussusception most commonly occur in children?
At the ileocecal valve.
Why does intussusception occur in children?
Often due to loose mesentery allowing excessive bowel movement.

What usually causes intussusception in adults?
An underlying pathology such as a polyp, inflammatory mass, or carcinoma.
Can intussusception occur anywhere in adults?
Yes, in both the small and large bowel.

What is transient intussusception?
A temporary form that resolves spontaneously, often seen on CT in celiac disease.
What are classic symptoms of intussusception in children?
Sudden severe abdominal pain, distension, vomiting, and a palpable right-sided mass.
What is 'red currant jelly' stool?
Stool mixed with blood and mucus, classic for pediatric intussusception.
What symptoms occur in adults with intussusception?
Recurrent abdominal pain, nausea, and vomiting.
Why is prompt treatment critical in intussusception?
Mortality is <1% if treated within 24 hours but rises sharply after 48 hours.
How is intussusception treated in children?
Air or water-soluble contrast enema.
How is intussusception treated in adults?
Enema plus investigation and correction of the underlying cause.
When is surgery required for intussusception?
If enema treatment is unsuccessful.

What is imperforate anus?
A congenital failure of the membrane between the rectum and anus to rupture.

What other names are used for imperforate anus?
Anal agenesis and rectal atresia.
How is imperforate anus classified?
Congenital.

What causes imperforate anus?
Idiopathic failure of rectum and anus development or membrane rupture.
Who does imperforate anus affect?
Newborn infants.
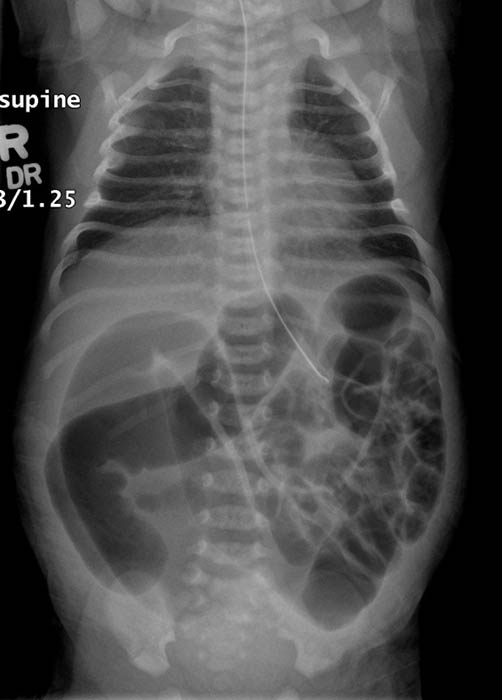
Why does bowel obstruction occur in imperforate anus?
The rectum does not communicate with the anus.

How is imperforate anus categorized anatomically?
As high or low, depending on distance from the anus.
What associated abnormalities are common with imperforate anus?
Genitourinary fistulas.

What is the earliest sign of imperforate anus?
Failure to pass meconium. (babies first stool)
What additional signs may be present with imperforate anus?
Abdominal distension and stool in urine or vagina.
How is imperforate anus treated?
Surgical correction and fistula repair.