6.0 altitude sickness
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
The air we breathe contains approximately 21% oxygen, a proportion that remains constant at all altitudes
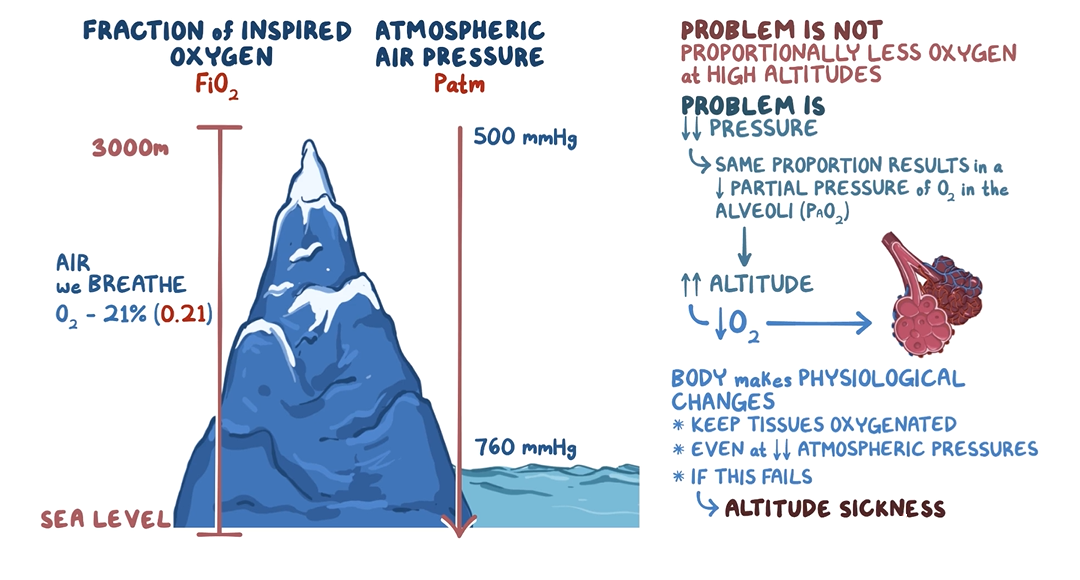
However, as altitude increases, the atmospheric pressure (Patm) decreases → a fewer number of oxygen molecules are inhaled with each breath
and so there are fewer oxygen molecules available to diffuse from the alveoli into the bloodstream which can cause altitude sickness.
Altitude sickness symptoms typically manifest 6 to 10 hours after reaching high altitude and may include symptoms such as
headache,
dizziness,
and shortness of breath due to insufficient oxygen supply.
In severe cases
high-altitude cerebral oedema (HACE)
and high-altitude pulmonary oedema (HAPE) can also occur.
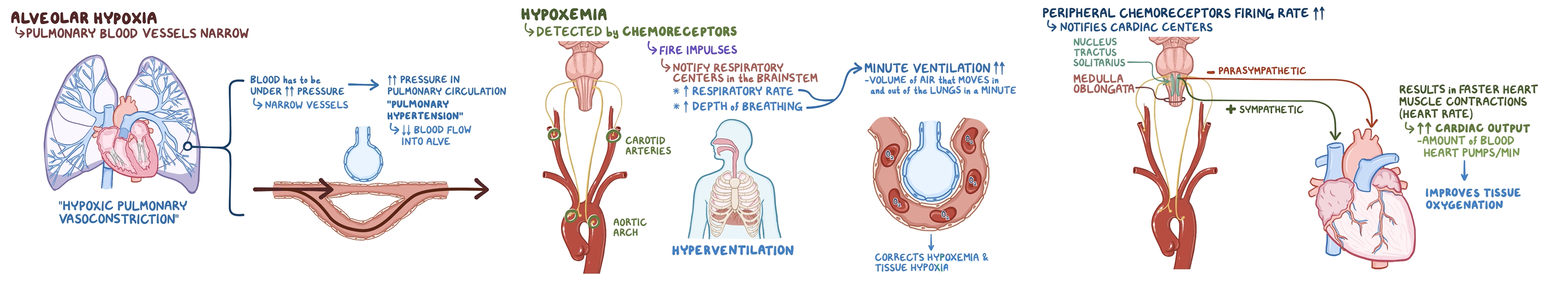
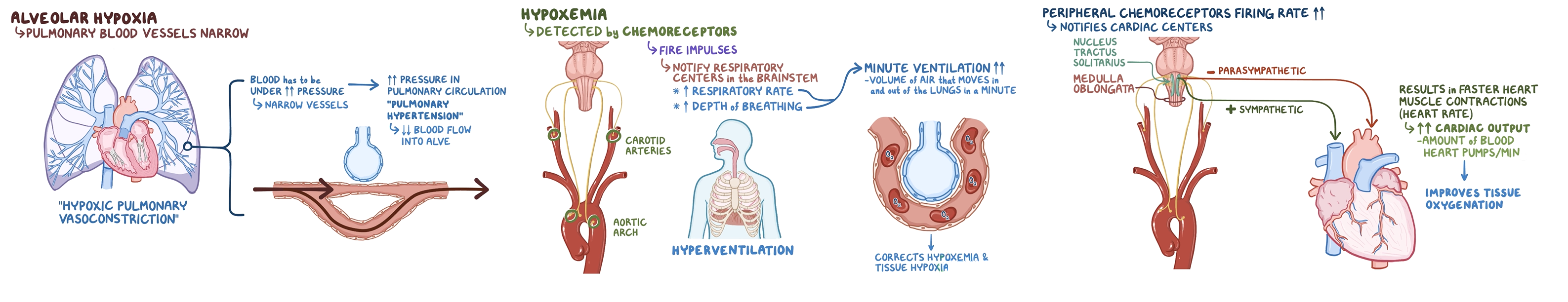
n response to alveolar hypoxia,
pulmonary blood vessels constrict, a process known as hypoxic pulmonary vasoconstriction.
hypoxic pulmonary vasoconstriction.
when some areas of the lungs have low oxygen the blood vessle sin those areas constrict causing blood to be diverted to areas with better oxygen elvels allowing for better gas exchange
When this happens across multiple pulmonary capillaries,
less blood reaches the alveoli for oxygenation, further worsening hypoxaemia and tissue hypoxia.
To prevent this cycle from escalating, peripheral chemoreceptors in the carotid arteries and aortic arch detect the low oxygen levels (hypoxaemia)
and start firing signals to the brainstem's respiratory centres.
In response, the brainstem increases the rate and depth of breathing—
a process called hyperventilation
This adjustment helps bring in more oxygen,
partially correcting hypoxaemia and improving tissue oxygenation.
At the same time, these chemoreceptors send signals to the cardiac centres in the medulla oblongata,
which control heart rate and blood pressure.
The medulla reduces parasympathetic activity and increases sympathetic stimulation,
which raises the heart rate and cardiac output—the amount of blood pumped by the heart per minute
These changes ensure that more oxygen is delivered to the tissues,
helping to counteract the effects of hypoxia.
Pulmonary Adaptations to Alveolar Hypoxia.
As altitude increases,
sustained hyperventilation becomes more pronounced, leading to an excessive loss of carbon dioxide (CO₂) through exhalation.
Normally, CO₂ combines with water in the blood to form carbonic acid (H₂CO₃),
which then dissociates into hydrogen ions (H⁺) and bicarbonate (HCO₃⁻) to help maintain a stable blood pH.
When too much CO₂ is lost due to hyperventilation, the concentration of hydrogen ions decreases,
making the blood more alkaline—a condition called respiratory alkalosis.
This increase in blood pH signals the peripheral chemoreceptors to reduce their firing rate, which, in turn, reduces respiratory drive.
As a result, hyperventilation slows down, which worsens hypoxia by decreasing oxygen intake.
To restore the body's ability to continue hyperventilating while maintaining pH balance,
the kidneys excrete bicarbonate (HCO₃⁻) into the urine, which helps compensate for the alkalosis.
This loss of bicarbonate allows more carbonic acid to dissociate into bicarbonate and hydrogen ions, bringing blood pH back to normal.
With pH corrected, the chemoreceptors resume their firing rate, allowing hyperventilation to continue, ensuring adequate oxygen uptake at high altitudes.