"Study Guide" muscle system
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
78 Terms
What makes up muscle tissue (ie organ)?
-nerves
-blood vessels
-various connective tissue
what does every muscle have attached to it?
motor neuron
what does every muscle have to have the capability of
-ability to contract
-ability to conduct action potential
Muscle functions (Production of...)
-movement of body parts and environment
-movement of blood thru vessels and heart and lymphatic vessels and food thru GI tract, etc
-movement of bile out of gallbladder, child thru birth canal, urine from urinary system, etc
Muscle functions (maintenance of...)
Posture. Muscle contraction is constantly allowing us to sit upright
Muscle functions (generation of...)
Thermogenesis (heat). Moderates body temp via shivering
Muscle functions (stabilization at...)
tendons (connect bone to muscle)
3 types of muscle tissue
-skeletal
-cardiac
-smooth
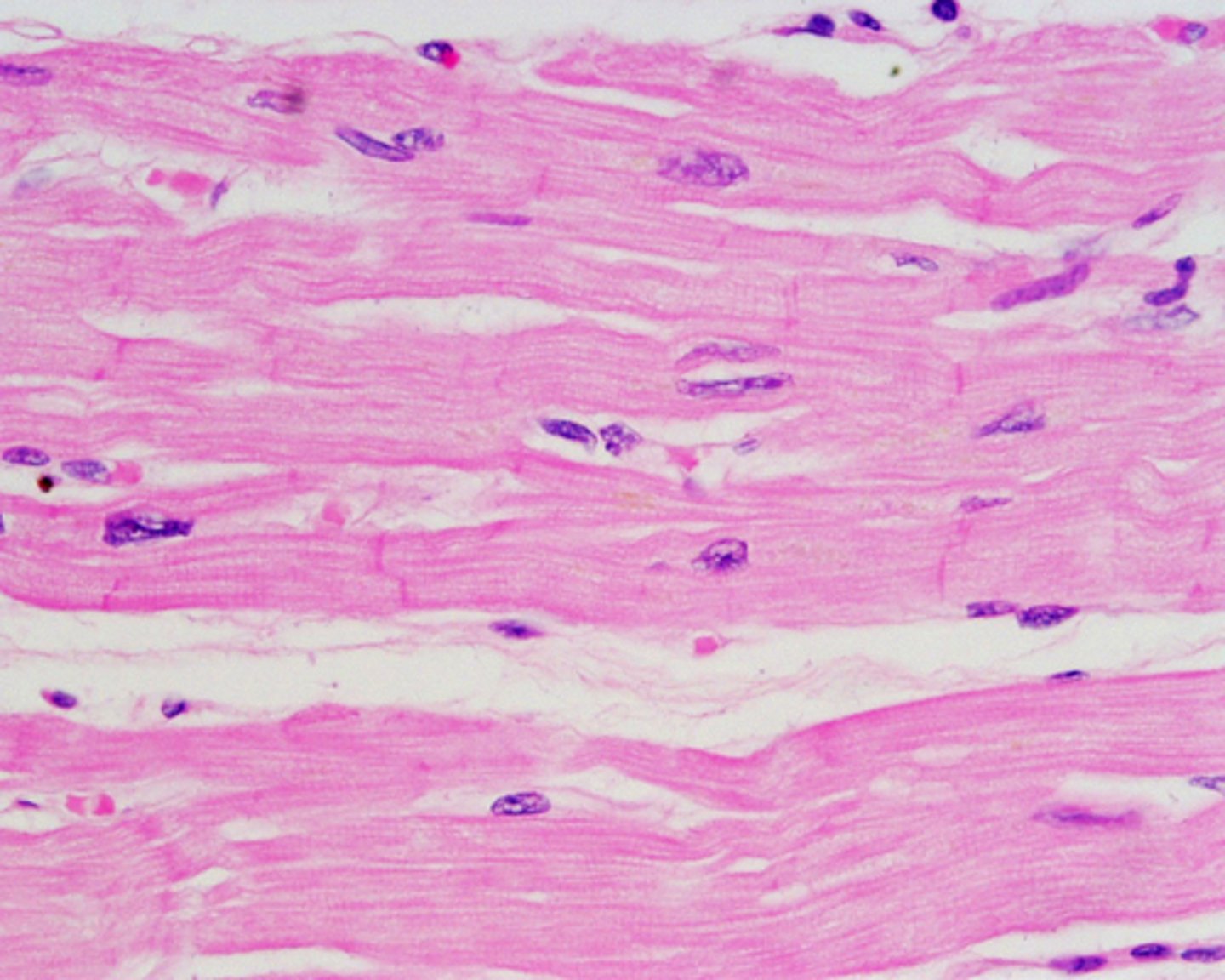
Skeletal Muscle
-striated
-multiple nuclei
-long striated fibers in bundles
-voluntary
-grow quickly, slow to regenerate

cardiac muscle
-striated
-one nuclei
-short and thick cells with branches
-involuntary
-don't regenerate
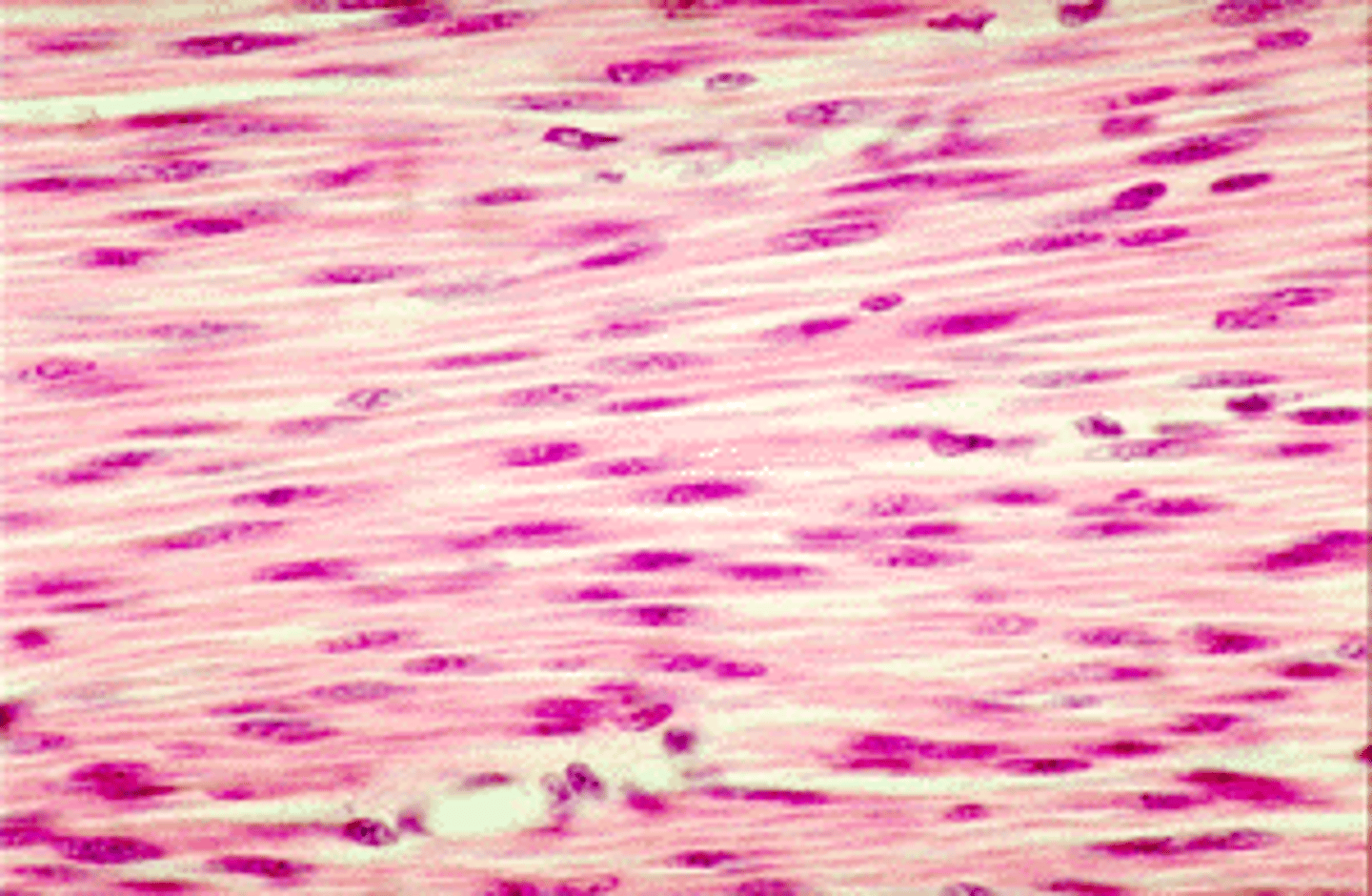
Smooth Muscle
-nonstriated
-one nuclei, centrally located
-spindle shaped, thick in middle
-involuntary
-regenerates the best
excitability
ability to receive stimulus (neurotransmitters and hormones) and identify potential stimuli. the responce is the generation of an electrical impulse
contractility
ability to get shorter (defining ability of muscle)
Extensability
ability to stretch
elasticity
ability to recoil and resume original length arfter being stretched
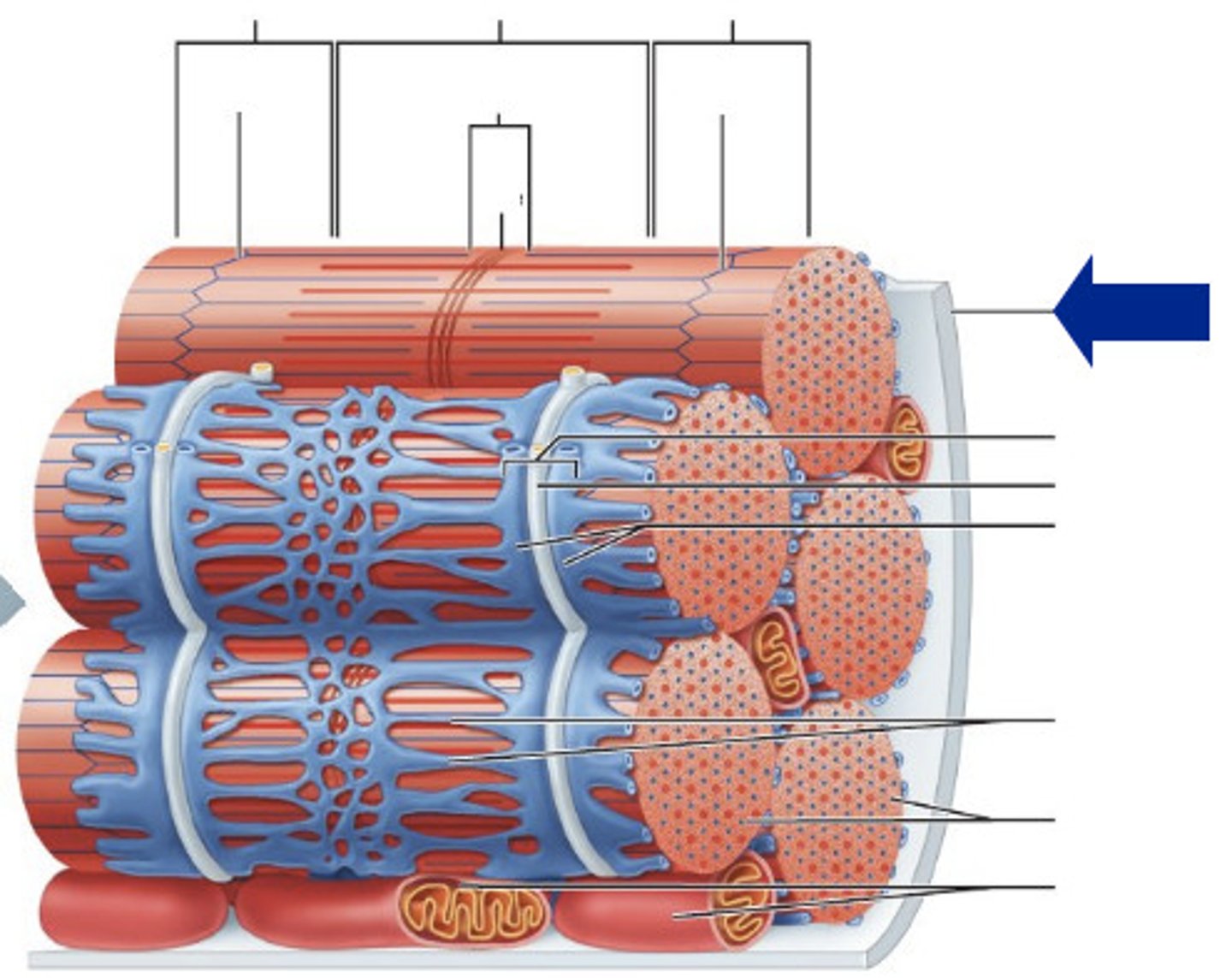
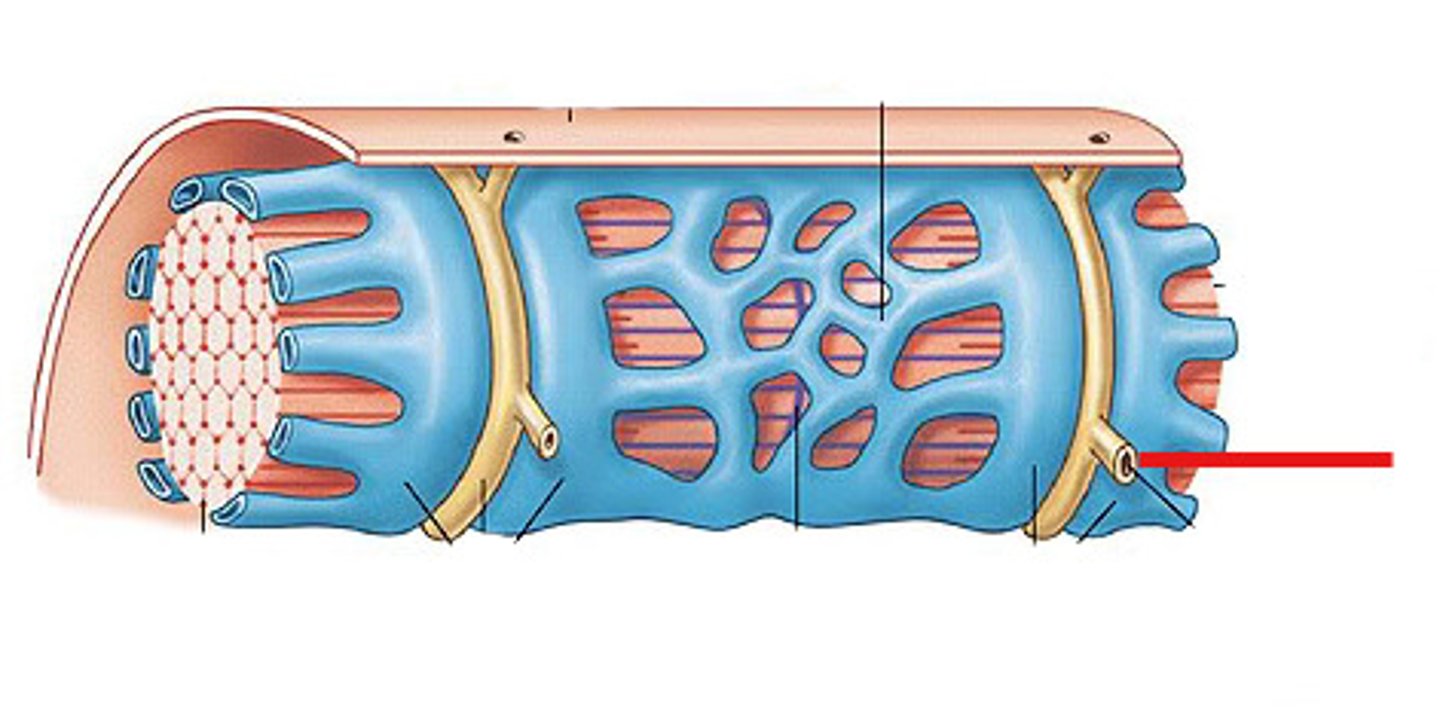
connective tissue membrane of muscle
Epimysium
perimysium
endomysium
levels of muscle (alphabetical)
fassicles
fibers
fibrils
filaments
artery
carries o2 in blood, carries blood away from heart
vein
carries blood to heart, and holds "waste" blood
neuron
motor neuron tells muscle to moves
how do the arteries, veins, and neurons enter the muscle
connective converings and branch extensively
epimysium
whole muscle and perimysium is held together by this ct
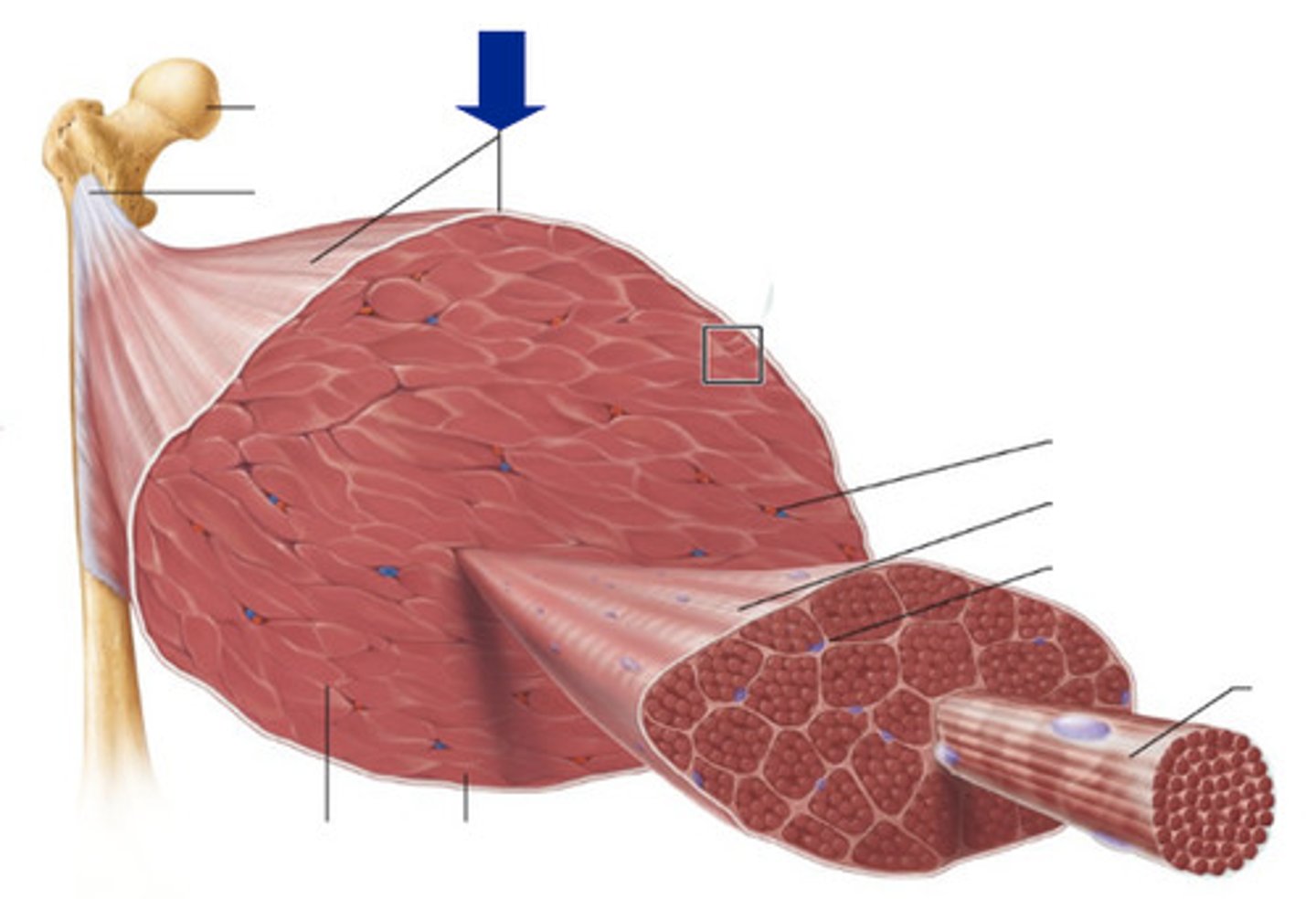
perimysium
holds fassicles, inside epimysium
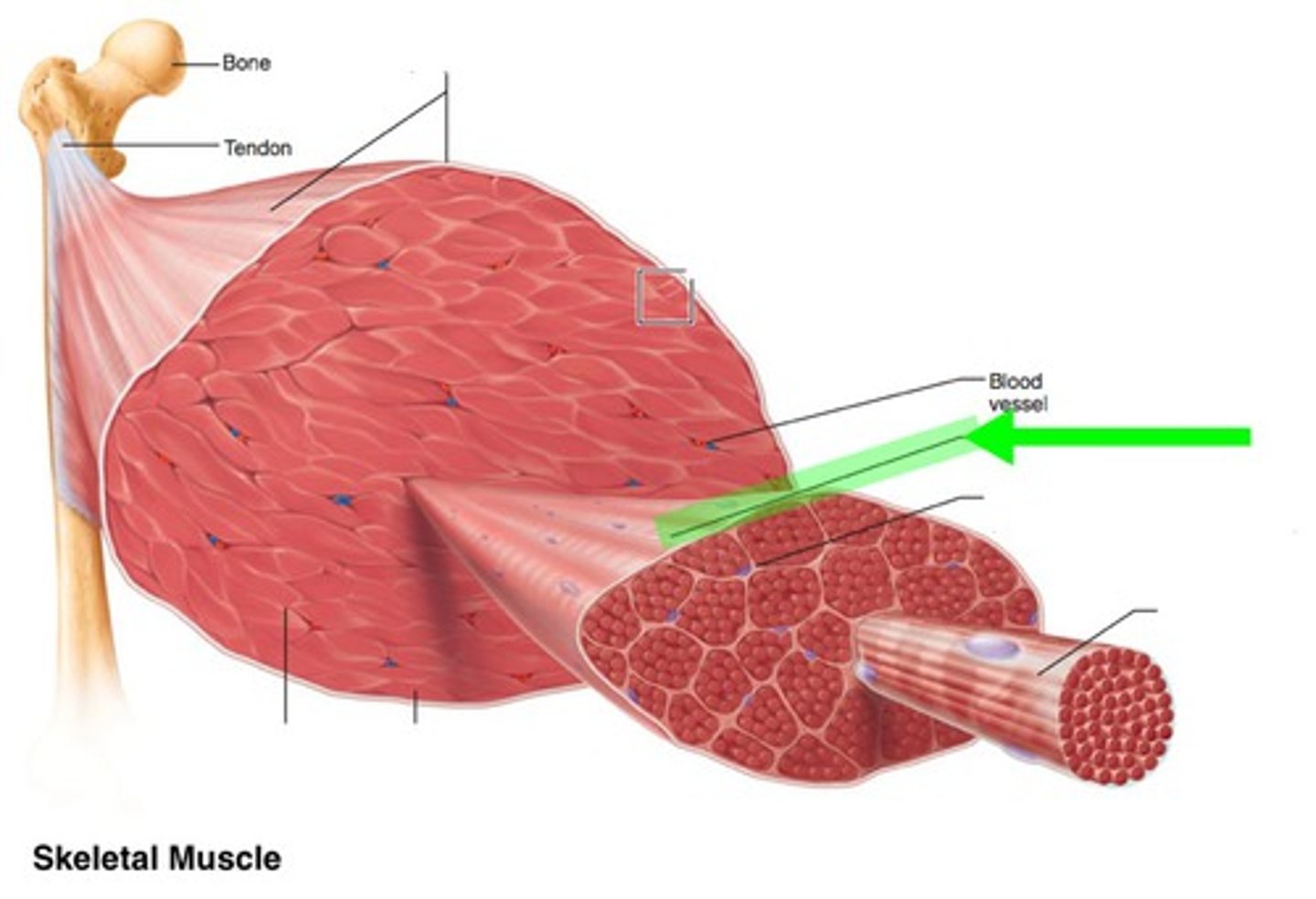
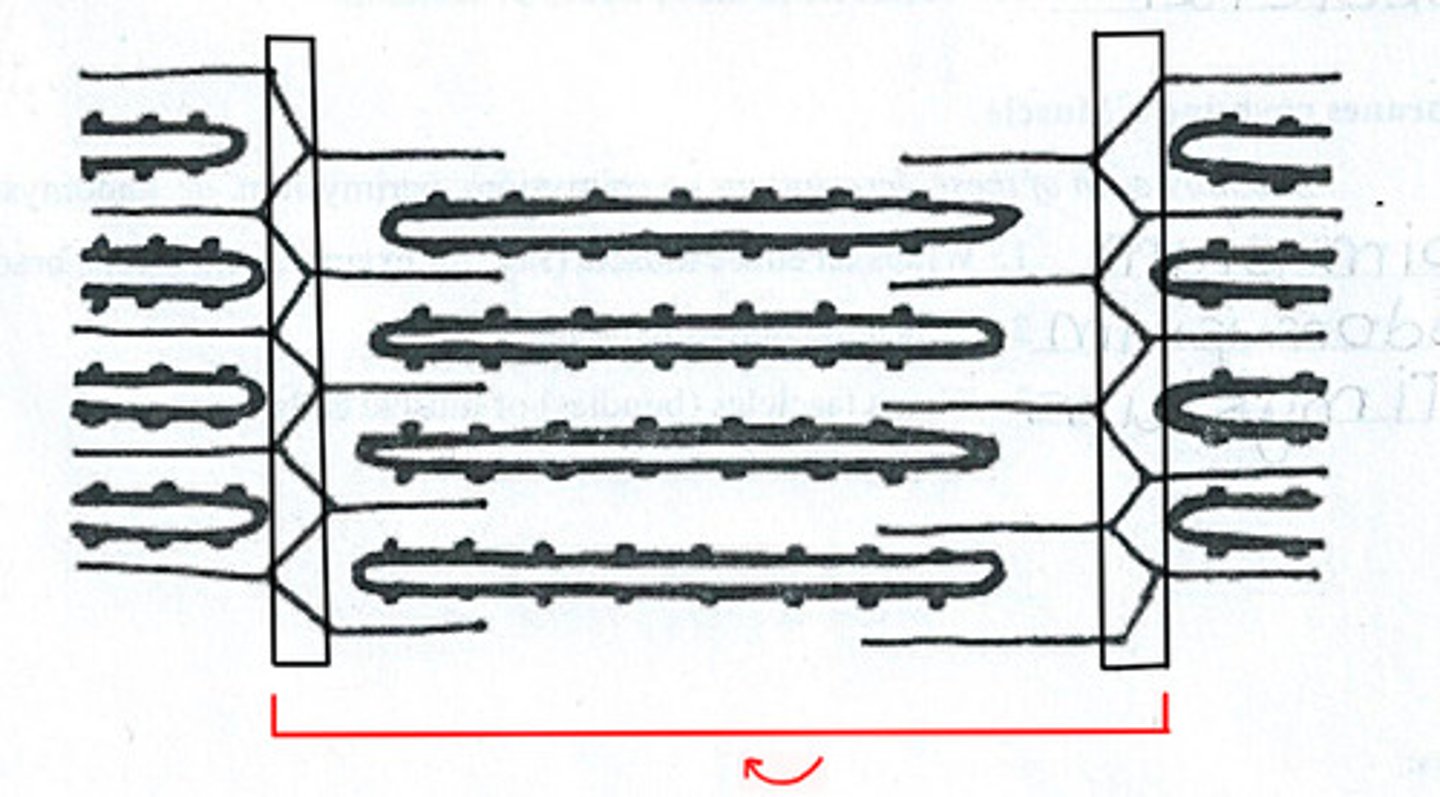
fassicles
bundles of cells inside perimysium. holds endomysium and fibers
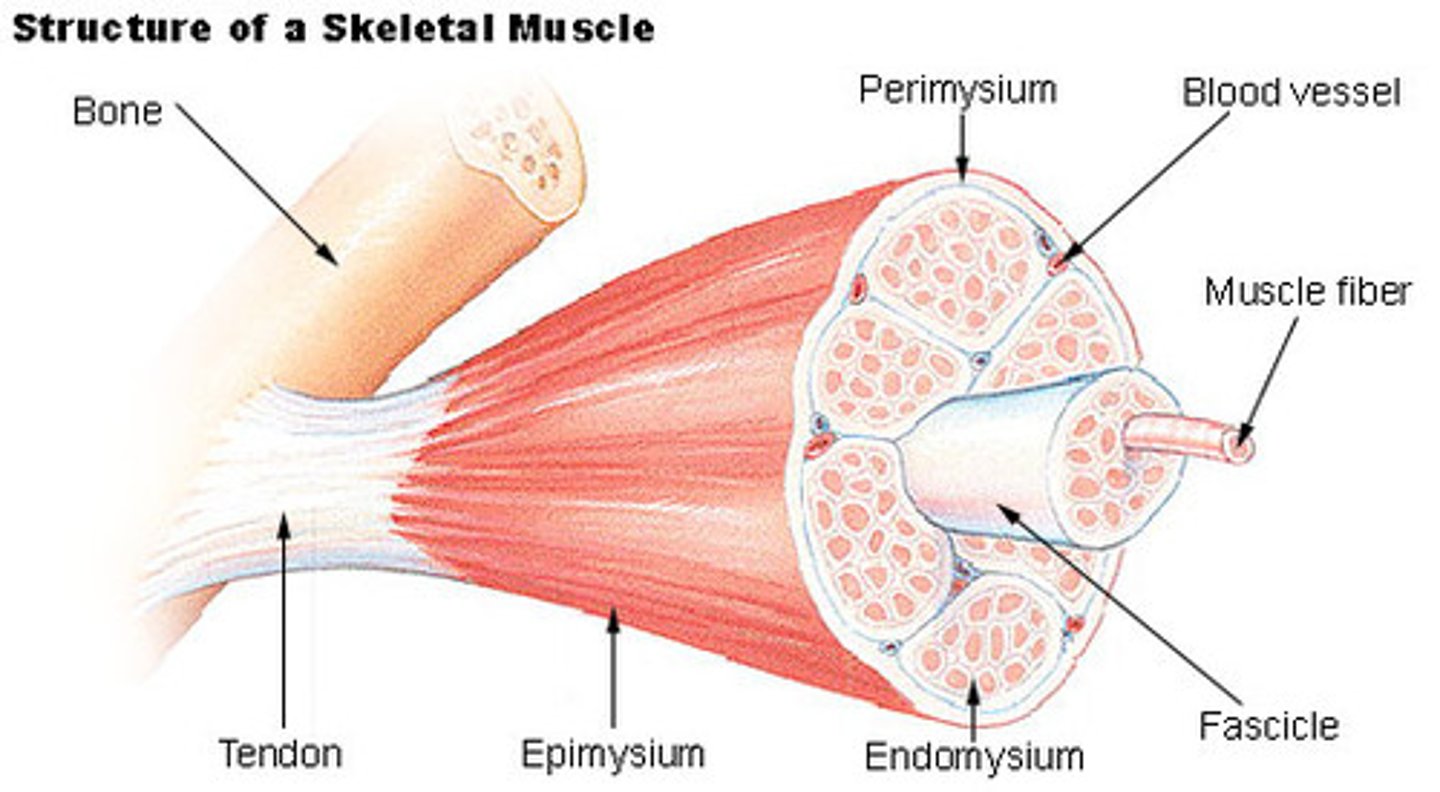
endomysium
inside fassicles, holds muscle fibers
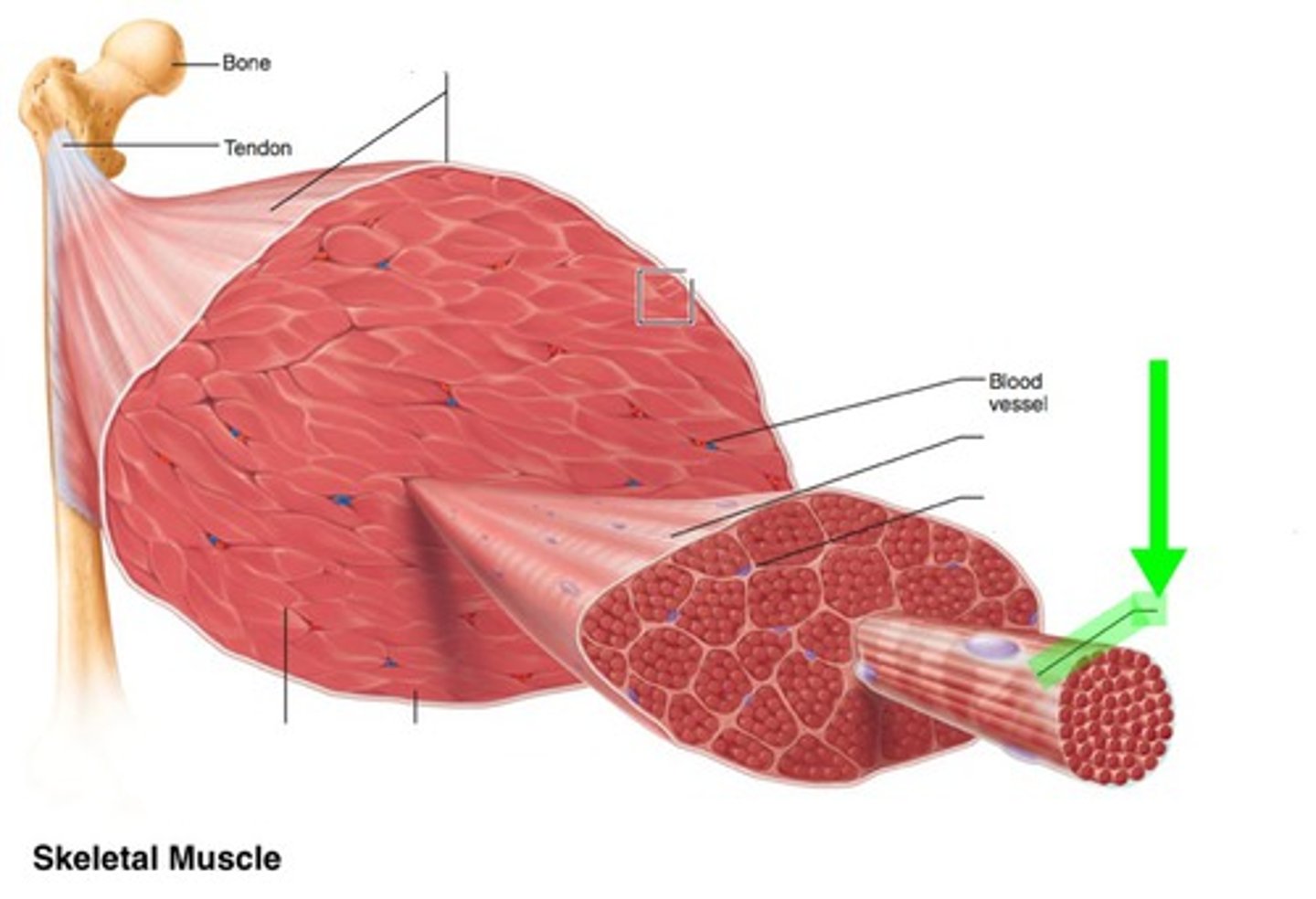
muscle fibers
muscle cell
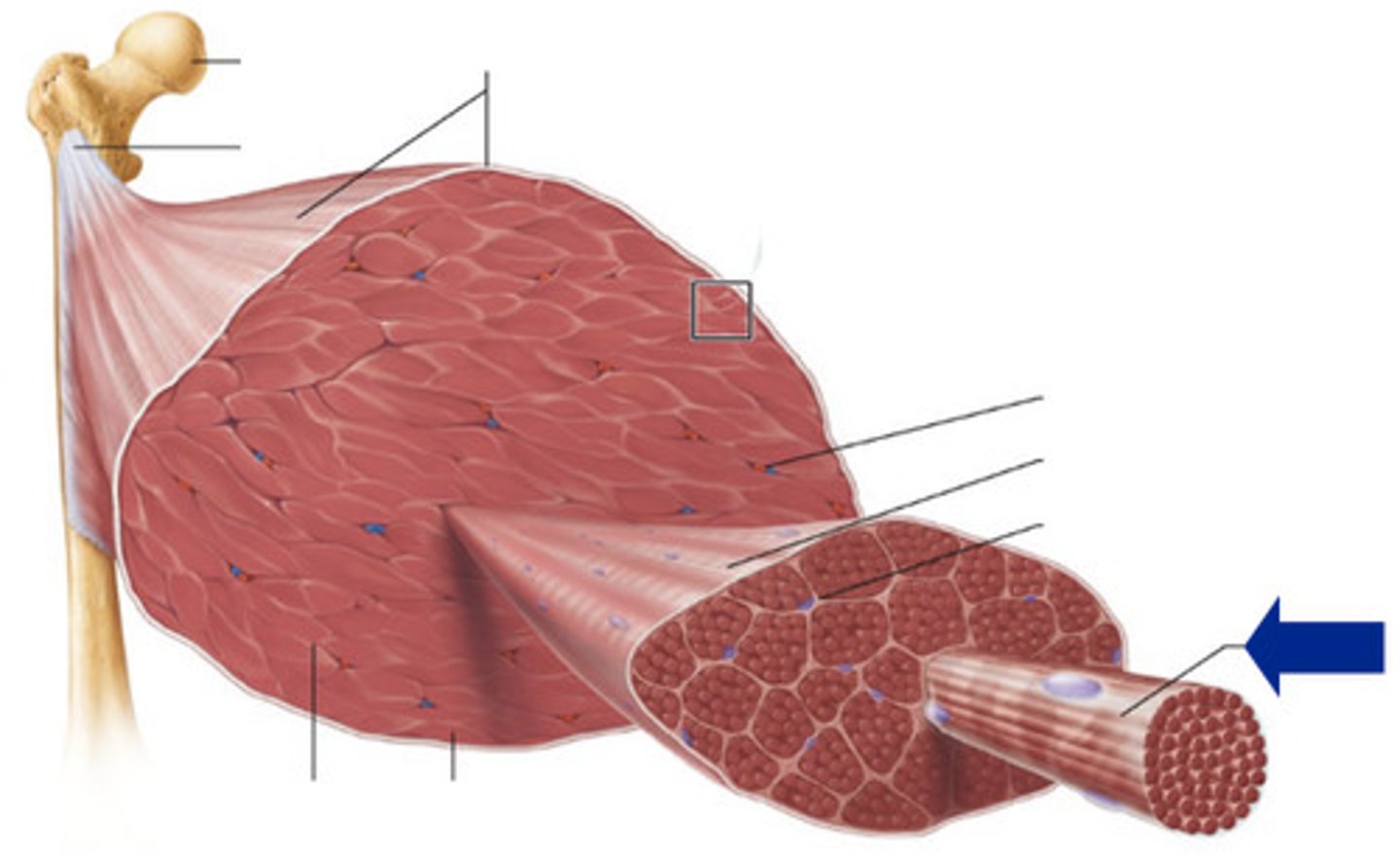
myofibrils
make up muscle cells

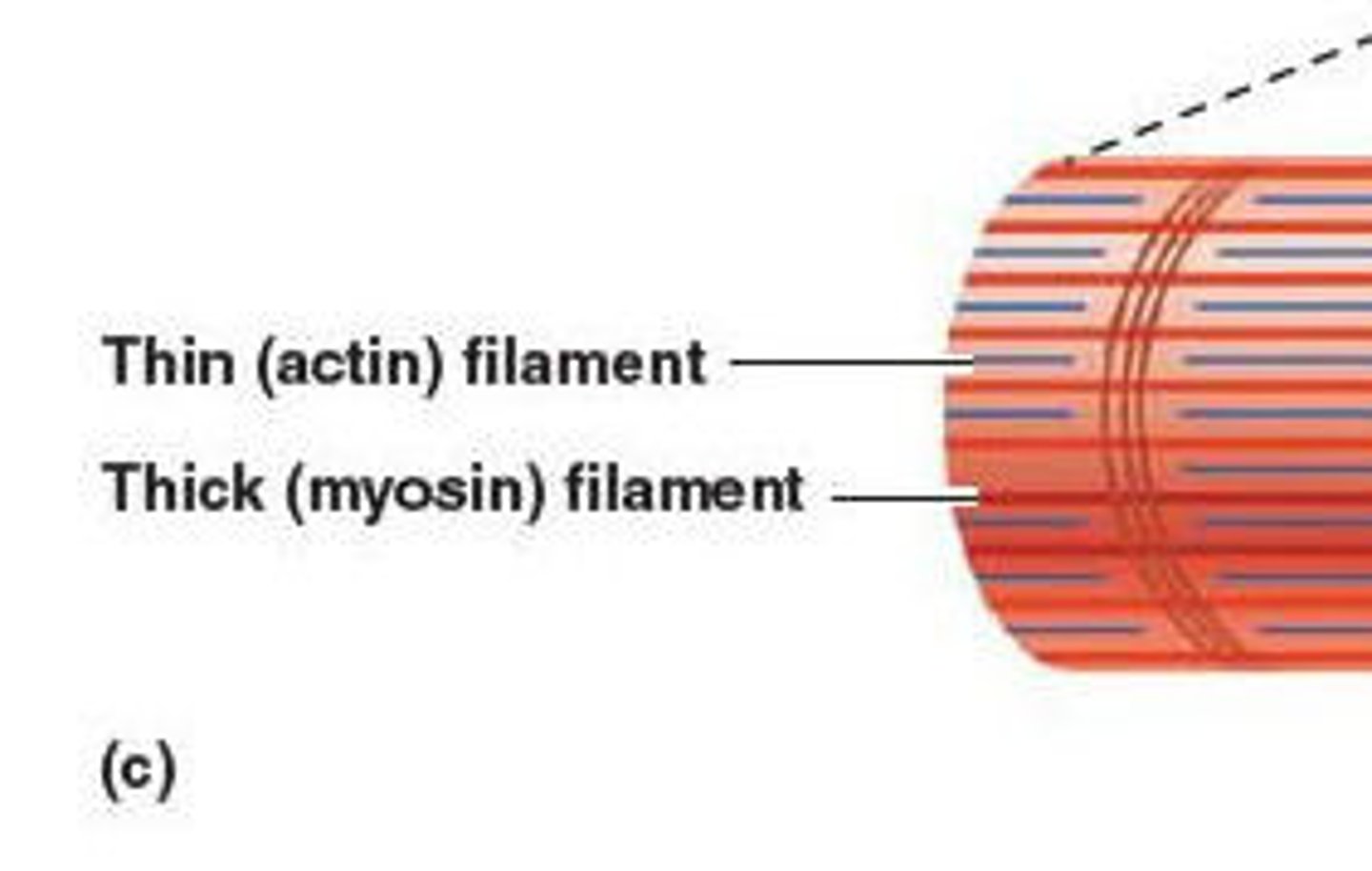
filaments
make up fibryls, thin and thick. Cause contraction
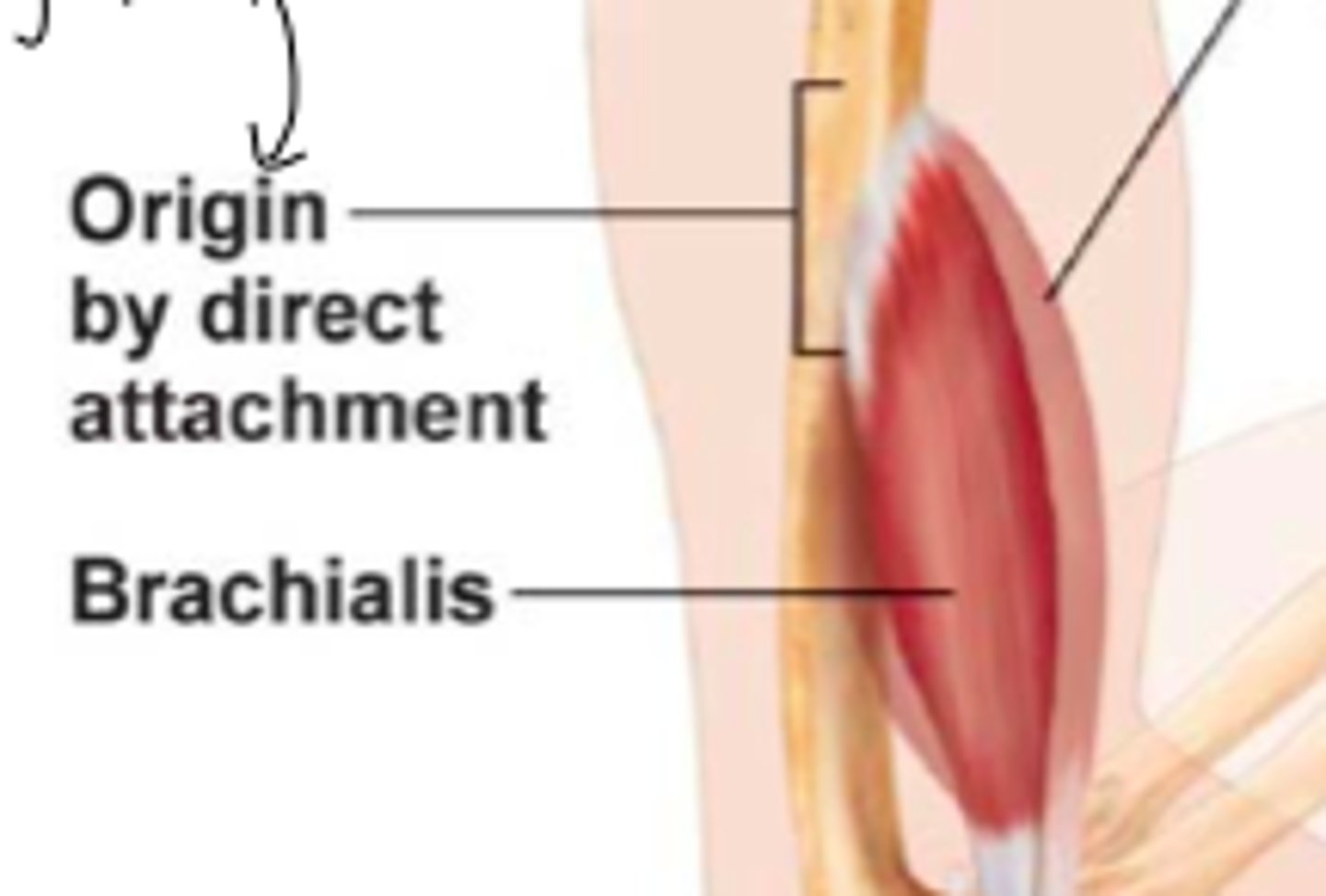
Skeletal muscle attachment
most span joints and are attached to bones
Origin of muscle
attachment of muscle to immovable bone
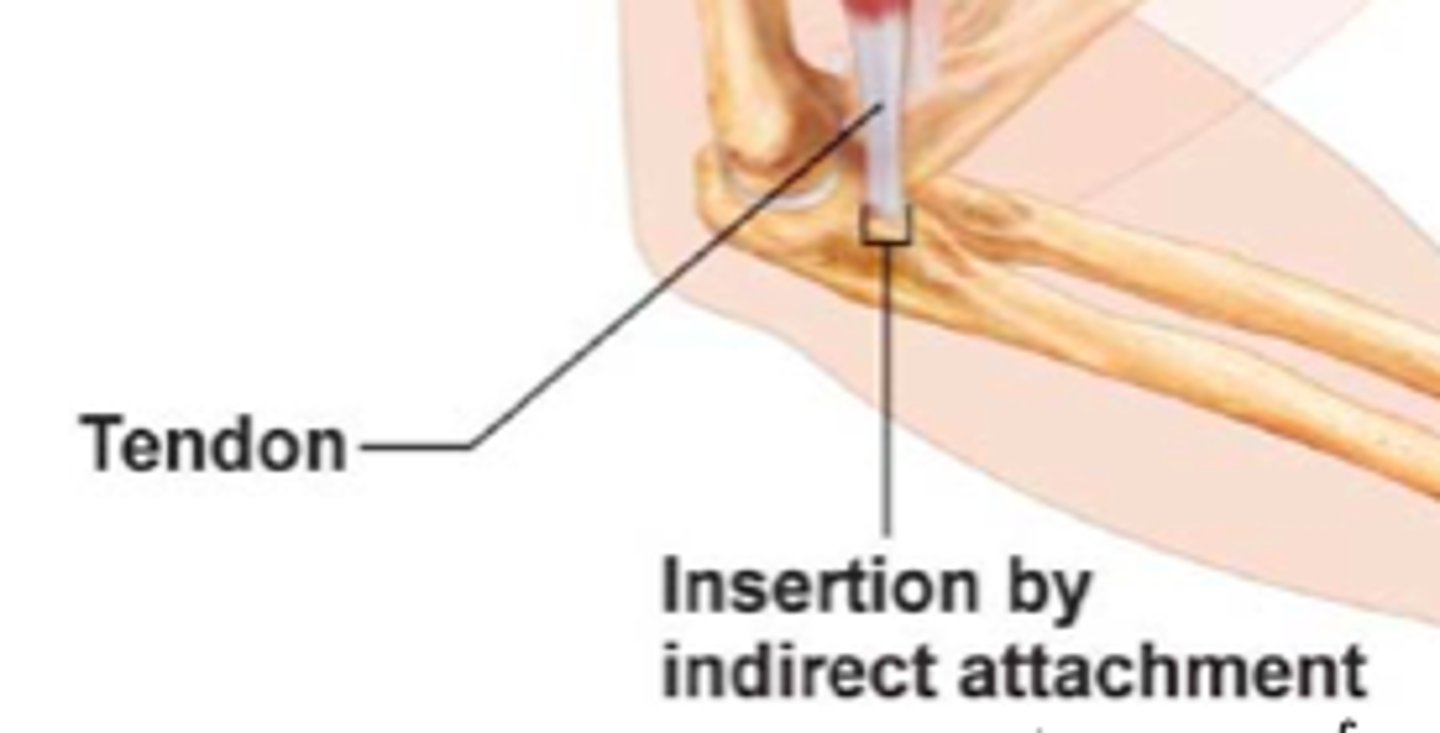
insertion
attachment of muscle to movable bone
direct muscle attachment
less common, epimysium is fused to a peristeum o pericerondrium
indirect attachment
typical, ct extends and forms tendon or aponeurosis, which attaches to peristeum or perichondrium
why are muscle cells known as muscle fiber?
they are very long (30cm)
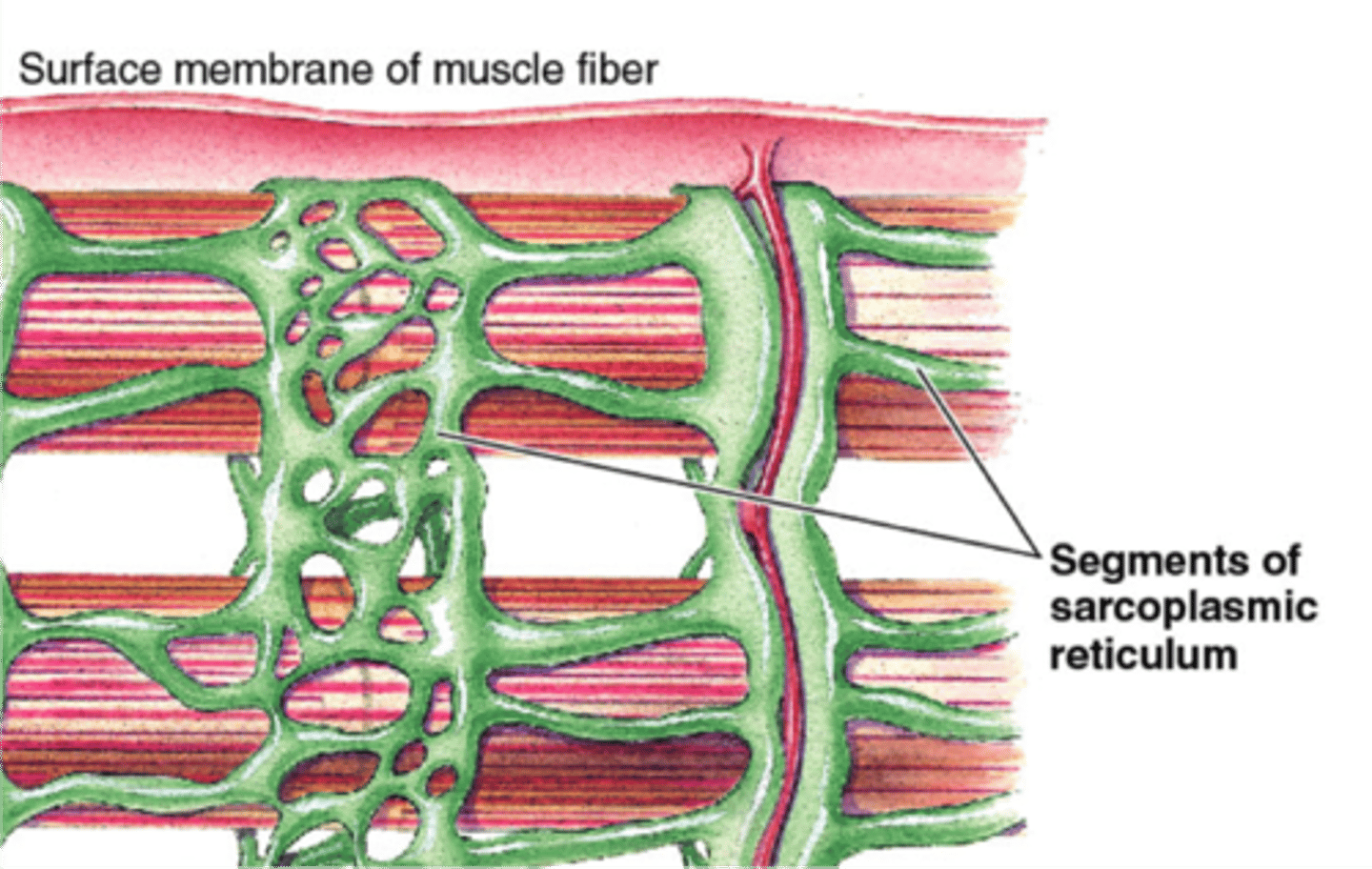
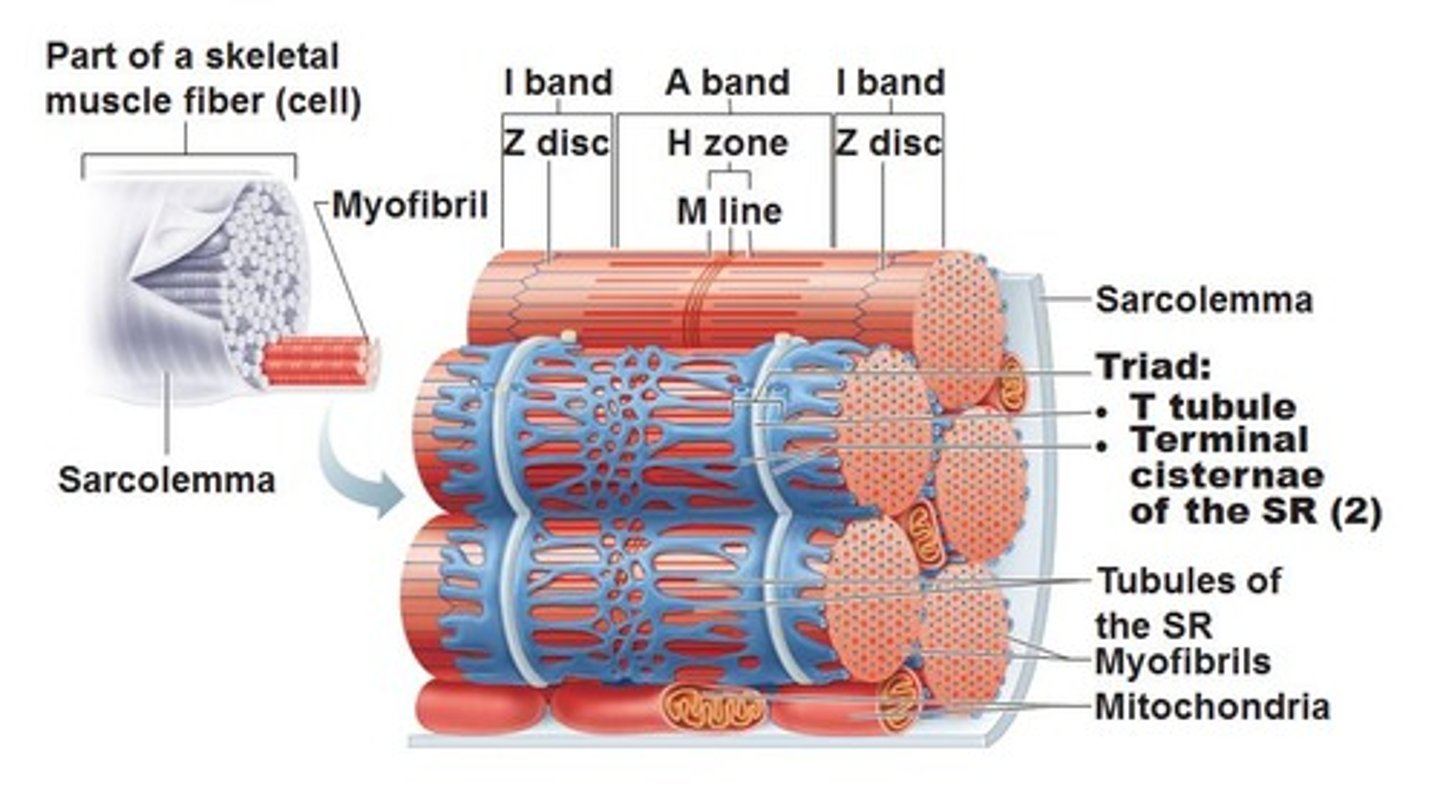
sarcolemma
muscl fiber's memebrane
sarcoplasm
muscle fiber cytoplasm

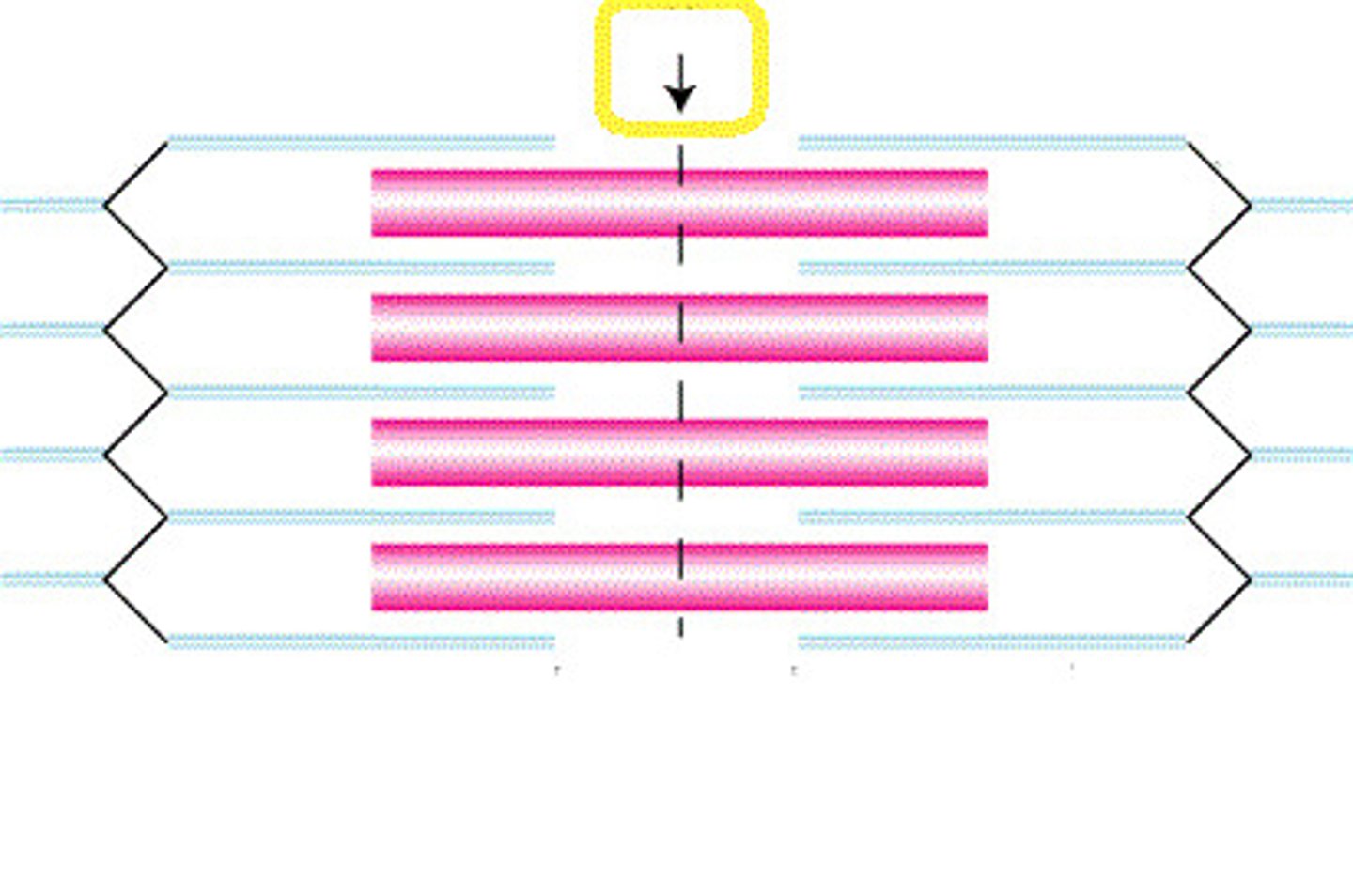
transverse tubules
sarcolemma's tubes that penitrate through cell. encircles myofibril at each A-I junstion
sarcoplasmic reticulum
stores Ca2+, surrounds the tubules and myofibrils
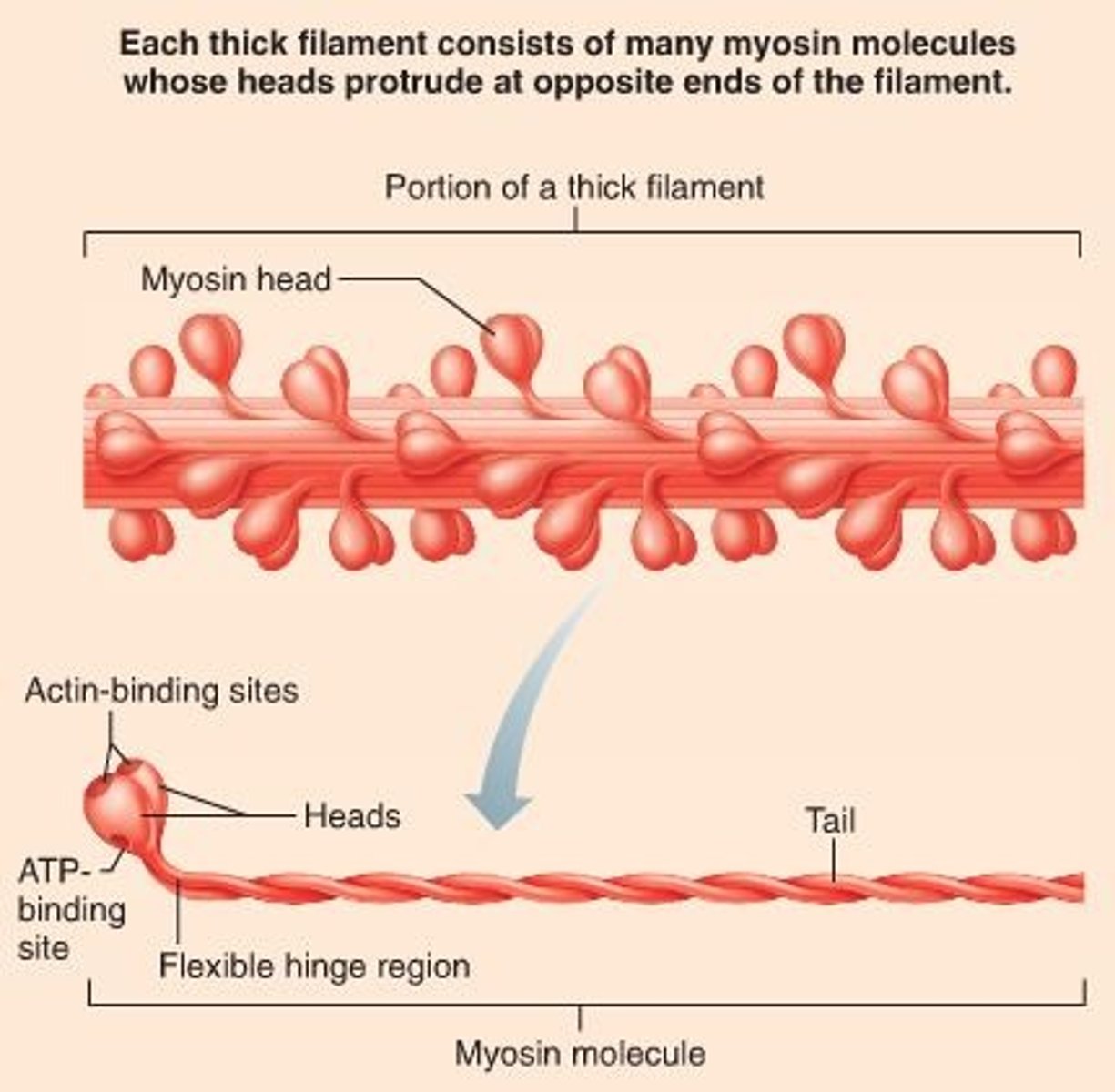
Thick filaments
myosin, with tail and head.
thin filaments
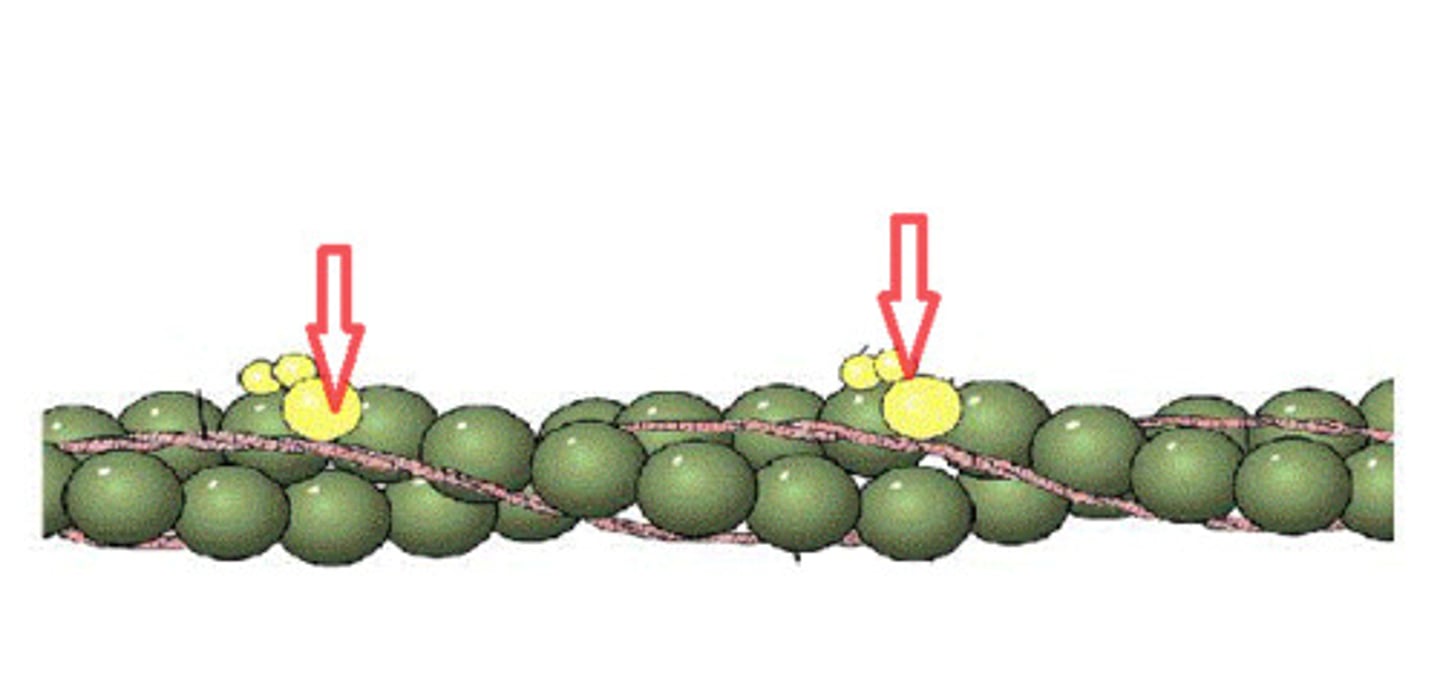
actin, tropomyosin, and troponin
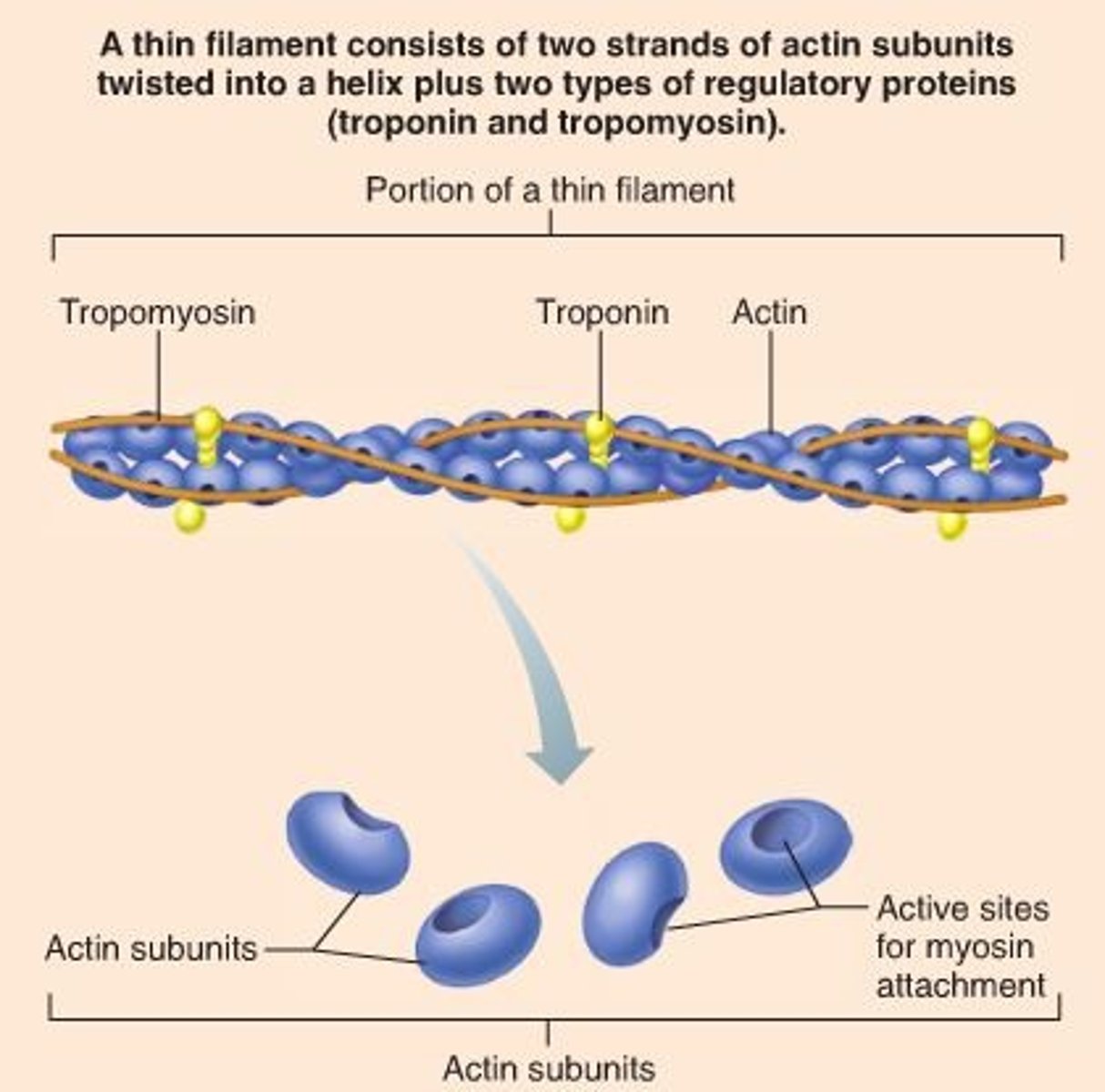
actin
myosin binding site
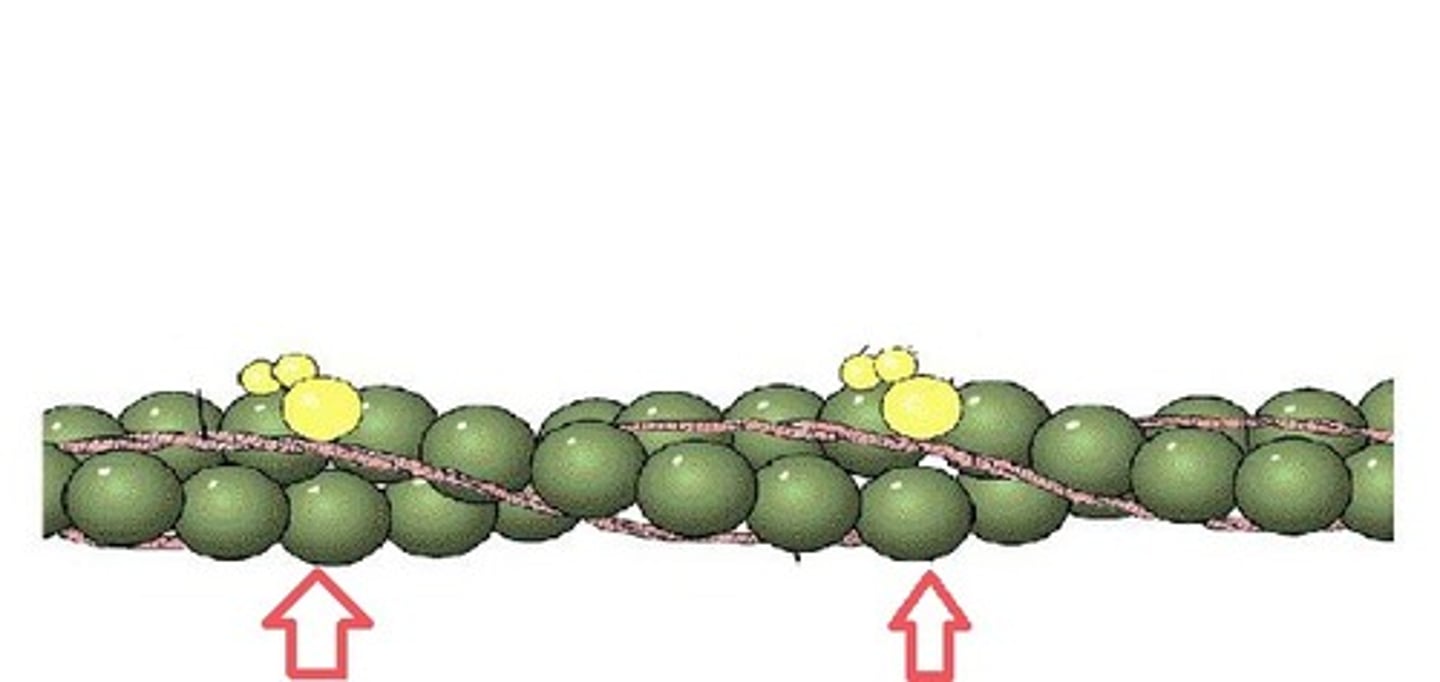
tropomyosin
blocks myosin binding site

troponin
moves tropomyosin so there will be a binding.
sacromeres
functional unit of contraction between 7 disks
a band
Length of thick filaments, dark under microscope. Stands for anisotropic
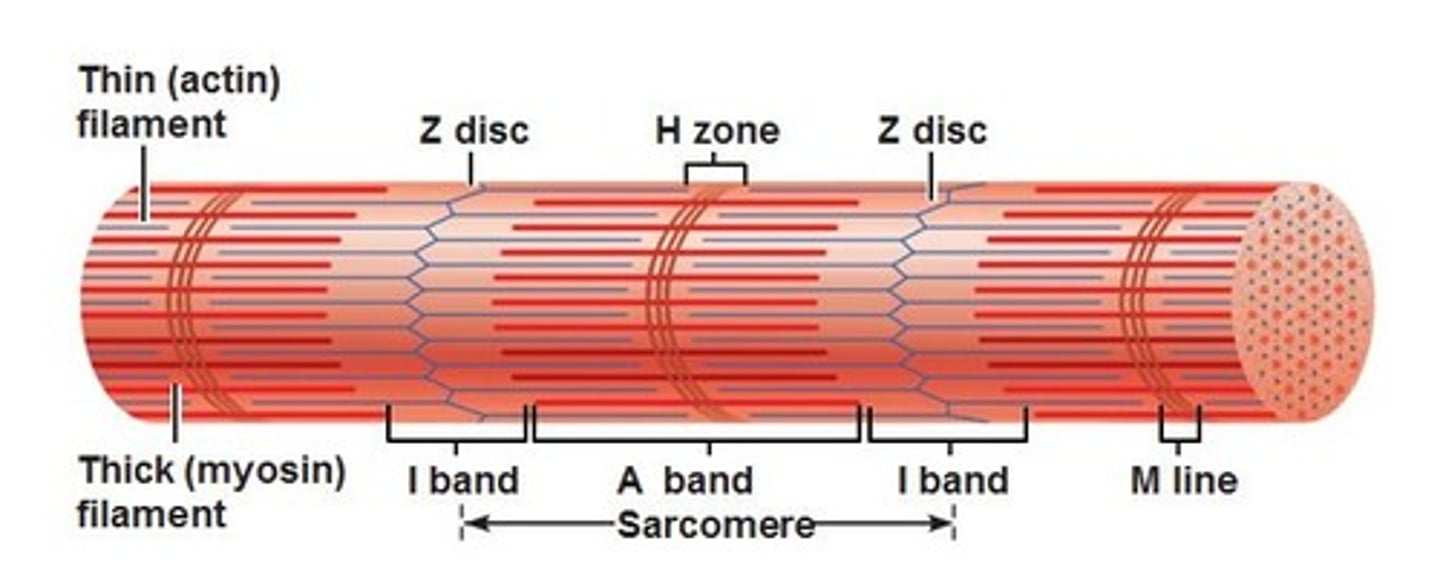
h zone
Area of only thick filaments between the thin

M line
center of thick filaments
I band
stands for iliotibial, appears light under micro, apart of two sacromeres. only thin filaments and z disc
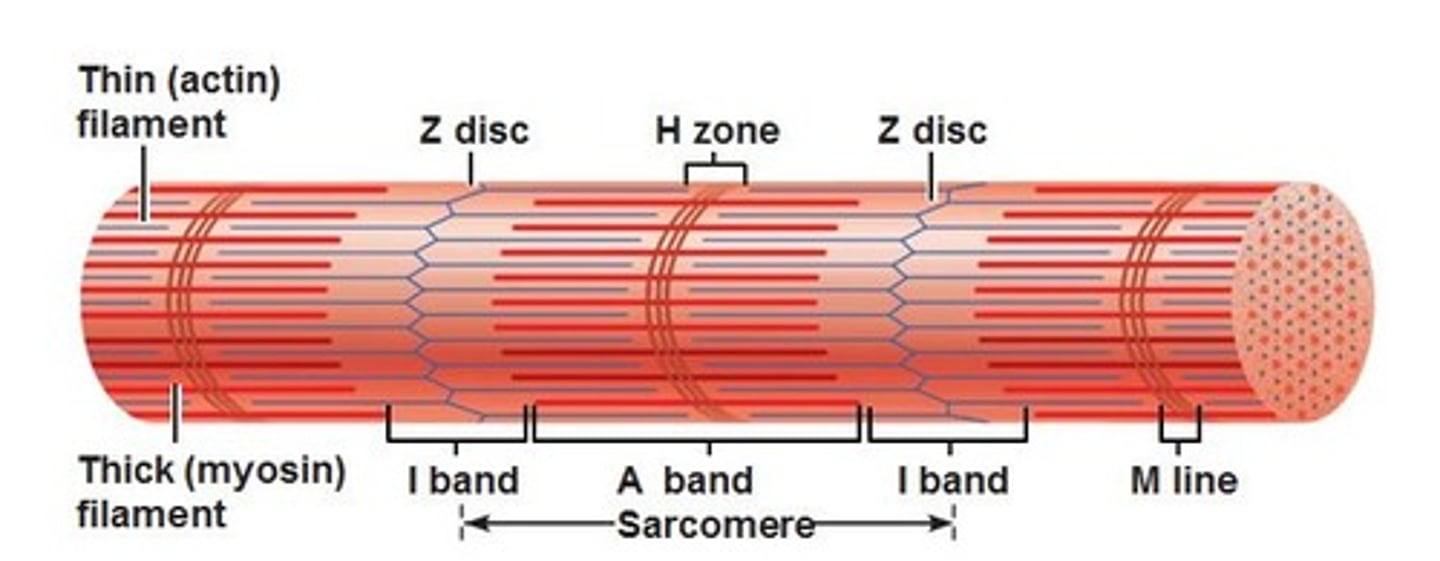
Z disc
center of thin filaments
terminal cisternae
enlarged ends of sarcolpastmic reticulum, surrounds t tubules more directly
triad
t tubules and 2 term cisterna
muscle contraction
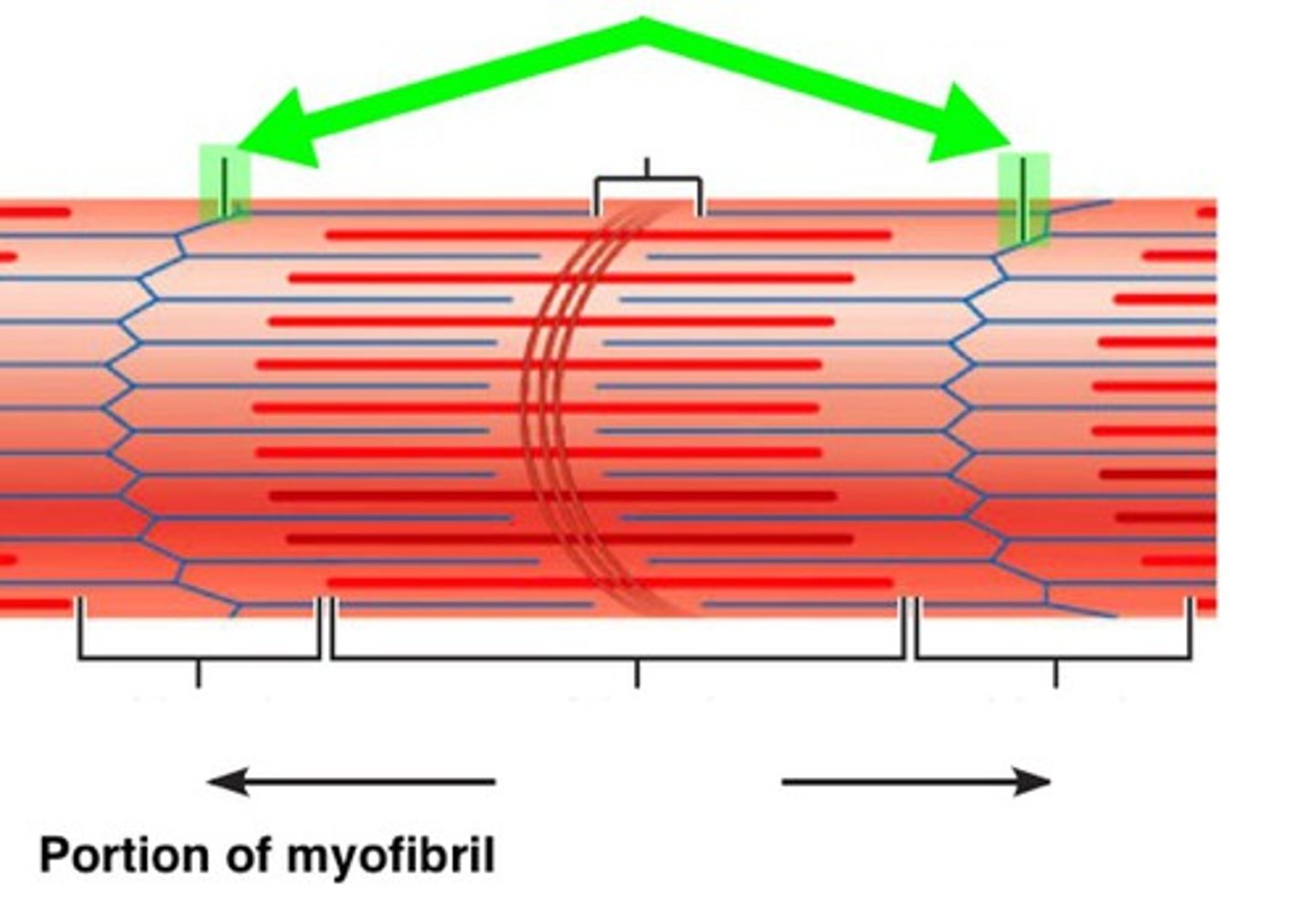
thin and thick filaments slide over each other, pulling z discs closer, shortening fiber and pulls on attached tendon (pulls on endomysium, perimysium, and epimysium
distance between z discs
shortens
length of A band
stays same
Lenght of H zone
shortens
Length of I band
shortens
muscle contractions are instigated by
nerve impulses
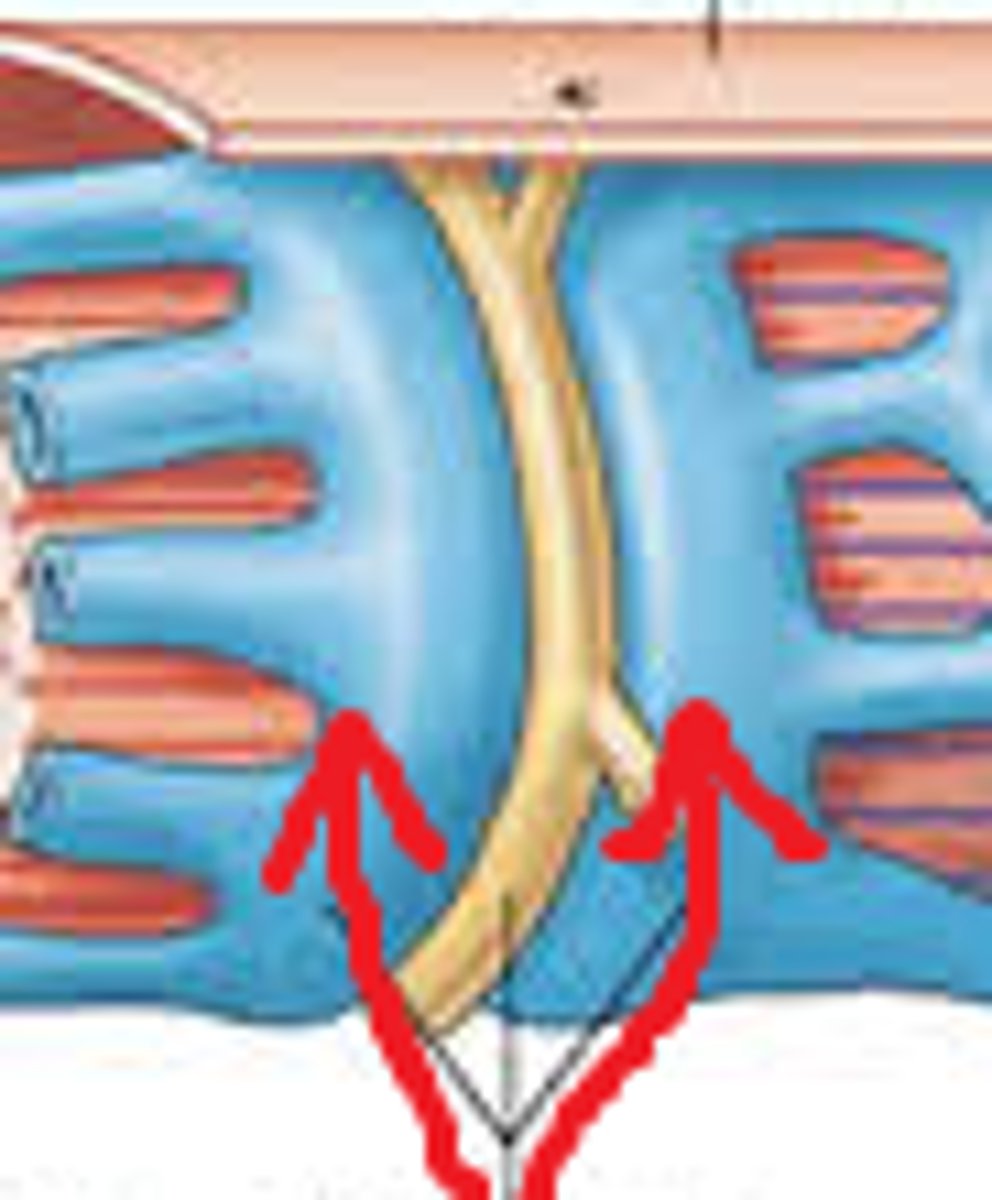
motor neurons and muscles meet at the
neuromuscular junction (NMJ)
where does the message btwn neuron and muscle
synapse
At the axon terminal (the end of the motor neuron) there are
vesicles filled with a neurotransmitter, Acetylcholine (ACh).
the cell membrane and releases the ACh by
exocytosis
Active transport, in the form of the Na+/K+ pump, is used by the
myofibers (muscle cells) to maintain a higher concentration of Na+ outside the cell membrane.
On the sarcolemma (muscle cell membrane) there are ACh receptors that will open up a channel when
ACh attaches, allowing the Na+ to flood into the cell through facilitated diffusion.
Inside the myofibers are
sarcoplasmic reticula that store Ca2+ ions by active transport
The change in Na+ concentration due to the ACh causes the SR to release
Ca2+ in the same flood-like fashion
the contraction of the sarcomere involves the binding
of the proteins Actin (thin filament) and Myosin (thick filament)
Contraction btwn actin and myosin is prevented by the
protein molecules Troponin and Tropomyosin, which wrap around the Actin molecules, covering the Myosin-binding site on the Actin molecule.
The Ca2+ ions bind to the
troponin molecules, thus causing them to change shape, and in turn cause the Tropomyosin to change shape, thus exposing the Myosin-binding sites.
Heads on the Myosin molecule, then bind with the Actin. This is called
a cross bridge and causes the rigidity of the muscles. The binding also changes the shape of the molecules thus moving the thin filament closer to the center of the sarcomere.
Rigor mortis
the release of Ca2+ ions from the SR once the active transport stops due to lack of ATP, always flexing
When ATP is present it is needed to break
the bond between the Actin and the Myosin filaments. The Myosin heads contain the enzyme ATPase, which breaks ATP down into ADP and a phosphate, and releases energy.
break btwn myosin and actin forms
a power-stroke that moves the thin filament closer to the center and allows the Myosin-binding site to bind to the next Myosin head.
Relaxation is
ach removal from the synapse.
Acetylcholinesterase (AChE)
breaks down the ACh, thus closing the ACh receptors and allowing the high concentration of Na+ ions to be reestablished by active transport and remain on the outside of the sarcolemma.
Active transport pumps in the
SR then work toward keeping the concentration of Ca2+ ions 10,000 times higher in the SR than in the sarcoplasm
This uptake of Ca2+ ions is facilitated by the binding of Ca2+ ions to a protein called
calsequestrin in the SR.
The lack of Ca2+ ions in the sarcomere causes
the Troponin and Tropomyosin to block the Myosin-binding sites on the Actin, thus preventing the cross bridges from forming
relaxation alone will not
return a muscle to its previous length, but that it requires the contraction of an antagonistic muscle