Electromagnetic modalities lec
1/103
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
104 Terms
what are Electromagnetic Modalities ?
diathermy
photobiomodulation (LASER)
what is Diathermy ?
The application of high-frequency electromagnetic energy
primarily used to generate heat in body tissues
Can be delivered continuously or through regular pulses or bursts of radiofrequency energy
what diathermy heat is produced by?
Resistance of the tissue to the passage of the energy
By friction between two surfaces which converts kinetic energy to thermal energy
Diathermy may also be used to produce ?
nonthermal effects
As a therapeutic agent may be classified as two distinct modalities:
o Shortwave
o Microwave
• A shortwave diathermy unit is basically a radio transmitter
• The Federal Communications Commission (FCC) assigns three frequencies to shortwave diathermy units:
o 27.12 MHz with a wavelength of 11 m
o 13.56 MHz with a wavelength of 22 m
o 40.68 MHz with a wavelength of 7.5 m (rarely used)
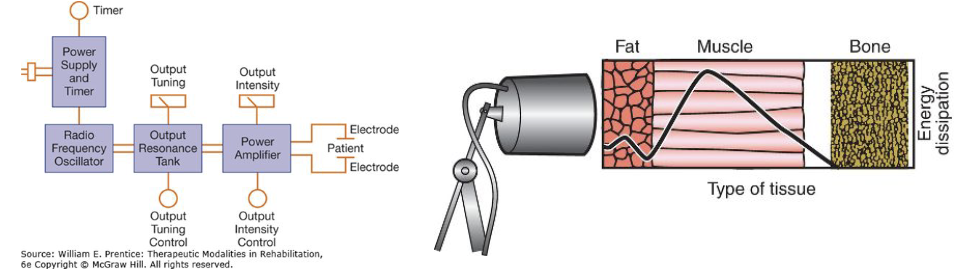
A __ unit consists of a power supply that provides power to a radio frequency oscillator
oscillator provides stable, drift-free oscillations at the required frequency
shortwave diathermy
The output resonant tank tunes in the patient as part of the circuit allowing?
maximum power to be transferred to the patient
The power amplifier generates the power required to drive the
different types of electrodes
Two types of SWD:
o Capacitive (Electric field method)
o Inductive (Magnetic Field Method)
SWD Can be delivered to body tissues either:
o Continuously
o Pulsed
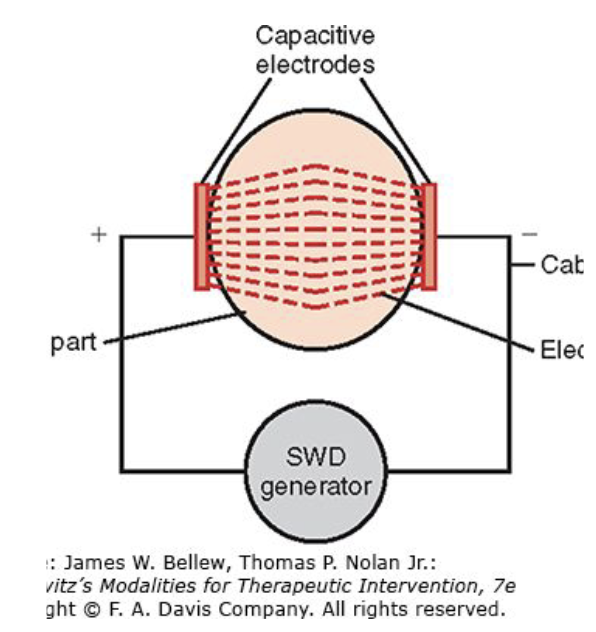
Uses an applicator system that requires that the patient’s tissues become part of a capacitor
Uses a rapidly alternating high-frequency current (AC) that creates a voltage differential between two electrodes
Electrodes are placed either one on each side
Or both on the same side of the part of the body
Each of the two electrodes has a different polarity
The patient is placed between two electrodes or plates and becomes part of the circuit
Capacitive SWD
Capacitive SWD Uses a rapidly alternating high-frequency current (AC) that creates a
voltage differential between two electrodes
for capacitive SWD electrodes are placed where?
either one on each side
Or both on the same side of the part of the body
Each of the two electrodes has a different polarity
The patient is placed between two electrodes or plates and becomes part of the circuit
Have adjustable arms with metal plates (electrodes) at their ends that deliver electromagnetic radio wave
Resistance to this current flow in the tissues results in tissue heating
Have a glass or plastic guard surrounding each metal plate to prevent contact between the electrode and the patient’s skin
An electrical burn may occur if either the therapist’s or the patient’s skin contacts the bare metal plate of the diathermy device
A single layer of terrycloth toweling should be placed between the plate guards and the patient’s skin to prevent concentration of the electric field on perspiration that may accumulate on the skin.
Capacitive SWD Application
Capacitive SWD Application Have adjustable arms with metal plates (electrodes) at their ends that deliver ?
electromagnetic radio wave
Resistance to this current flow in the tissues results in
tissue heating
Have a glass or plastic guard surrounding each metal plate to prevent contact between
the electrode and the patient’s skin
An __ may occur if either the therapist’s or the patient’s skin contacts the bare metal plate of the diathermy device
electrical burn
A single layer of __ should be placed between the plate guards and the patient’s skin to prevent concentration of the electric field on perspiration that may accumulate on the skin.
terrycloth toweling
The plastic plate guard should be located about __ from the skin for optimal heating
2 to 10 cm (1 to 3 inches)
Proper positioning of the plate and guard in relation to the skin provides effective absorption of thermal energy and safe heating of tissues
As the plate-to-skin distance increases, heat perception decrease
fat tissue may be heated considerably more than muscle when both tissues are exposed to the capacitive SWD electric field
Capacitive plates should not be placed over areas of thick subcutaneous fat
Capacitive SWD plates can be positioned in two possible arrangements:
o Contraplanar
o Coplanar
what is contraplanar?
The plates are placed on each side of the body part so that the body part creates a biological capacitor
what is coplanar?
The plates be positioned parallel on the same body surface rather than placing the body part between the plates
Coplanar arrangement is best for treating:
o Lumbar Spine
o Pelvis
Contraplanar arrangement is best for treating
extremities
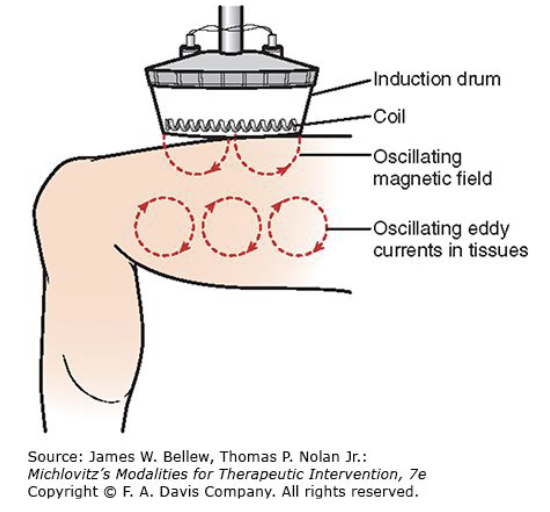
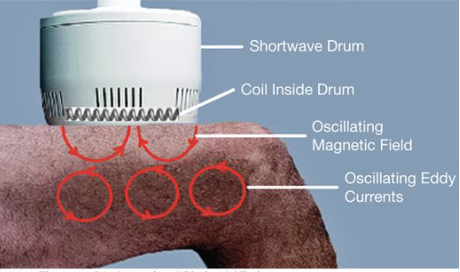
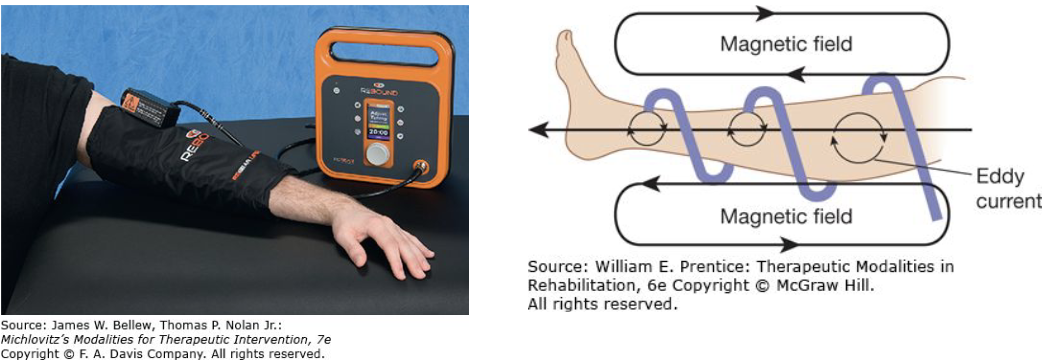
Shortwave Diathermy Inductive Method requires an?
inductive applicator that creates an oscillating magnetic field that induces “eddy” currents in body tissue
Eddy currents flow along pathways of higher conductivity causing?
heating in these tissues
The greatest density of eddy current activity occurs in low-impedance (high-conductivity) tissues containing the highest electrolyte content
Causes greatest heating in skeletal muscle and blood
Less heating occurs in
high-impedance tissues such as skin and fat

What is an Eddy Current?
A magnetic field generates small circular electrical fields
Fields vibrate and increase cell membrane permeability, which causes heat.
Creates a stronger magnetic field than an electrical field.
Induction diathermy relies primarily on a magnetic field to produce changes in tissue
Friction between the rotating dipoles results in an increase in kinetic energy, which results in heat (thermal effects)
With inductor electrodes the patient is in a magnetic field and is not part of the circuit
Shortwave Diathermy Inductor Electrodes
Shortwave Diathermy Inductor Electrodes creates a?
stronger magnetic field than an electrical field.
Induction diathermy relies primarily on a
magnetic field to produce changes in tissue
Friction between the rotating dipoles results in an
increase in kinetic energy, which results in heat (thermal effects)
Two types of inductive coil applicators can be used:
o Drums
o Sleeves
There are two types of drum applicators:
monode
diode
A monode is a drum used to
treat a single body surface
Requires a single layer of terrycloth toweling to create additional spacing and moisture absorption from the skin
The diplode is a
hinged drum that allows one or more body part surfaces to be treated simultaneously.
Approximately 1 cm of terrycloth toweling is recommended to separate the diplode applicator from the patient’s skin because the coil is closer to the treatment surface
An induction sleeve is a new method of delivering diathermy to a patient
Deliver shortwave diathermy at a power of 35 W and a frequency of 13.56 MHz
Sleeves are designed to fit around a body part
Heating ability is limited to moderate tissue temperature increases
Increases ease of application
It is important that the cables not touch each other because they will short out and cause excessive heat buildup
SWD Inductive Coils
__ on shortwave diathermy units vary considerably from one unit to another
control panels
Most modern shortwave diathermy units allow the clinician to select:
o average power
o pulse width
o frequency
The amount of energy absorbed by the tissue determines
change in tissue temperature
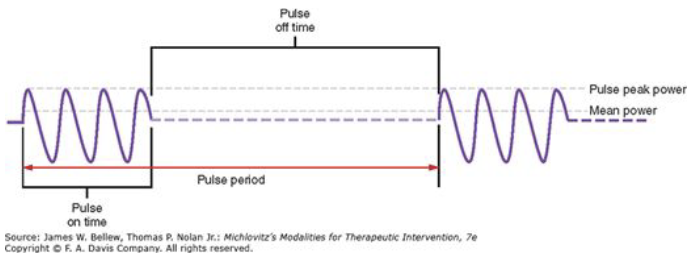
Most diathermy devices today are either PSWD or have both continuous and pulsed modes
use the inductive method with a drum electrode
Bursts of electromagnetic waves are created by interrupting the flow of continuous waves generated by the device
Pulse duration is in a range usually from 20 to 400 microseconds
(μsec).
The peak pulse power (the power in watts delivered during a pulse) ranges between 100 and 1,000 W in most devices that provide PSWD
The interpulse interval or off time depends on the pulse repetition rate, which ranges between 100 and 800 Hz
Average power output >38 W will cause increase in temperature
Pulsed Shortwave Diathermy (PSWD)
Pulsed diathermy is claimed to have
therapeutic value
produces nonthermal effects with minimal thermal physiologic effects
Pulsed shortwave diathermy can also have
thermal effects
When used with intensities that create an increase in tissue temperature
It has been suggested that a measurable heating effect can occur at power levels which are greater than
5 watts mean power
In clinical practice, the heating effect on the body’s tissues depends on the average power of the device. The average power can be determined by the following equation:
peak power (W)×pulse duration (s) ×pulse frequency=average power
Example: if the peak power of a PSWD device is 250 W, the pulse duration is .0004 second, and the pulse frequency is set at 145 Hz, the average power is 14.5 W
Calculating Mean Power
is seldom used as a clinical treatment modality by clinicians
Has two FCC-assigned frequencies in this country
2456 MHz (requires airspace b/w electrode and skin)
915 MHz
Microwave Diathermy
Microwave has a much higher frequency and a
shorter wavelength than shortwave diathermy
will not penetrate as deep as SWD or ultrasound
Microwave diathermy cannot penetrate the
fat layer as well as shortwave diathermy
SWD is preferred over MWD because of
greater depth of heating and a more predictable heat distribution pattern.
Selecting Diathermy Parameters
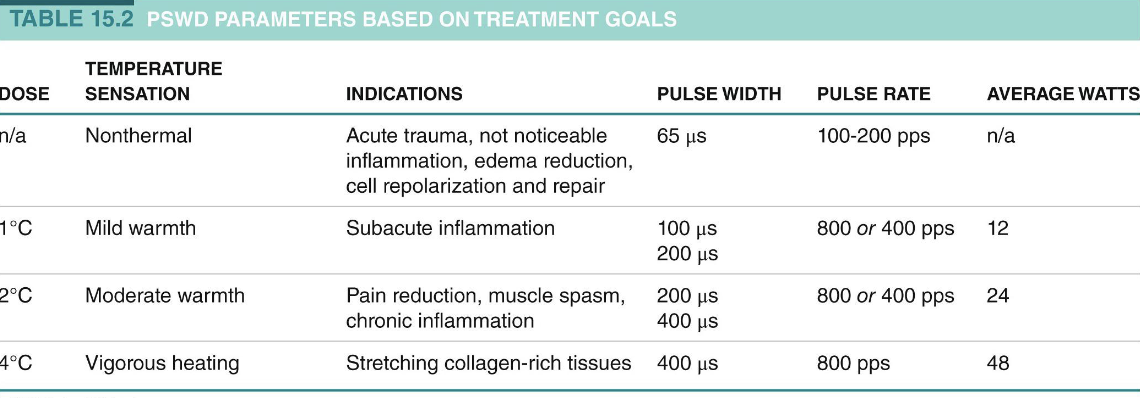
The most critical factor that determines whether a shortwave diathermy unit will increase tissue temperature is the amount of energy absorbed by the tissue
The power output of a shortwave diathermy unit should produce sufficient energy to raise the tissue temperature into a therapeutic range
As pulse rate, pulse width, and average watts increase, tissue temperature increases as follows during a 15–20 minute treatment time:
A 1°C increase occurs with an average power output of 12 W, pulse rate 800 pps, burst duration 100 μs, and interburst interval 850 μs.
A 2°C increase occurs with an average power output of 24 W, 800 pps, burst duration 200 μs, and interburst interval 850 μs.
A 3°C increase occurs with an average power output of 36 W, 800 pps, burst duration 300 μs, and interburst interval 850 μs.
4°C increase occurs with an average power output of 48 W, 800 pps, burst duration 400 μs, and interburst interval 850 μs.
Selecting Diathermy Parameters
A 20-minute treatment all that is necessary to reach vigorous heating in deep tissue
Vigorous heating = 104°F, or 40°C, from a baseline temperature of (98.6°F or 37°C)
When a vigorous heating protocol was applied for 20 minutes, average tissue temperature in the center of the treatment area increased an average of 4.5°C
average temperature 5 cm toward the periphery only increased an average of 3°C
Treatment Time
__ treatment all that is necessary to reach vigorous heating in deep tissue
20 minute
Vigorous heating =
104°F, or 40°C, from a baseline temperature of (98.6°F or 37°C)
__ in the radiofrequency range are nonionizing radiation
Electromagnetic waves
__ delivers only a fraction of the energy level required to produce ionization in tissue
Radiofrequency energy
Energy at a frequency of 100 MHz (in the FM radiofrequency band)
approximately 300 million times too weak to produce ionization
• Increased tissue temperature
• Heats deeper than superficial agents (such as hot packs), and heats larger and deeper areas compared to ultrasound
• Increase blood flow
• Vasodilation
• Relaxation
• Increased metabolism
• Decreased muscle spasm
• Reduced pain
• Realignment of collagen fibers and collagen content to increase tensile strength
SWD thermal Effects
Pulsed shortwave diathermy at a very low power (10 watts) has also been used for its nonthermal effects in the treatment of soft tissue injuries and wounds
Facilitate tissue healing by inducing a magnetic field which reactivates the sodium-potassium pump
restoring cell membrane potential which reestablishes normal polarity by returning normal ionic balance
Diathermy Nonthermal Physiological Effects
• Repolarization of damage cells
• Acceleration of cell growth
• Reestablishment of sodium pump
• Increased microvascular perfusion
• Improved cell function
• Increased white blood cells at wound site
SWD Nonthermal Effects
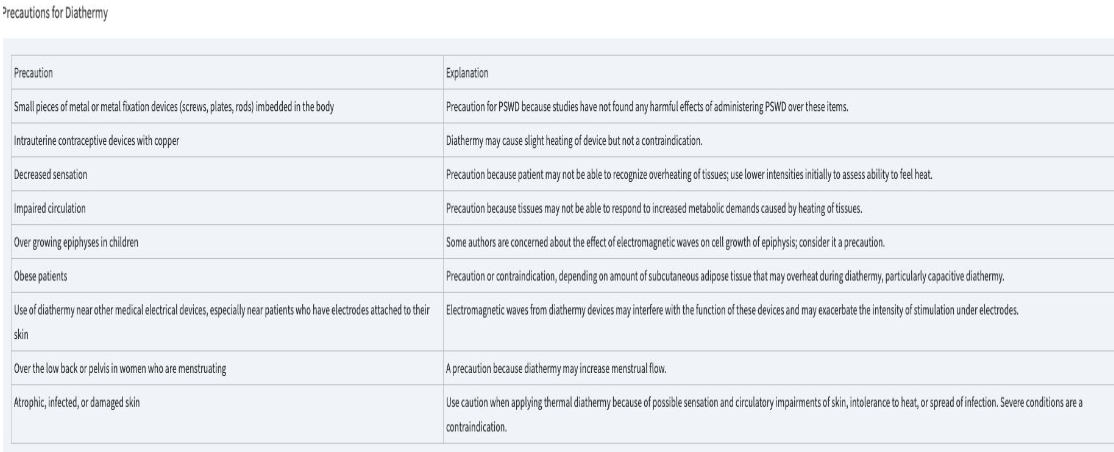
Precautions to Diathermy

Contraindications to Diathermy
magnetic field effect
electrical field
cell membrane permeability owing to electrical effect on cell Ca+ gating
PSWD
acoustic streaming
stable cavitation
micromassage
cell membrane permeability owing to mechanical effect on cell Ca+ gating
ultrasound
a few more contraindications
no couplant needed
can be applied over most clothing
easy to use
less affordable clinician can attend to other duties
heats large areas
retain heat two to three times longer
SWD
a few contraindications
couplant required
possible disrobing
easy to use
affordable
monitoring by clinician
heats small areas
retain heat
ultrasound
can heat tissues 3-5 cm deep to > 40 degrees celsius
heat large areas
long stretch /thermal window
5-10 minutes
less mess
can apply over some clothing
PSWD
can heat tissues 3-5 cm deep to > 40 degrees celsius
heats small areas
short stretch/thermal window
5-10 minutes
ultrasound
Increased Angiogenesis and Neovascularization-Oxygen to injured tissue
Increased Collagen Production-good alignment reduces internal scar and enhances elasticity
Muscle regeneration-repair of damaged fibers leading to regeneration
Decreases inflammation and edema-increases macrophages
Nerve Regeneration, Cartilage Production, and Bone Formation-growth factors, chondrocytes and osteocyte development
Indications for LASER
What are approved indications?
• Indications that are approved by the FDA (Very Specific)
o Increase in local circulation
o Relief of minor muscle and joint ache, pain, and stiffness
o Relaxation of muscle tissue
o Relief of spasms
o Relief of arthritis associated minor pain/stiffness
Therapeutic use is based upon photons being absorbed into body tissues, triggering biochemical effects in cells
Examples: laser, light-emitting diode (LED), and superluminescent diode (SLD)
Light exposure has been shown to stimulate the production of ATP and augment RNA synthesis in body cells
Electromagnetic Radiation: Lasers and Light
Light exposure is also believed to
• Affect calcium channels in body cells
•Promote the formation of collagen by stimulating fibroblasts
•Control inflammation by decreasing inflammatory cells
• Inhibit growth of microorganisms
• Promote vasodilation and formation of granulation tissue
•Affect nerve conduction velocity
•Affect nerve regeneration
Photobiomodulation Other terms are used synonymously
o Phototherapy
o Biostimulation
o Laser Therapy
• LASER = Light Amplification by Stimulated Emission Radiation
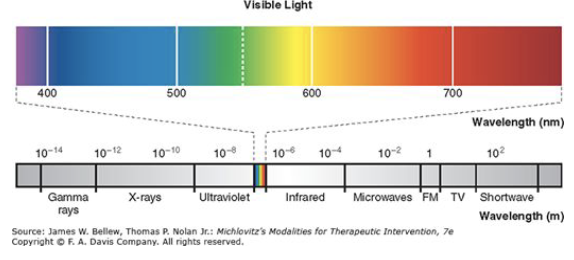
A form of electromagnetic energy that has wavelengths and frequencies that fall within the infrared and visible light portions of the electromagnetic spectrum
Electromagnetic light energy is transmitted through space as waves that contain tiny “energy packets” called photons
Wavelengths are typically between 600-1200 nm
Longer wavelengths penetrate better
Water has a high absorption between 1200-2000 nm
Melanin has high absorption between 400-600 nm
Physics of LASERs
The laser light is emitted in an organized manner
Differing from the random pattern from incandescent and fluorescent light sources
Three properties distinguish the laser:
o Conherence
o Monochromaticity
o Collimation
what is Coherence?
The individual light waves are in phase and aligned with one another in space and in time
what is Monochromaticity?
o Refers to the specificity of light in a single, defined wavelength
o If on the visible light spectrum, it is only one color
what is collimation?
o There is minimal divergence of the photons in the laser beam
o photons move in a parallel fashion
The four most commonly used lasers are:
o Helium neon (HeNe)
o gallium arsenide (GaAs)
o gallium aluminum arsenide (GaAlAs)
o neodymium-doped yttrium aluminum garnet (Nd:YAG)
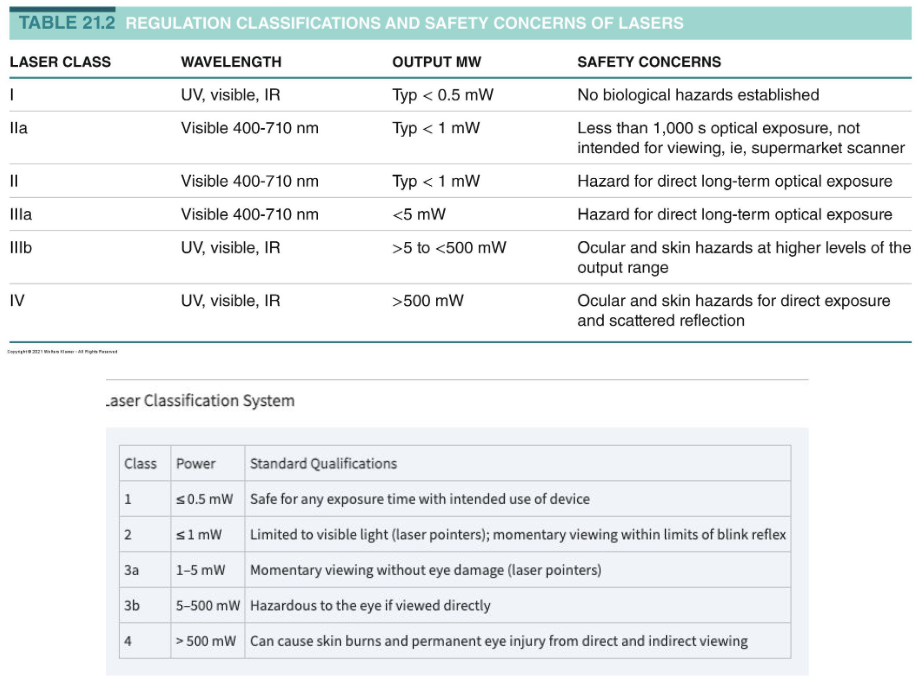
Classification is by risks associated with exposure-higher the higher the risk
PTs typically use low level lasers
High level Class 4 are an option (>500mW)
Class 3B<500mW is consider low level
Lasers are a point or cluster
classification of LASERs?
• Wavelength (nm)
• Duty cycle (%) and frequency (Hz)
• Beam size (cm)
• Power and irradiance (W/cm2)
• Treatment time (s)
• Fluence (J/cm2)
• Total energy (J)
Photobiomodulation Treatment Parameters
• Wavelength determines the color of light
• Is constant for device
wavelength (nm)
Duty cycle is similar to ultrasound or diathermy
Duty cycle equals the on-time and off-time of the light
(Time on/(Time on + Time off))/100
If the light is pulsed, the light’s frequency should be reported
Current clinical trials suggest that pulsed light may be superior to continuous PBM
Duty cycle (%) and frequency (Hz)

It’s the radius of the light aperture.
Size of the beam effects PBM irradiance.
Irradiance = Device Power (W)/Beam Size (cm2)
beam size (cm)
Irradiance = Device Power (W)/Beam Size (cm2)
o Usually reported in W/cm2
Power and irradiance (W/cm2)
Reported in seconds
Maybe reported in seconds/spot or total treatment time during a scanning mode
Should be determined for each device based on the device’s irradiance and the desired fluence
Treatment time (s)
Often referred to as the PBM dose
Represents the number of photons delivered per unit area of tissue
Fluence (J/cm2) = Irradiance (W/cm2) × Time (s)
Fluence (J/cm2)
The total energy delivered to the tissue
Total energy (J) = fluency (J/cm2) x beam size (cm2)
Currently, there is no consistency in reporting fluency or total energy.
World Association of Laser Therapy (WALT) has created specific guidelines based on 780- to 860-nm and 904-nm wavelengths
Total energy (J)
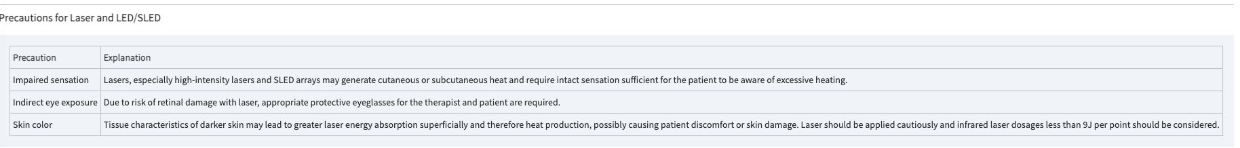
laser precuations

LASER Contraindications
Class II and higher can cause damage to eye
Class 3b and IV lasers require both the clinician and patient to wear protective eyewear when devices are being used
Treatments should be performed in private room that protects others
Eyewear is unit specific and is made for the associated wavelength
DO NOT wear protective eyewear designed for other units
LASER Safety
The laser, parameters, and treatment technique selected will depend on the desired treatment effect
The wavelength of the laser will impact the penetration depth of the light
The laser’s power intensity and the tissue properties of the chosen treatment area play a role in the light being reflected or absorbed.
LASER Parameters
The goal of laser therapy is to supply a sufficient amount of light energy to the designated treatment area for a period of time
It is important when setting up or documenting a treatment you consider all the parameters
The power output of a laser device is measured in watts (W) or milliwatts (mW), which is 10 −3 watts
A watt describes the amount of energy released by the laser device per second
W = J/Sec
Laser energy density is determined by knowing the surface area of the applicator probe tip and would be measured in J/cm2
Laser dosimetry is often measured as total joules per treatment session or in joules per treatment point or body surface area depending on the mode of application
LASER Parameters
The World Association for Laser Therapy (WALT) has published recommendations to help clinicians determine appropriate parameters for different pathologies
They recommend daily treatments for 2 weeks or laser treatments every other day for 3–4 weeks.
The current WALT guidelines indicate greater energy is needed for the GaAlAs lasers from 780 to 860 nm compared to the superpulsed GaAs lasers at 904 nm
Selecting Dose