IMED1004 - Diabetes 1 and 2 (L23 and 24)
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Pancreas and Insulin
- the endocrine portion of pancreas is formed by pancreatic islets or "islets of langerhans"
- the islets have different populations of cells
- alpha cells -> glucagon
- beta cells -> insulin
- gamma cells -> somatostatin
.
Diabetes Mellitus describes two conditions where insulin secretion and/or signalling are disrupted
Symptoms of diabetes
- in both types of diabetes, insulin signalling is disrupted
Normally, insulin:
- decreases high, post-prandial blood glucose concentrations
- promotes the transport of glucose into tissues for use and storage
.
Without insulin:
- blood glucose concentrations become elevated
- energy from blood glucose is not stored
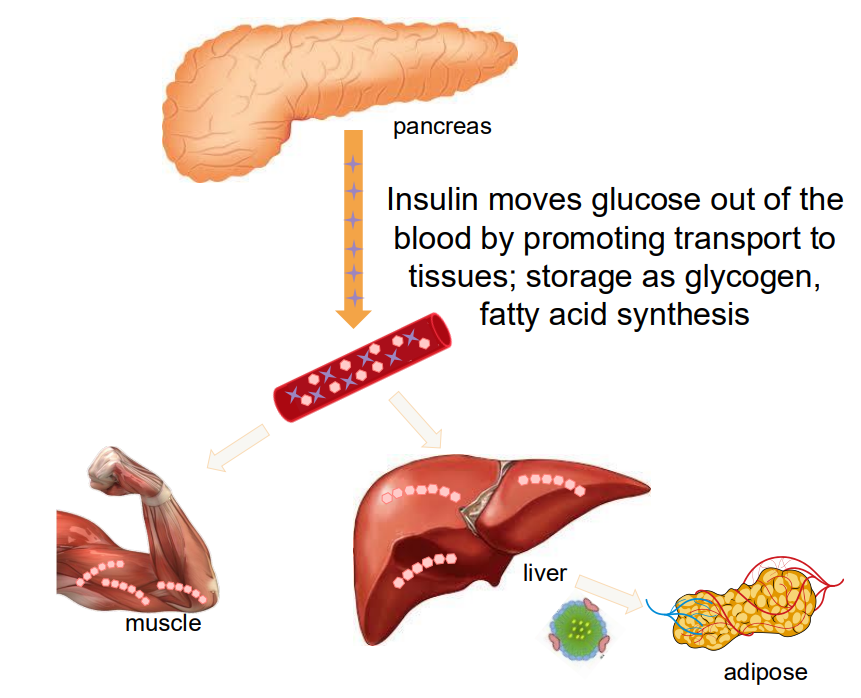
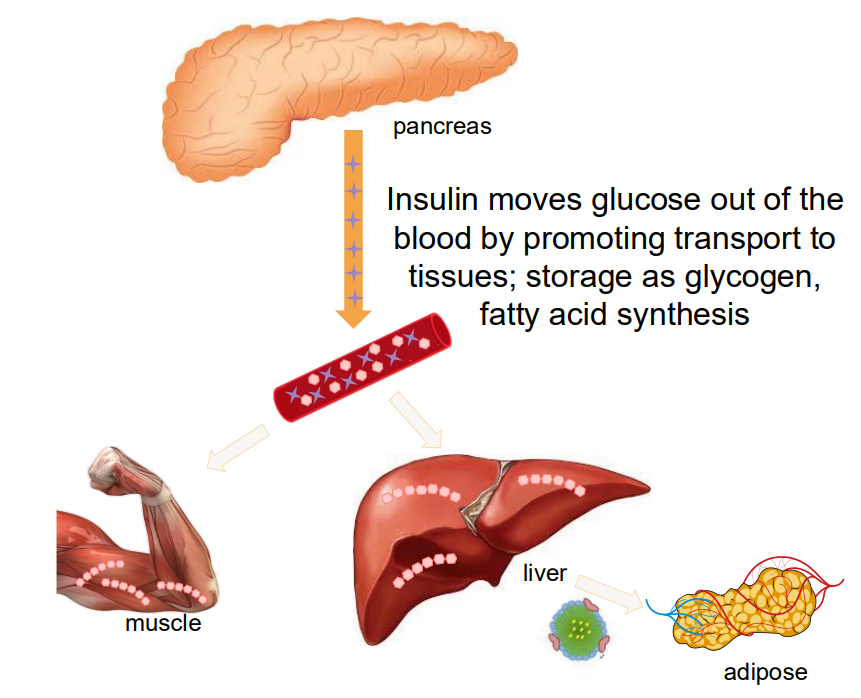
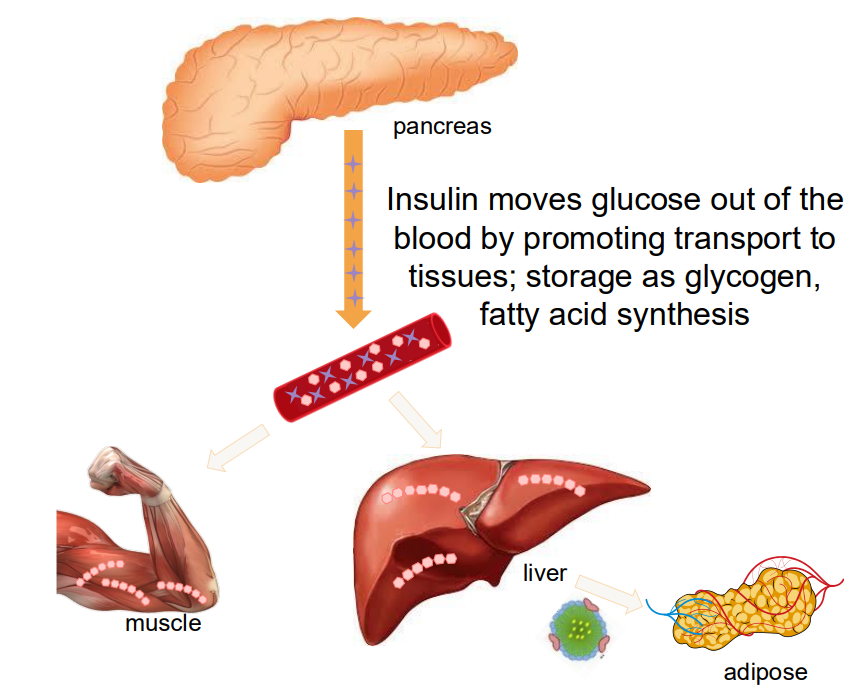
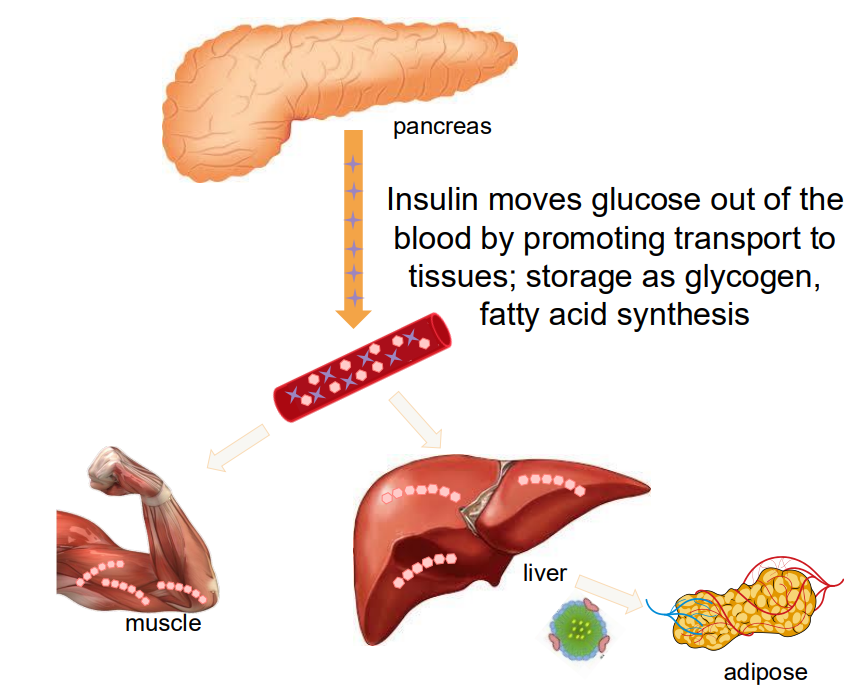
Insulin path
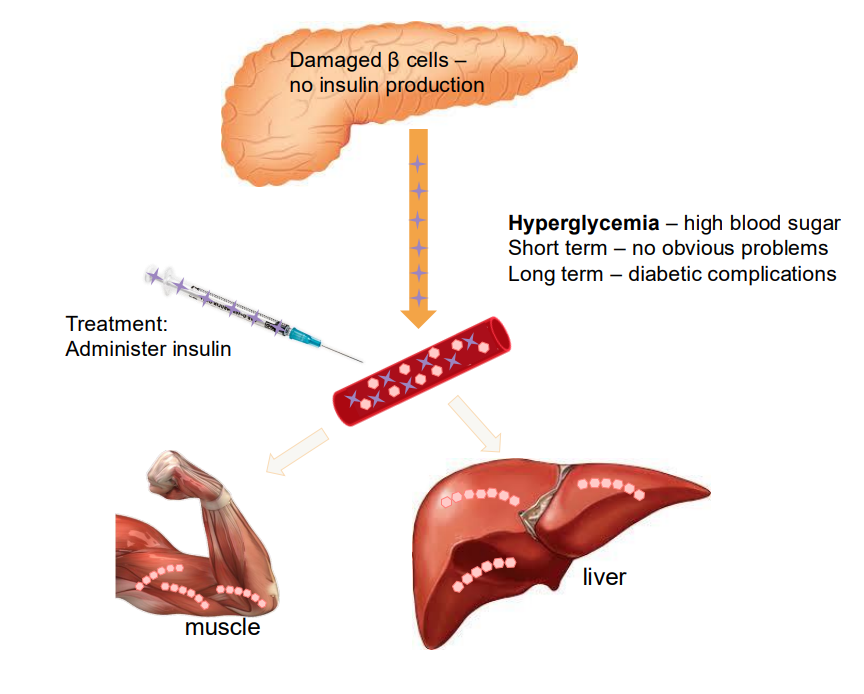
- insulin moves glucose out of the blood by promoting transport to tissues; storage as glycogen, fatty acid synthesis
DIAGRAM ON SLIDE 7
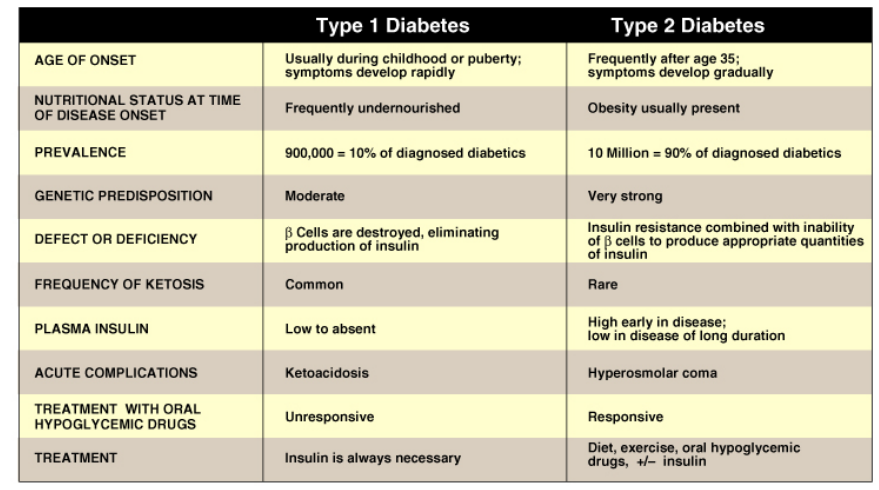
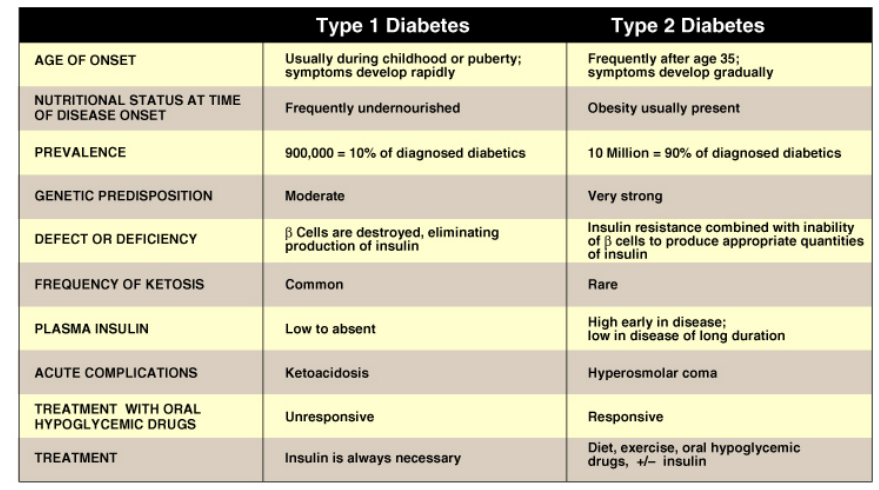
There are two types of diabetes mellitus
TYPE 1: INSUFFICIENT PRODUCTION OF INSULIN
- autoimmune destruction of beta cells
- usually develops early in life
- previously known as: insulin-depdendent diabetes, juvenile diabetes
- 10-15% of all diabetic cases
.
TYPE 2: INSULIN RESISTANCE:
- usually develops in late adulthood
- associated with obesity
- cells don't respond appropriately to insulin
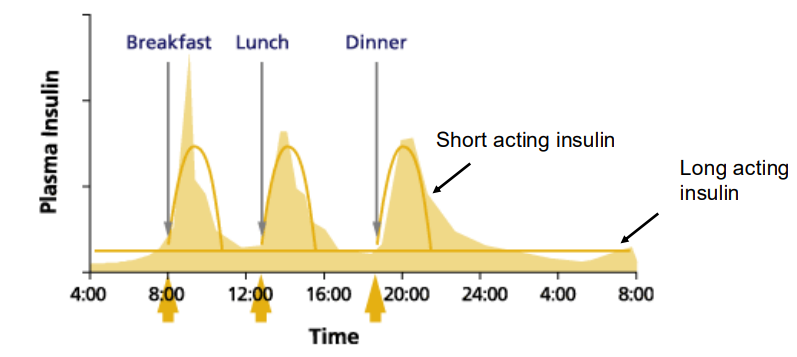
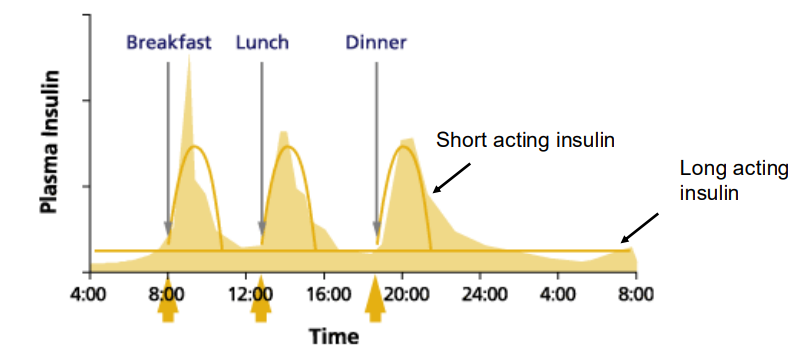
Management of blood glucose levels in type 1 diabetes
TWO TYPES OF INSULIN:
- long acting - maintains basal rate of glucose uptake
- short acting - after eating, when a high level of glucose is available
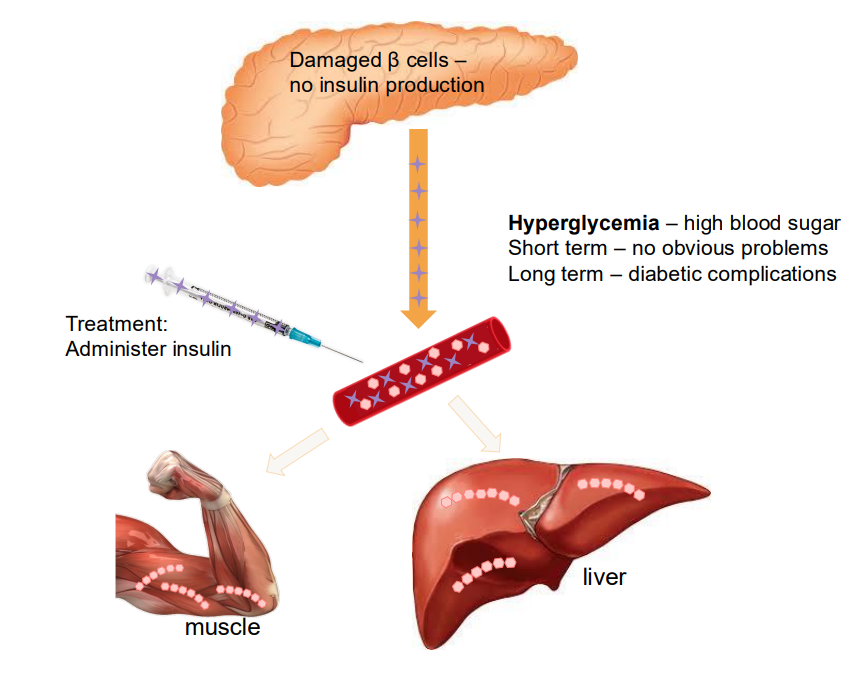
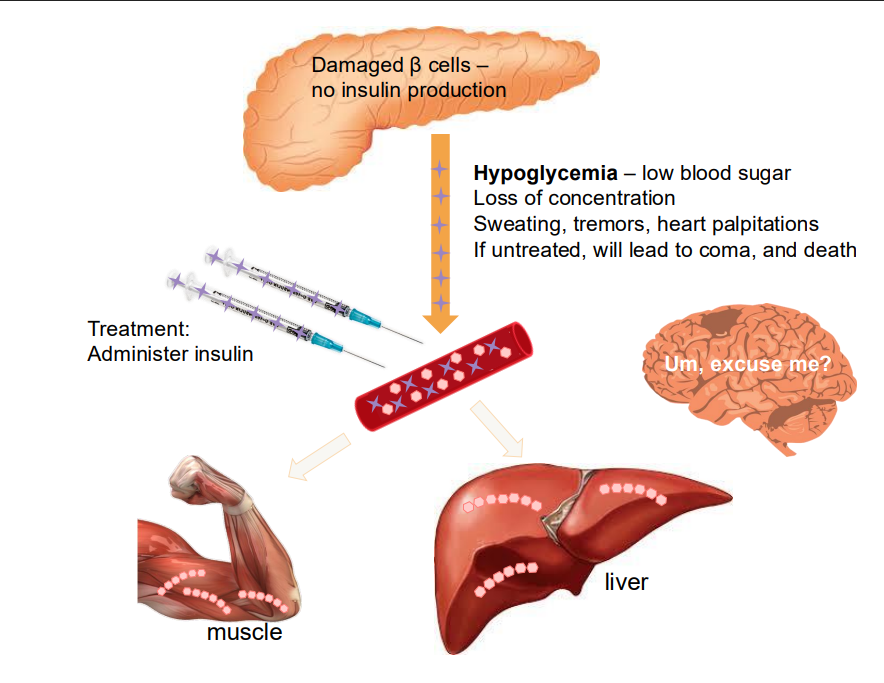
Damaged Beta cells
- no insulin production
- hyperglycaemia - high blood sugar. Short term has no obvious problems but long term has diabetic complications
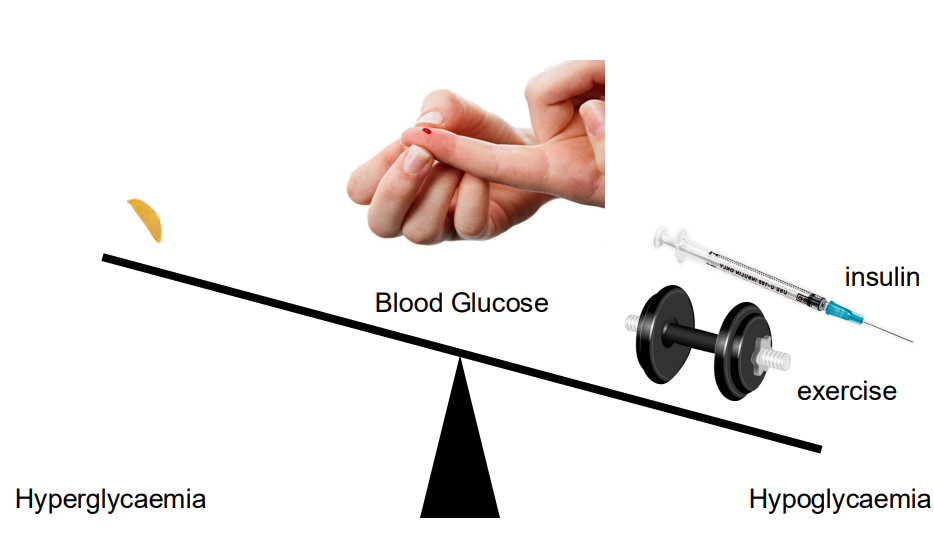
Managing blood glucose levels in type 1 diabetes - a matter of balance
- we have to balance the amount of carbohydrate we consume vs how much insulin we inject
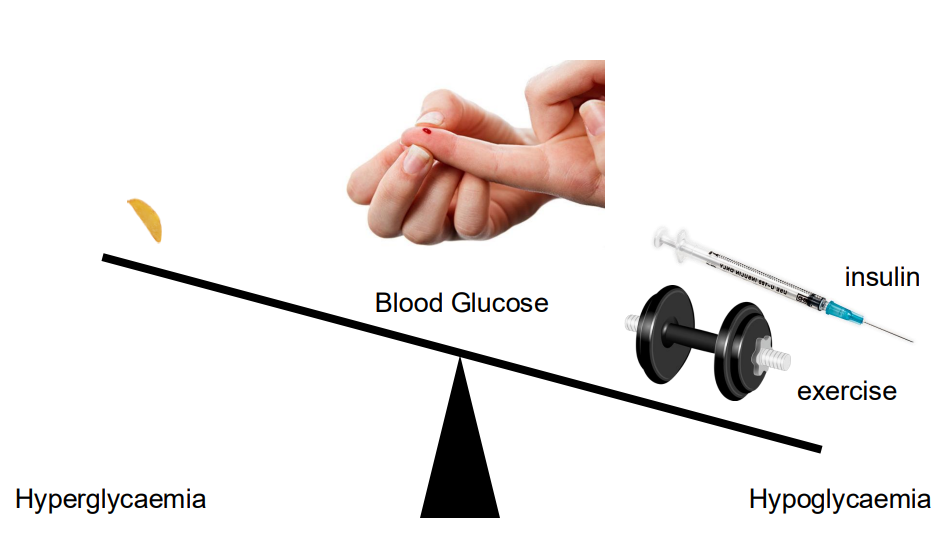
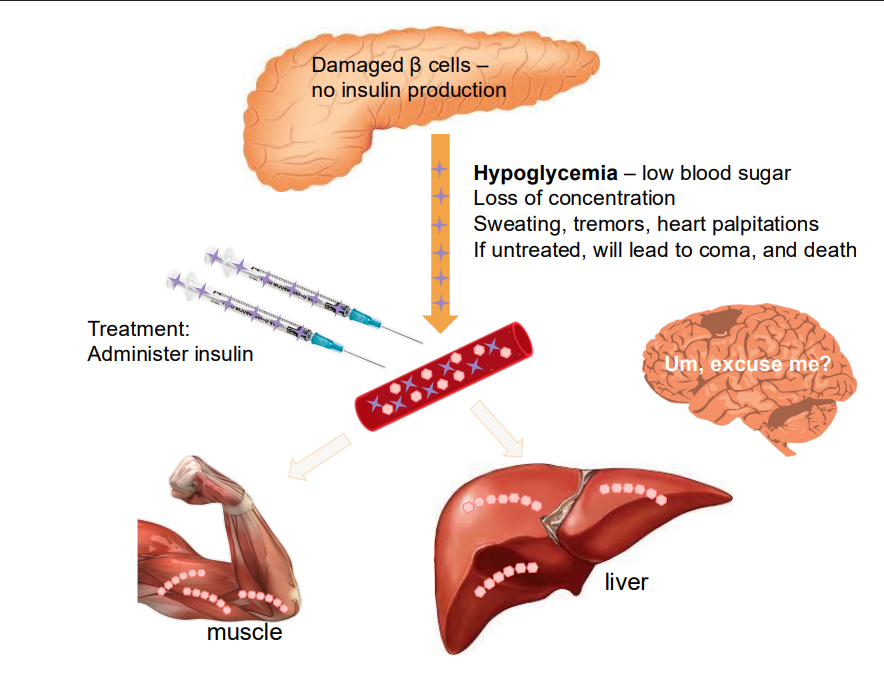
Hypoglycaemia
- can be caused if we add too much insulin
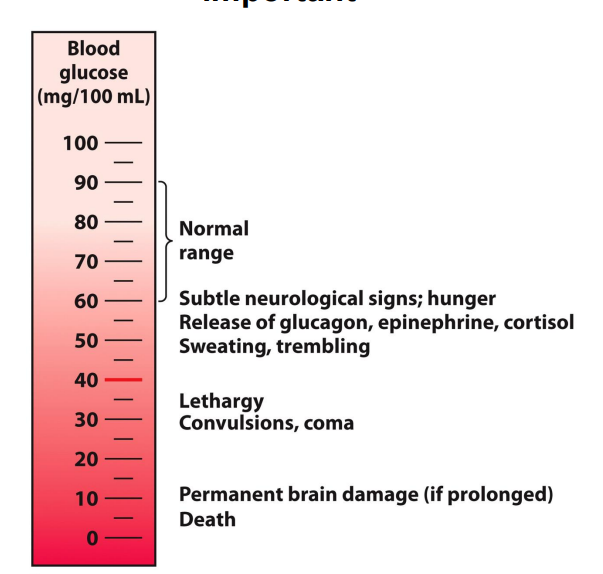
Maintaining appropriate blood glucose levels is important
- normal range: 60-90mg/100mL
Ketoacidosis and Type 1 Diabetes
- fat breakdown is accelerated -> high production of ketone bodies
.
without any insulin, there is uncontrolled ketone production - no "brake" on producing ketone bodies (hence rapid weight loss)
- Some of the ketones are ketoacids
- Blood [H+] is raised -> ketoacidosis
- Bicarbonate buffering system activated (compensation: breathing is altered (remove more CO2 to increase pH)
- Breakdown of ketone body acetoacetate producces acetone (expelled in breath)
- untreated diabetes leads to dramatic weight loss

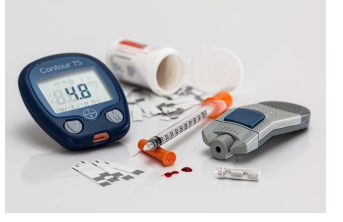
Blood Glucose Monitoring
- Type 1 diabetes frequently monitor blood glucose levels (fingerprick blood glucose, 4 times a day)
Blood glucose monitoring: glycaemic control
HbA1c (DIAGRAM ON SLIDE 15, the text of HbA1c)
- measures glycosylation of haemoglobin in red blood cells
- indicates average glycaemic control
- measures every 3 months
.
- protein glycosylation (free amino groups)
- haemoglobin can become glycosylated (abundant, many exposed amino groups, entry of glucose into erythrocytes isn't regulated -> easily glycosylated)
Now the slides will focus on type 2
- usually develops later in adulthood
- asociated iwth obesity
- calls dont respond appropriately to insulin
Insulin receptor signalliong
- insulin is a Receptor Tyrosine Kinase
NO LEARNING OUTCOME
Risk factors for type 2 diabetes
- Age > 40
- Family history of diabetes
- Ethnicity
- Obesity; abdominal fat distribution (sedentary lifestyle)
- hypertension, hyperlipidaemia
- previous impaired glucose tolerance
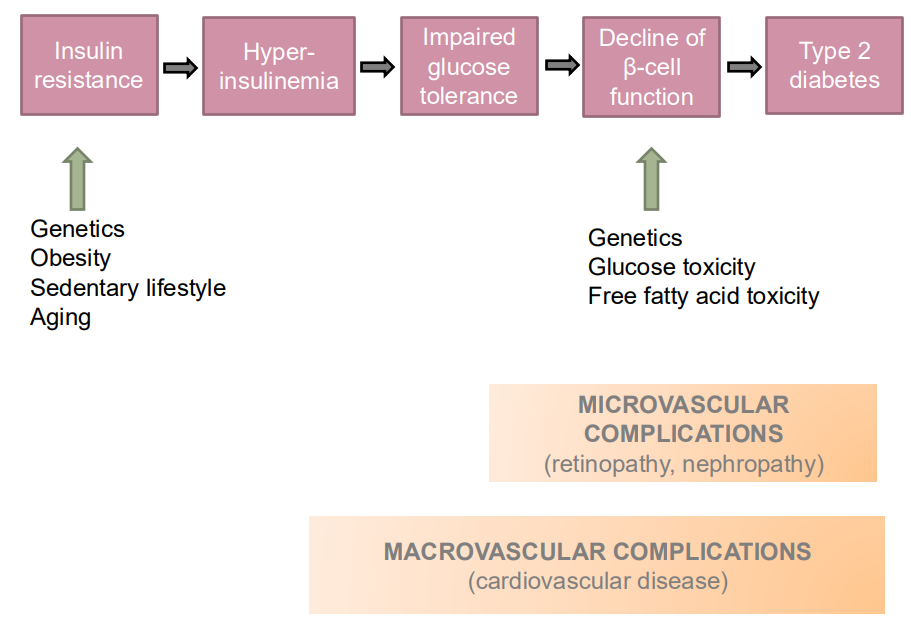
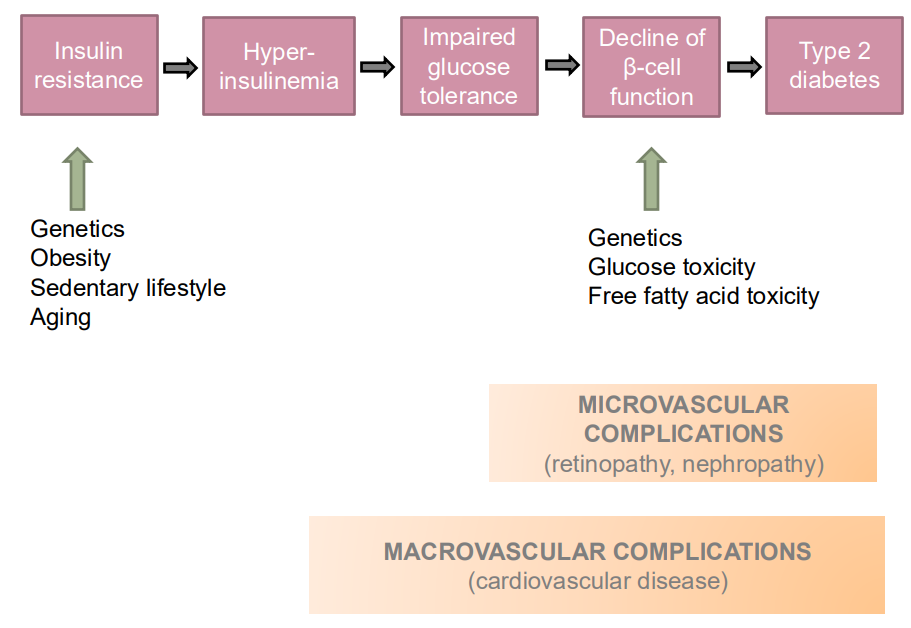
Type 2 Diabetes flow chart
- insulin resistance leads to hyperinsulinemia which leads to impaired glucose tolerance, leading to decline of beta cell function, which leads to type 2 diabetes
- we tend to have type 2 diabetes as soon as there is impaired glucose tolerance, slides a little misleading
Pre-Diabetes or Metabolic Syndrome
- a serious, treatable medical condition in which blood glucose levels are higher than normal but not yet high enough to be diagnosed as diabetes
- without intervention, nearly one-half of these individuals progress to clinical diabetes in around 5 years
Metabolic Syndrome
- Also known as "insulin resistance syndrome", Syndrome X
- Clustering of cardiovascular risk factors first noted in framingham heart study (visceral adiposity, insulin resistance, low HDL, systemic pro-inflammatory state)
- Substantially increasees the risk of: cardiovascular diseaes, cancer and type 2 diabetes
Adiposity and Insulin Resistance
- this slide answers why does increased adiposity result in insulin resistance
- in early type 2 diabetes, elevated insulin secretion: insulin inhibits lipolysis in adipose tissue and increased fat storage in adipose
- adipose tissue is an endocrine organ: secretes adipocytokines
- when fat cells are "stuffed", their secretion of adipocytokines changes (less adiponectin, more resistin, more TNF-alpha, more IL-6, more leptin)
.
- these changes promote insulin resistance
Prevention of Type 2 Diabetes
GOALS:
- reduce adiposity
- increase activity (walking 30 min/day and gym 3 days/week)
.
Results:
- one case of diabetes is prevented for every 7-8 participants in a lifestyle intervention program (3 years duration)
- achieving all diet and exercise goals stalls progression to diabetes
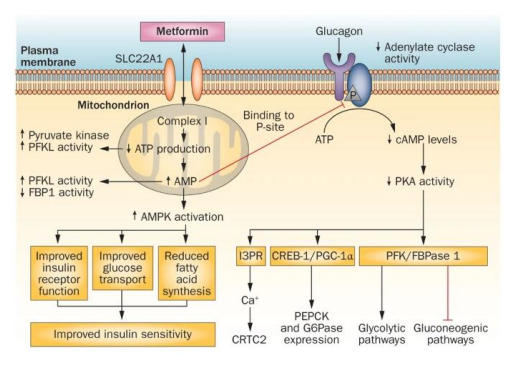
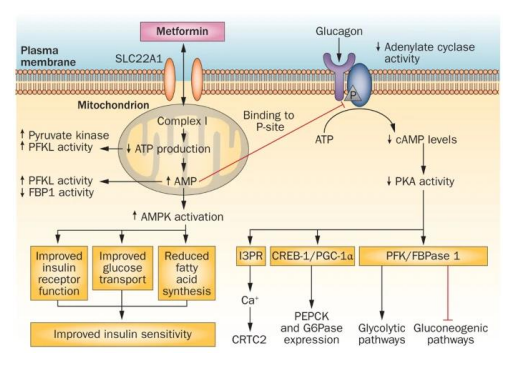
Treating insulin resistance
- the drug Metformin decreases liver glucose production by over 1/3
Disrupts glucagon signalling:
- inhibits gluconeogenic pathways
- stimulates glycolytic pathways
- reduces FA synthesis
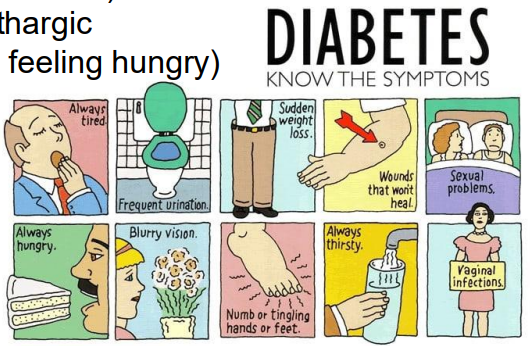
Symptoms of Diabetes
- in both types of diabetes, insulin signalling is disrupted
Normally, insulin:
- decreases high, post-prandial blood glucose concentrations
- promotes the transport of glucose into tissues for use and storage
.
Without insulin:
- blood glucose concentrations become elevated
- energy from blood glucose is not stored
Complication of Diabetes
- all cells are affected -> complications in all organs
.
MICROVASCULAR COMPLICATIONS:
- neuropathy (nerve damage)
- nephropathy (kidney disease)
- vision disorders (retinopathy, glaucoma, cataract, corneal disease)
.
MACROVASCULAR COMPLICATIONS:
- heart disease
- stroke
- peripheral vascular disease (can lead to ulcers, gangrene, amputation and diabetic foot ulcers)
Long term effects of elevated blood sugar
INCREASED RISK OF:
- cardiovascular disease
- renal failure
- damage to small blood vessels and nerves
Long term effects of elevated blood sugar - glycosylation
- Protein glycosylation (free amino groups)
- Haemoglobin can become glycosylated (abundant, many exposed amino groups, entry of glucose into erythrocytes isn't regulated (easily glycosylated)
- Glycosylation of haemoglobin (glycated haemoglobin)
- Compromises O2 delivery (effects especially experienced in extremities)
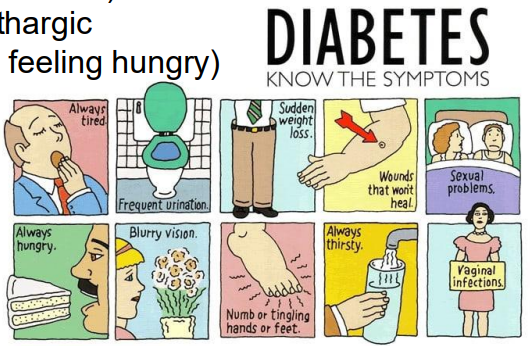
Symptoms of Diabetes ALL
- Polyuria (increased urine production)
- Polydipsia (increased thirst)
- Feeling tired and lethargic
- polyphagia (always feeling hungry)
- slow-healing cuts
- skin infections
- blurred vision
- mood swings
- headaches
- feeling dizzy
- leg cramps
- unexplained weight loss (type 1)
- gradual increase in body fat (type 2)
Complications of Diabetes
OTHER COMPLICATIONS:
- infections, including oral infections
- metabolic difficulties
- impotence
- autonomic neuropathy
- pregnancy problems
Measuring blood glucose is important for diagnosis
RANDOM GLUCOSE TEST:
- Non-fasting
- assumes recent meal
.
FASTING GLUCOSE TEST:
- no food or drink (other than water) for 8 hours before test
Testing for glycaemic control
HbA1c:
- measures glycosylation of haemoglobin in red blood cells
- indicates average glycaemic control over 6-8 weeks
- measure every 3 months
- complement to self blood glucose monitoring (BGM - at a particular time, glycaemic pattern over 24h cycle)
- Venous blood
- Higher HbA1c correlates with risk of microvascular complications
.
HbA1c, or glycated hemoglobin, is a blood test that measures your average blood sugar (glucose) levels over the past two to three months. It works by measuring the percentage of hemoglobin in your red blood cells that has glucose attached to it, and it's used to diagnose and monitor diabetes. A higher HbA1c level indicates higher average blood sugar, while a lower level indicates better control.
Diabetes results in abnormal blood glucose levels
NORMAL FASTING BLOOD GLUCOSE is 3.5-5.5mmol/L
DIABETES INDICATED WHEN:
- fasting blood glucose >7mmol/L
- random blood glucose >11.1mmol/L (verify with a repeat trest, also glucose tolerance test)
.
ORAL GLUCOSE TOLERANCE TEST required if:
- fasting blood glucose is between 5.5 and 6.9
- random blood glucose is between 5.5 and 11.0
Oral Glucose Tolerance Test (OGTT)
- "gold standard" test
- 3 days preceding - 150g carbohydrate/day (10x40 slices of bread)
- fast overnight (from around 22:00)
- no smoking, no caffeine
.
- patient to remain seated and still for duration
- orally consume glucose "load" - 75g
- blood taken before and 2h after glucose meal
Diabetes results in abnormal responses of blood glucose level (OGTT)
NORMAL VALUES:
- fasting blood glucose <6.1 mmol/L
- 2h blood glucose <7.8mmol/L
.
IMPAIRED FASTING GLUCOSE:
- fasting blood glucose between 6.1 and 6.9 mmol/L
- 2h blood glucose <7.8mmol/L
.
IMPAIRED GLUCOSE TOLERANCE:
- Fasting blood glucose <7.0
- 2h blood glucose betwen 7.8 and 11.0
.
DIABETES:
- fasting blood glucose >7.0
- 2h blood glucose >11.1
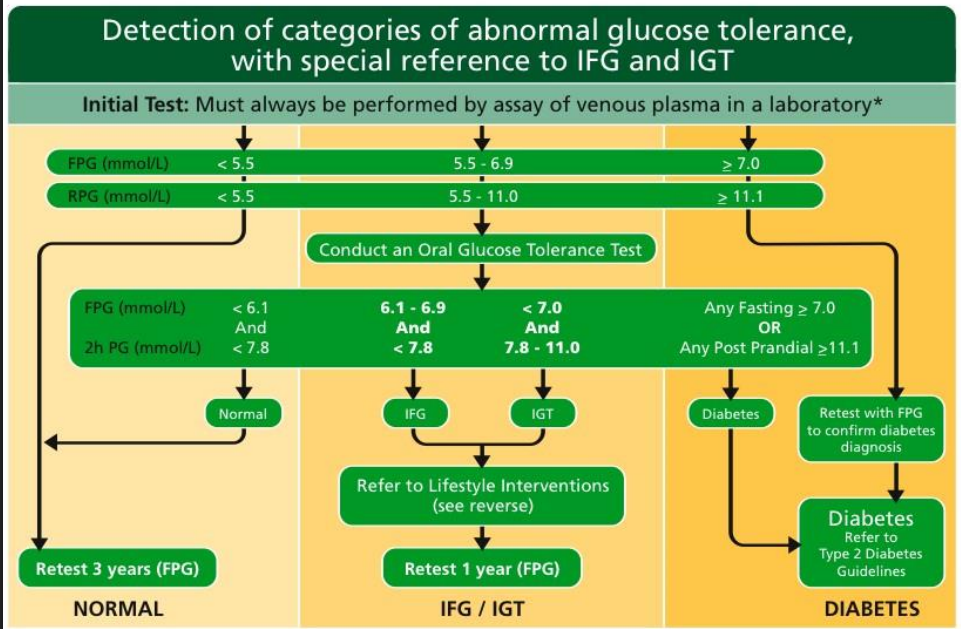
SUMMARY SO FAR
DIAGRAM ON SLIDE 41
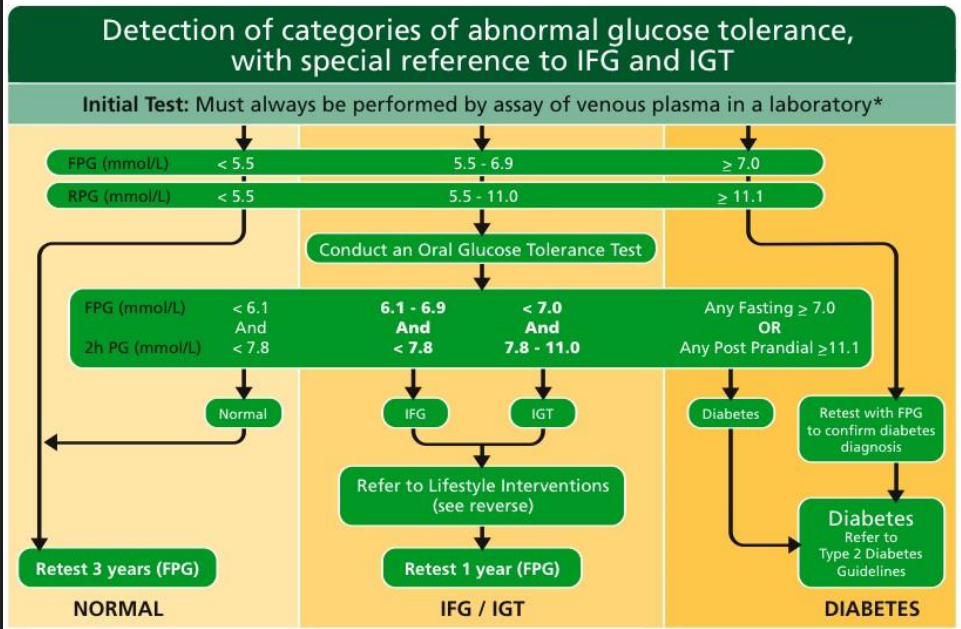
In summary
- IFG means impaired fasting glucose
- IGT means impaired glucose tolerance