**4. Events at Different Segments of Nephron
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
13 Terms
How do kidneys maintain water balance during drastic changes in water intake? (when dehydrated or overhydrated)
If dehydrated = Produce urine that is more concentrated than plasma (hypertonic)
If overhydrated = Produces urine that is diluted than plasma (hypotonic)
Excretion of hypertonic urine (less water, more solutes)
Requires
How
Occur
Requires: Antidiuretic hormone (ADH or arginine vasopressin) to alter transport (permeability) characteristics of collecting duct
How:
ADH = hormone that reduces water loss by increasing water reabsorption back into the blood
So ADH makes the CD more permeable to water by inserting aquaporins in principal cells
Allowing water to leave the duct and be reabsorbed into the blood
Producing concentrated urine as this leaves only solutes in the urine
Occurs: Dehydrated to retain water volume in the body
1.Proximal Tubule
What occurs here
Permeable to
Tubular interstitial fluid are
What occurs here: Reabsorption and secretion
Permeable to: Water
Tubular interstitial fluid are: Isotonic
Descending Loop of Henle #ff00b3
Water permeability
Not permeable to
What type of transport doesn’t occur here
So what type of transport does
What occurs
What diffuses out
What secreted in
Therefore what occurs to the tubular and interstitial fluid
What else helps produce it
Water permeability: Permeable
Not permeable to: Solutes
What type of transport doesn’t occur here: Active transport
So what type of transport does: Passive transport
What occurs:
Water diffuses out of tubules due to osmotic gradient
Between tubular lumen and interstitial fluids of renal medulla
Sodium secreted into tubules
Therefore what occurs to the tubular and interstitial fluid: Becomes hypertonic
What else produces it: Transport of Na+ and Cl- into interstitium without water
Ascending Loop of Henle #9800ff
Water permeability
So permeable to
Therefore tubular fluid leaving ascending LoH is
What is actively reabsorbed
Aided by which hormone
How
How is it sodium linked
Water permeability: NOT permeable
Permeable to: Solutes
Therefore tubular fluid leaving ascending LoH is: Hypotonic
What is actively reabsorbed: Sodium and chloride
Hormone: Aldosterone from adrenal gland
How: By co-transporters of Na+, Cl- and K+ —> cell
How is it sodium linked: Na-L-ATPase pump maintains the low intracellular sodium concentration
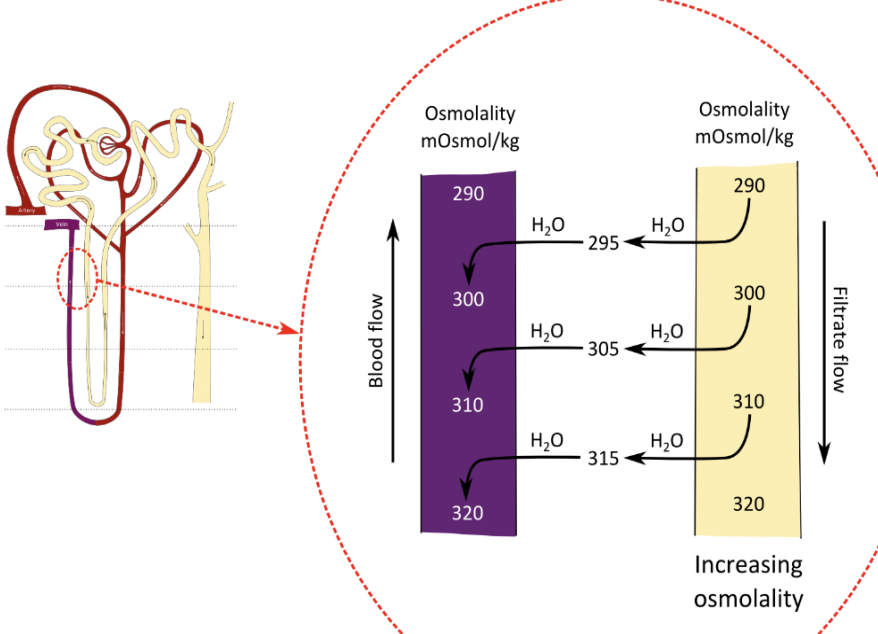
How is an osmotic gradient produced in the interstitial fluids of renal medulla and what is this mechanism called?
Because the asce- and desce- limb of LoH are close together in medulla
And tubular fluid flows in opposite directions
Called: Countercurrent mechanism
Where does interstitial fluid osmolality increase?
From outer zones —> inner zones of renal medulla
Counter-Current Mechanism: LoH
Involves
Interaction between
Involves: 2 fluids flowing in parallel but opposite directions in 2 U shaped tubes
Interaction between:
Flow of filtrate through LoH (countercurent multiplier) AND
Flow of blood through vasa recta blood vessels (countercurrent exchanger)
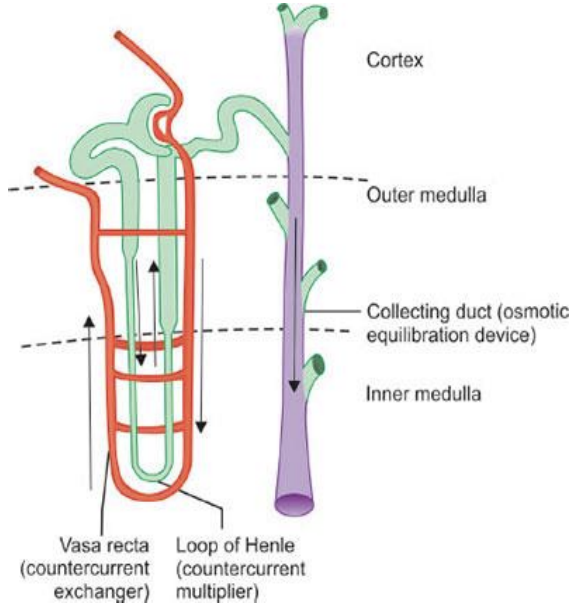
Collecting ducts in deep medulla permeable to?
Urea
Distal Tubule #ff8e00
In the presence of ADH, what occurs
In the absence of ADH, what occurs
In the presence of ADH: Water is reabsorbed and tubular fluid becomes isotonic
In the absence of ADH: Tubular fluid remains hypotonic
Collecting Duct
What occurs here
What are the target cells for ADH
What occurs in the presence of ADH
Inhibits
What occurs in the absence of ADH
Promotes
What occurs here: Regulation of electrolytes (Cl-, K+, H+ and HCO3-)
What are the target cells for ADH: Principal cells
What occurs in the presence of ADH: Stimulates the insertions of aquaporins allow for reabsorption of water
Inhibits: Diuresis (increase amount of urine production)
What occurs in the absence of ADH: Luminal cell membrane of principal cells are water impermeable so water enters urine
Promotes: Diuresis
So in what order does the fluid flow through?
PCT
Descending limb of LoH
Ascending limb of LoH
DCT
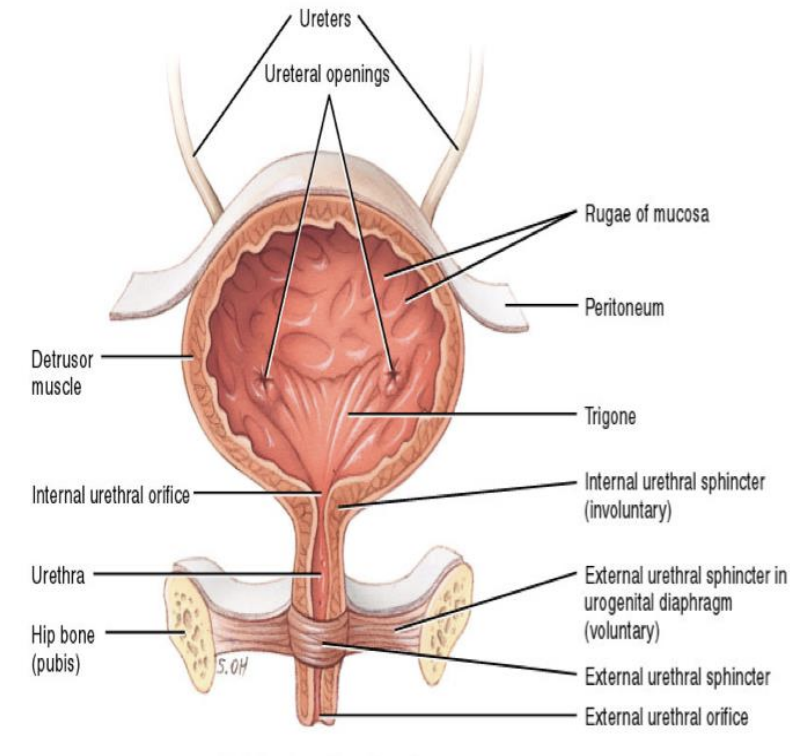
Micturition #ffc200
What
What stimulates micturition reflex
Activated by
How does urine reach bladder continuously
What does the bladder do during urine accumulation
When does micturition reflex activate
What happens
What nerves are responsible for bladder contraction
What: Expulsion of urine
What stimulates micturition reflex: Stretch receptors in bladder wall
Activated by: Distension from accumulating urine
How does urine reach bladder continuously: Through ureters
What does the bladder do during urine accumulation: Relax
When does micturition reflex activate: When bladder stretch becomes great enough to stimulate reflex centers in spinal cord
What happens:
Smooth muscle sphincter in bladder neck relaxes
Detrusor muscle contracts
What nerves are responsible for bladder contraction: Sacral parasympathetic nerves