S1W7: AMD-non LV considerations
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
What is the relationship between nutrition and AMD according to oxidative stress theory?
Oxidative stress theory = most popular explanation
Research focuses on antioxidant therapy to reduce circulation of ROS
Antioxidants linked with risk reduction:
Vitamins C and E
Zinc
Omega-3 fatty acids
Carotenoids (xanthophylls and carotenes)
Largest related clinical trials: AREDS I and II
What is the role of Vitamin C in AMD management?
Water-sol antioxidant -protects against free radical damage
Acts as an e- donor, interrupting oxidative proc’s
e.g citrus fruits, tomatoes, green peppers, broccoli, cauliflower
Often administered alongside other vits + minerals
AREDS I: showed reduced risk of progression to advanced AMD after 6.3 years in those w/ existing AMD
Results came from a well-nourished population; outcomes may differ in other groups

What is the role and evidence for Vitamin E in AMD?
Group of 8 fat-soluble compounds w/ antioxidant ability
Key function: stops ROS production when fats undergo oxidation
e.g almonds, safflower oil, corn oil
Women’s Health Study: no signif reduction in visually signif or advanced AMD vs placebo
What did the Cochrane review find?
Vitamin E
Vitamin E + beta-carotene does not delay or prevent AMD onset
Highlighted that vitamin supplements may also have harmful effects
What is the role of Zinc in ocular health and AMD?
Mostly found in retina + choroid
Acts as a cofactor for antioxidant enzymes
Helps transport vitamin A to the retina, necessary for melanin production
Not produced by the body → must be obtained through diet, supplements, or fortified foods
e.g red meat, seafood, poultry, eggs, wheat germ, mixed nuts, black-eyed peas, tofu, beans

Where is zinc found in the human body and how is it taken up?
Human body contains ~2–3 g zinc
Found in muscle + bone
Oral uptake occurs via small intestine
Distributed by serum, most zinc bound to proteins (albumin, transferrin, p-macroglobulin)
Uptake can also occur by inhalation + through the skin
What factors affect zinc levels, and what issues can arise from supplementation or diet?
High supplemental zinc dosage can lead to copper deficiency due to competitive absorption
Diet surveys show low zinc intake in the elderly, irrespective of country
Causes incl:
reduced consumption of zinc-rich foods (e.g., red meat)
reduced absorption w/ older age
What are the key types and functions of PUFAs relevant to ocular health?
2 groups: Omega-3 + Omega-6 PUFAs
DHA:
major dietary + structural omega-3 long-chain PUFA, predominantly present in disc mem’s of PR’s
EPA :
thought to have anti-inflammatory properties
Rich omega-3 sources
e.g flaxseeds, walnuts, sardines, and salmon
How are PUFAs linked to AMD risk, and what considerations affect serum lipid interpretation?
High dietary intake of omega-3 FA’s =assoc’d w/ a reduction in risk of late AMD
AREDS 2 reported no additional risk reduction in progression of advanced AMD
Serum lipid levels must be interpreted w/ caution
comparisons depend on underlying medication + disease

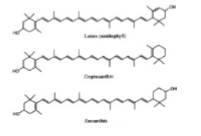
What are carotenoids and how are they classified?
Organic pigments
found in plants, algae, fungi, and some bacteria
Cannot be synthesised by humans or animals → must be consumed
2 types:
Xanthophylls (oxygen-containing)
Carotenes (hydrocarbons only)
Which carotenoids have vitamin A activity and which form the macular pigments?
4 carotenoids w/ vit A activity:
β- + α-carotene, γ-carotene, and β-cryptoxanthin (can be converted to retinal)
These+ other carotenoids can act as effective antioxidants
Lutein, meso-zeaxanthin, + zeaxanthin = xanthophylls that form the macular pigments
Pigments give macula its characteristic yellow appearance
Highest conc of lutein + zeaxanthin at fovea, dec’ing w/ eccentricity
What are the properties of xanthophylls?
Absorb blue light
Are antioxidants
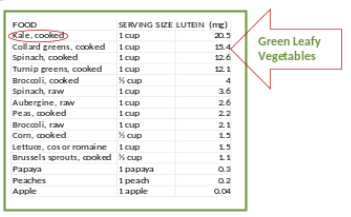
What are macular pigments and where are they found in the diet?
Macular pigments: lutein + zeaxanthin
Food sources incl green leafy vegetables (spinach, kale) + fresh fruit
What is the evidence linking macular pigment levels and dietary intake with AMD risk?
Dec’d serum, dietary, + retinal levels have been assoc’d w/ inc’d AMD risk in some but not all observational studies
In AREDS I, higher dietary intake (measured via FFQ) was linked to a lower risk of developing advanced AMD
What is known about lutein supplementation, macular pigment optical density, and AMD progression?
Lutein supplementation + inc’d macular pigment optical density have been assoc’d,
but their relevance + relationship to AMD is NOT fully established
AREDS 2 reported
NO extra reduction in risk of progression to advanced AMD from adding lutein + zeaxanthin
What key factors should be considered when evaluating a study on AMD risk or progression?
Study outcomes:
reducing risk of AMD incidence or reducing risk of AMD progression
Study sample:
age, ethnicity, location, sample size, effect size/change
Study type:
observational, cross-sectional, intervention, placebo-controlled, cross-over, longitudinal
Outcome measures:
VA, serum, CS, OCT parameters, lesion size
Measurement of study parameters:
How was diet assessed?
How was supplement intake controlled?
What is the current evidence regarding diet, supplements, and AMD incidence versus progression?
Most studies have evaluated risk of AMD progression
To date, there is NO evidence that diet or dietary supplements can prevent AMD development
Why is it difficult to measure whether diet or supplements can prevent AMD from developing?
Measuring prevention would req using the same pt twice:
Once w/o intervention, hoping they develop AMD
Then again w/ intervention, hoping they do not develop AMD
Imposs due to absence of reincarnation + cloning
What factors related to age, ethnicity, and location should be considered when evaluating a study sample?
Age:
consider age range in relation to study methods, incl compliance + cognitive abilities
Ethnicity:
results useful for your clinical setting? applicable to your pt population
Location:
May influence diet, population characteristics + environ factors
What sample size and effect size considerations are important when interpreting study findings?
Sample size:
how large (sample) + how much power study had?
Can you draw concl’s from this study to suit a larger population/ your pt population?
i.e. if all cases of a given disease were assessed -any "stronger" conclusions from it compared to a situation where you might have only a proportion of a population
Effect size
how much did the parameter change/ what is the spread?
What should be considered when evaluating study type and outcome measures
Was study ST/LT + how were concl’s drawn?
Were all measurements repeated at each time point?
Are the outcome measures perceivable by the pt?
What “improvement” means (e.g., better vision/overall health?).
Check whether control subjects or placebo treatments were used.
How is dietary nutrient intake measured in study parameters?
Sampling info from indiv
Non-contact methods (no practitioner required):
Food frequency questionnaires
Food diaries
Compare frequency questionnaires and food diaries
Frequency questionnaires
Pt ticks off foods on a list that they have eaten each day.
Foods often left out of the lists.
Food diary
Pt journalises their intake.
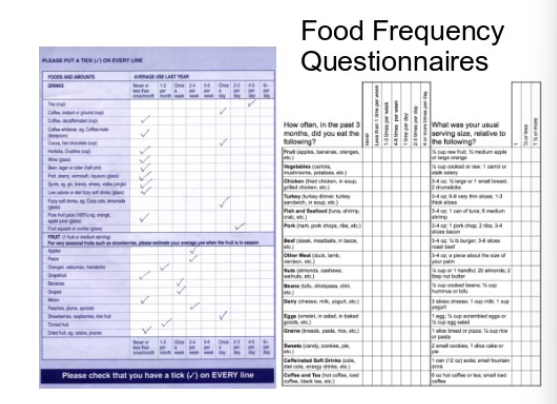
What are the limitations of frequency questionnaires and food diaries?
Self-report method tends to underestimate food intake.
Portion sizes = diffic to det unless everything is weighed + measured.
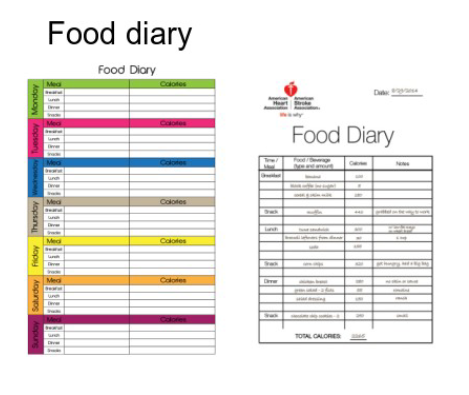
What discussion points highlight limitations of FFQs and food diaries?
Are all food groups listed?
Seasonality.
Weight measures.
Difficulty remembering food from 1 week ago.
Difficulty remembering food from 50 years ago (e.g., age 70).
Tendency to tick “what you should eat” vs “what you really ate”.
What problems occur with Food Frequency Questionnaires and Food Diaries?
FFQs issues:
Often no record of portion intake
Summary over several days
No info on meal prep
Predefined lists lead to omitted or wrongly grouped foods
Food diary issues:
Very focused on calorie counting
Diffic to judge portion size unless defined
Does not accommodate changes in calorific intake from cooking methods
Difficulty collating “food groups”
What are the contact methods used to measure or estimate nutrient intake?
Contact methods require a practitioner.
Blood serum levels (HPLC): reflects S-T nutrient intake.
MPOD (macular pigment optical density): reflects L-T dietary exposure, only an indirect measure.
What are the limitations of blood serum testing for nutrient intake?
Invasive for pt’s
Must be used alongside food diaries/FFQs
Absorption + excretion vary with age, disease, meds
Usefulness = debatable due to indiv variability
How much antioxidant intake is enough for macular health and AMD?
Healthy macula: varied, balanced diet provides sufficient antioxidants.
Indiv’s w/ or at risk of AMD req higher antioxidant intake to slow oxidative effects.
Research has investigated effects of diff antioxidant doses on AMD progression
results remain inconclusive.
What were the inclusion criteria for the AREDS study?
Age 50–85 years
Either:
Bilat large drusen, or
Large drusen in one eye + advanced AMD (neovascular AMD or central GA) in fellow eye
At least 75% run-in medication consumed (verified by remaining tablet/capsule count)
Smokers allowed to participate
What were the exclusion criteria for the AREDS study?
Under 50 or over 85 years
AMD affecting one eye only
Non-compliance with supplementation adherence
Taking any other supplementation
What were the key findings and formulation details of the AREDS study?
Clinical trial on supplementation in AMD
Taken for 6 years:
• Vitamin C 500 mg
• Vitamin E 400 IU
• β-carotene 15 mg
• Zinc oxide 80 mg
• Cupric oxide 2 mgShowed 25% risk reduction in progression to advanced AMD over 5 years in pt’s w/ intermediate AMD or advanced AMD in one eye
19% reduction in risk of losing ≥3 lines of vision
What were the key design features and participant details of the AREDS study?
3640 pt’s w/ AMD
Pt’s ranged from:
• No evidence of AMD in either eye
• To advanced AMD with vision loss in 1 eye but good vision in the other90% of participants followed for ≥5 years
Always look at pt no’s + FU numbers
What were the key findings of the Age-related Macular Disease Study (AREDS II)?
2013
Study added lutein (L) and zeaxanthin (Z) to the original AREDS formulation
Overall: Did not further reduce risk of progression to advanced AMD
Sub-analysis: substituting L and Z for beta-carotene reduced progression risk by an extra 18%
Beta-carotene may have masked benefits of L + Z in overall analysis
L + Z =useful substitutes for beta-carotene in the original formulation
What were the AREDS 2 study enrolment criteria and patient characteristics?
Study added lutein + zeaxanthin to orig AREDS formula
At enrolment pt’s had either:
bilateral large drusen
large drusen in 1 eye + advanced AMD (neovascular AMD or central geographic atrophy) in the fellow eye
What were the AREDS original and new supplement formulations?
Original formula:
Vitamin C 500 mg, Vitamin E 400 IU, β-carotene 15 mg
Zinc: zinc oxide 80 mg + cupric oxide 2 mg
Zinc reduced from 80 mg to 25 mg
Lutein + zeaxanthin substituted for beta-carotene
What were the outcome findings of AREDS 2?
Adding L + Z did not further reduce risk of progression to advanced AMD
No adverse effects found w/ this formulation
What is the current gold-standard supplement formulation for AMD?
AREDS 2 formulation is the current ‘gold standard’ (only large-scale clinical trial)
Lutein = 10 mg
Zinc = 25 mg
Zeaxanthin = 2 mg
Copper = 2 mg
Vitamin C = 500 mg
Vitamin E = 400 IU
How was compliance tested in AREDS 2?
Trial phase prior to study enrolment
Why is a balanced diet insufficient for lutein/zeaxanthin intake in those with or at risk of AMD?
Simple balanced diet generally does not provide the req’d 10 mg of L+Z
Standard portions of most veg + fruits do not contain enough lutein to meet this req
What is the current situation with UK dietary supplements for eye health?
No regulation (classed as complementary meds)
Often contain antioxidants in varying doses plus extra ingredients (e.g., vit B, bilberry extracts, sunflower seed oil, marigold extract, beeswax)
Aggressively marketed + often claim to be “backed by professionals”
Where are nutritional supplements sold in the UK?
Pharmacies
Supermarkets and other food shops
High-street optical and contact lens practices
Hospitals and university institutes
Internet pharmaceutical companies
Internet shopping companies (e.g., Amazon)
No regulation on who can buy them
Many have no age restriction (some packaging states “not for under 18s” but not enforced)
When and how much nutritional supplementation should be used for AMD?
Only formulations supported by large-scale clinical trials are from AREDS + AREDS 2.
Incl+ excl criteria guide decisions on who, which + when supplementation is appropriate.
Problem: AREDS 2= complex study, practitioners may be confused about what to advise.
What are the problems with over-the-counter or remote-purchased medications?
Diff combo’s + dosage rec’s for which no evidence exists
Dosage rec’s largely vary
Remote purchasing or in outlets w/ no professional advice
Risk of not considering interactions w/ current medication or health status
What did the Aston University survey reveal about AMD patients’ nutrition and supplement use?
Many AMD patients confused over beneficial foods
Pts taking variety of supplements, none AREDS 2, some doubling or tripling dose
Food diary analysis: avg 1.3mg lutein/day, much lower than recommended 10mg/day for AMD or at-risk patients
What additional issues did the Aston University survey find regarding AMD patients’ information and knowledge?
Pt’s felt they did not have enough info from optoms or ophthalmologists
Concern over conflicting advice from ECP’s
When quizzed on nutrition, none could name useful nutrients or describe why they were beneficial
When is supplement advice proven to affect AMD progression?
Pts aged 50–85 years
Pts with drusen >125 µm and/or geographic atrophy involving the centre of the macula
Plus a fellow eye with drusen >125 µm and/or geographic atrophy not involving the centre of the macula
What dietary modification advice is given for AMD patients or at-risk patients outside supplement criteria?
To get a good mix of antioxidants, L+Z, incorporate one of the following daily:
2 eggs
1 cup (150 g) cooked kale
1 cup (150 g) cooked spinach
Must be eaten every day to get the required L+Z
What is the optometrist’s role in nutrition advice for AMD patients?
Give nutrition advice to all patients w/ or at risk of, AMD
Ensure pt’s have access or can prepare + cook healthy food
Pts with visual impairments may need extra help; may require referral for low vision support
What tools and considerations support optometrists in advising AMD patients?
Clinical decision-making aid (Aston University) -help decide when and what to advise
Knowledge of products + their indications
Follow best practice + clinical guidelines on prescribing supplements
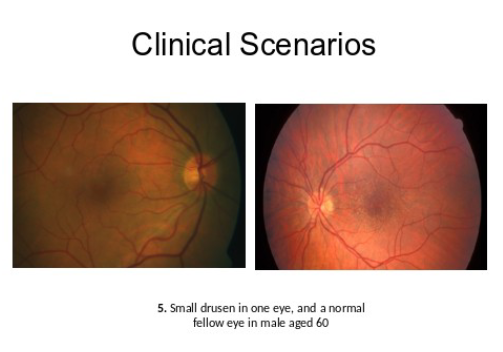
What should be considered when evaluating AMD patients for exercise-based case studies?
Evaluate disease stage from images
Assess evidence for benefit from supplementation or dietary modifications
Consider:
evidence, age+ disease stage
reducing risk of developing AMD vs risk of AMD progression
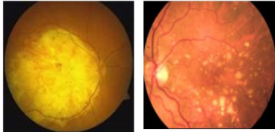
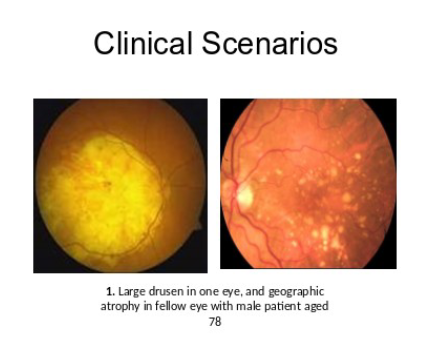
Clinical scenario 1
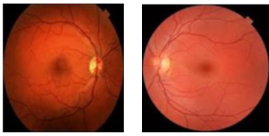
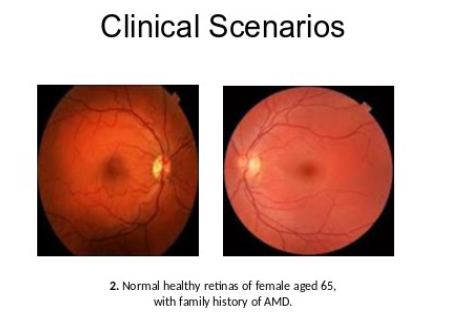
Clinical scenario 2
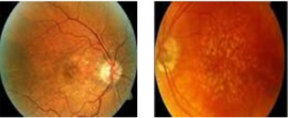
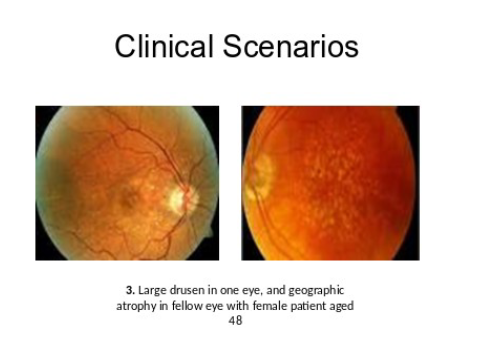
Clinical scenario 3
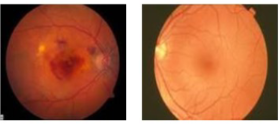
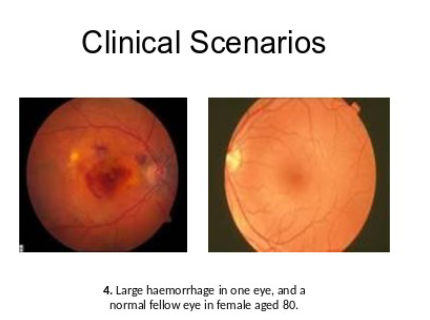
Clinical scenario 4
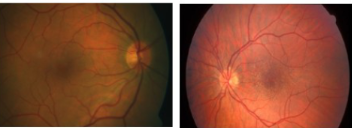
Clinical scenario 5
What are the key conclusions about nutrition and AMD?
Nutrition can slow AMD progression, poss via an overall healthier lifestyle, evidence = inconclusive
Optoms responsibility to give nutrition advice to those with, or at risk of, AMD
Advice can be based on AREDS 2 incl/excl criteria
What is the take-home message regarding nutrition and supplements for AMD?
Nutritional substances can benefit AMD pts + those at risk
Req’d amounts depend on indiv diet + lifestyle
Consider diet, lifestyle + other factors
What considerations are needed when recommending nutritional supplements in AMD?
Nutrient uptake depends on indiv absorption; some combos may be unsuitable due to competition
Those recommending supplements must advise on adverse effects and overdosing, as supplements fall outside medicine regulation
What future developments are anticipated in eye health and AMD?
Anti-ageing for the eye: synolitics
Microbiome analyses: gut-ocular and gut-brain axes