PH Exam 2
1/203
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
204 Terms
Doneisha Bohannon MPH
Director of community health initiatives at BJC healthcare
STL city infant death rate
9.4 deaths per 1000 live births
higher than national and state average
Maternal mortality racial difference
Black women die at 2.5x the rate of white women, it peaked during the pandemic
Social determinants of health
education access and quality
economic stability
social and community context
neighborhood and built envio
healthcare access and quality
Drivers of health percentages
40% socioeconomic
10% physical envio
30% health behaviors
20% healthcare
Socioecological model for health
policy
community
institutional
interpersonal
individual
Why doulas
higher satisfaction with birth
less c-sections
higher rates of breastfeeding
less pre-term babies
less post-partum depression
What is maternal mortality
death associated with pregnancy, childbirth (and up to 30 days later), miscarriage, or abortion
what is Infant mortality
death during first year of life
what is neonatal mortality
stillbirths, deaths to 30 days
Is infant mortality going down from 1965-2005
yes
Infant mortality and education and race
it goes down with more education, blacks always the most though and at first hispanic is the least but then with college+ asian is the least
Causes for infant mortality
congenital
LBW and premature
SIDS
Old standard to judge infant mortality
NCHS - 1978, US
new standard to judge infant mortality
WHO - 2008, US, NHANES, plus data from brazil, ghana, india, oman, norway
What is looked at when looking at infant mortality
weight for age z score (WFA or WAZ)
height for age z score (HFA or HAZ)
weight for heigh z score (WFH or WHZ)
mid-upper arm circumferemce in cm.
Why do you use a z score when looking at kids health
age and sex lead to differences in expectation so the z-score and percentiles make it easier to compare
Wasting
low weight for age or weight for height
what does wasting mean
measure of acute malnutrtion
occur at any age
recovery is possible
how is wasting classified
moderate acute malnutrition: WHZ < -2 and >-3
severe acute malnutrition: WHZ < -3 with additional symptoms
Stunting
low height for age
what does stunting show
usually measure of chronic malnutrition
often occurs by age 2
catch-up growth is possible but often height deficits persist
Kwashiorkor
protein-energy malnutrition
accumulation of fluid (edema) in tissues
dermatitis, hair color change
Marasmus
energy malnutrition
loss of weight, fat, muscle
low body temp
low blood sugar
infection
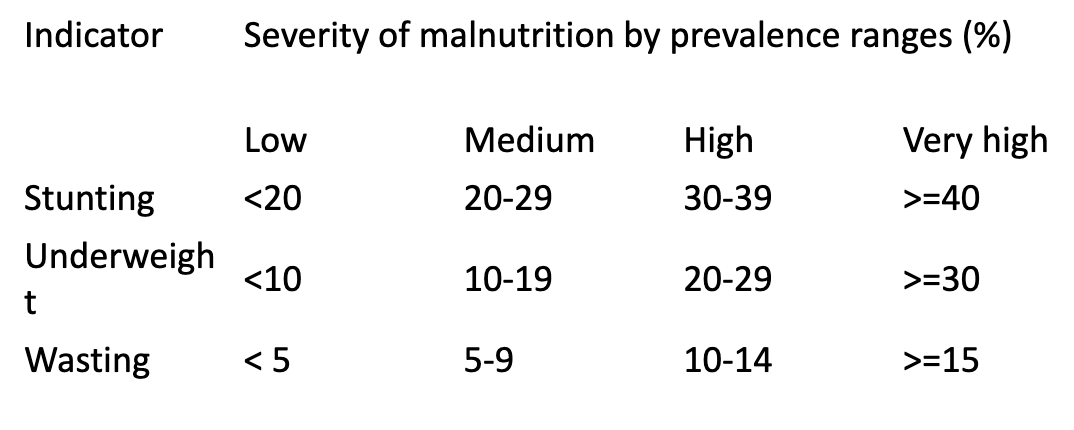
severe malnutrition by prevalence ranges
How many children have SAM
20 million kids
How many children have MAM
41 million kids
Where does most SAM and MAM occur
southern asia, subsaharan africa
How many ppl have expereince(d) stunting
195 million children, 800 million including adults
In 20 countries what percent of kids experience SAM, MAM, stunting, etc.
85%
Micronutrients
micronutrients are nutrients needed in very small amounts compared to macronutrients (fat, carbs, protein)
Why are micronutrients important
balance is associated with dietary diversity
six common micronutrients
iodine
vitamin a
iron
vitamin c
thiamine
niacin
iodine purpose
produce specific thyroid hormones
source of iodine
marine foods
iodine deficiency can lead to
goiter which is the expansion of the thyroid can cause cretinism in pregnancy (serious growth and mental problems)
vitamin a
fat soluble vitamin needed for retinal function
vitamin a deficiecny can lead to
night blindness and retinal defects (congenital)
sources of vitamin a
meat and vegetables
iron deficiency anemia prevelance
one of the most common forms
1.62 billion ppl have it
symptoms of iron deficiency
fatigue, muscle weakness, cold hands, cold feet, change to heart rate, change to nails, change to skin, irritability
what is anemia associated with
infection, poor dietary intakes
what does anemia have impact on
growth and cognitive function
vitamin c deficiency where is it found
emergency situations or displaced ppl
what can a lack of vitamin c lead to
increased bruising, bleeding, loss of teeth, fatigue
what provides a lack of vitamin c
lack of fresh fruits and veggies
thiamine deficiency (beriberi) leads to
loss of motor control, difficulty walking, overall muscle weakness, GI and cardiovascular issues
thiamine purpose
breakdown of glucose, neurons
what is thiamine associated with in terms of diet
rice based diet, modern commercial rice commonly fortified
niacain deficiency (pellagra) common in
corn, maize consuming population
symptoms of pellagra
diarrhea, dermatitis, dementia, death
how pellagra is treated
treatment of corn with lime and consumption of beans
contributors to malnutrition
infection
marginal nutrition
complimentary foods/inappropriate
improperly prepared foods
infection types as a contributor to malnutrition
fever
viral/bacterial
helminthic
marginal nutrition as a contributor to malnutrition
seasonality in food supply
difficulties accessing food
sex based priorities in feeding
complimentary foods/inappropriate or improperly prepared foods in malnutrition
contaminated foods
early introduction
suboptimal breastfeeding
non-fortified foods (low iron, other vitamins)
infection
vector borne (dengue, malaria)
communicable (pneumonia, measles)
helminths (worms)
associated with increase in metabolic needs, wasting, stunting
contributes to morbidity and mortality
malnutrition infection synergy
inadequate diet —> infection —> weight loss, decreased immunity, growth faltering —> more disease, increased severity —> increased nutritional needs, loss of appetite
helminths
intestinal parasites (worms)
extremely common in children
infection start at 6 months
weight loss, growth stunting (even if they have enough calories)
malaria
common in many parts of the world
mosquito borne illness
once infected can have later cycles of malaria without reinfection
associated with significant <5 year old mortality
marginal nutrition
acute or chronic
seasonality of food intake
inappropriate weaning practices
acute marginal nutrition
disruption due to natural disaster, conflict, displacement, etc.
chronic marginal nutrition
chronic low nutrient intake reflection larger social, political, economic forces (structural violence)
seasonality and malnutrition
seasonal changes can impact food availability and infection risk
access to food often decreases before a harvest, when workload increases
rainfall (rainy vs. dry) also alter pathogen risk by limiting clean water (dry) or flooding (rainy)
london 1854 two competing disease theories
miasma theory (the establishment)
germ theory (john snow)
Miasma theory (the establishment)
disease is spread by “bad air”
supported by leading physicians
made intuitive sense (bad smells = disease)
treatment: perfumes, flowers, flee to countryside
germ theory (john snow)
disease spread by contaminated water
based on mapped evidence
contradicted common sense
treatment: remove pump handle
When has “common sense” killed
thalidomide for morning sickness —> 10,000+ birth defects
bed rest for back pain —> prolonged disability
SIDS and stomach sleeping —> thousands of preventable deaths
evidence based medicine
individual patients
RCTs common
clear outcomes
direct physician-patient relationship
evidence based public health
entire populations
RCTs often impossible
complex long-term outcomes
multiple stakeholders, politics
bradford hill criteria
strength of association
consistency across studies
specificity of effect
temporality (exposure before outcome)
biological gradient (dose response)
plausibility (makes biological sense)
coherence with existing knowledge
experimental evidence
analogy to similar exposures
research to reality
research
evidence synthesis
guidelines
implementation
evaluation
tradeoffs in PH decisions: type 1 error (false positive)
implementing ineffective intervention
wasted resources
potential harm
example: vitamin e
tradeoffs in PH decisions: type 2 error (false negative)
missing effective intervention
continued suffering
example: delayed seat belt laws
when evidence is incomplete when should we do smth before cause and effect is fully established
precautionary measures should be taken if not raises threats to harm health
when evidence is incomplete when should we do smth before cause and effect is fully established examples
banning CFCs before ozone mechanism
COVID masks before aerosol transmission proven
climate action despite uncertainty
where to look for findings (databases)
pubmed/medline
cochrane library
campbell collab
guide to preventative services
where to look for findings (key resources)
CDC’s community gudelines
WHO guidelines
NICE (UK)
USPSTF recommendations
where to look for findings (grey literature)
gov reports, NGO evaluations, unpublished data
Forumulating answerable questions using PICO
population (who)
intervention (what)
comparison (compared to what)
outcome (what are we measuring)
gold standard of evidence
systematic review
meta-analysis
systemic review
comprehensive search
explicit inclusion criteria
quality assessment
narrative synthesis
meta-analysis
stat pooling of results
forest plots
heterogenity assessment
When science decisions cant wait
during emergencies when there are rapid reviews, living systematic reviews, real-time surveillance, adaptive trial designs, precautionary actions
Skills for EBPH practice
ask answerable questions (PICO)
acquire evidence efficiently
appraise evidence critically
apply evidence appropriately
assess impact and adjust
other types of knowledge
qualitative research (understanding why)
community knowledge (local context)
indigenous knowledge (traditional practices)
practice based evidence (what works in real world)
emerging trends in research
big data and predictive analytics
machine learning for evidence syntheis
real world evidence from EHRs
citizen science
implementation science focus
equity centered evidence
when evidence conflicts with values (scenarios)
evidence supports needle exchange, community opposes
RCT would be ideal but unethical
evidence is weak but need is urgent
when evidence conflicts with values (framework)
transparency about evidence quality
community engagement
clear value trade-offs
monitoring and adjustment
important notes about evidence
evidence based does not equal evidence paralyzed
best available evidence is not perfect evidence
context always matters
absence of evidence is not the evidence of absence
evidence is necessary but not sufficient
community values and feasibility matter
17 points of public health
surveillance
disease and health event investigation
outreach
screening
referral and followup
care mgmt
delegated functions
health teaching
counseling
consultation
collaboration
coalition building
community organizing
advocacy
social marketing
policy development and enforcement
Population health
involves choices and value judgements in both construction and application
opportunity for healthcare systems, agencies, orgs to work together to improve healt outcome
population health vs. public health
Public health focuses on the health of entire communities through policies, education, and disease prevention, while population health uses data analysis to improve the health outcomes of specific subgroups within a larger population. Population also can be more focused on a particular group
Populations
often geogrpahic
groups like employees, ethnic groups, disabled ppl, prisoners
determinants of health like med care systems, social envio, physical envio have biologcial impact on individuals at pop level
population health research concerned about
interactions between them, prefer to refer to them as patterns
methods used by population health researchers have what characteristics
examin systematic differences in outcomes across pops
complex interactions among determinants
biological pathways linking determinants to population health outcomes
influence of different determinants over time and throughout the life cycle
population health considers
multiple levels of factors that drive health and how these levels intersect
Sweet and Kuzawa use two different explanatory models for population health
social
genetic
Population health: social
social forces like economics, psychosocial stress, institutional, interpersonal, discrimination account for health disparities
Population health: genetic
genetic variation in conventional racial clusters accounts for higher rates of health disparities