Adaptive Immune System
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
what is the adaptive immune system
is specific, can recognise and react to different pathogens with different responses due to different receptors coded for in our genes
has a great diversity of possible responses to pathogens
has memory
capable of self-tolerance (doesn’t attack itself)
what is the humoral response?
effective against pathogens in body fluids
utilises B cells
characterised by the production of antibodies
what is the cellular response?
effective against intracellular pathogens (pathogens inside host cell)
utilises T cells
characterised by the destruction of infected cells
how are antigens recognised?
T and B cells have specific receptors which can bind to antigens on their cell surface
Each T and B cells has a unique antigen receptor which can bind to one type of antigen
different receptors coded for in the genes are present from birth
what is the cell mediated response?
T cells target and destroy infected cells
T cells can bind to infected cells via the receptors on their surface
this cell mediated immunity is effective in defending the body against:
pathogens inside cell
macroparasites
tumour cells and transplanted tissue
antibodies cant get to pathogen inside cell therefore cell-mediated response is needed
uses chemicals for the attack of the infected cell
what do the T cells and MHC molecules do?
T cells recognise fragments of antigens which are displayed on the surface of the cells
allows T cells to recognise antigens that have been partially digested by macrophages, etc
specific surface markers called MHC molecules are involved in recognising self-cells
bind to peptide fragments of digested antigens and display them on the cell surface for recognition by T cells
what does MHC I do?
cell infected pathogen will display fragments of the pathogen on its MHC molecule
what does MHC II do?
antigen presenting cells, activated B cells and macrophages, present the antigen fragments on MHC II molecules.
what are T lymphocytes
produced in bone marrow
mature in thymus gland
released into blood and migrate to lymph nodes and other parts of the body
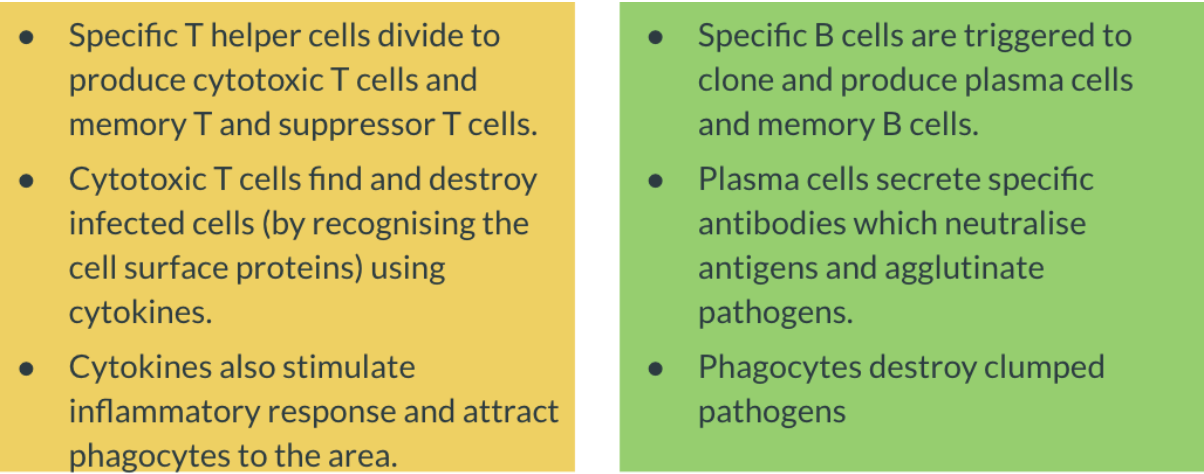
how all the cells work together?
1) antigen presenting cells (B cells, macrophages, dendritic cells) migrate to the lymph nodes
2) receptors on the surface of a specific T helper cell bind to the antigen
3) activates the T helper cell and stimulates the release of cytokines
4) cytokines have a variety of effects, including stimulating T cells to rapidly clone and produce cytoxic T cells that bind to infected cells and kill them through the release of more cytokines
5) cytokines cause infected cell to die by triggering lysis by apoptosis
6) cytokines also attract phagocytes (chemokines) to the area to clear up the cell debris and trigger inflammation (histamine and prostaglandin)
7) when the production of cytoxic T cells is triggered, supressor T cells and memory T cells are also produced
how are b lymphocytes made?
responsible for adaptive immune response outside cells
made in bone marrow,
stored in lymph nodes,
circulate in the blood
how are B lymphocytes activated and what do they do?
activated by cytokines released by Helper T cells
activated by binding to an antigen
once activated:
make copies of themselves (clone)
differentiate into 2 possible cell types:
plasma cells - they are capable of making antibodies
memory B cells - remember the pathogen for subsequent infection
what are antibodies?
molecules produced by plasma cells in response to a certain pathogen
also called immunoglobulins
act to neutralise a pathogen
ways antibodies neutralise a pathogen? 3
antigen neutralisation
bound antibodies block antigens from binding to other targets, prevent toxins from destroying a cell
agglutination
pathogen becomes trapped in a network of antibodies, making them immobile + susceptible to destruction.
remember glued together
complement activation
bound antibodies activate a cascade of compliment proteins
complement protein can punch holes in the pathogen or create an inflammatory response which attracts macrophages and neutrophils.
flowchart of the process 🙈
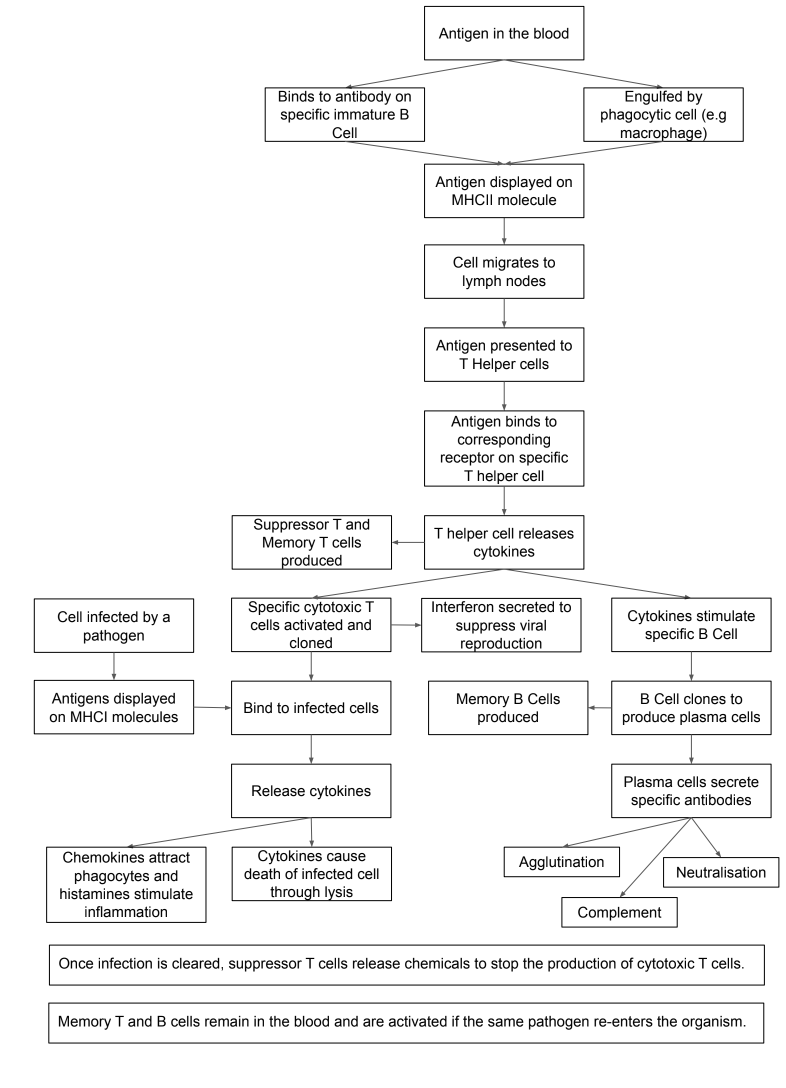
how do T and B cells interact?
they both attack the anitgen
Helper T cells assist in interaction by releasing chemicals (cytokines) to stimulate B cells and T cells to clone
B cells can also activate Helper T cells
if a B cell encounters an antigen it binds to the antigen and presents it to the helper T cell
T helper cells release cytokines that activate more Helper T cells and macrophages
outline the third line of defence?
vaccine enters and triggers inflammatory response
initially mediated by the non-specific immune system
dendritic cells are attracted to antigen
antigens are taken up by dendritic cells and presented on the cell surface membrane; migrate to lymph nodes
T cells that recognise specific pathogen being presented by dendritic cell bind to the anitgen
process activates T cell to become helper T cell
immature B cell pick up antigen on there surface by immunoglobulins
helper t cells bind to antigen on the B cell then releases cytokines that stimulate the B cell
once stimulated, B cell go through rapid proliferation, differentiating into plasma cells and memory B cells
further stimulation of B cells by T cell action leads to affinity maturation where the affinity antibodies are produced
when infection is over, plasma cells die off, antibody concentration falls
contraction phase
second response of encountering the same disease?
adaptive immune system retains memory of the anitgen for future use
continue to secrete low level of high-affinity
immunological memory
when body exposed to same antigen the high-affinity antibodies in the blood bind to the antigen
acts as a signal
memory B cells and T cells are activated faster
memory B cells proliferate into plasma cells in higher concentrations
there further muturation, cells are more specific
antibody becomes quicker, more sustained, higher-affinity
what happens to T and B cells when the T helper cell with complementary antigen receptors activated?
why is the primary immune response slower?
the time taken to fight an infection is longer because once antigen has been identified appropriate T cell and B cells have to be activated.
takes time to build clones of these cells
called the lag phase 4-7 days (can be longer)
time needed for the cytotoxic T cell to kill infected cells + for the B cells to produce plasma cells that secrete antibodies that bind with the antigen to neutralise it
antibody peak is 7-10 days after infection
if sufficient antibodies are made to destroy all infecting antigens, person recovers completely:
primary immune response
same time memory T cells + memory B cells specific to antigen are produced and remain in the body
why is the secondary immune response faster?
if same antigen reentered the body, the second response if quicker
after identification of antigen, memory cells activate the production of the cytotoxic T cells + B cells
large number of B cells from many plasma cells, secrete larger amounts of antibodies than in primary response
lag phase reduced to 1-4 days
antibody peak is 3-5 days after infection
effect is to destroy invading antigens before their numbers are large enough to cause symptoms
secondary response is:
quicker
requires less antigen to intiaite it
produces a much greater quantity of antibodies
Comparing immune responses
Feature | Primary Response | Secondary Response |
Definition | The reaction of the immune system when it contacts an antigen for the first time | The reaction of the immune system when it contacts an antigen for the second time and subsequent times |
Responding Cells | Naive T + B cells | Memory T + B cells |
Lag Phase | Long (4-7 days) | Short (1-4 days) |
Antibody Peak | Antibody level reaches peak in 7-10 days | Antibody level reaches peak in 3-5days |
Strength Of Response | Weaker than secondary | stronger |
Antibody Level Over Time | Declines to the point where it may be undetectable | Tends to remain high for longer |
graph of primary and secondary response explain every number
1) antigen is detected by immune system, B cells activated
divide to produce plasma cells, that produce antibodies
takes time, causing lag phase 4-7 days
memory B cells also produced
2) as more plasma cells are produced, amount of antibody released increases
3) antibody peaks
pathogen destroyed
antibody production decreases as less anitgen present
memory cells are still present
4) memory T cells activate memory B cells which quickly differentiate into plasma cells, produces large amounts of antibody quickly
high peak of antibody due to presence of more plasma cells producing antibodies
pathogen destroyed before symptoms begin
5) antibody production decreases as fewer antigens present
more memory T + B cells have been formed
what is inside the vaccines - three types?
vaccines contain cultures of microorganisms, may either be:
living but attenuated - weakened - therefore harmless, rabies
dead, typhoid
contain toxins called toxoids (tetnus)
vaccines may be given orally or by scratching skin surface
may use nucleic acids, mRNA, DNA
how do vaccines work?
are all harmless to the body, will ot cause the disease they are specific for
some contain antigens that make your body undergo an immune response + produce memory cells for that particular antigen
if body is exposed to antigen in future, secondary response is activated
antigen destroyed before symptoms of disease are experienced
immunity formed is lifelong to the one type of disease
compare vaccination to immunisation?
vaccination involves introducing vaccine into body
immunisation is a process where the body reacts to the vaccine by going through the immune response, producing memory cells for the antigen
confers immunity to the body so if antigen enter in future secondary response occurs - no symptoms suffered
what is the effectiveness of vaccines?
a series of vaccines should be given over a number of years
each vaccine introduced produces small response
a series of vaccinations, lymphocytes will more rapidly recognise the antigen and the number of memory cells will be enough for a long time
# of memory cells can decrease over time, booster injections neededto increase number of circulating memory cells, ensures disease is maintained
e.g. booster injections given to maintain immunity for tetanus and whooping cough as the number of memory cells for this decreases over time.
what is passive acquired immunity?
involves introducing antibodies (immunoglobulins) into the body to prevent a disease from developing
these antibodies are produced by another organism that suffered the disease
E.g. being exposed to disease Hepatitis A, you may be given injections of immunoglobins to preent you from contracting the disease
Immunity will last for only a couple of months no memory cells have been produced
what is herd immunity?
form of indirect protection from disease that happens to individuals when most of population around them is immune
vulnerable people who haven’t been exposed to or vaccinated against disease are safer and it cant spread easily
what is polio?
virus transmitted by oral contact, with secretions or faecal material from infected person
Most cause no symptoms with viral replication limited to cells of the digestive tract
Less then 1% of infections, polio virus invades the nervous system and can cause irreversible paralysis
People with paralysed respiratory muscles may spend the rest of their life in iron lungs
There is no cure and no medication, but since 1955 there have been safe and effective polio vaccines