CNS- Serotonergic neurotransmission
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
53 Terms
what are mood disorders?
Major depression has a lifetime prevalence of about 5% to 17%.
Sex differences→ women have almost twice the prevalence rate vs. men
Increasing the prevalence in childhood
High comorbidity with other conditions
DSM-V classification
what are the two main types of mood disorders?
Depressive Disorders - MDD, PMDD, PDD, DMDD
Bipolar Disorders - Bipolar I, Bipolar II and cyclothymic
what are the types of depressive disorders?
Major depression — at least two weeks and often longer than four weeks
Seasonal affective disorder — associated with change of season
Persistent depressive disorder — a long-term form of depression
Disruptive mood dysregulation disorder — children and teenagers
Premenstrual dysphoric disorder — 10 days before a menstrual period
what are the types of bipolar disorders?
Bipolar I disorder — more mania episodes and more severe symptoms
Bipolar II disorder — hypomania, which is a less severe form of mania, doesn’t affect your ability to function
Cyclothymia — chronically unstable mood state. Hypomania and mild depression for at least two years
what are the theories of depression?
Monoamine theory
Negative affective bias
Neuroendocrine mechanism
what is the monomaine theory?
Depression is caused by a functional deficit of the monoamine transmitters, noradrenaline and 5-hydroxytryptamine (5-HT)
Mania is caused by a functional excess of the same neurotransmitters
what are the problems with the monoamine theory?
There is no clear evidence depressed patients have deficient serotonergic or monoaminergic signalling
Antidepressants increase neurotransmission hours therapeutic benefit take weeks
Some antidepressants not monoaminergic pathways
what is the negative affective bias theory?
Perception of the event in a negative manner
Focus on the negative information
Recall negative information
One single dose of antidepressant revert the effect – the drugs need time to become aware of the improvements in their mood
what is the neuroendocrine mechanism?
Corticotrophin-releasing hormone
– Animal models: ↑ CRF mimic some aspect of depression and stress
– Hypothalamic neurons→ Na and 5-HT inputs
Hypothalamic cells release CRT → pituitary cells secrete ACTH → ↑ cortisol
↓ growth hormone
↑ prolactin
what are the trophic effects?
Relation between lower levels of BDNF and depression
– Treatment with antidepressant increase BDNF levels
• GSK3β implications due to lithium target
• Higher levels of glutamate
– Depressed patients ↑ level of Glu in cortical areas
– Antidepressant depress NMDA receptor function
what is neuroplasticity?
Neuronal loss in the hippocampus and prefrontal cortex
Animal models→ antidepressant drugs or electroconvulsions→ promote neurogenesis→5-HT1A and α 2 adrenoceptors
how are antidepressant drugs tested on animal models?
Mild stress (e.g. the forced swim test, inescapable foot shock)
– Behavioural states (withdrawal from social interaction, loss of appetite, reduced motor activity, etc.)
– Genetically modified mice (e.g. knock-down of 5-HT, noradrenaline and glutamate transporters, mutations or knock-down of 5-HT receptors, etc.)
how are antidepressant drugs tested on humans?
Hamilton Rating Scale for Depression (HAM-D) and the Montgomery-Asberg Depression Rating Scale (MADRS)
Young Mania Rating Scale (YMRS)
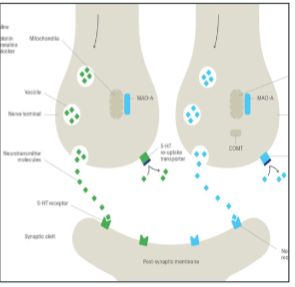
what is central serotonergic neurotransmission?
5-HT-containing cells within the raphe nuclei
– projections to the spinal cord modulate pain perception, visceral regulation, and motor control
– projections to the forebrain are important in modulating mood, cognition, and neuroendocrine function
– Autoreceptors (control local neurotransmitter concentration)
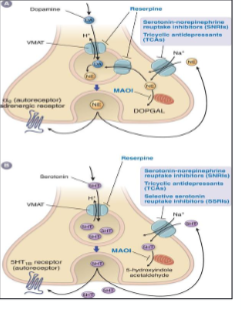
what is 5-HT synthesis and metabolic cycle?
Synthesised from tryptophan
• VMAT transport 5-HT
METABOLIC PATHWAY
• 5-HT transporter (SERT)
• Cytoplasmic 5-HT
VMAT
monoamine oxidase (MAO)

what are 5-HT receptors?
All G-protein coupled receptors but one
• mediate excitatory and inhibitory neurotransmission
• Presynaptic and postsynaptic expression
• 15 receptors classified in 7 families
where are 5-HT receptors located?
CNS
Body organs such us lungs, heart, stomach, smooth muscle…
what is norepinephrine?
NE-containing cells within the locus coeruleus
– projections throughout the cortex modulate vigilance, stress responses, neuroendocrine function, pain control, and sympathetic nervous system
Auto-receptors (control local neurotransmitter concentration)
what is NE synthesis?
DA transported into the vesicle by VMAT
Inside the vesicle→ DA is converted to norepinephrine by dopamine β-hydroxylase
Autoreceptors→ α2-adrenergic→ provide feedback inhibition

what is the NE metabolic cycle?
NE cleared from synapse by the NE transporter (NET)
Cytoplasmic NE
VMAT
monoamine oxidase (MAO)

what is the pharmacology for depressive disorders?
Reuptake inhibitors
Tricyclic antidepressants (TCAs)
Selective serotonin reuptake inhibitors (SSRIs)
Serotonin / Noradrenaline reuptake inhibitors (SNRIs)
• Monoamine receptor antagonists
• Monoamine oxidase inhibitors
• Melatonin receptor agonist
• Other agents→ Ketamine
what are the clinical implications of antidepressants?
5-HT release is controlled by the inhibitory activity 5- HT 1A receptors
Clinical effect affect some weeks (around 6 weeks)
what are the clinical implications of antidepressants before treatment?
5-HT pathologically low levels → low baseline level of postsynaptic receptor activity
what are the clinical implications of antidepressants during short-term usage?
↑ release or duration of neurotransmitter → ↑ stimulation of inhibitory autoreceptors → postsynaptic receptor activity = pretreatment levels
what are the clinical implications of antidepressants after chronic use?
desensitization of the presynaptic autoreceptors → ↑ postsynaptic receptor activity
what are tricyclic antidepressants?
Second-line treatment, widely used, mainly imipramine
As or more effective as SSRIs, worse side effects, overdose risk
• Mechanism of action
– Blocking SERT and NET
– Increased receptor activation→ enhancement of postsynaptic responses
what are the side effects of tricyclic antidepressants?
– No selective drugs
– CV effects (lethal conduction delays)
– Anticholinergic side effects→ nausea, vomiting, anorexia, dry mouth, blurred vision, confusion, constipation, tachycardia, and urinary retention
– Antihistaminergic side effects→ sedation, weight gain, and confusion
what are selective serotonin reuptake inhibitor mechanism of action?
All SSRIs are highly selective for SERT
• Depending the dose→ higher doses binding with NET
• Sertraline and Vilazodone→ 5-HT1A partial agonist
what are the side effects of SSRIs?
– GI issues (esp. nausea), sexual dysfunction, agitation / anxiety, insomnia, drowsiness, increased appetite
Low overdose risk lower adverse effect
All SSRIs have a long half-life (18+ hours); oral tablets once daily – Fluoxetine→ Long duration (t1/2 up to 96h)
what is serotonin syndrome?
Excessive serotonergic activity
• Mostly associated with SSRIs and MAOIs (overdose or drug-drug interactions)
– Avoid with MAOIs (2-week gap)
what are the symptoms of serotonin syndrome?
• High body temperature (potentially >41C)
• Sweating
• Agitation
• Tremor & hyperreflexia
• Dilated pupils
• Diarrhoea
• If severe, potentially seizures & rhabdomyelitis
what is venlafaxine?
Serotonin and Noradrenaline reuptake inhibitors
– Block the 5-HT reuptake transporter lower doses
– Block NE reuptake transporter higher doses
what is duloxetine?
a type of SNRI
– inhibits NE and 5-HT reuptake
– is non-selective → also inhibits DA uptake
– fewer side effects than Venlafaxine and low risk of overdose
what are the side effects of SNRIs?
– similar to SSRIs
– greater risk of high blood pressure
– Withdrawal symptoms
what is mirtazapine?
– presynaptic alpha2-adrenoreceptor antagonist
– increases central noradrenergic and serotonergic neurotransmission
what are the side effects of mirtazepine?
Anxiety, appetite increased, back pain, confusion constipation, dizziness, drowsiness, dry mouth, fatigue, headache…
Cautions: Cardiac disorders; diabetes mellitus; elderly; history of mania (discontinue if patient entering manic phase)
what is trazodone?
– Blocks 5-HT2A, 5-HT2C, Histamine H1. Weak 5-HT reuptake inhibitor
what are monoamine oxidase inhibitors?
Inhibit the monoamine degradation → increase cytoplasmic and storage level/ leakage in synaptic cleft
what is the classification of MAOIs?
– MAO-A and MAO-B
– reversibility or irreversibility of their binding
what are newer MAOIs?
Moclobemide, befloxatone, and brofaromine
– Moclobemide → Selective MAO-A inhibitor. Short acting and reversible
– Specific MAO-B inhibitors are not used for depression, but are useful for Parkinson’s disease
what are the major side effects of antidepressants?
Sexual dysfunction → sexual arousal suppressed by 5-HT1A receptor agonism
Weight gain - 5-HT2C agonism suppresses appetite; desensitisation chronic use
Insomnia → Regulation of sleep via numerous 5-HT receptors
Anxiety & agitation → NA & 5-HT (esp. via 5-HT2C) promote brain activity
GI disturbances & nausea → 5-HT major neurotransmitter of the enteric nervous system; 5-HT3 receptors in emesis
Adherence → ~50% patients still taking antidepressants without consultation 6 months after first prescription.
what are general cautions with antidepressants?
High bleeding risk→ Role of serotonin in platelet signalling
Gastrointestinal bleeding→5-HT major role in GI tract
Migraine medications
“triptans” also work via 5-HT receptors
Suicide risk→ Abrupt withdrawal from SSRIs→ SSRI-discontinuation syndrome
what is vortioxetine?
SERT inhibitor, 5-HT3 antagonist & 5-HT1A agonist
– Lower effects of sexual dysfunction
what is agomelatine?
– Melatonin MT1 & MT2 agonist; 5-HT2B & 5HT2C antagonist
– Disinhibition of prefrontal NA/DA activity; use in sleep disorders (MT)
– Low sexual dysfunction, weight gain, withdrawal side effects
– Cautions with patients with liver disease
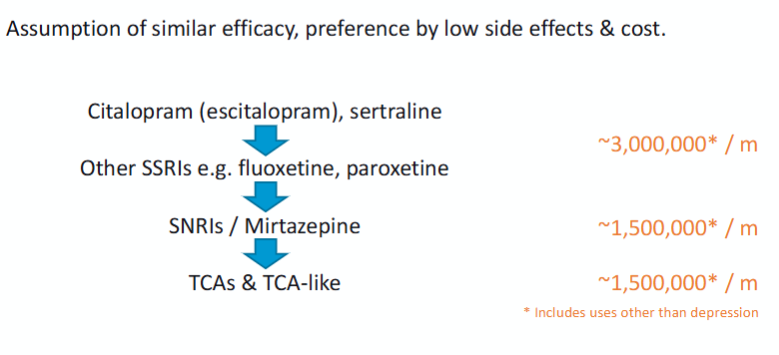
what is the effectiveness of antidepressants?
Controversy: many studies suggest little better than placebo
Generally held to be effective→ especially in severe depression
All antidepressant classes have similar effectiveness
– Usually side effects determine preference
– SSRIs > SNRIs > TCAs
what is the stepped care model?
Step 1 Mild depression: assessment, support, psychoeducation & monitoring
Step 2 Mild-moderate depression: low intensity psychosocial & psychological interventions, medication, referral to further assessment
Step 3 Moderate depression: medication, high intensity psychological interventions, combined treatment, referral to further assessment
Step 4 Severe depression: medication, high-intensity psychological interventions, ECT, crisis service, combined treatments, multiprofessional and inpatient care
what are the prescribing guidelines?
what is the drug treatment of bipolar disorder?
– lithium
– several antiepileptic drugs (carbamazepine , valproate , lamotrigine)
– some antipsychotic drugs (olanzapine , risperidone , quetiapine…)
– Other agents→ BZD (to calm, induce sleep and reduce anxiety)
what is lithium?
– an inorganic ion (taken orally as lithium carbonate)
The classical drug
– in prophylaxis and treatment of mania
– prophylaxis of bipolar or unipolar disorder (recurrent depression)
– there is a narrow therapeutic window and long duration of action
what is the mechanism of action of lithium?
is not understood
– interference with inositol trisphosphate formation
– inhibition of kinases
what are the side effects of lithium?
– Acute toxic effects include cerebellar effects, nephrogenic diabetes insipidus and renal failure
Dose must be adjusted according to the plasma concentration
what are antiepileptic drugs?
carbamazepine , valproate , lamotrigine
– better side effect and safety profile
– sodium-channel blockade
Valproate and carbamazepine are effective in treating acute attacks of mania and
in the long-term treatment
Lamotrigine effective in preventing the recurrence of both mania and depression.
what are second generation antipsychotic drugs?
Atypical antipsychotic drugs
– Olanzapine , risperidone , quetiapine , aripiprazole and also haloperidol
• Mechanism of action
– D2 and 5-HT2A receptor antagonist
– Actions in other receptors/ transporters
• Mainly, to treat mania
• Used in combination with lithium or valproate