Term 3 Week 1
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
history specific for orthopedic patient
presenting complaint
onest, duration, progression
hx of trauma
previous hx of lameness
change over time/situation
recent changes in management
tx (rest, medication)
distant exam for orthopedic patient: you will look at?
posture
symmetry: conformation, BCS, Muscle, footsize/shape, localized swelling
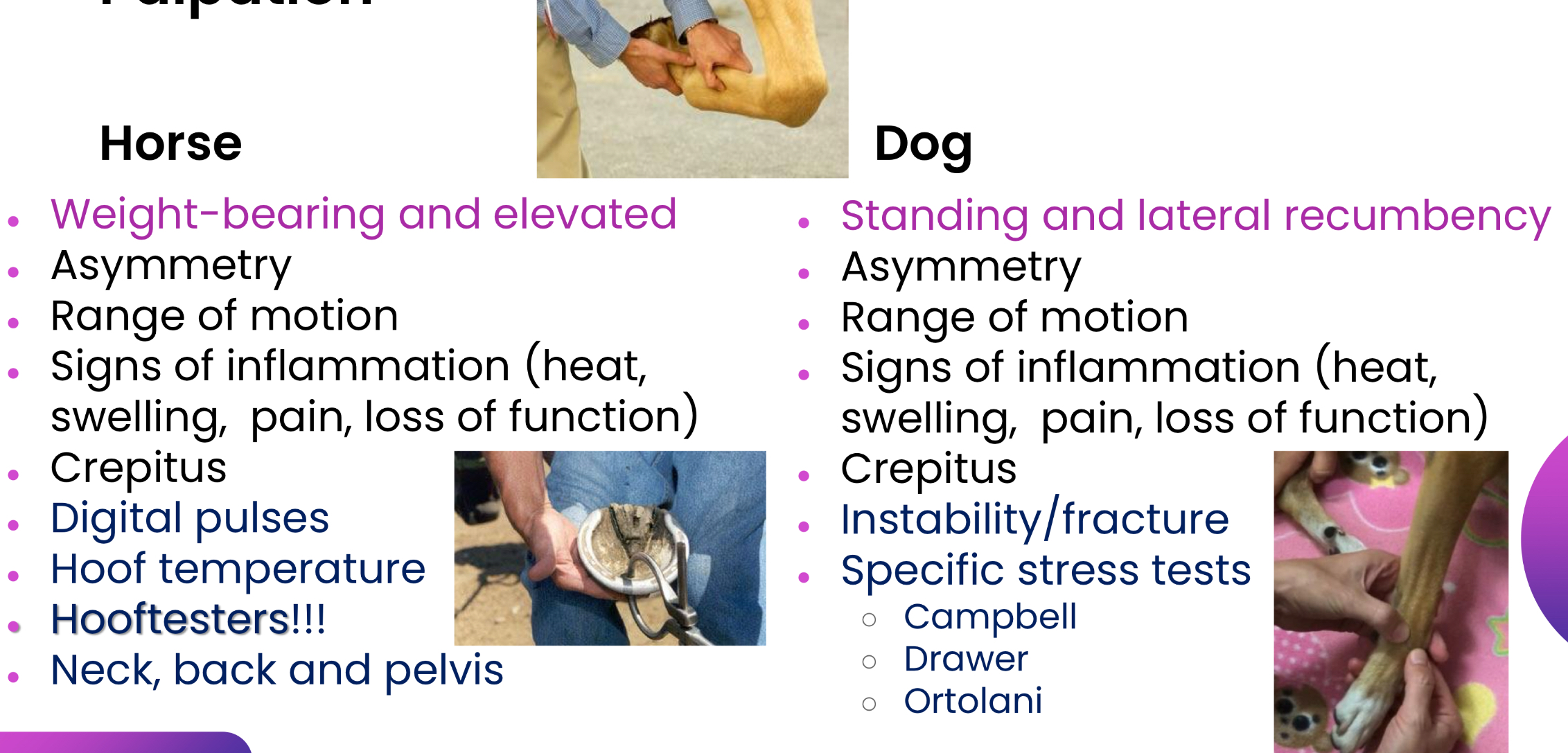
Palpation for orthopedic exam: horse and dog
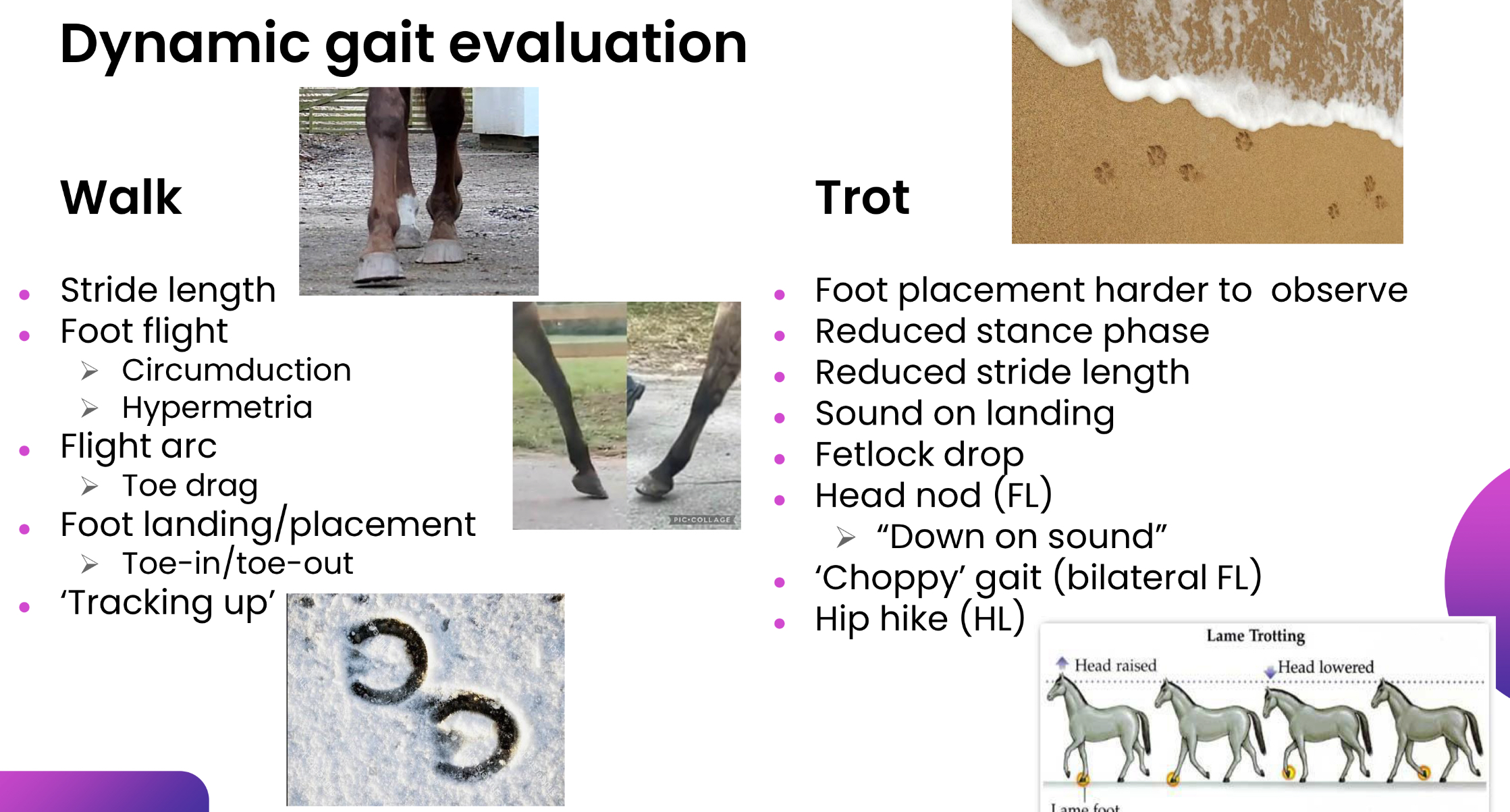
Dynamic gait evaluation for orthopedic exam
even, straight, firm surface free from distractions
horses temperament: Acepromazine (0.02-0.04 mg/kg) no analgesia or xylazine (0.1-0.3 mg/kg) local anaesthesia, can result in ataxia, analgesic
steady pace, straight, observe: going away, coming to, going past, turning, walk, trot, circles, over obstacles
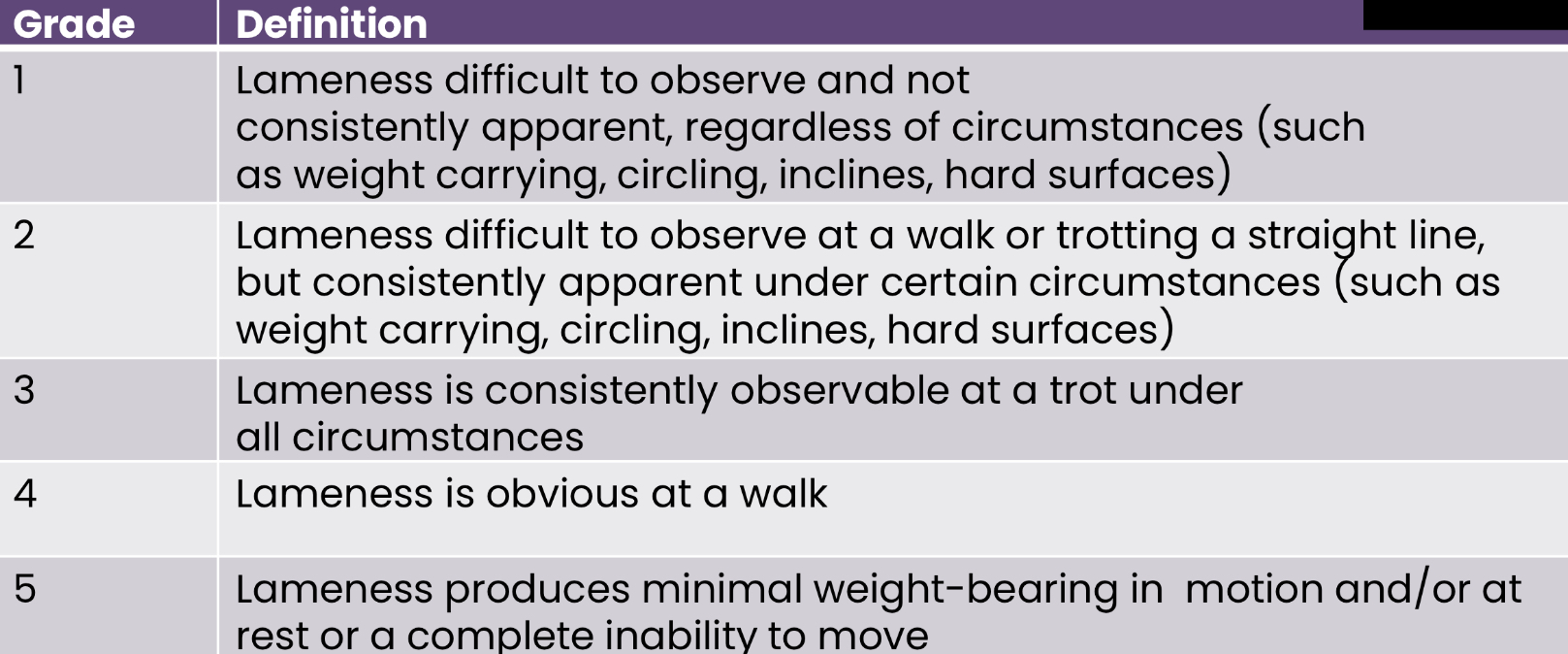
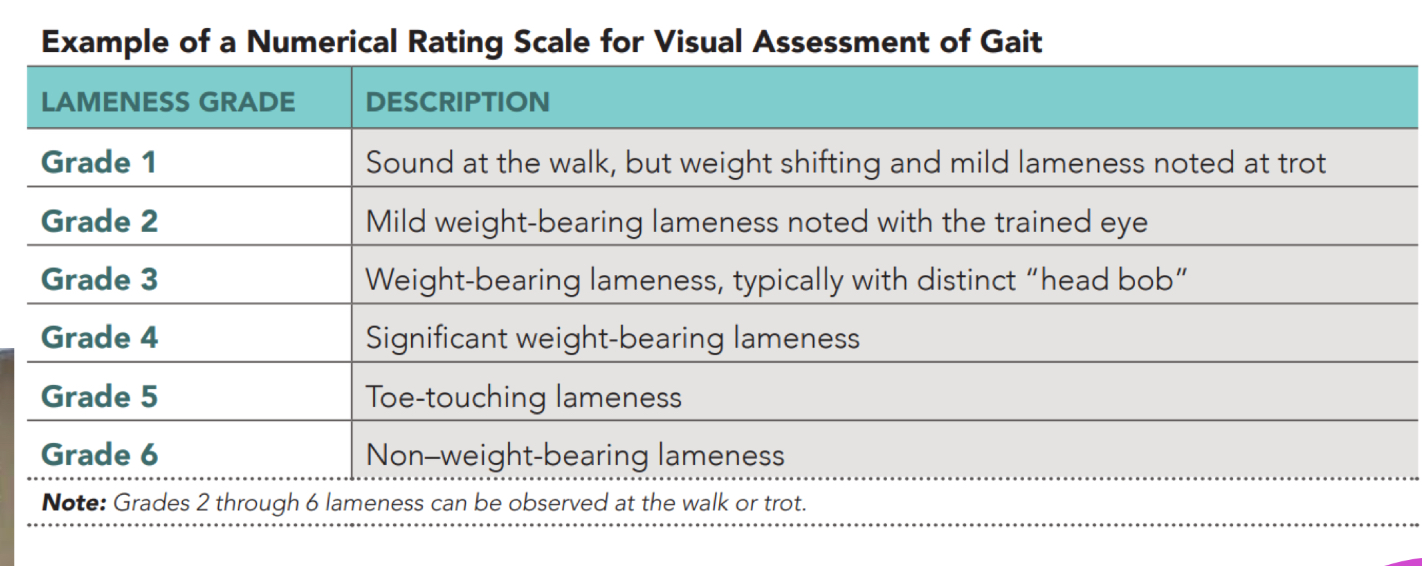
Dynamic gait evaluation grade scale: horse
Dynamic gait evaluation grade scale: dog
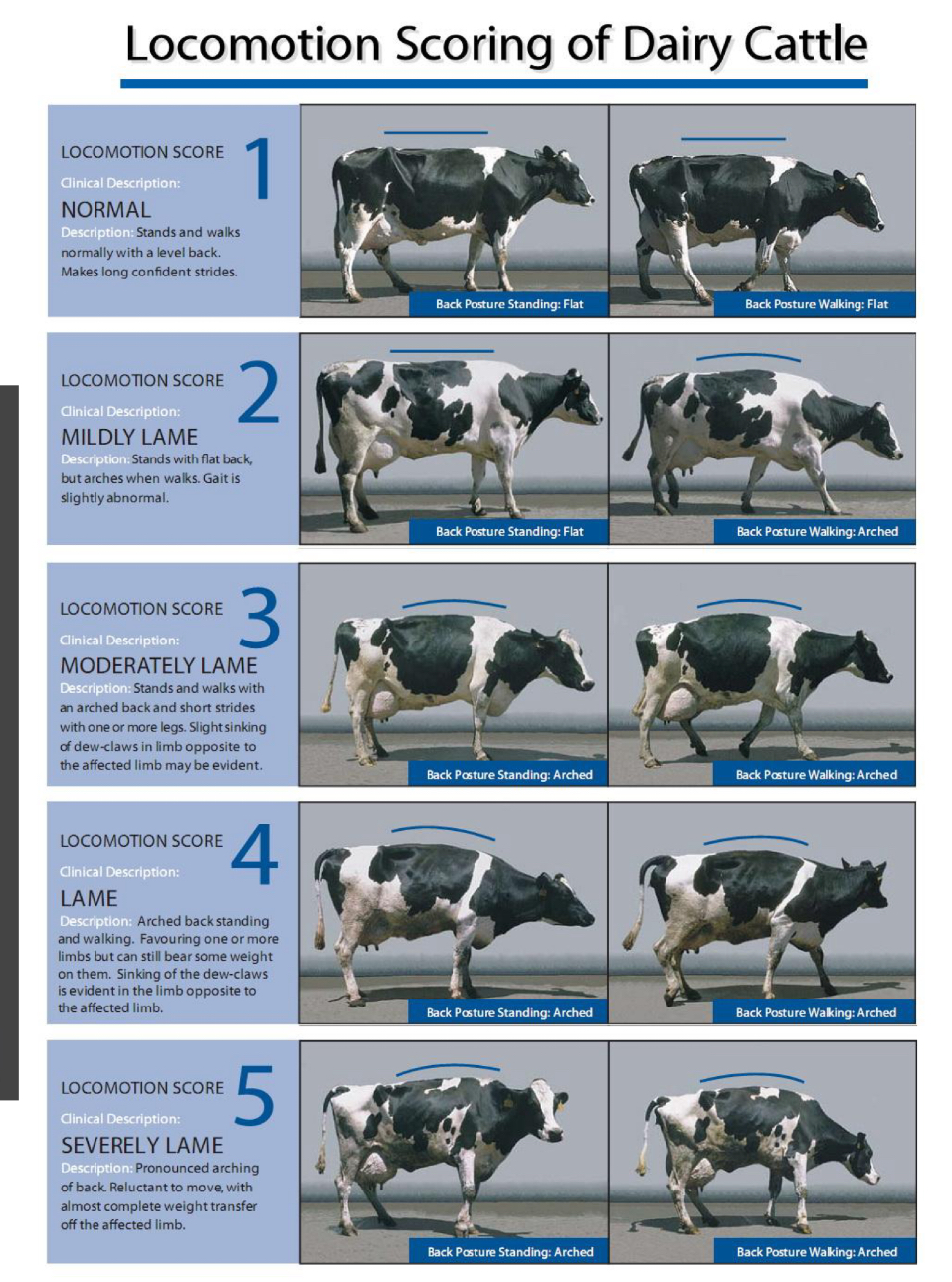
Dynamic gait evaluation grade scale: cattle
mechanical lameness
stringhalt
shivers
fibrotic myopathy
upward fixation of the patella
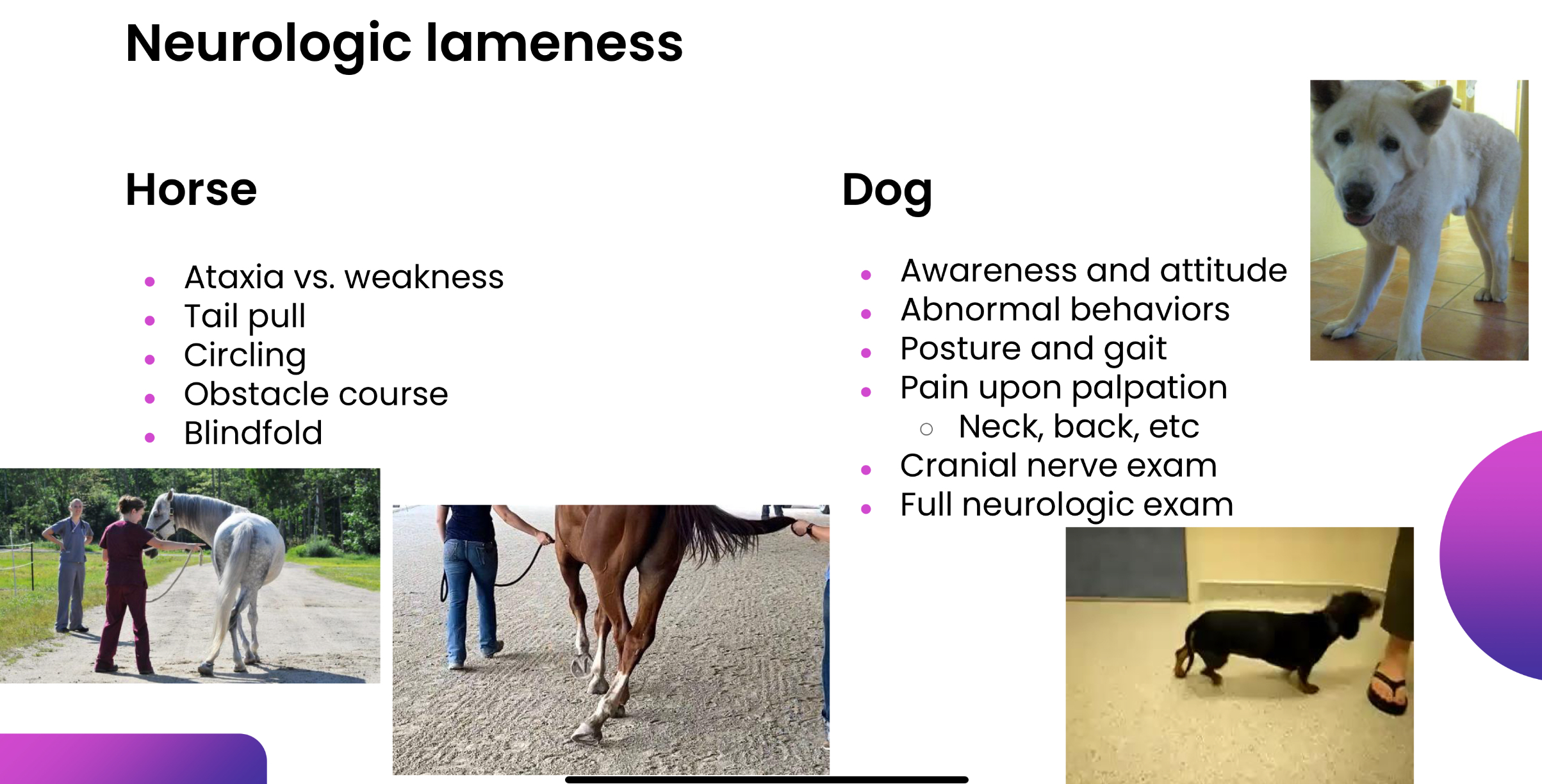
neurologic lameness
Exacerbation tests
ridden exercise: inexperienced rider exacerbate lameness, experienced rider can mask lameness, or help id subtle lameness
lunging: choppy gait/ bilateral lameness, different surfaces
flexion test: not specific, force amount/duration, lower limb, upper limb, full limb
other: wedge/extension, direct pressure: churchill test
Objective gait assessment
kinetics: direction/magnitude of force, hoof strain guages
kinematics: position in time and space, cameras, computers
lameness locator: high speed camera and treadmill, 3 wireless sensors transmit data to computer
AI- Sleip: live video, equine biomechanics data points, artificial neural networking
localization of pain horse vs dog:
Horse: negative localization = lameness is alleviated by eliminating the pain
→ diagnostic analgesia for horses: removes afferent pain impulses to brain, nerve blocks, synovial cavities (joint, tendon sheath, bursa)
dog: positive localization= pain is exacerbated by manipulation
Imaging for orthopedic issues:
x-ray: great for bone, but 2-D not good for soft tissue, radiation
ultrasound: great for soft tissues, serial monitoring possible, but 2-D, no bone or gas penetration, portable versions less sensitive
Nuclear scintigraphy: Id early physiological changes, great for bone, But 2-D, radiation, non specific
computer tomography: 3-D, eliminates superimposition, great for bone and okay with soft tissue, But radiation, only lower limbs and head/neck, artefacts around metal implants, expensive
magnetic resonance imaging: 2-3D, great for all tissues, but only lower limbs, head/neck, artefacts
arthoscopy/tenoscopy: simultaneous diagnosis and tx of conditions, direct visualization of damage, BUT general anasthetic, expensive, access some areas difficult
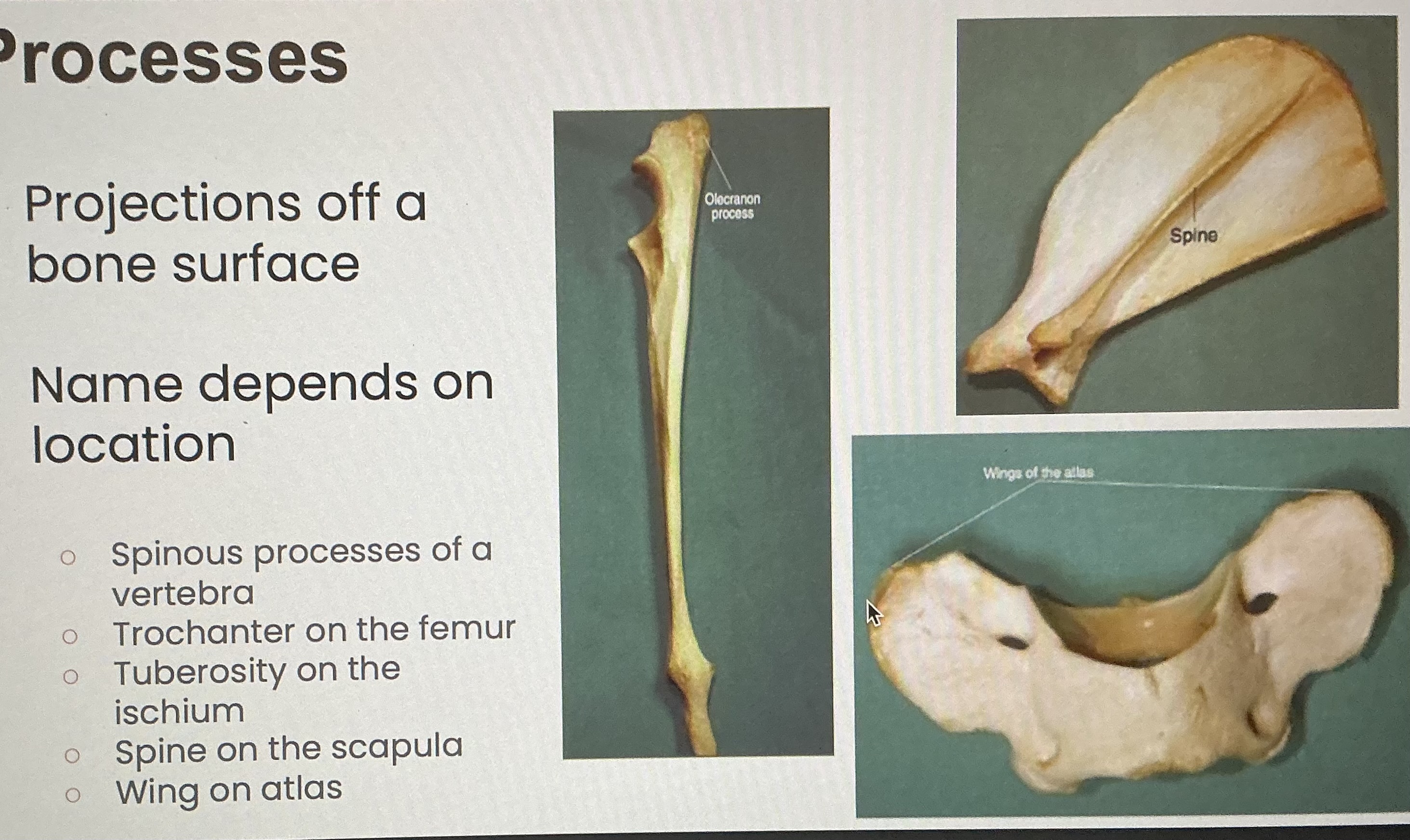
Tuberosity/ trochanter/ tubercle
Protuberance on bones, which are usually from the attachment of muscles
Trochlea
Bony structures through or over which tendons pass; usually grooves in the bone and allow tendon to act as pulleys
Condyle
A rounded production on a bone, usually for articulation with another bone
Epicondyle
A projection of bone on the lateral edge above its condyle
Foramen (pl. formina)
An opening or passage into or through a bone (To allow the passage of blood vessels and nerves)
Fossa
A hollow or depressed area on a bone
Head
A rounded surface of articulation, crucial for joint movement and articulation
Neck
The narrower or constricted region connecting the head to the shaft/ diaphysis of the bone
Shaft/diaphysis
Long, tubelike mid portion of a long bone
Tendon
Connects muscle to bone
Ligament
Connects one bone to another bone
Girdle
Bone that is broad, flat and joins the limbs to the spine
Four limbs consist of:
Girdle, one long upper bone, two long lower bones, several smaller bones in the wrist or ankle and five digits
Functions of the skeletal system
Support: internal scaffold
Locomotion: attachment for muscles
Protection: protects major organs
Hemopoiesis: hemopoietic tissue within the bone marrow manufactures blood cells
Bone shapes
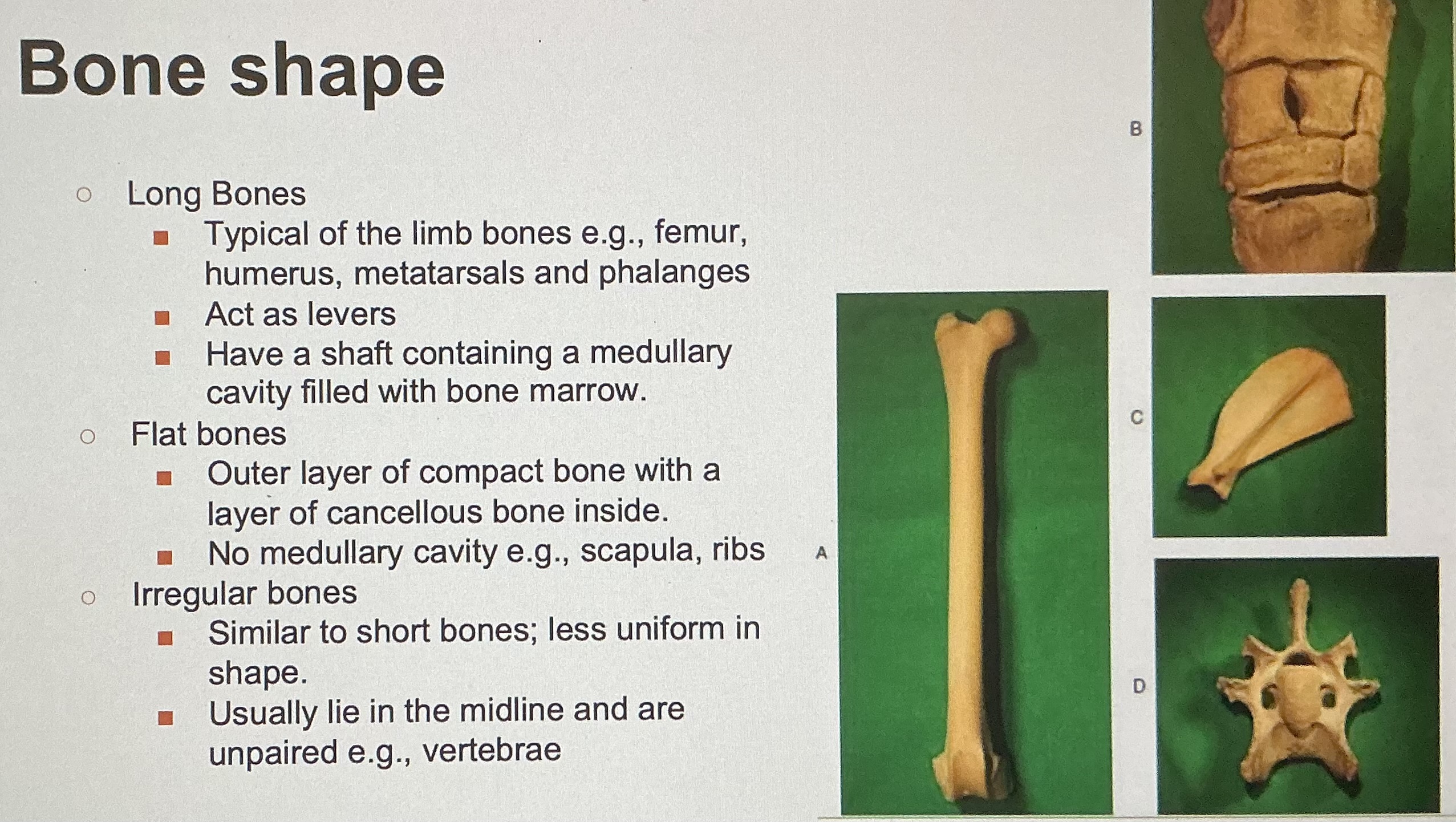
Atypical bones
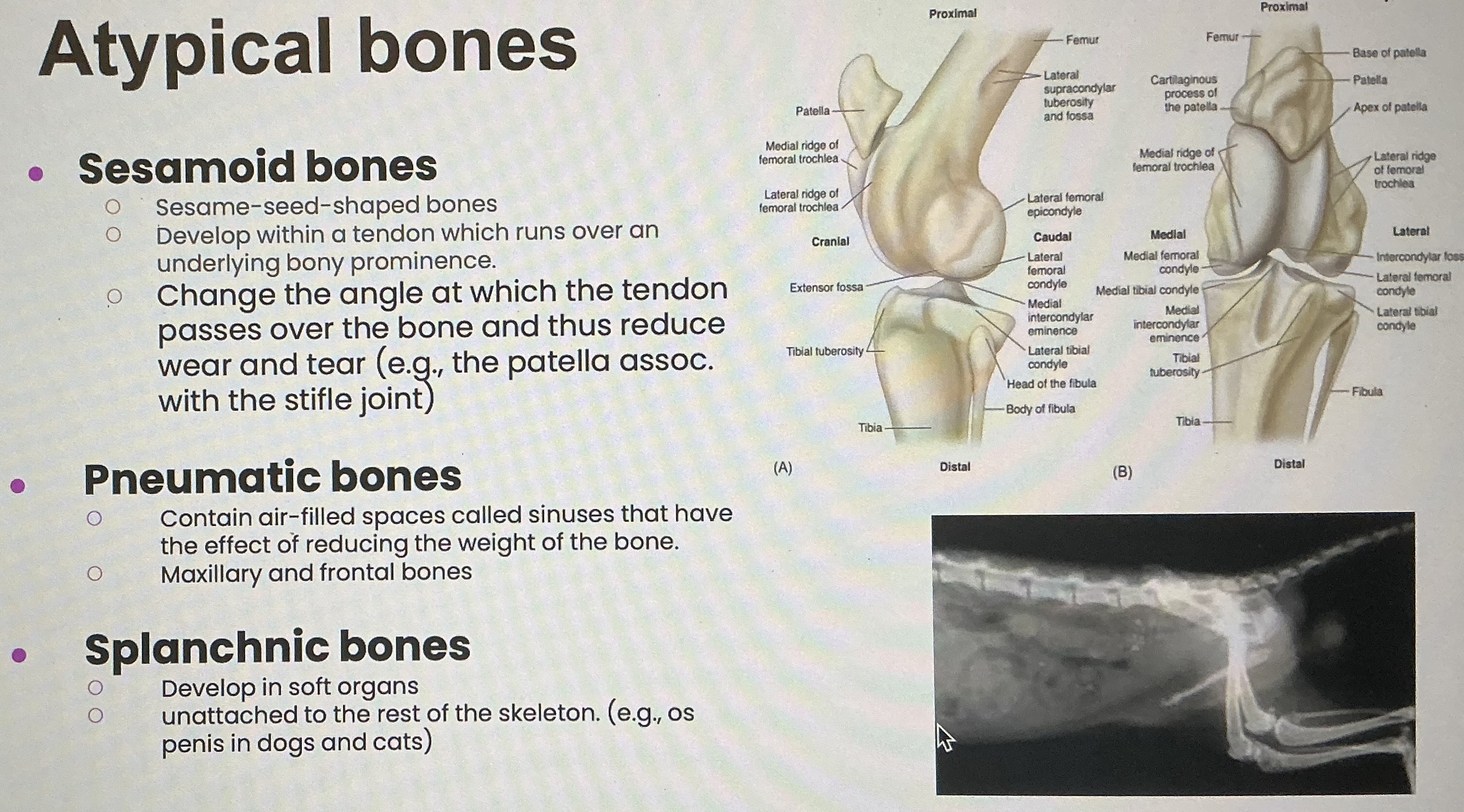
Articulate surfaces: condyle, head, facet
Condyle: large round articulate surface
Head: spherical articulation surface on the proximal end of a long bone
Facet: flat articulate surface
Bone processes
Projections off a bone surface
Foramen vs fossa
Foramen= hole in bone, may contain blood vessels, nerves
Fossa= depressed area on the surface of a bone
3 Divisions of the skeletal system
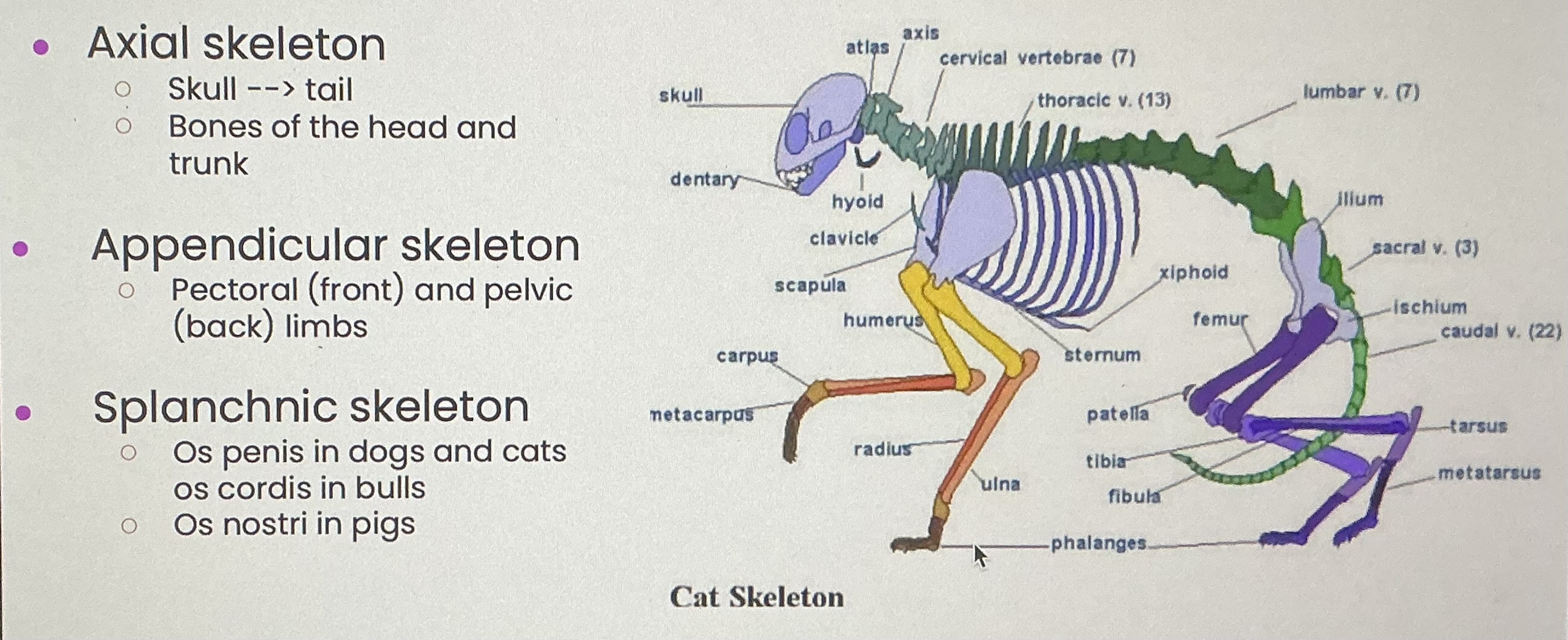
Axial skeleton bones
Skull, vertebrae, ribs, sternum, hyoid
Skull
Protects brain, provides attachment for facial muscles, usually 37/38 separate bones, contain sutures (joints between skull bones), the mandible is connected to the rest of the skull by a synovial joint
Hyoid apparatus
Lies in mandibular space, suspends the larynx and tongue from the skull
Vertebrae
Consists of a body , an arch, and processes
Spinous process, transverse process, articular process
Intervertebral disc= cartilage that separates adjacent vertebrae
Cervical, thoracic, lumbar, sacral, coccygeal
Ribs
Elongated flat curved bones
Dorsal head of the ribs articulate with thoracic vertebrae
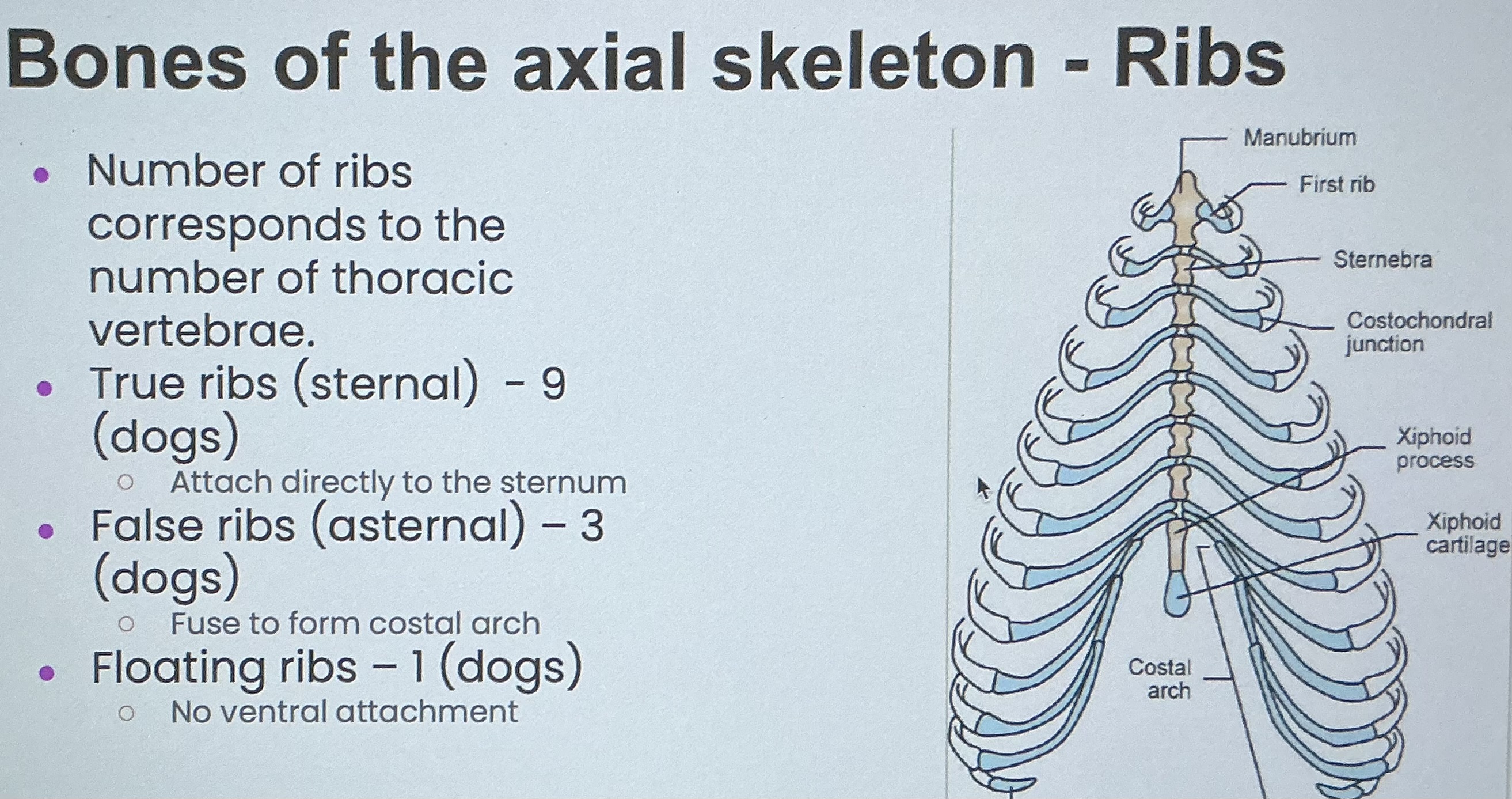
Sternum
Osseocartilaginous bone
Medially-placed segmented bone forming the floor of the thorax
Consists of 7 segments in bovine and equine, 8 in dogs and cats, 6 in pigs and rabbits
Siphons process- most caudal sterner a
Connected by intervening cartilages
Bones of the appendicular skeleton
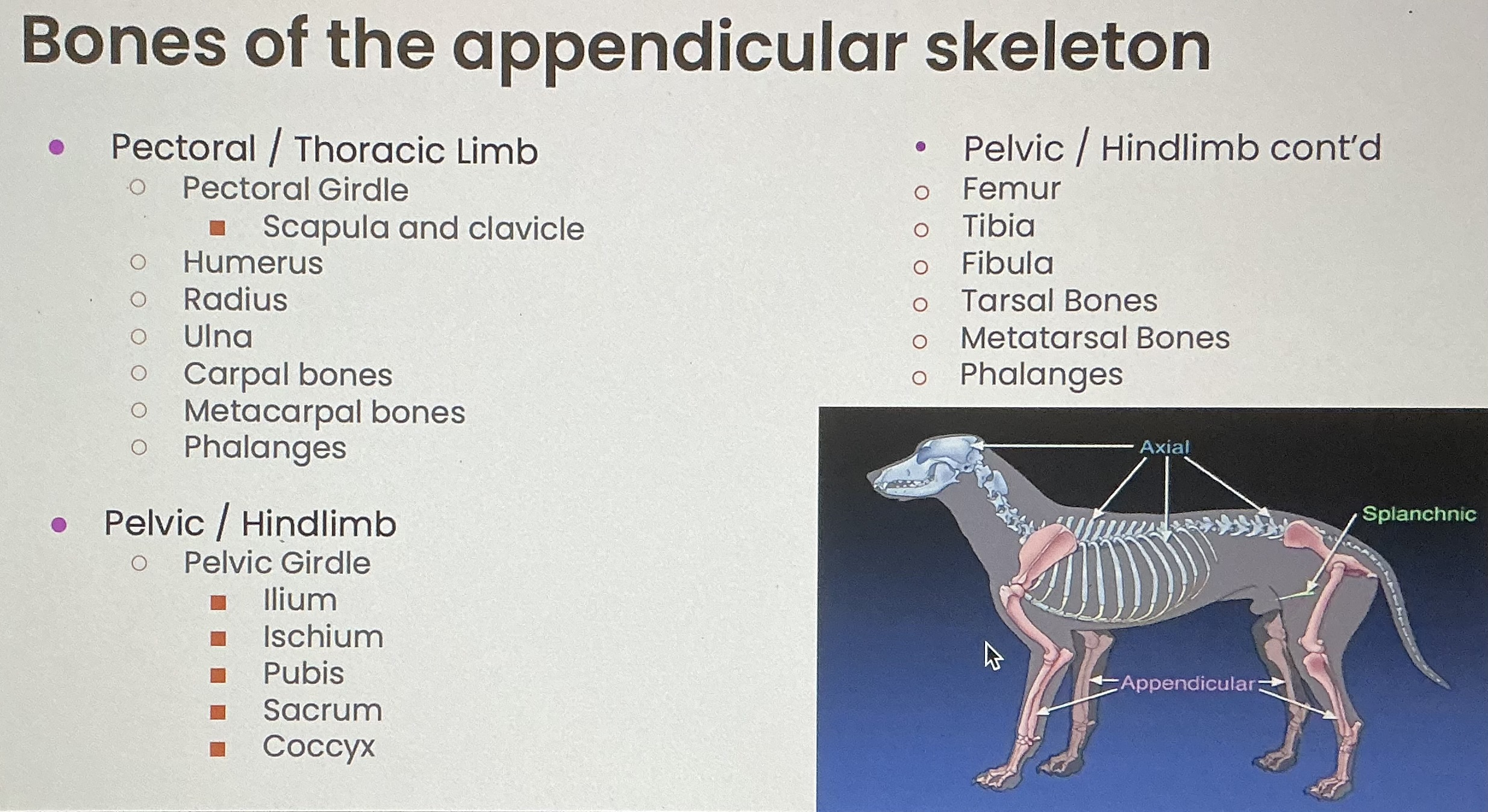
Pectoral/ Thoracic limb
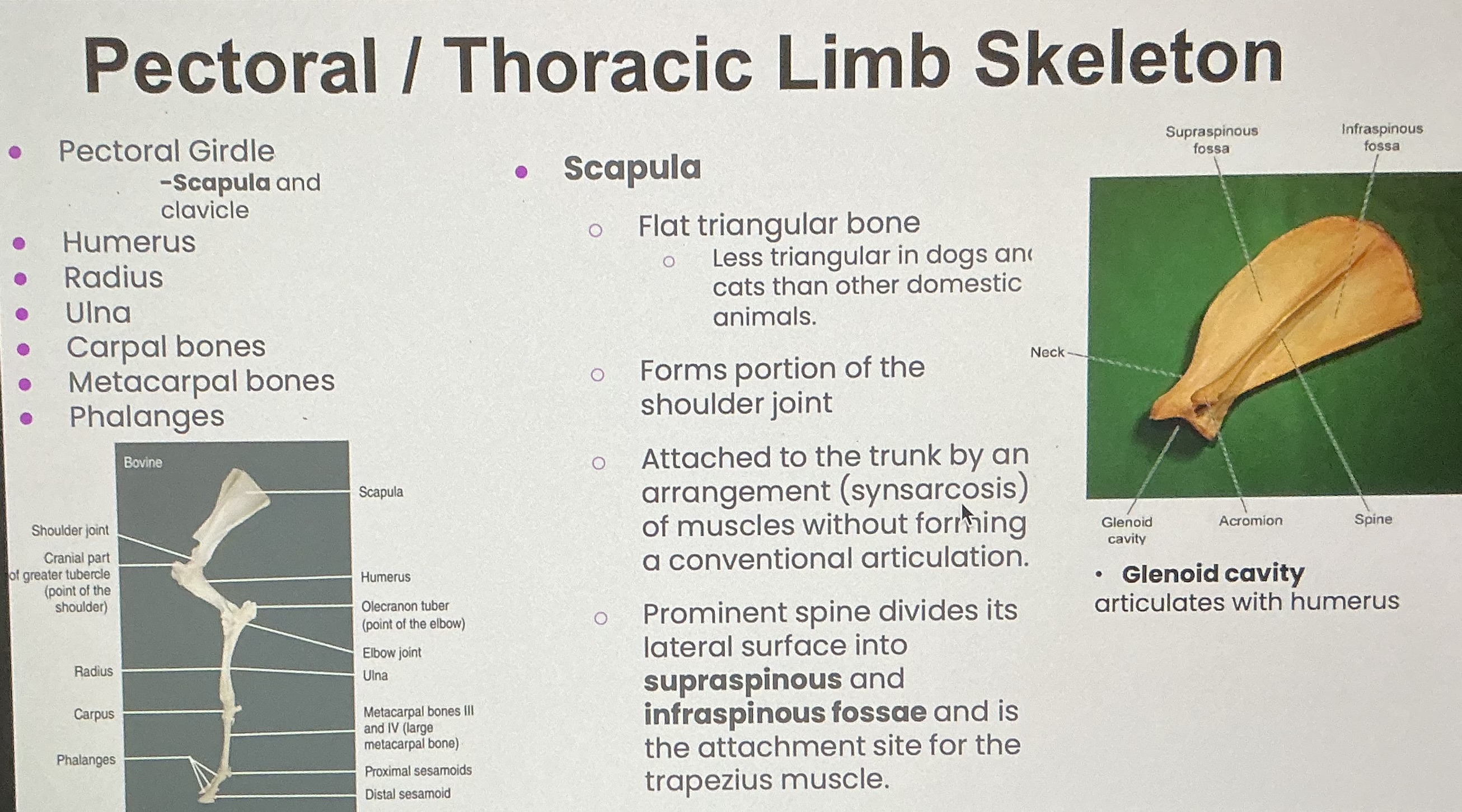
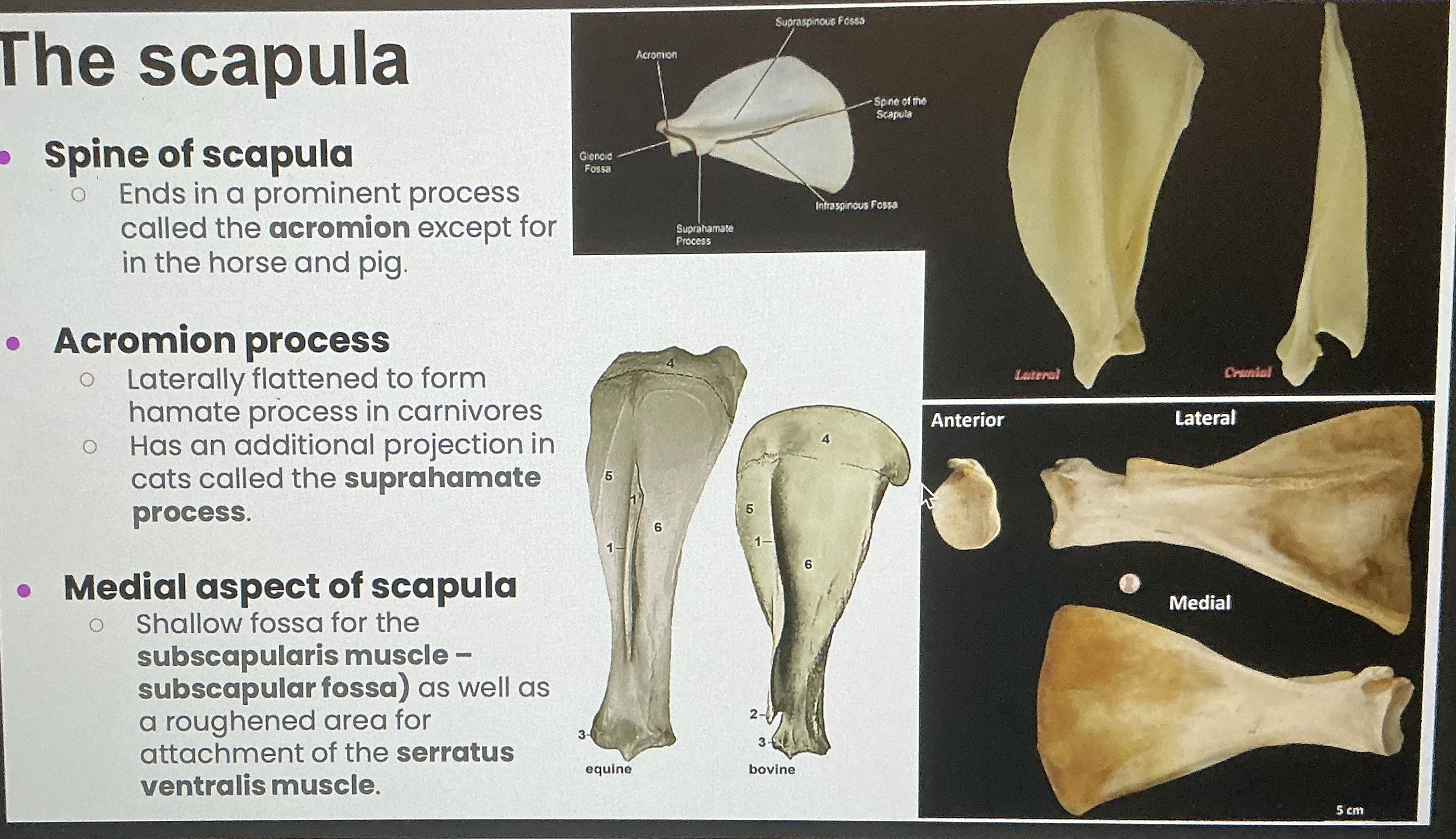
The scapula
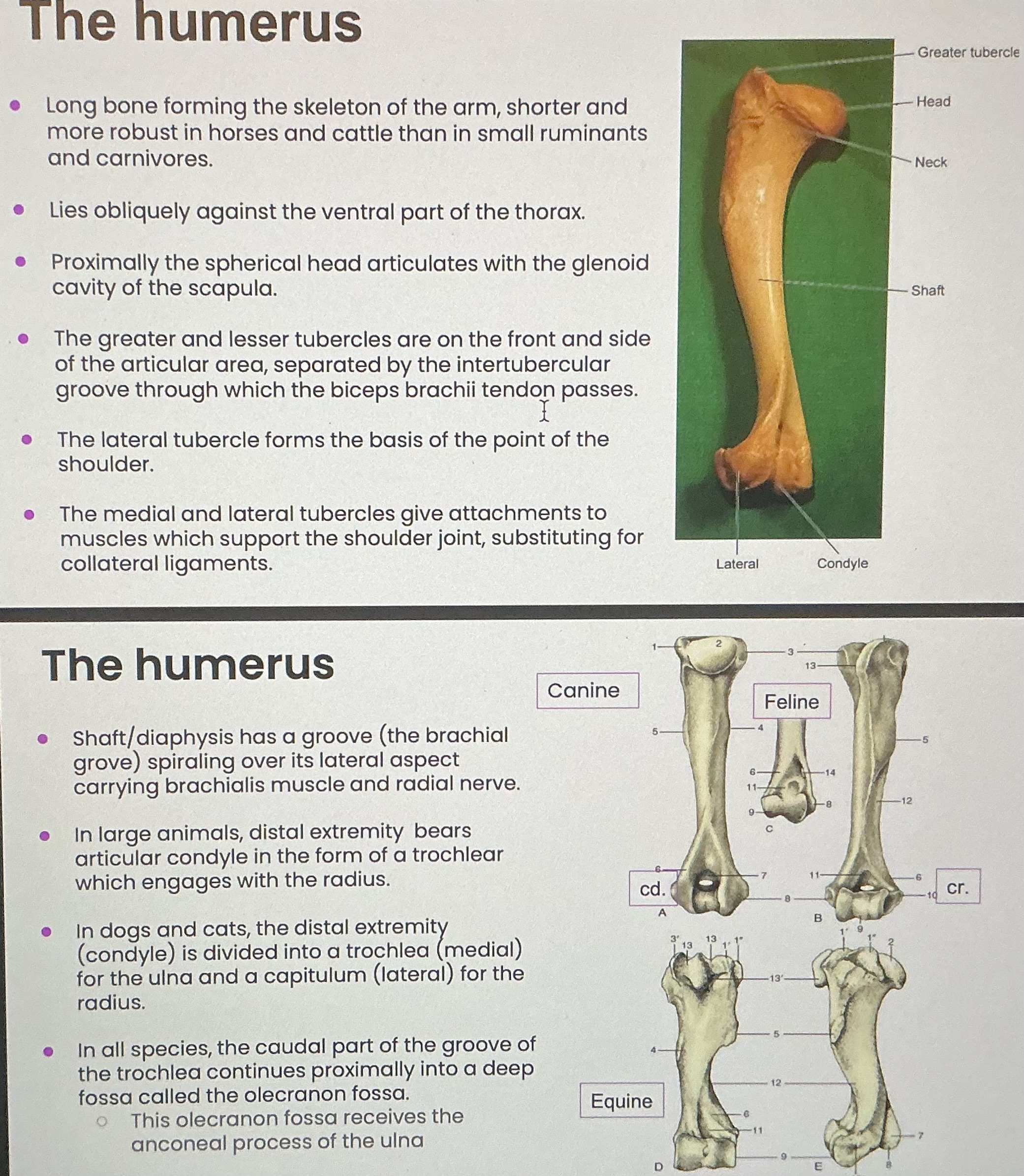
The humerus
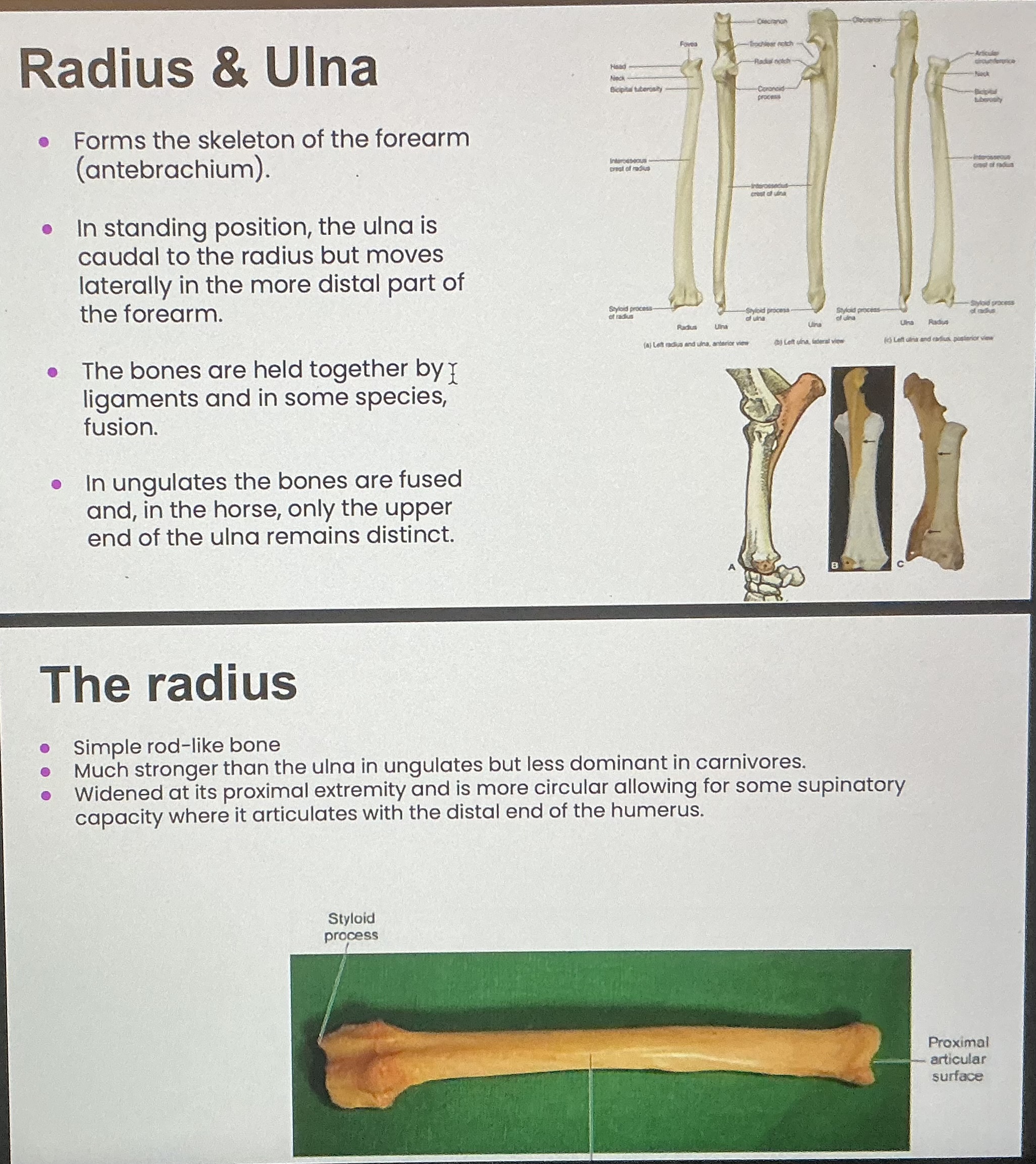
Radius and ulna
Carpus/carpal joint
Wrist, composed of two carpal bones
Proximal row bones are named, distal row are numbered medial to lateral
muscles of the vertebral column
Epaxial muscles: muscles of the back, dorsal to the transverse process of the vertebrae which form a continuous column throughout most of the vertebral column. Potential relevance in spinal surgery. • Receives nerve supply from dorsal branches of the spinal nerves
Hypaxial muscles: muscles ventral to the transverse process of the vertebrae. • Receives nerve supply from the ventral branches of the spinal nerves.
Function of the muscles: flex, extend, abduct, adduct, and rotate the backbone.
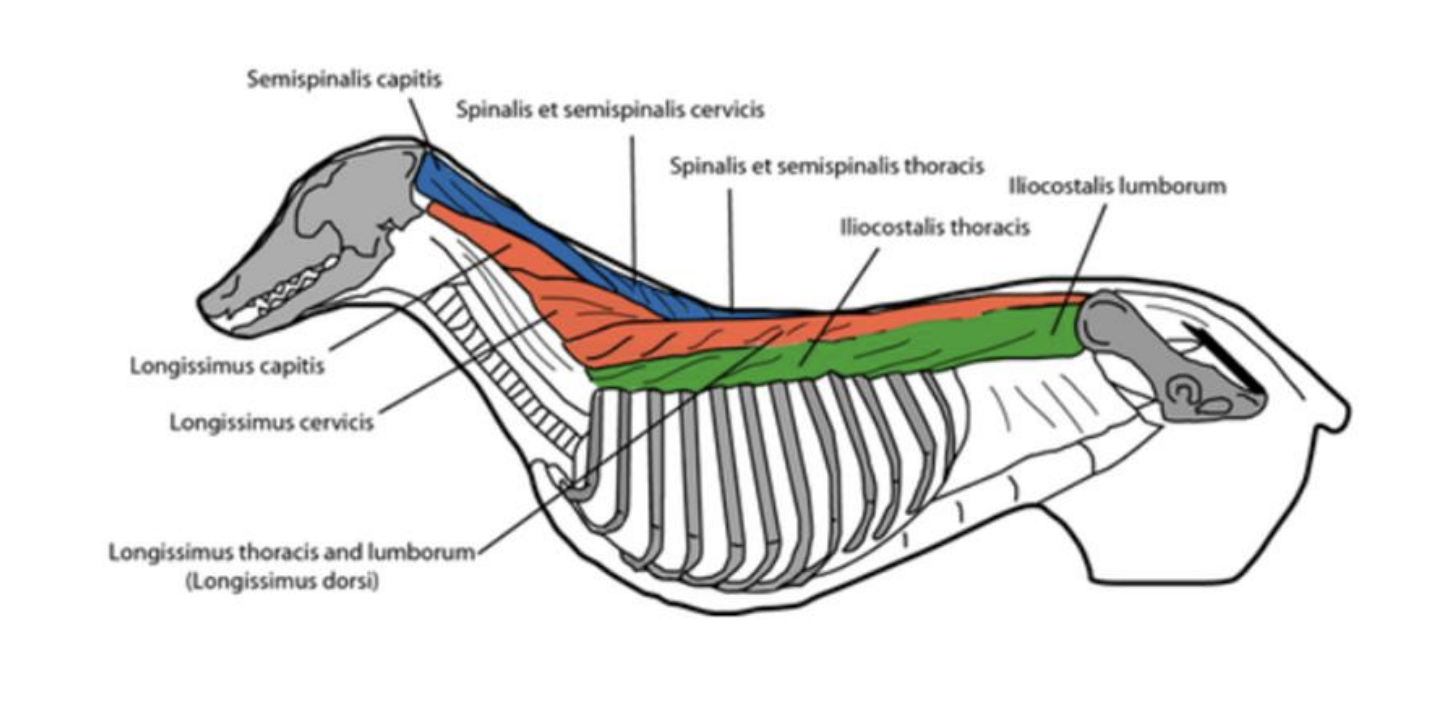
epaxial spinal musculature parallell systems
extend between the skull and the ilium
liicostalis system: located laterally consists of lumbar and thoracis bundles of overlapping fibers between the lumbar and cervical vertebrae action: lateral flexion of the trunk (green)
longissimus system: divides from the ileum to the head into thoracolumbar, cervical, and capital muscle fascicles action: extensors of the back, also assist in expiration (orange)
transverseospinalis system: most medial to the spinous process of the vertebral column, extends from the sacrum to the head, fascicles are named according to location, commonly reflected in a laminectomy procedure action: stabilize the thoracic region of the column raise head and neck (blue)
function: extend the vertebral column, produce unilateral movement of the trunk
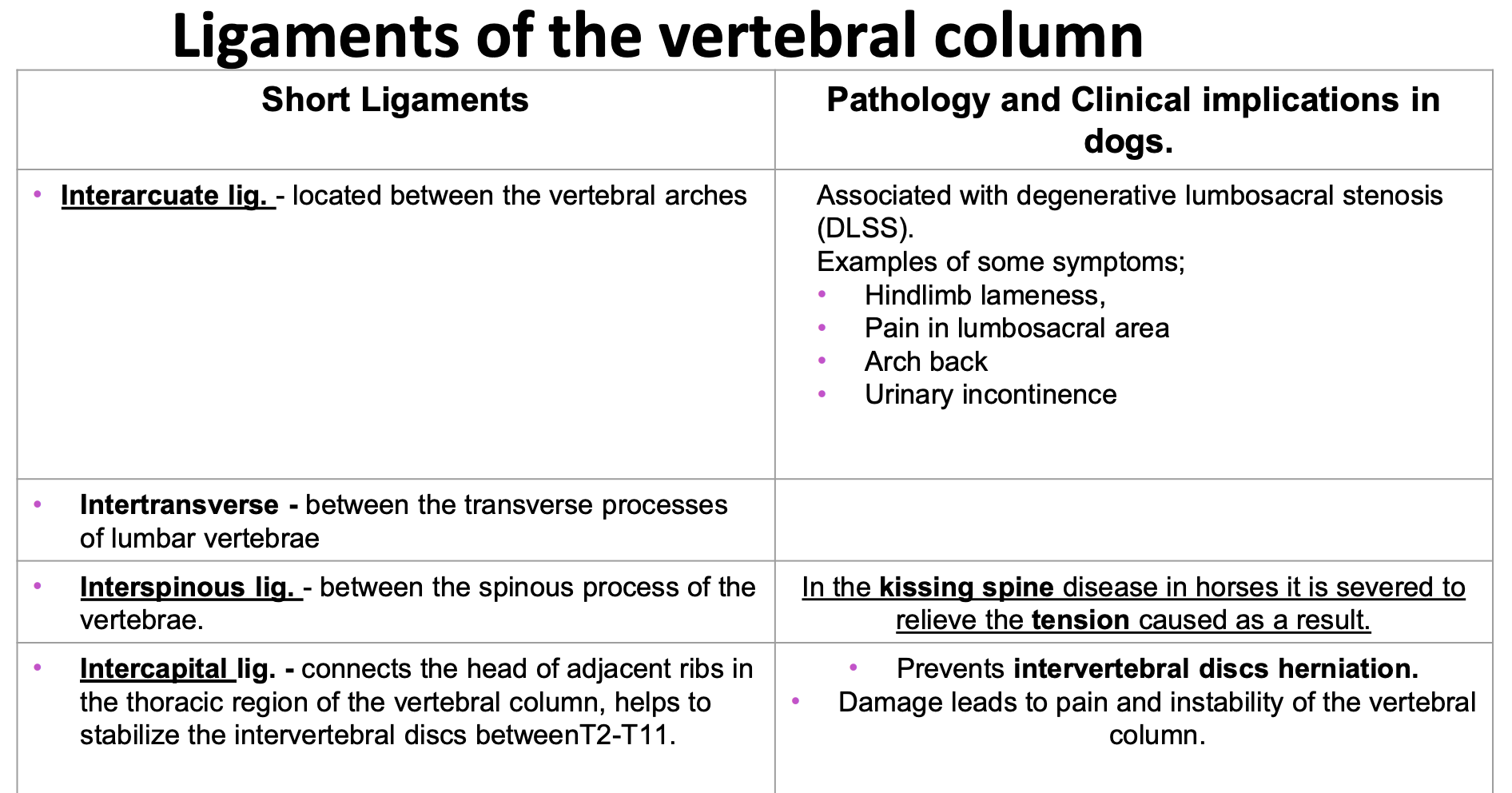
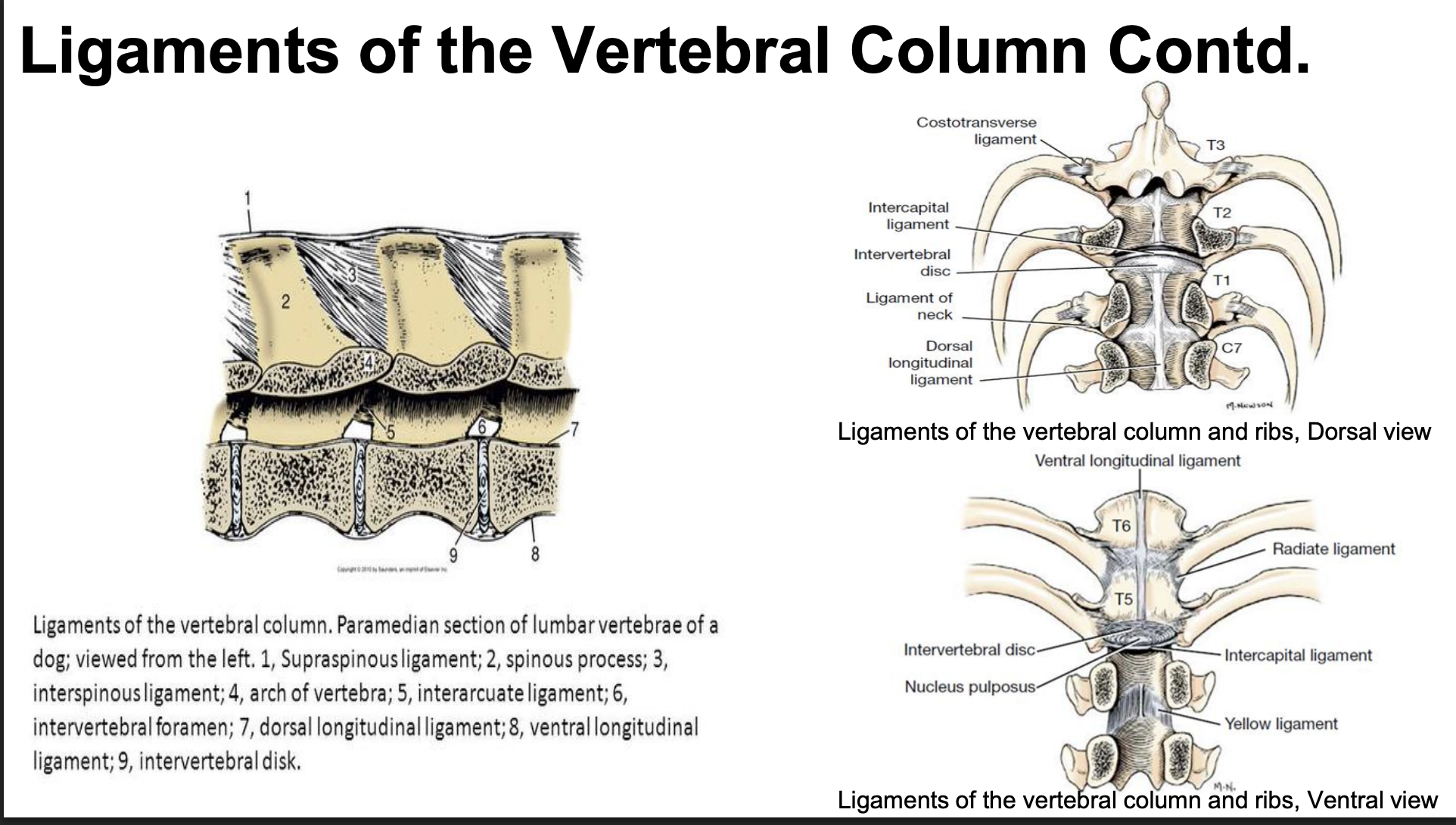
ligaments of the vertebral column: short
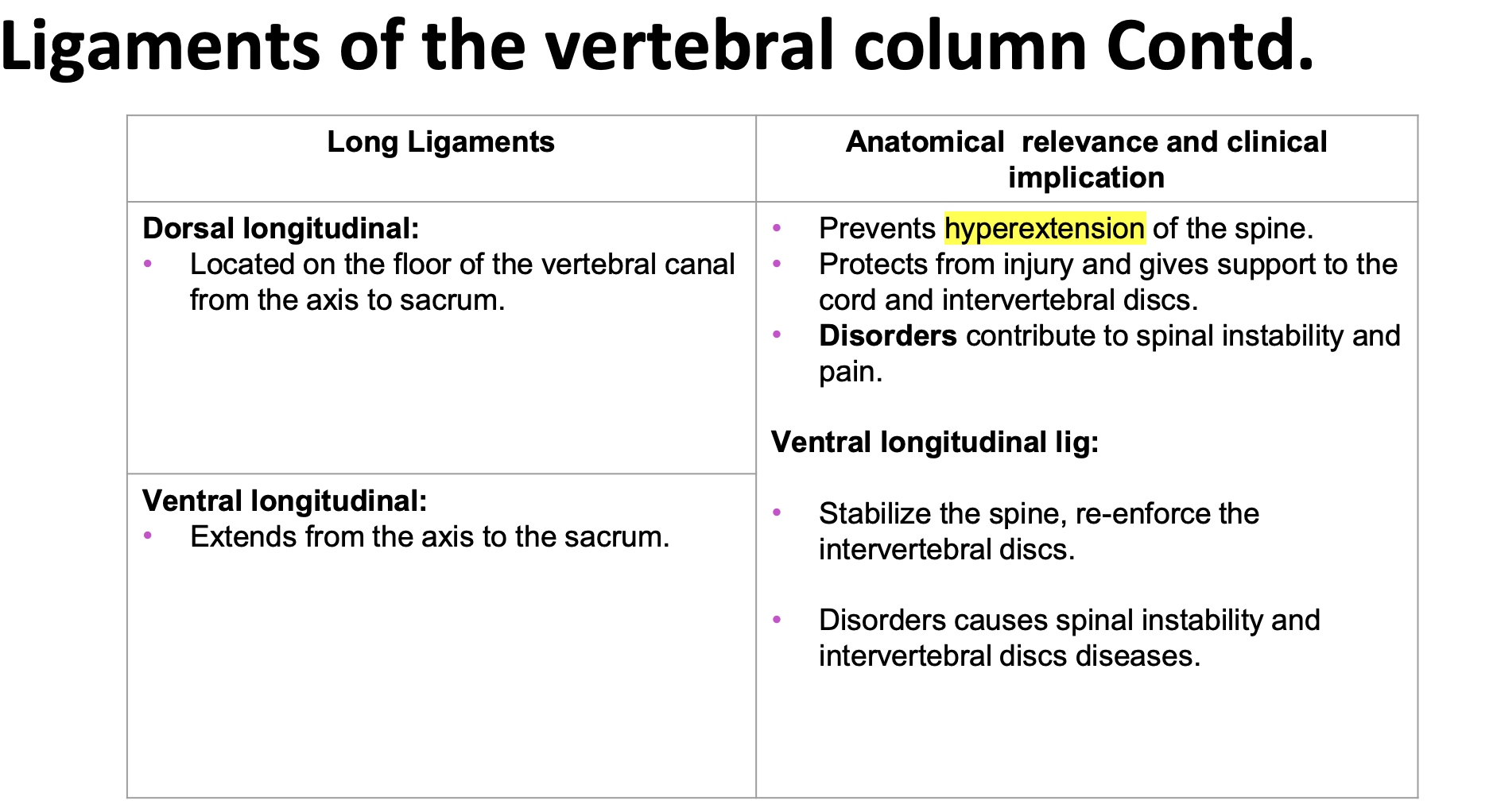
ligaments of the vertebral column: long
ligaments of the vertebral column: nuchal ligament
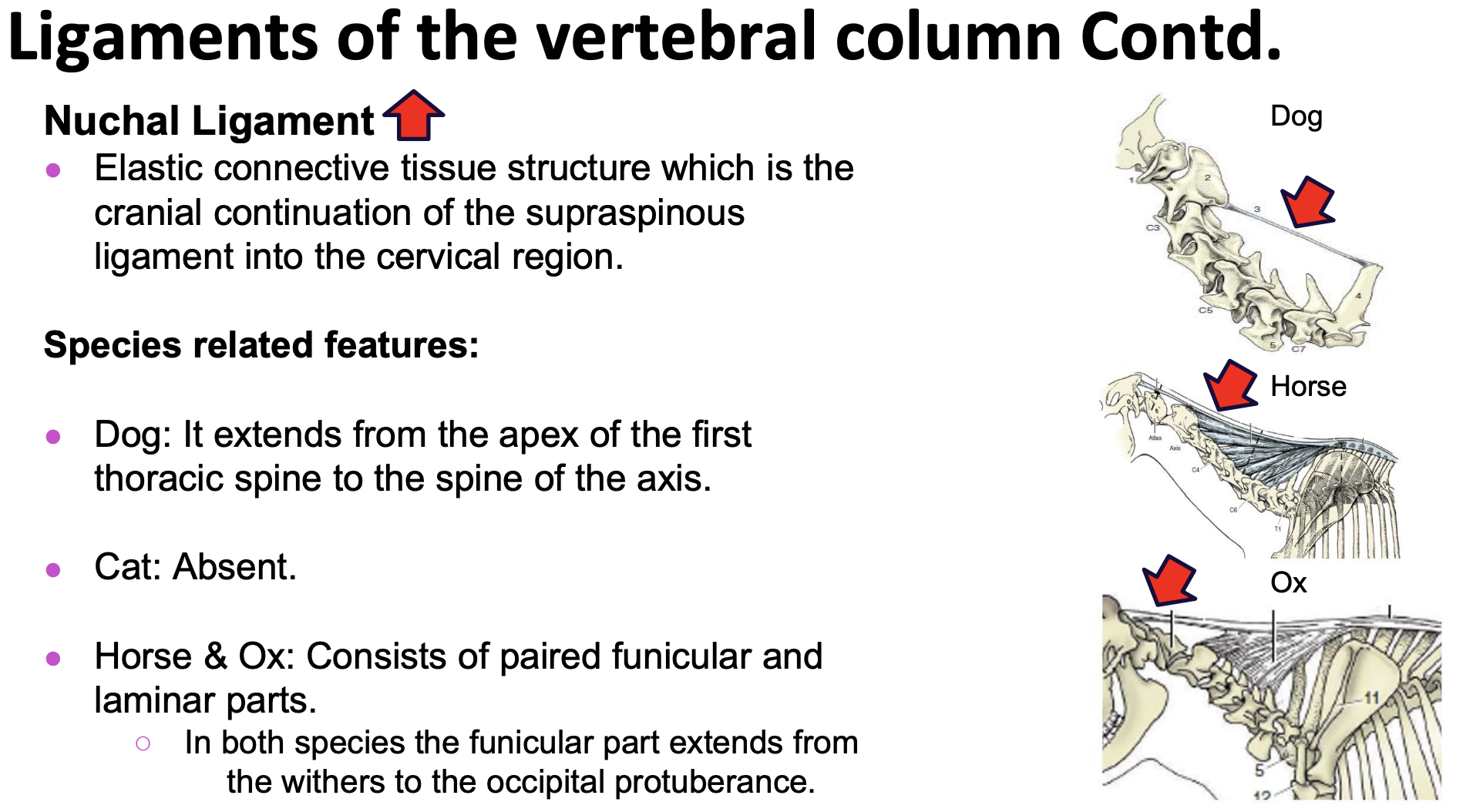
functions: supports the weight of the head, relieves load from the head and neck when the head is held high
in ungulates: provides support to the atlantoaxial and atlantooccipital joints, heavy head, its elasticity allows for sufficient flexibly so that the head can be raised and lowered when grazing and running
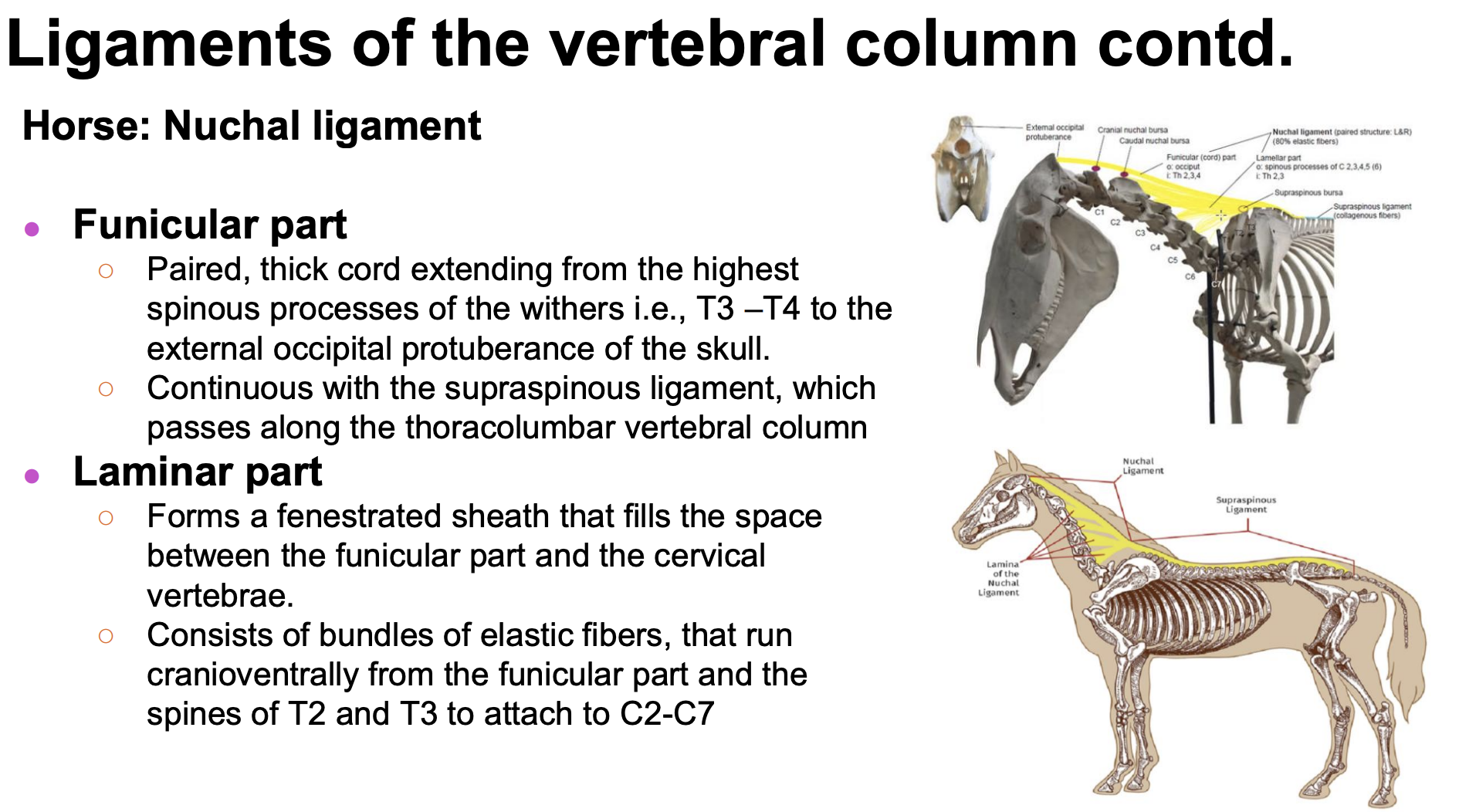
Horse nuchal ligament
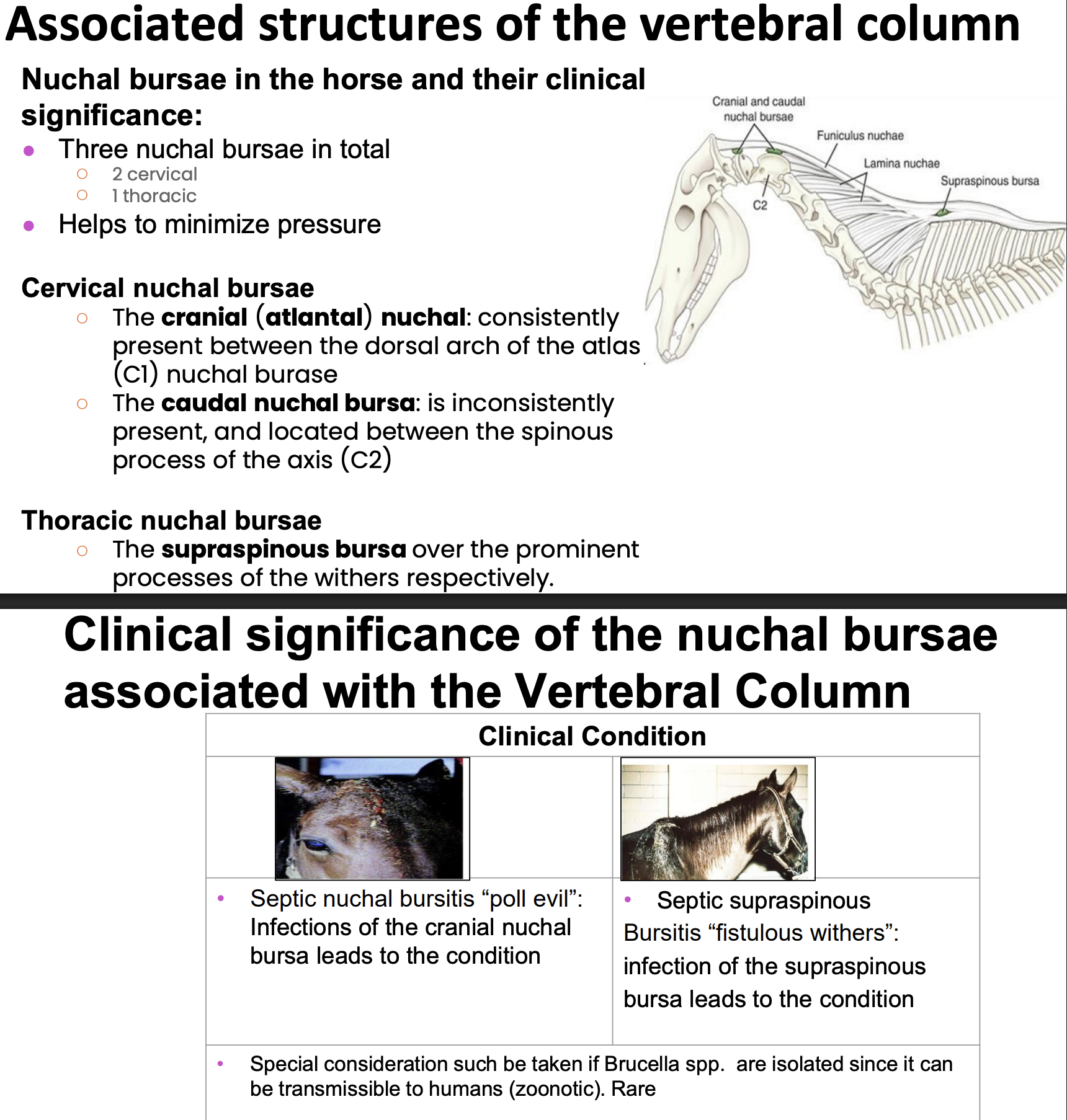
Nuchal bursae in the horse
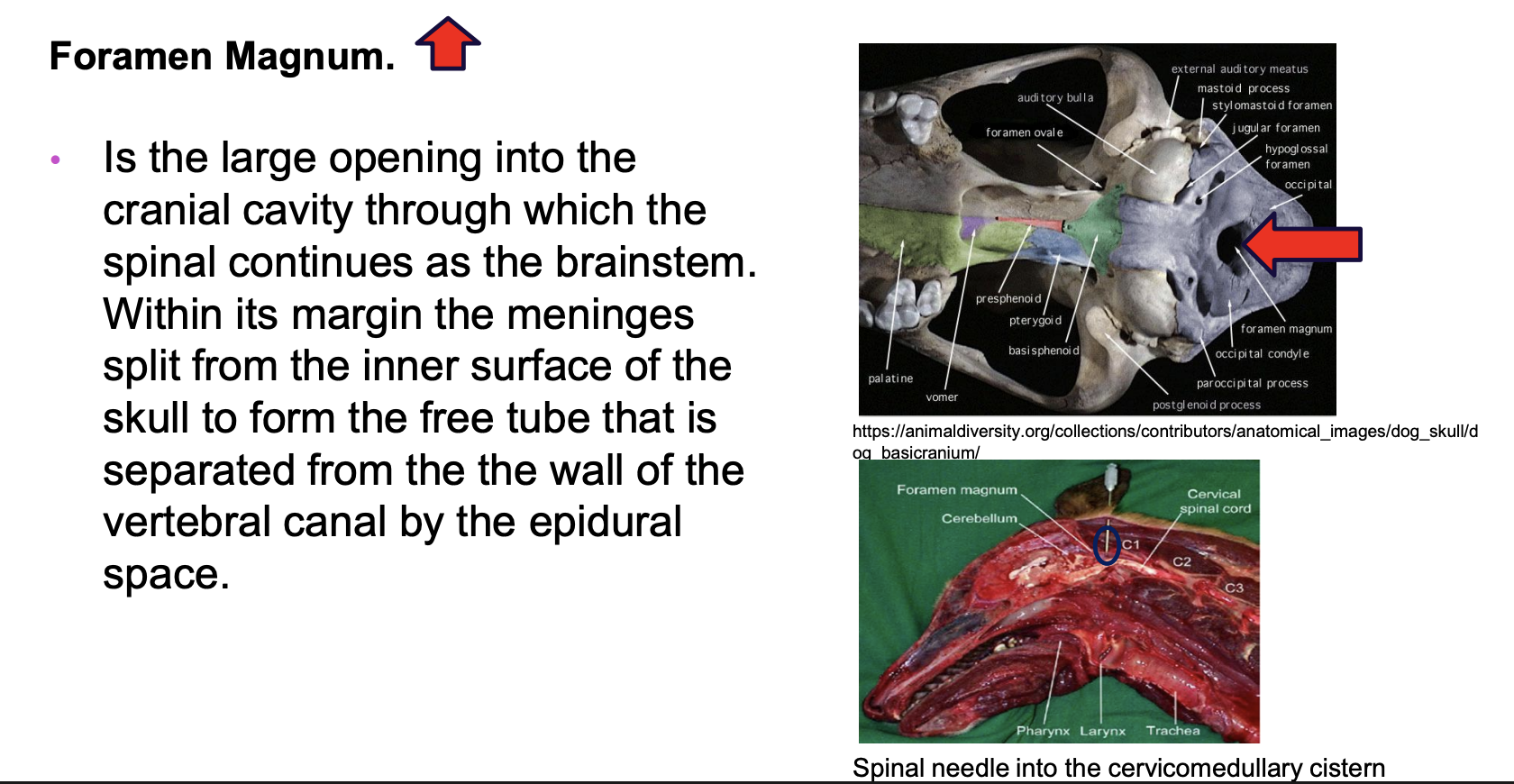
foramen magnum
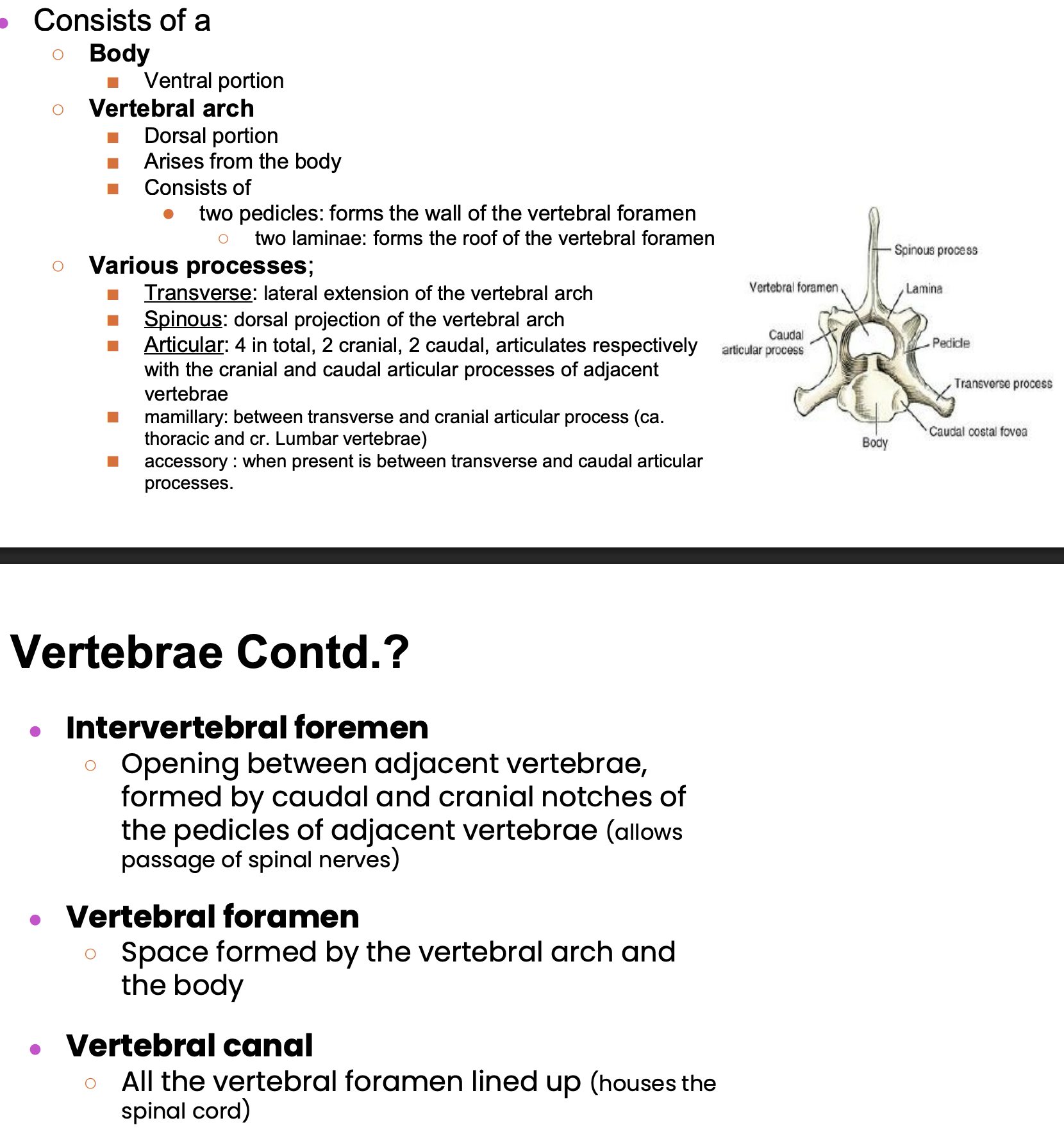
vertebrae consists of:
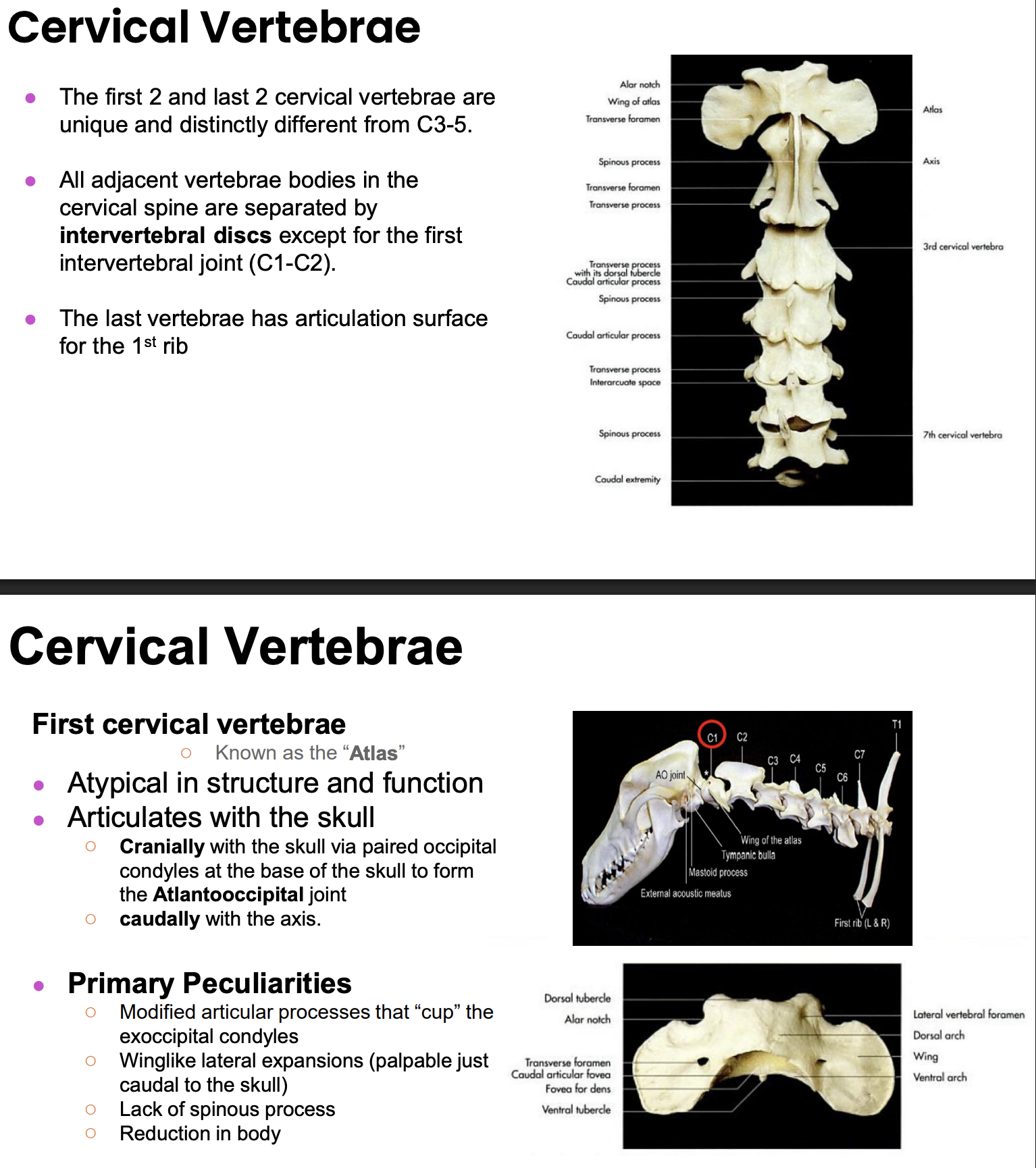
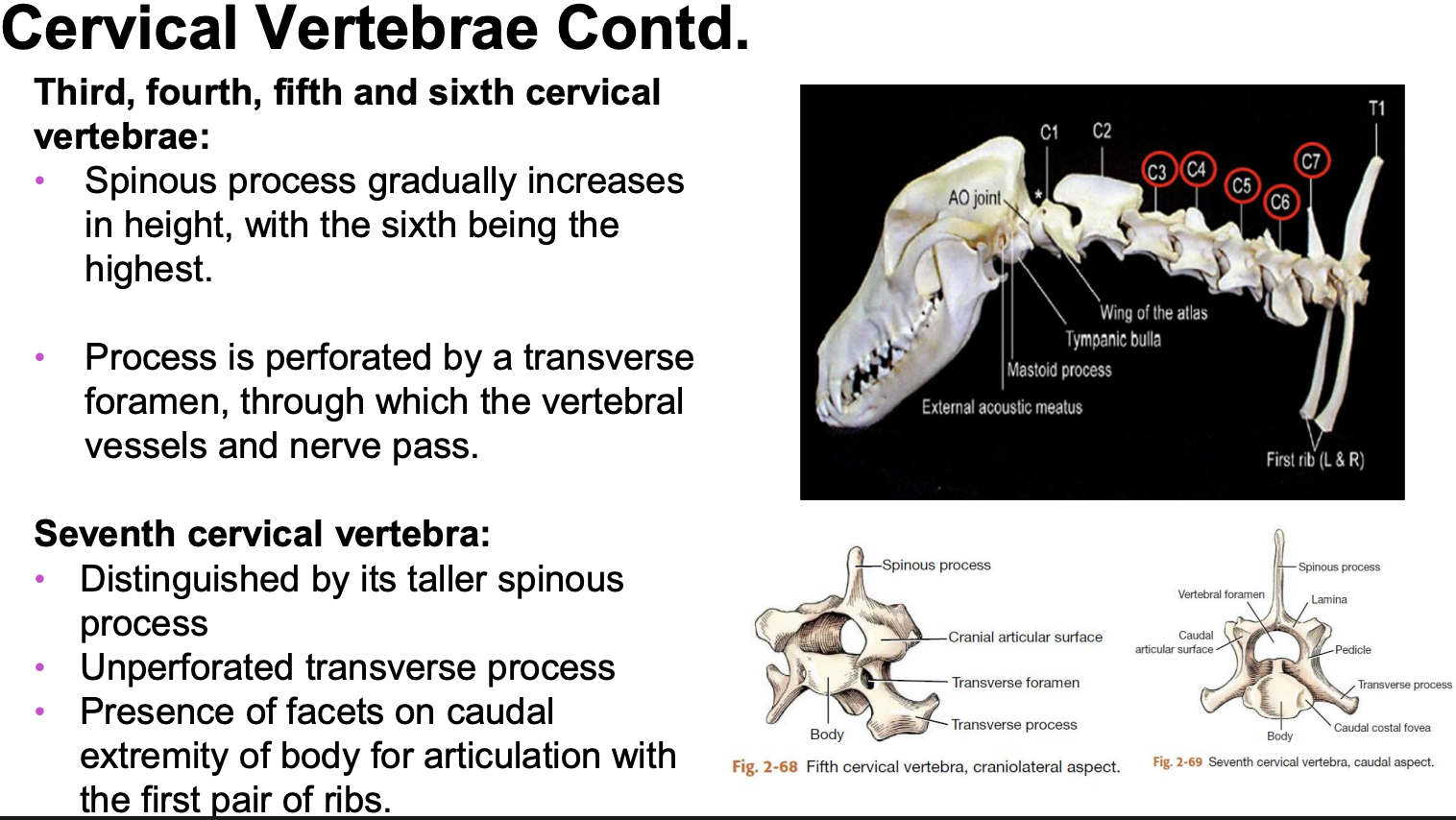
organization of the cervical vertebrae: overview and c1 info
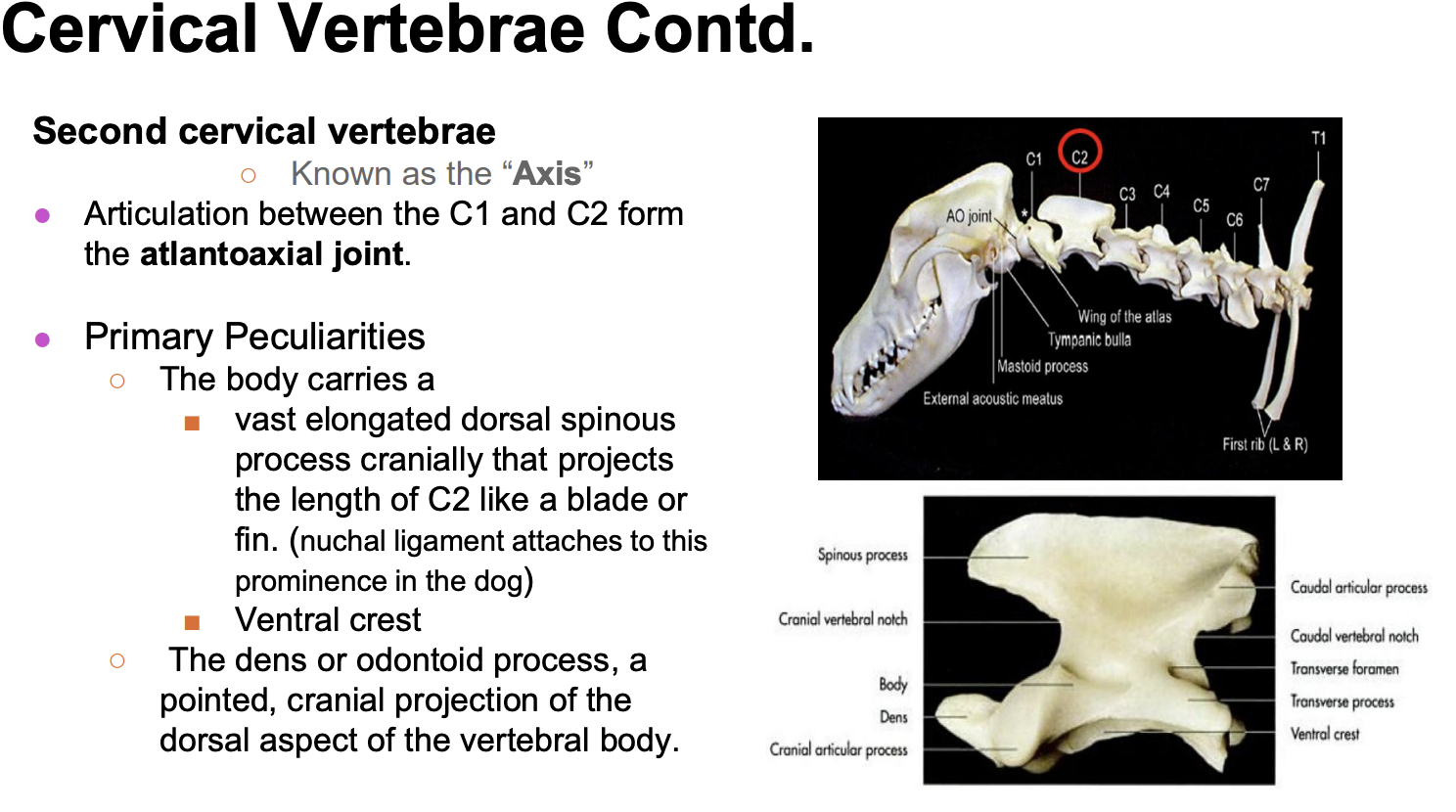
organization of the cervical vertebrae: c2
organization of the cervical vertebrae: C3-C6 and C7
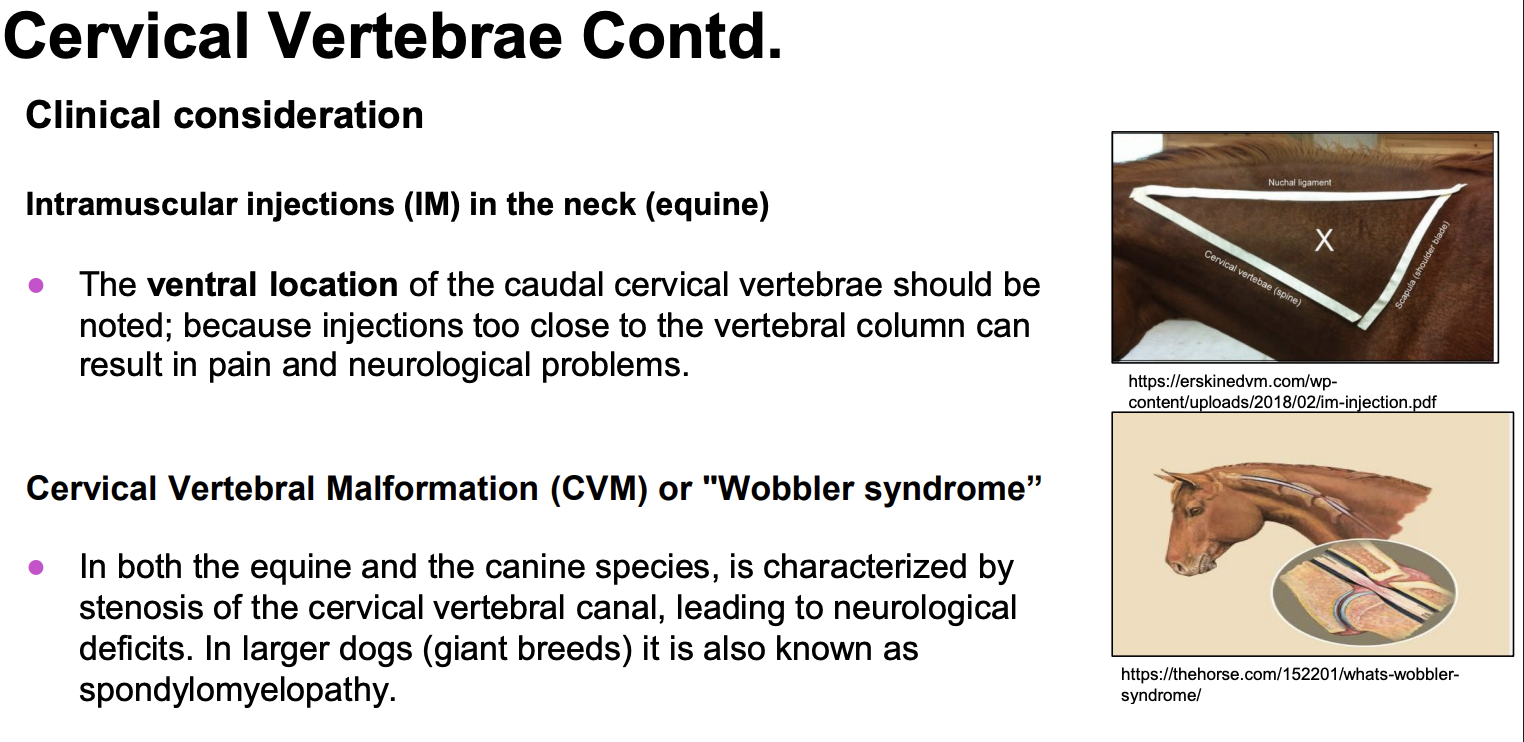
Im injections on a large animals
wobbler syndrome
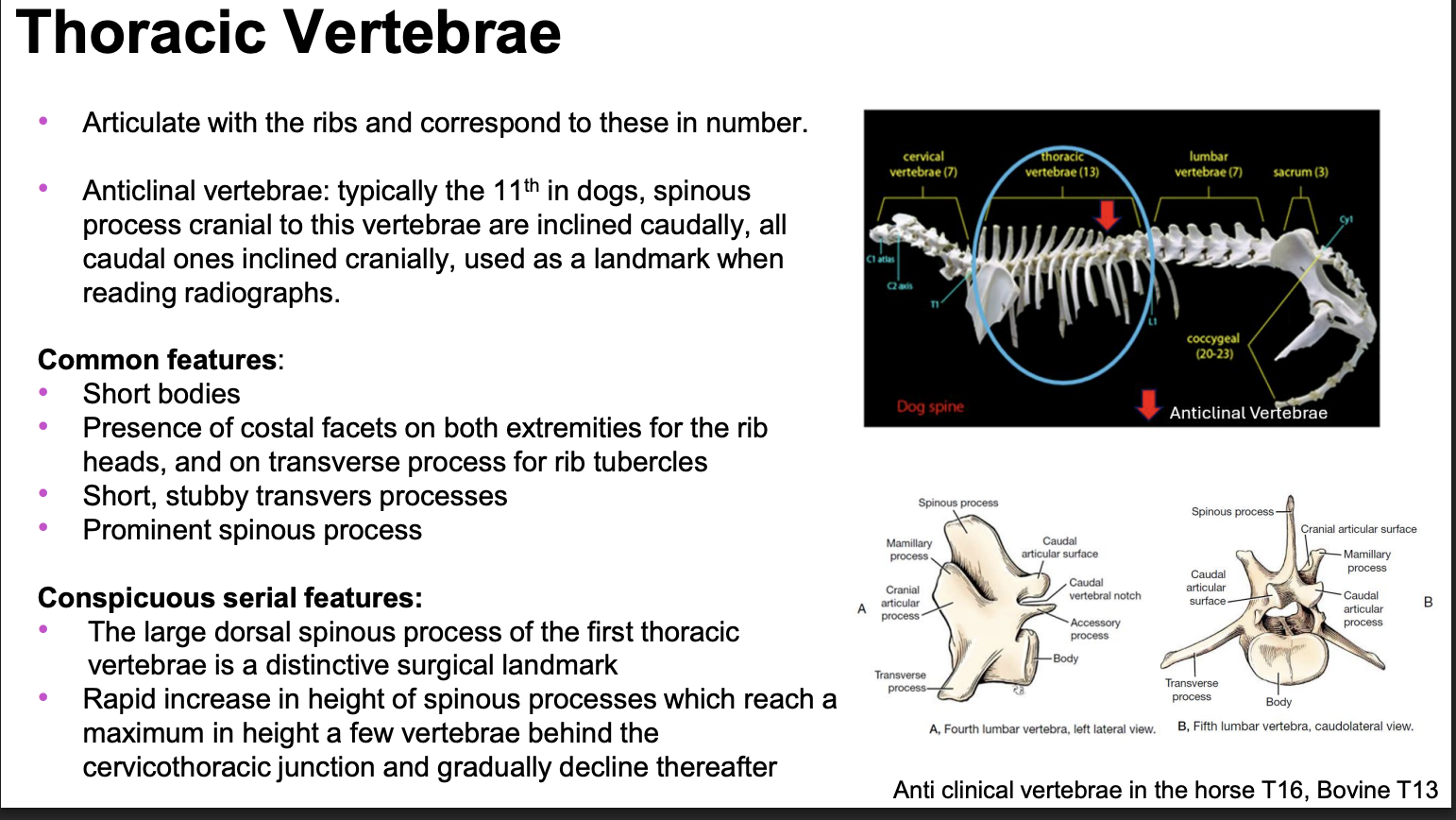
organization of the thoracic vertebrae:
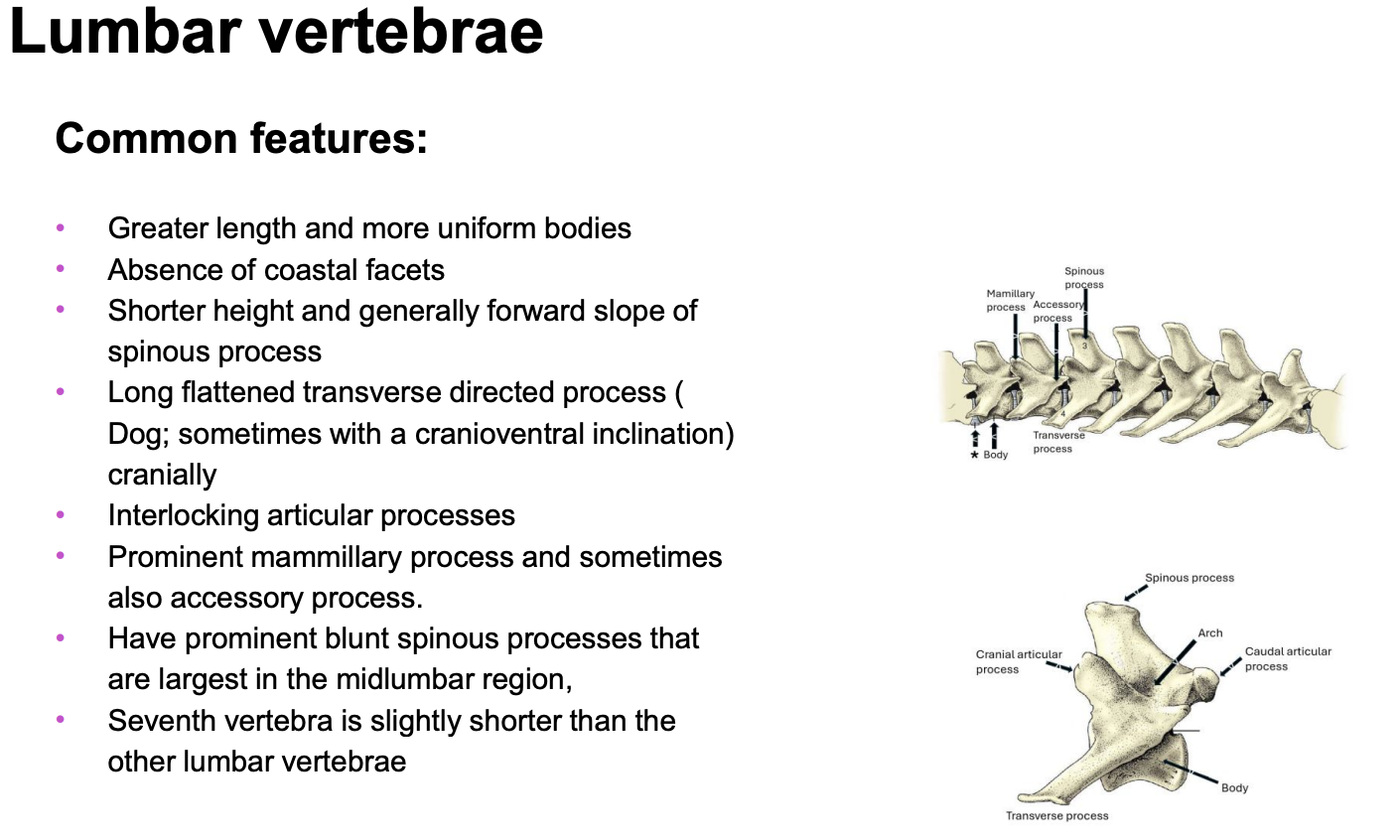
organization of the lumbar vertebrae
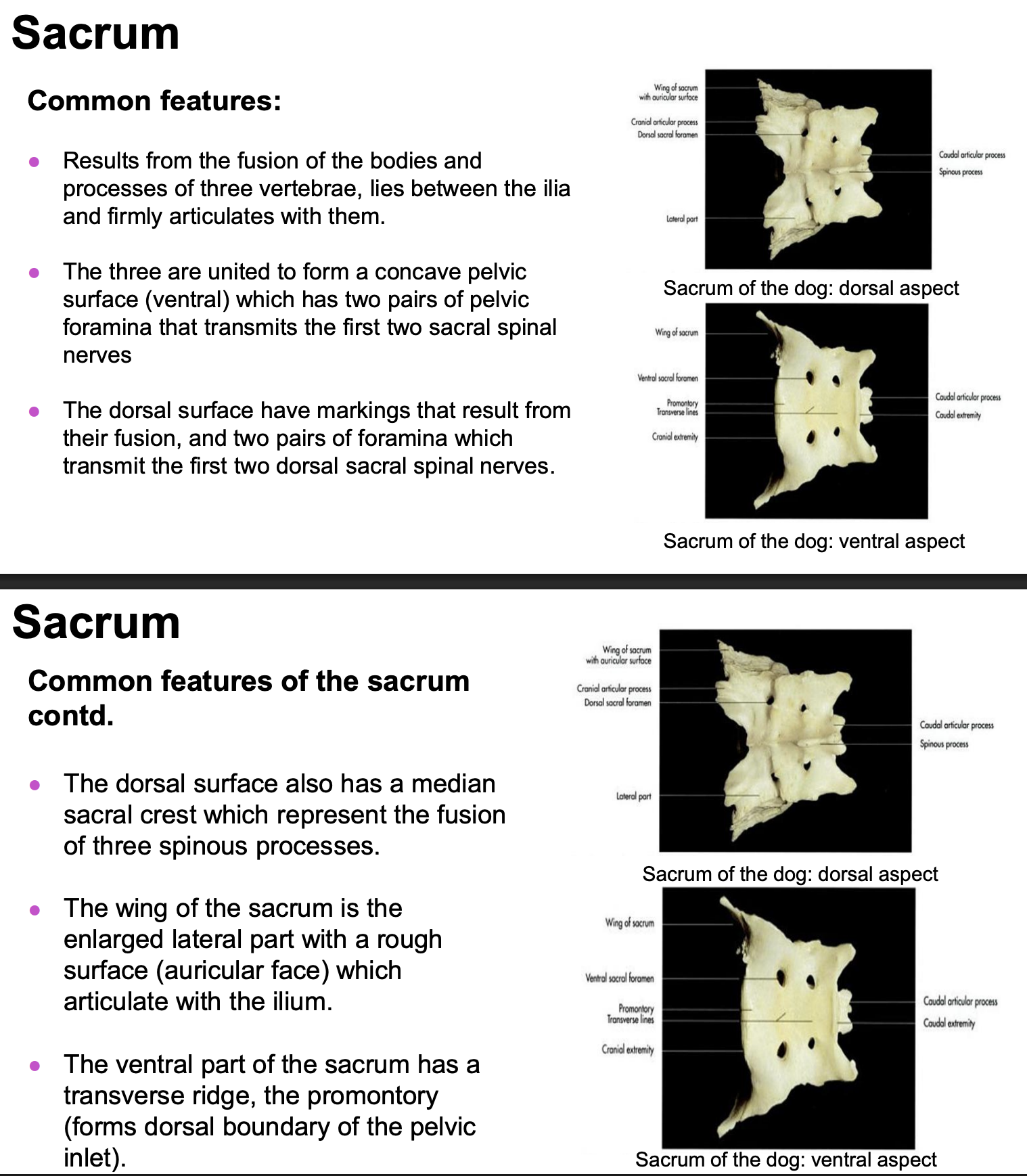
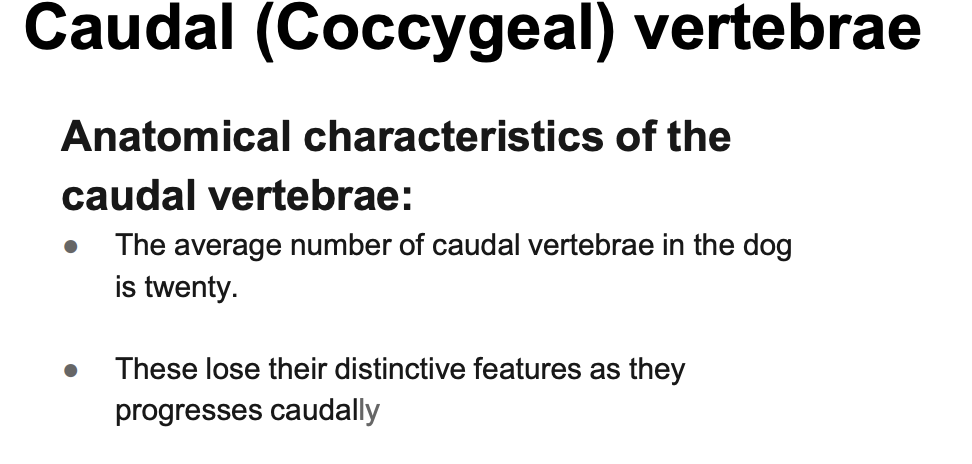
organization of the sacral vertebrae:
organization of the caudal (coccygeal) vertebrae:
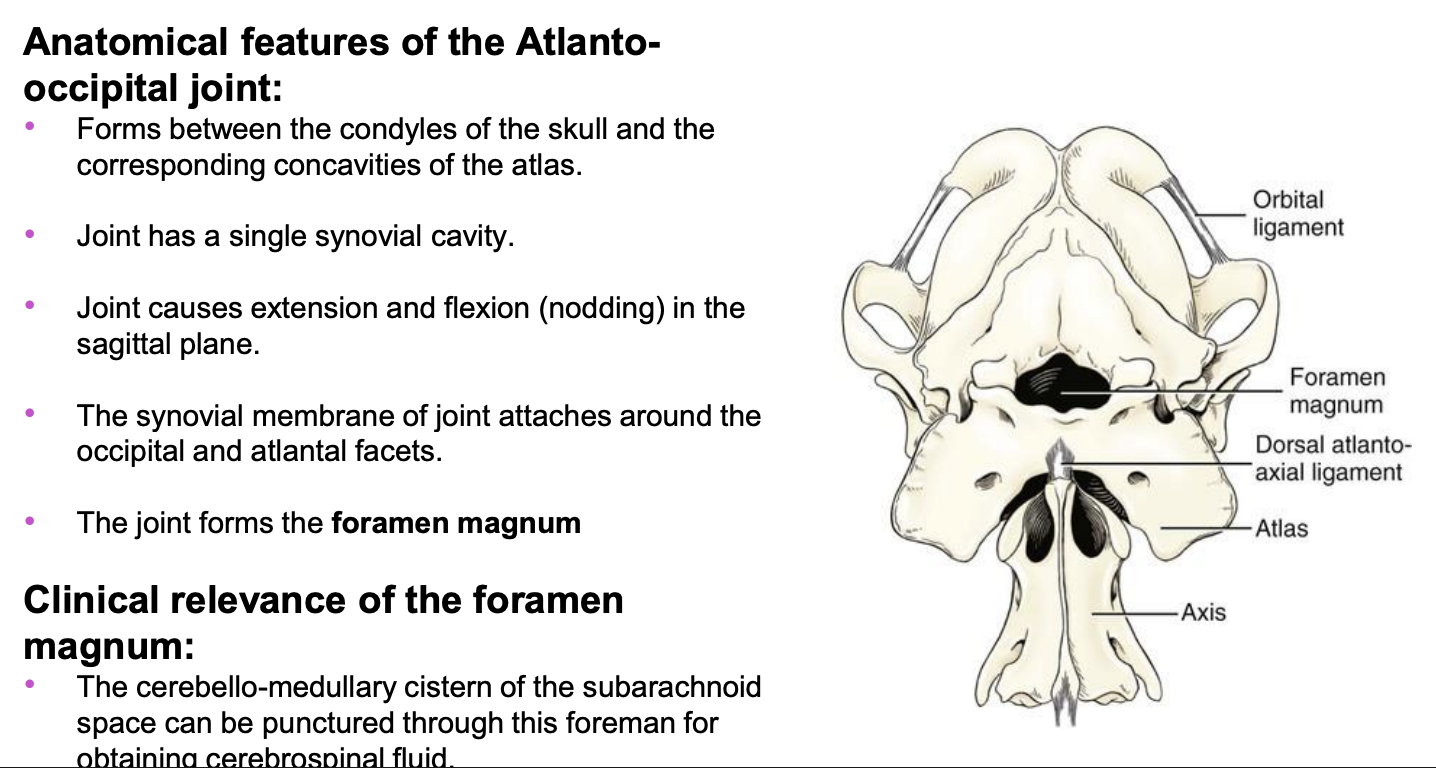
anatomical features of the atlantooccipital joint
anatomical features of the atlantoaxial joint
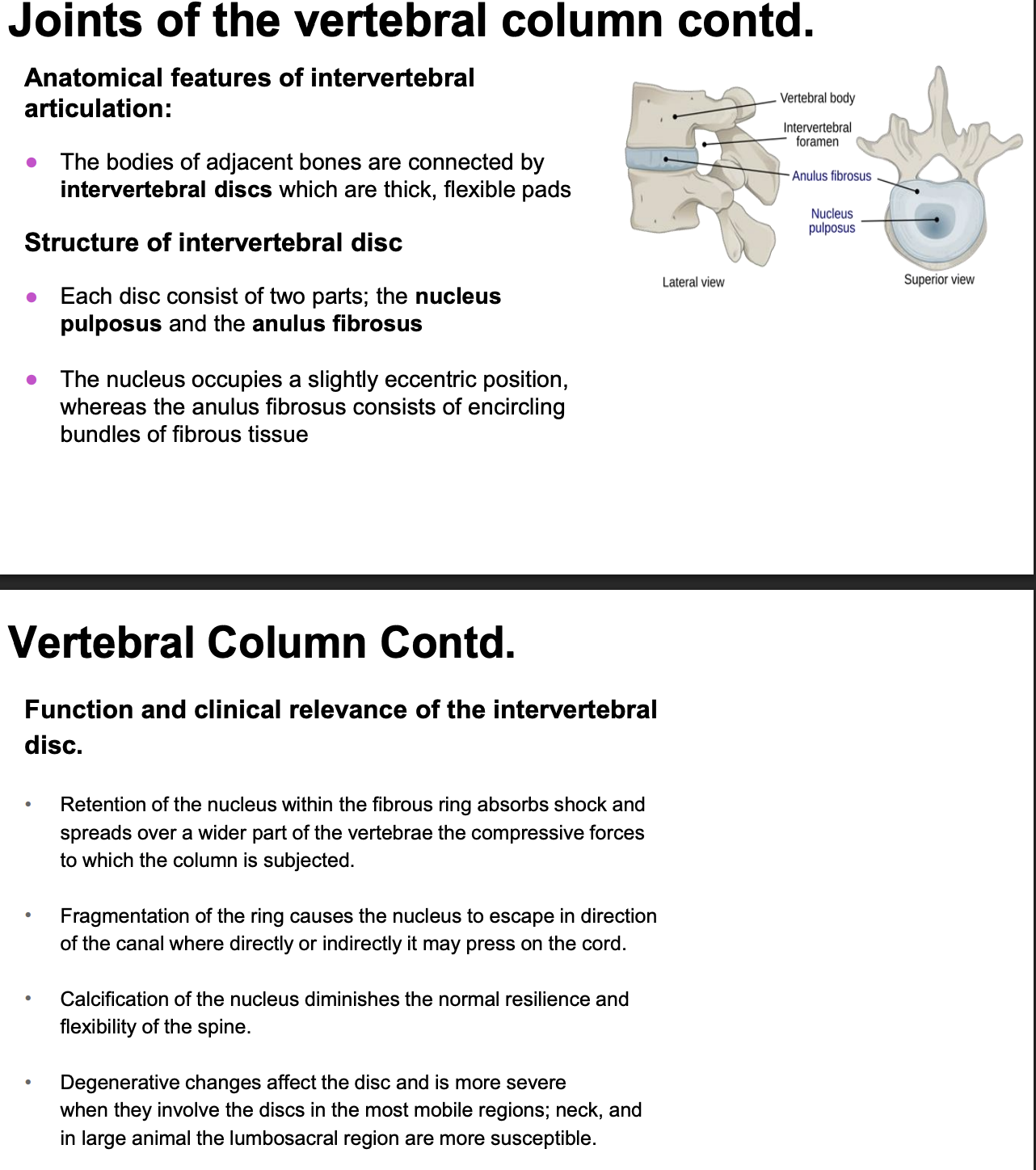
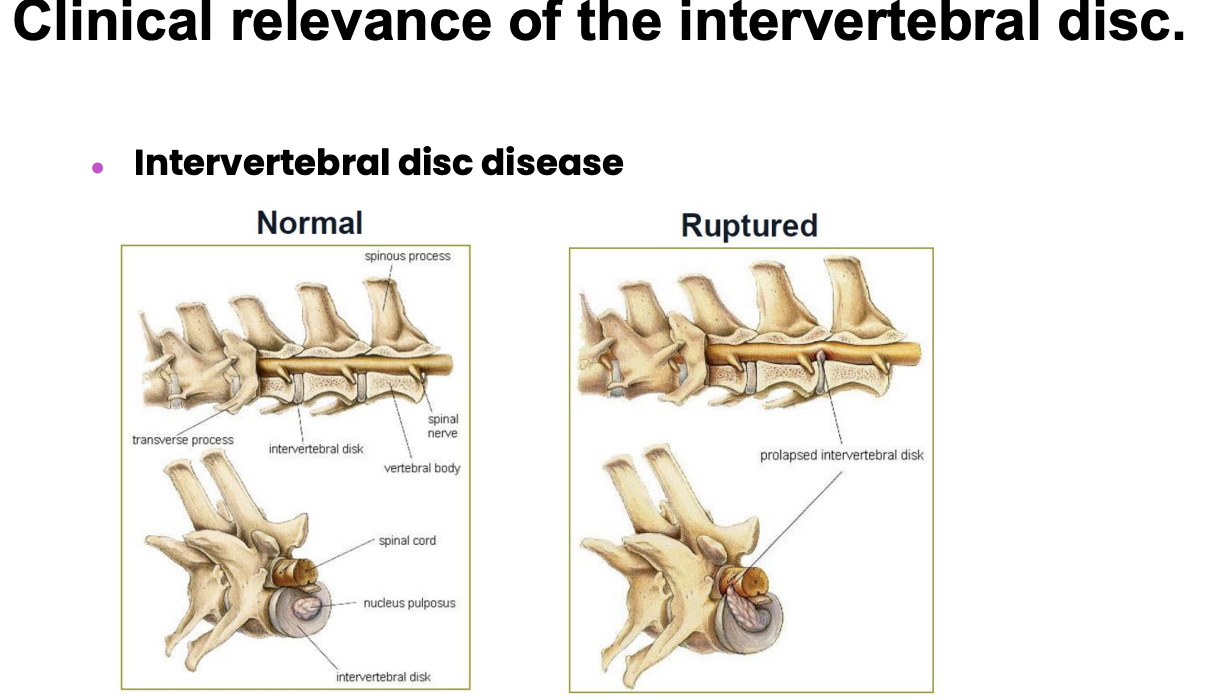
anatomical features of the intervertebral articulation
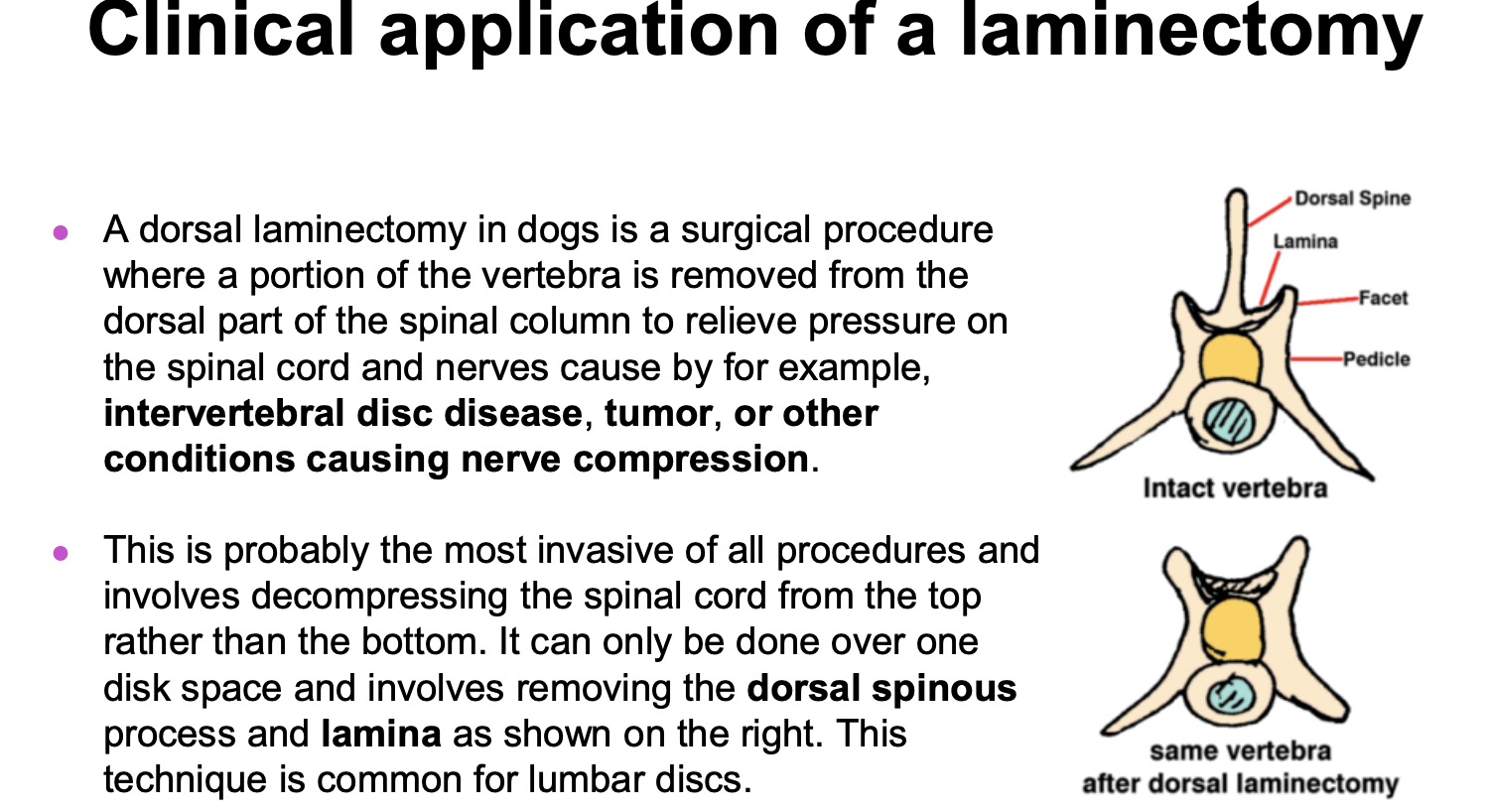
clinical application of a laminectomy
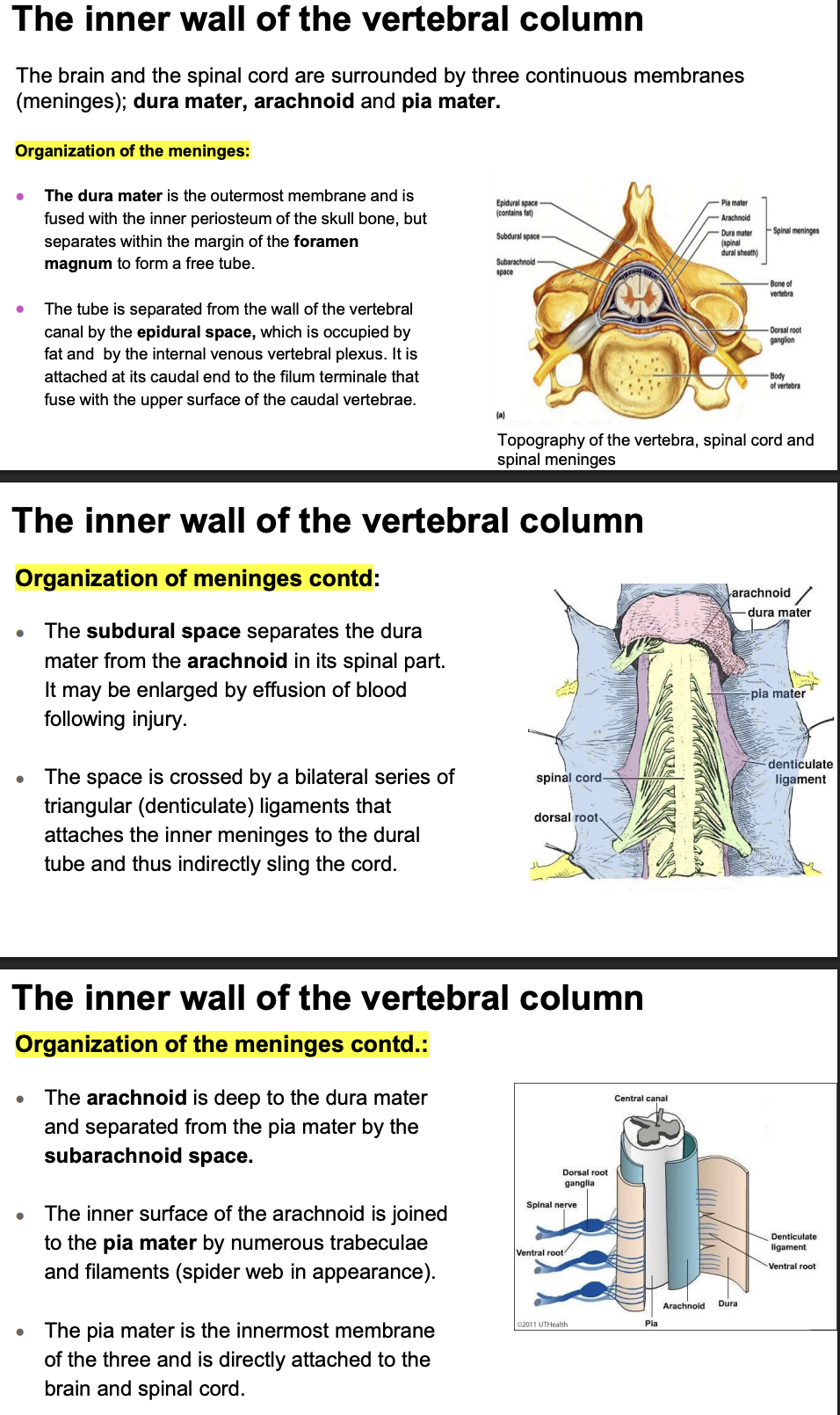
Inner wall of the vertebral column
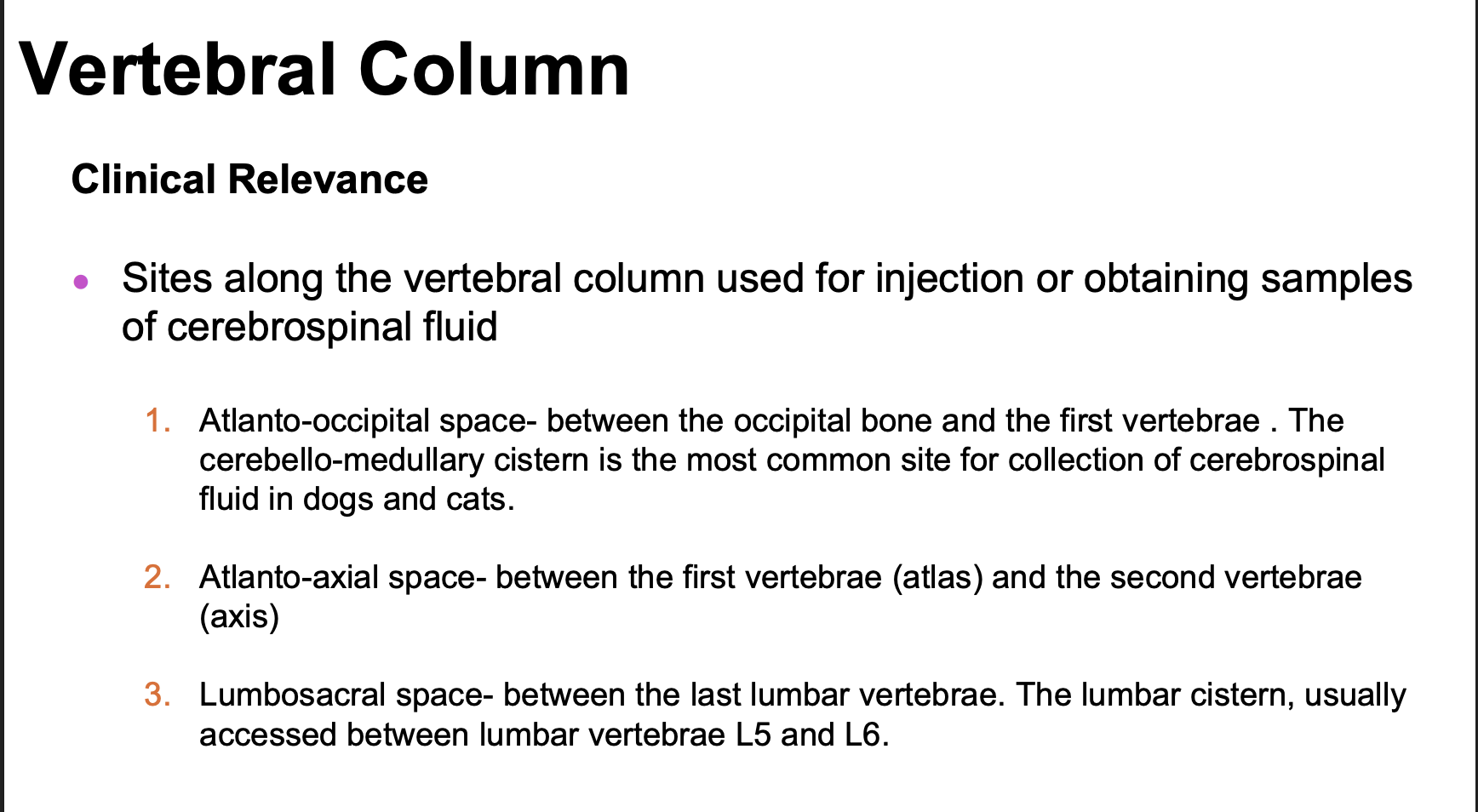
sites along the vertebral column for injection
skeletal muscle function
movement from one place to another
movement of one part of the body in relation to another
stabilizing joints to prevent their collapse under load
generating heat/ regulation: panting or sweating, shivering
skeletal muscle locations
cutaneous (panniculus reflex)
head and neck
abdominal muscles
thoracic limb
pelvic limb
muscles of respiration
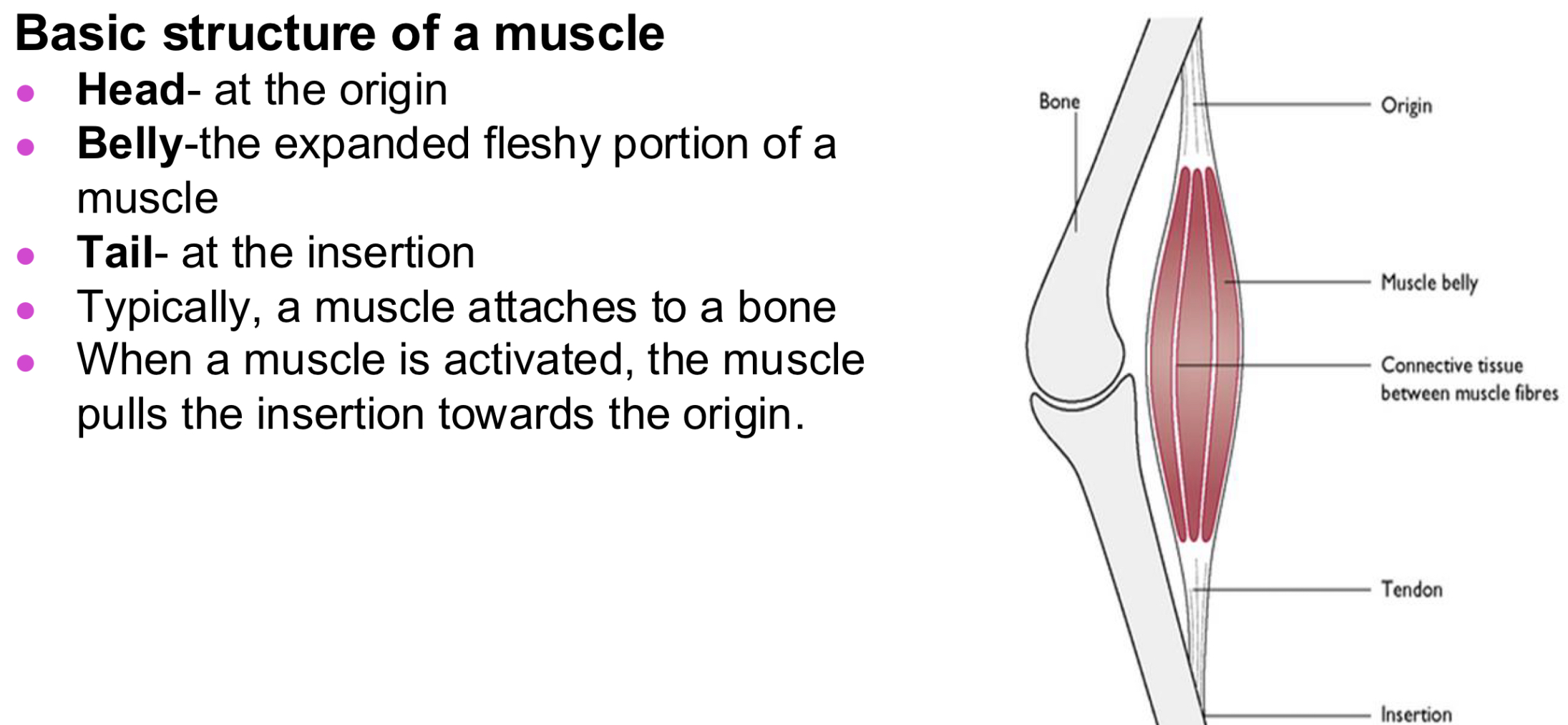
Muscle structure and the different forms of muscle
spindle-shaped
wide muscles
two headed
three headed
four headed
two bellied
circular
sphincter
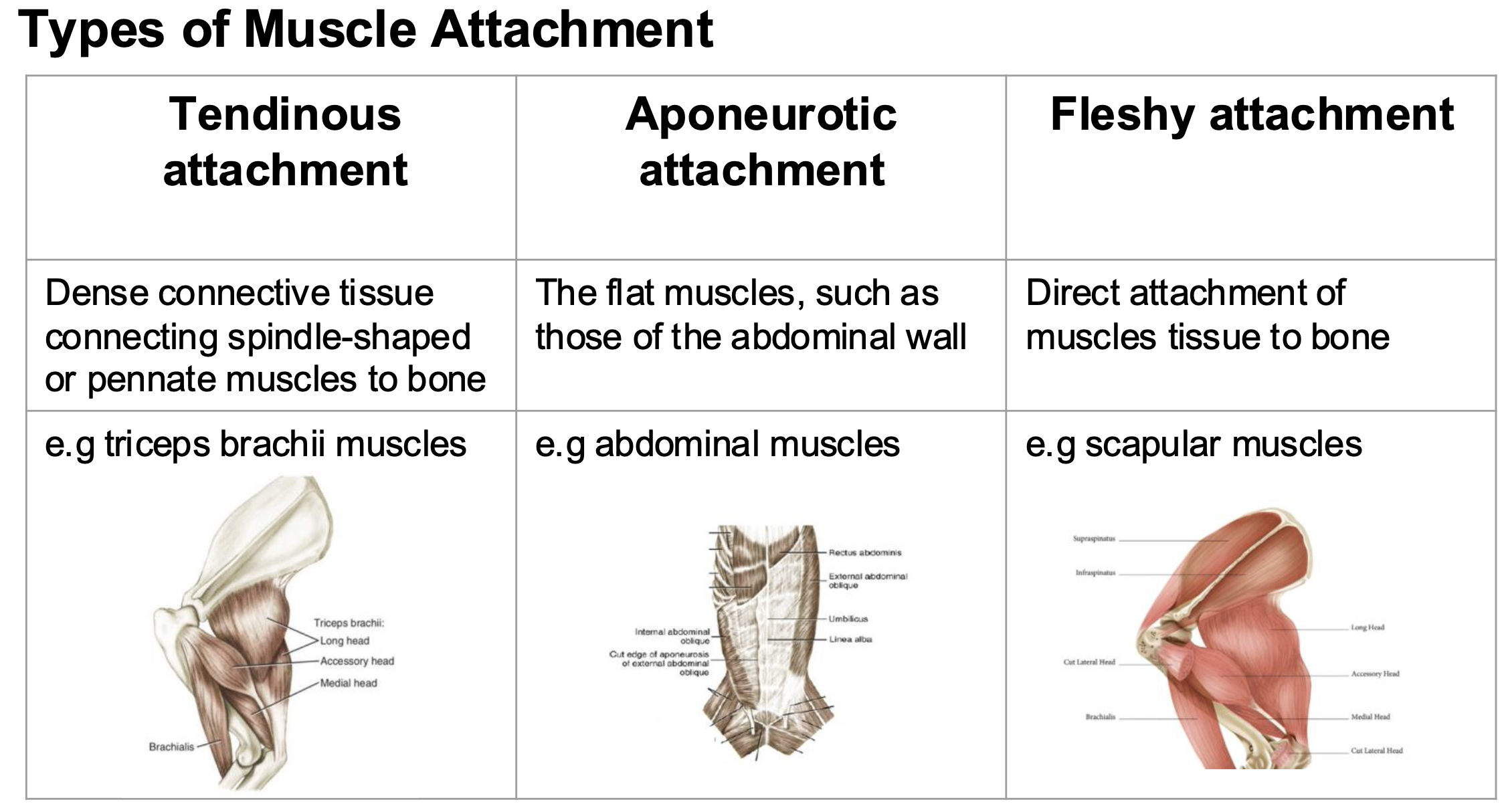
aponeurosis (apo-ner-row-sis)
sheet of pearly fibrous tissue that takes the place of a tendon in flat muscles having a wide area of attachment
origin vs insertion
origin= more fixed part of the muscle attachment, moves least during contraction
insertion= more moveable point or attachment (distal to its origin)
types of muscle attachment
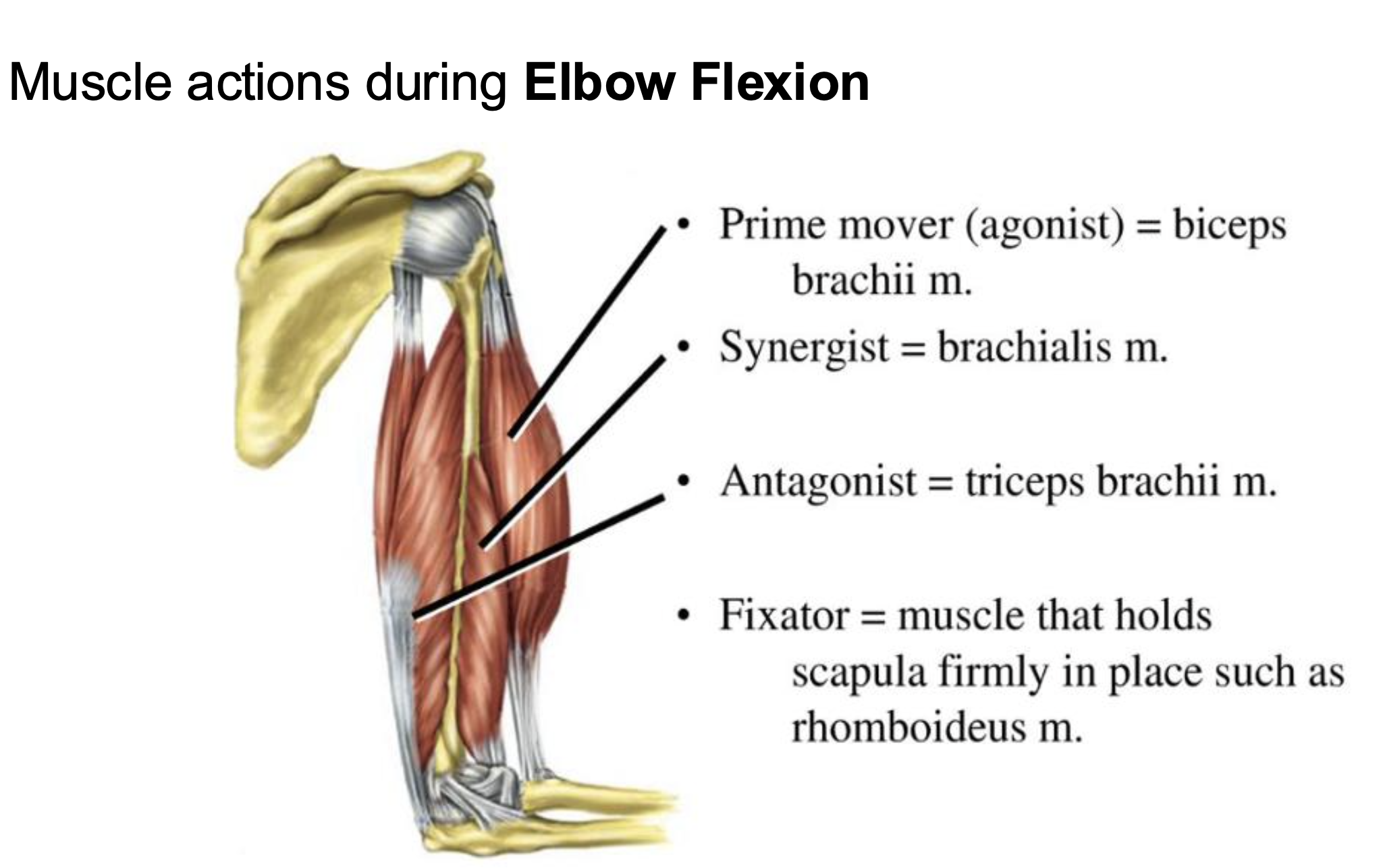
muscle action classifications:
prime mover or agonist= muscle or muscle groups that produce the characteristic movement of a joint (principle muscle)
antagonist= a muscle or muscle groups that opposes the action of a prime mover or agonist
synergistic= assists the action of a prime mover in carrying out its function
fixator= a muscle that stabilizes the proximal end of a limb while the distal end moves
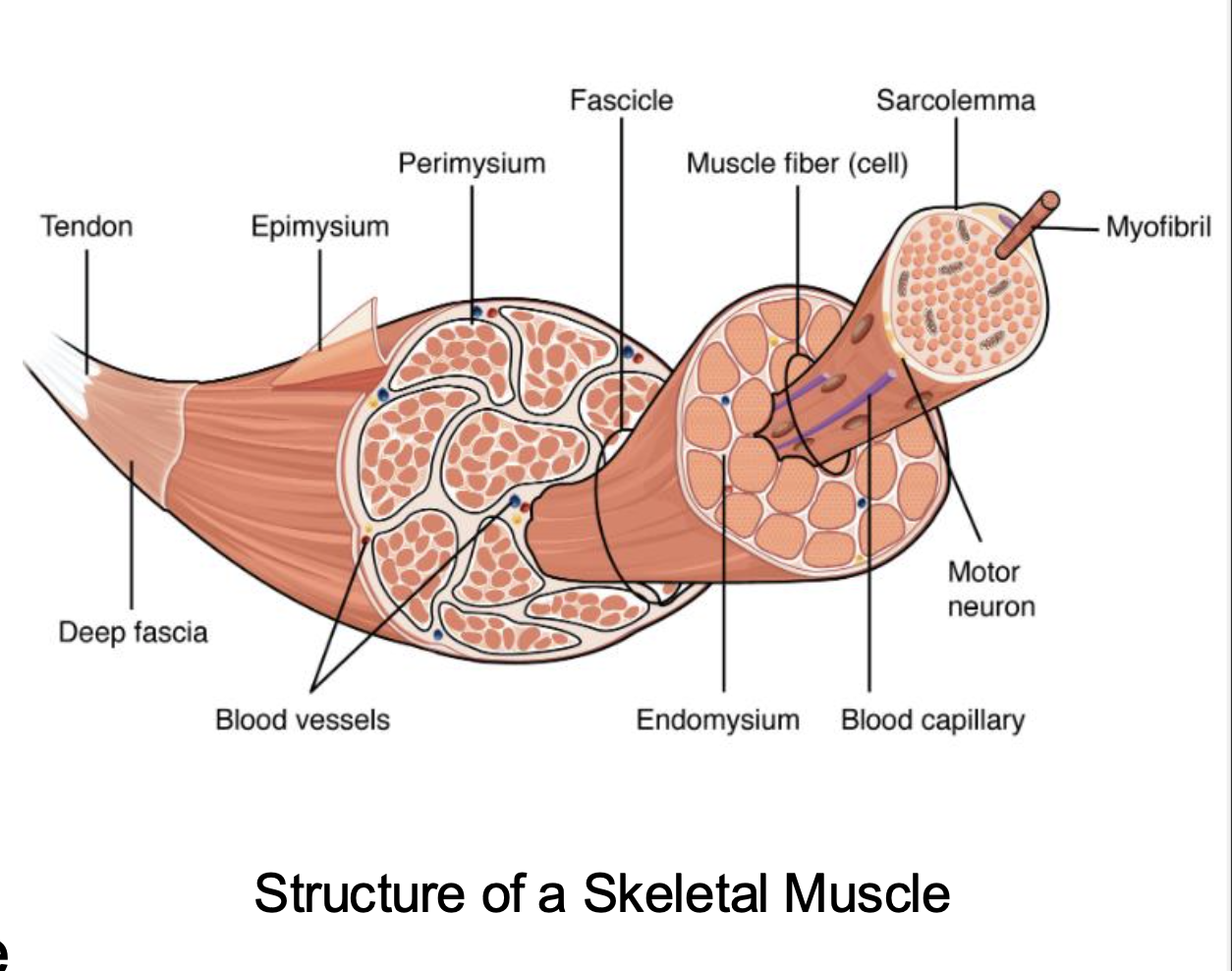
muscle architecture: Fascicles in skeletal muscle, myocytes, myofibrils
fascicles in skeletal muscle are composed of muscle cells called myocytes, organized in patterns such as: parallel, pennate, circular this impacts the whole function of the muscle (range of motion and strength)
the cells are referred to as muscle fibers in skeletal muscle
myocytes contain small contractile myofibrils which contractile elements in the muscle cells use to contract
longer fiber muscles vs shorted fiber muscles
longer= greater range of motion and cover greater distance (parallel)
shorter= higher cross-sectional area have more force (tension) (pennate)
Fascicle and fiber arrangements
parallel: fibers and fascicles run parallel to the muscles long axis and tendon of insertion (greater range of shortening and thus faster movement velocity)
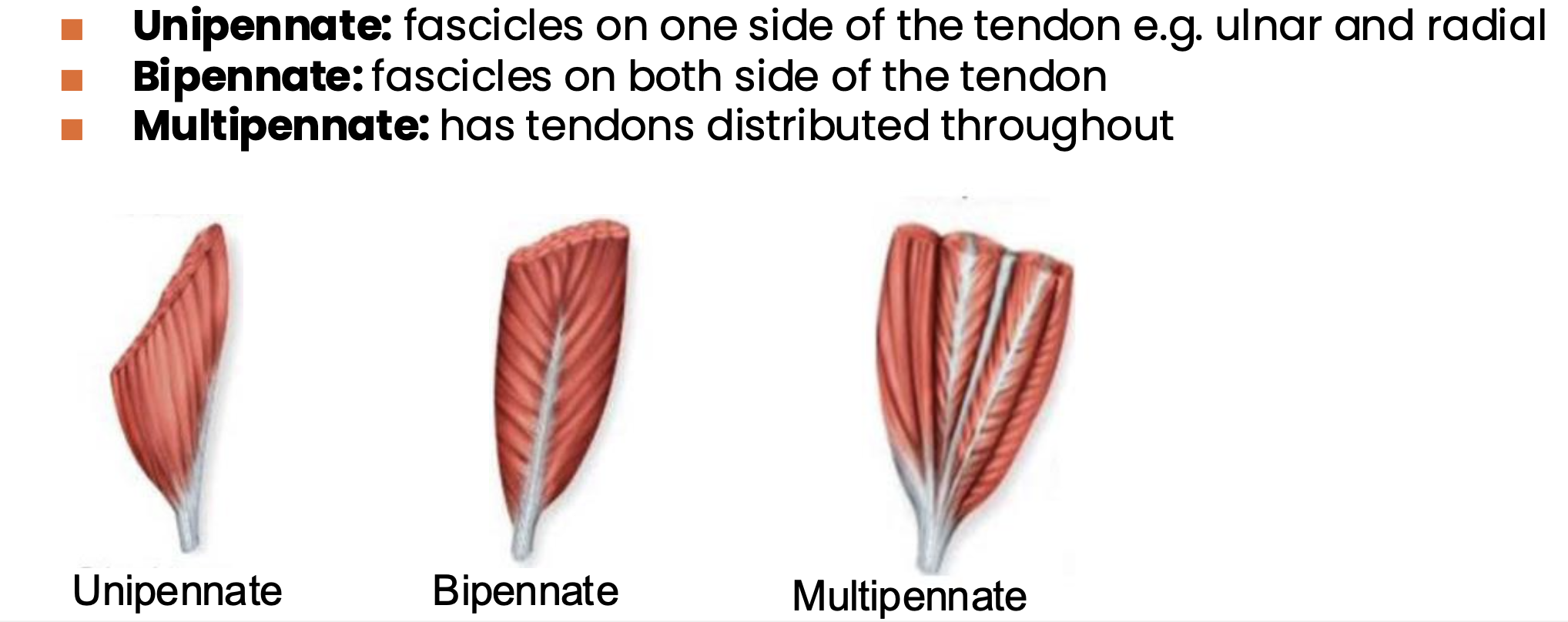
pennate:fibers and fascicles run at an angle to the direction in which the tendon moves, resulting in a greater cross section/area of muscle tissue along axis of contraction maximizing the muscles force potential (more strength)
obliquely orientated muscles have a limited range of motion or excursion of muscle is limited
*these are classified depending on the number of similarly angled sets of fibers that attach to the central tendon
sphincter arrangement: fibers and fascicles are arranged in rings around openings which constrict to close openings
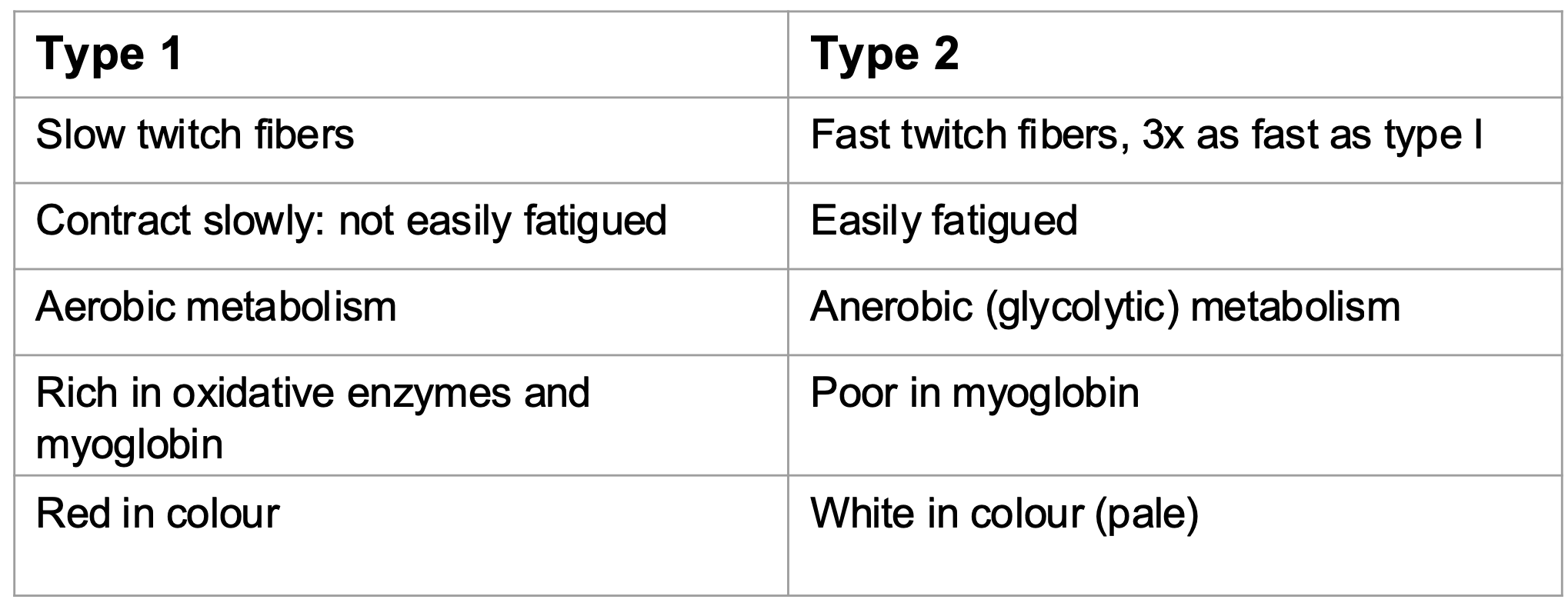
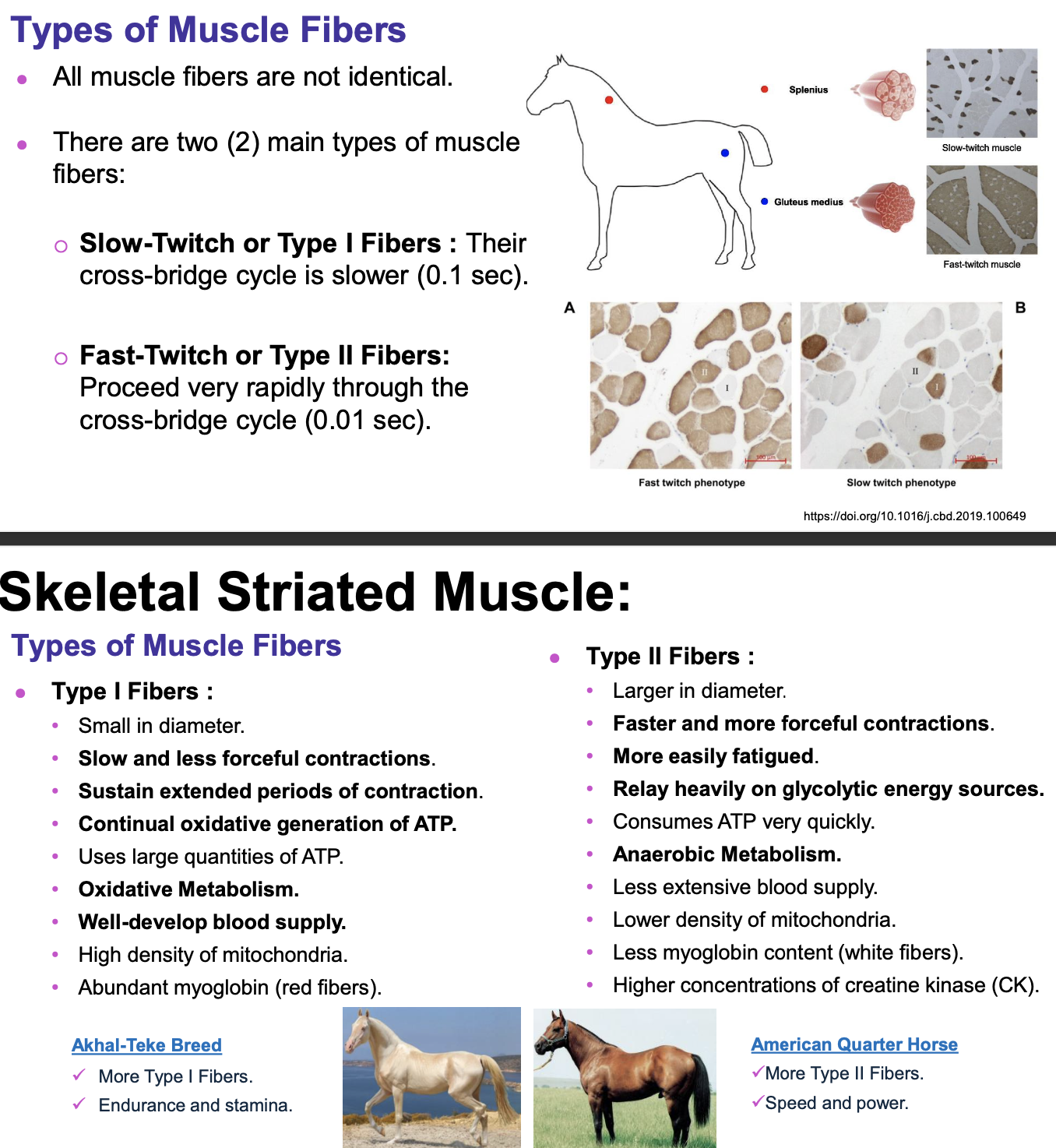
Muscle fiber types: slow vs fast twitch fibers
primary movements of locomotion and accompanying movements
primary: 1. extension: straighten bone alignment, or open a joint (increase angle)
flexion: angulate the bones, or bend the joint (decrease angle)
accompanying:
adduction:movement of an extremity towards the median plane
abduction: movement away from the median plane
circumduction: moving an extremity in a place describing the surface of a cone
rotation: moving a part around its long axis
elevation: lifts part relative to other parts
protraction: advances cranially, a protractor
retraction: pulls part caudally; a retractor
pronation: movement of the dorsal surface of limb to a dorsal position
supination: movement of palmer/planter surface of the limb to as dorsal position
tendon consists of
dense fibrous connective tissue (collagen) by which muscles are attached to bones (some muscles appear to attach directly to bone so called FLESHY attachment)
have great tensile strength and some elasticity, low metabolic needs and are poorly vascularized and do not hemorrhage when cut (slow to heal)
Tendon protection:
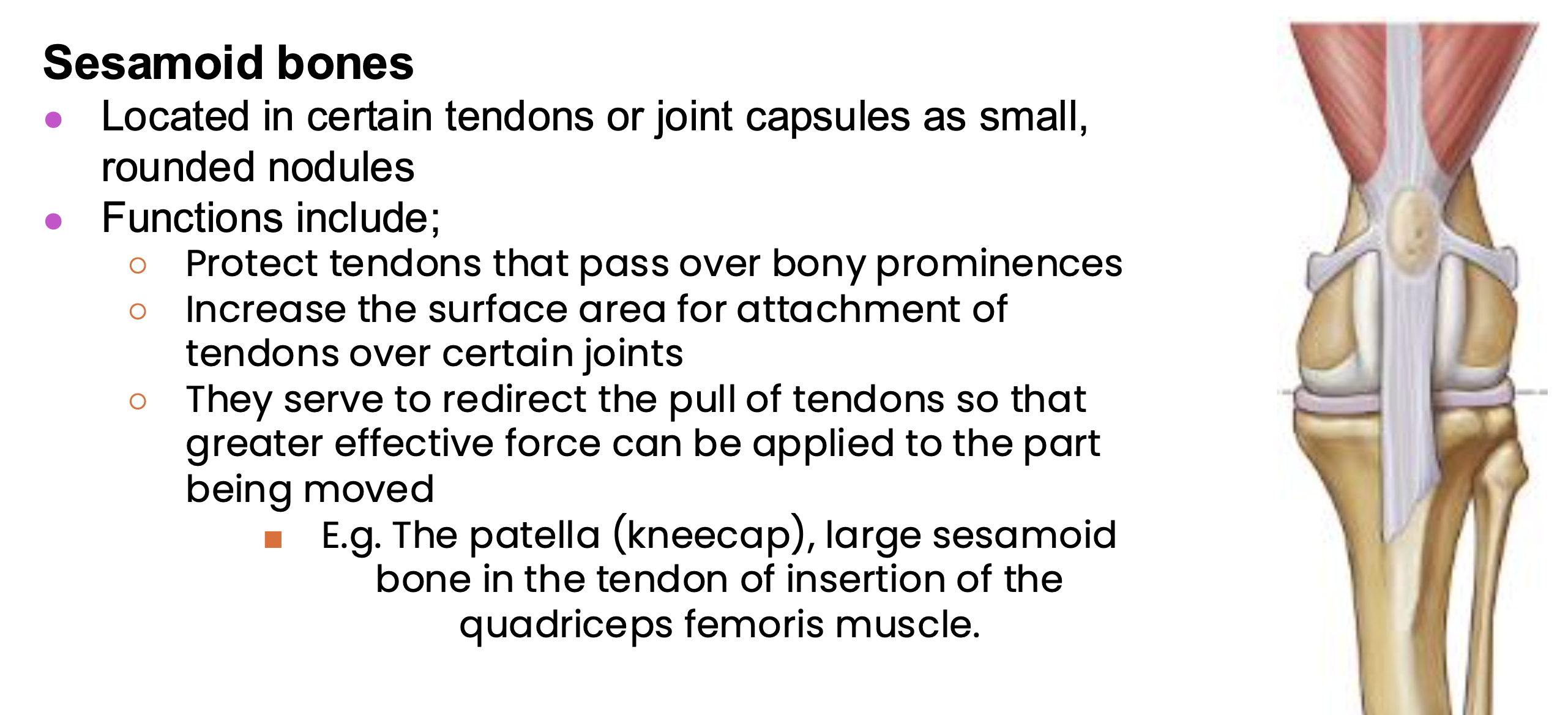
muscles are supported in their many functions through passive structures such as:
sesamoid bones, bursae, tendon sheaths
Fasciae, bursae, synovial tendon sheaths, sesamoid bones
function of tendon
transmit muscle force to skeleton, promote joint stability, store and return elastic energy
accessory structures of muscles: Fasciae superficial vs deep
Fasciae: connective tissue that surrounds the body and compartmentalizes the muscle
superficial:(subcutis or hypodermis) areolar loose connective tissue and is a filler between the skin and underlying structures, usually site for injections can accommodate large volumes of fluid medication hence hypodermic /subcutaneous injection, infections spready easily in this tissue, adipose tissue accumulation seen here usually in pigs
deep: beneath the superfical fascia, surrounds and breaks muscles into groups, may be attachment for some muscles, may be named into different regional fasci, impermeable fluids such as pus spread along them, distinct fascial septa separate groups of muscles from one another and result in fascial planes along which infection may spread or fluid drains
accessory structures of muscles: synovial bursae
simple connective tissue sacs containing a viscous fluid and serving to reduce friction, found everywhere in the body where muscles, tendons, or ligaments glide over bone
classified according to formation: congenital (true) or acquired (false) and anatomical location
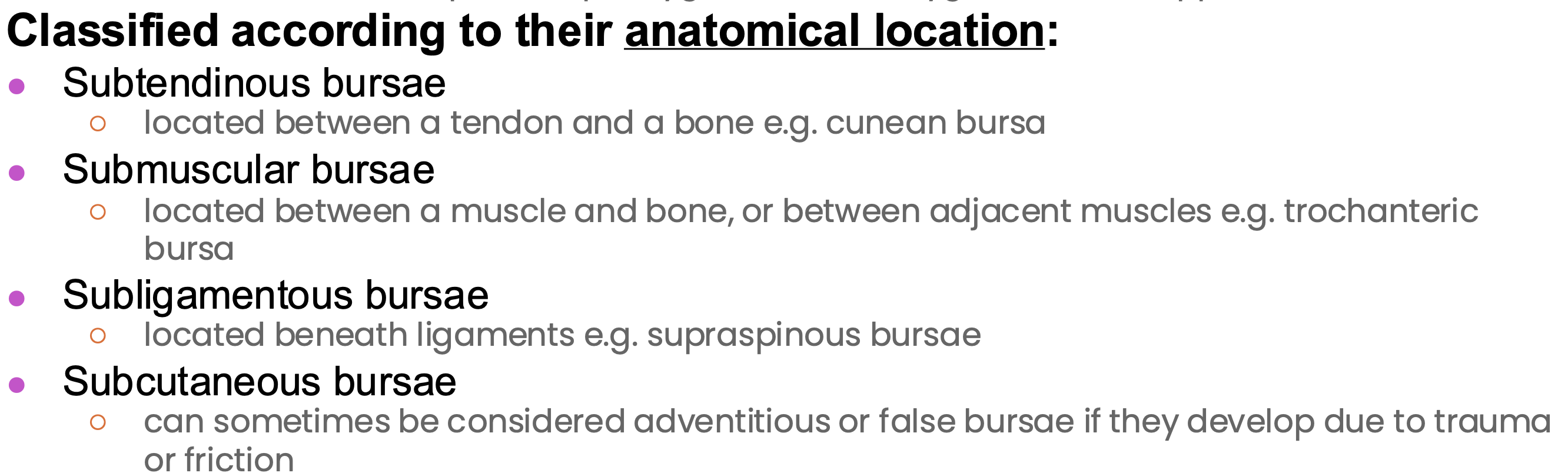
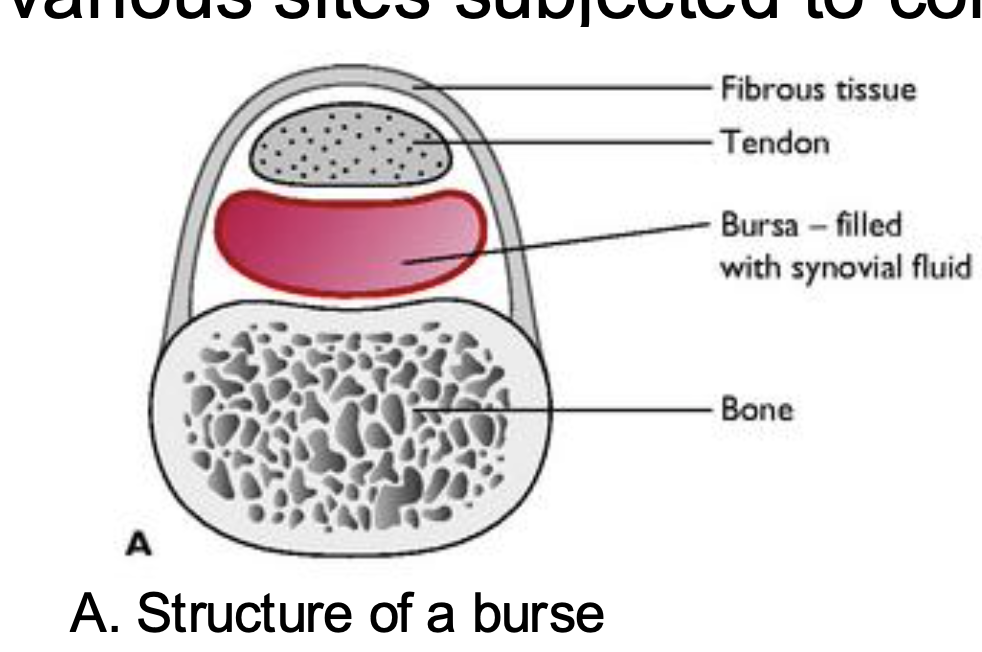
inconsistent bursae may develop subcutaneously at various sites subjected to constant mechanical pressure
accessory structures of muscles: synovial (tendon) sheath
completely sheathe the tendons like a tube, double layered, elongated sacs containing synovia that wraps tendons, the cavities are filled with synovial fluid, protects the underlying tissues from pressure exerted by the tendon and reducing friction during movement
two layers: visceral and parietal with synovial fluid between them allowing gliding
accessory structures of muscles: sesamoid bones
skeletal muscle functions:
contractile, energy, excitability, calcium storage
sacromere
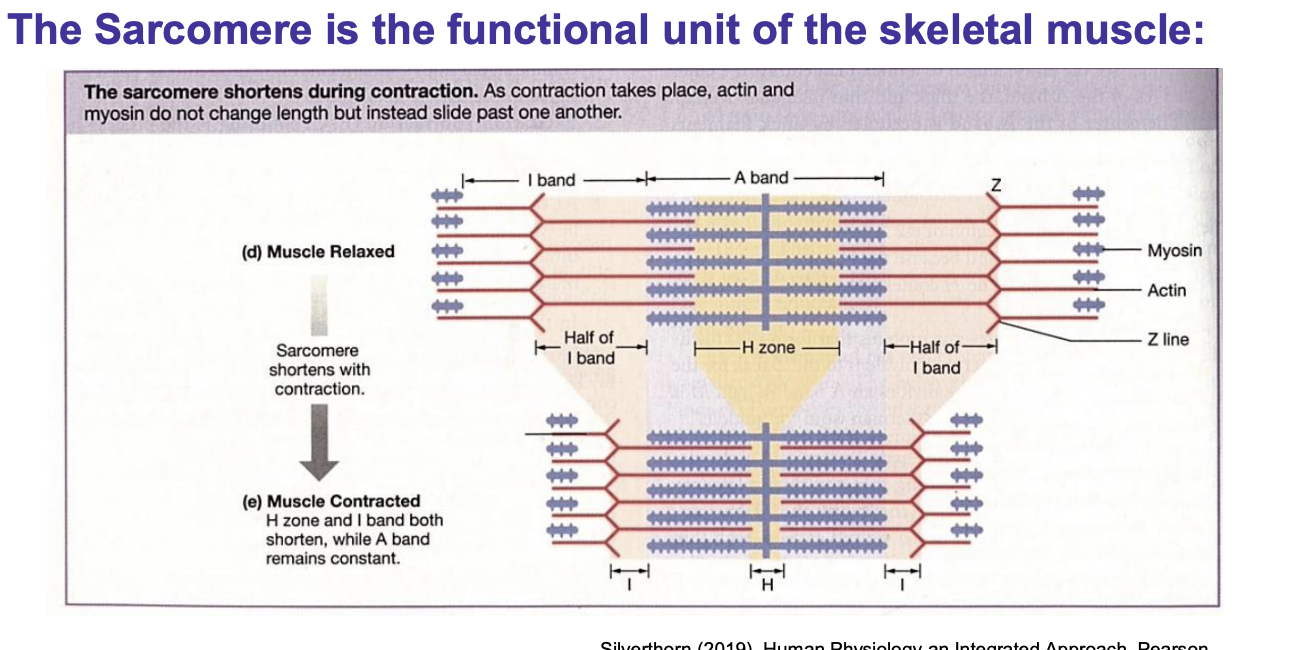
Myosin and Actin
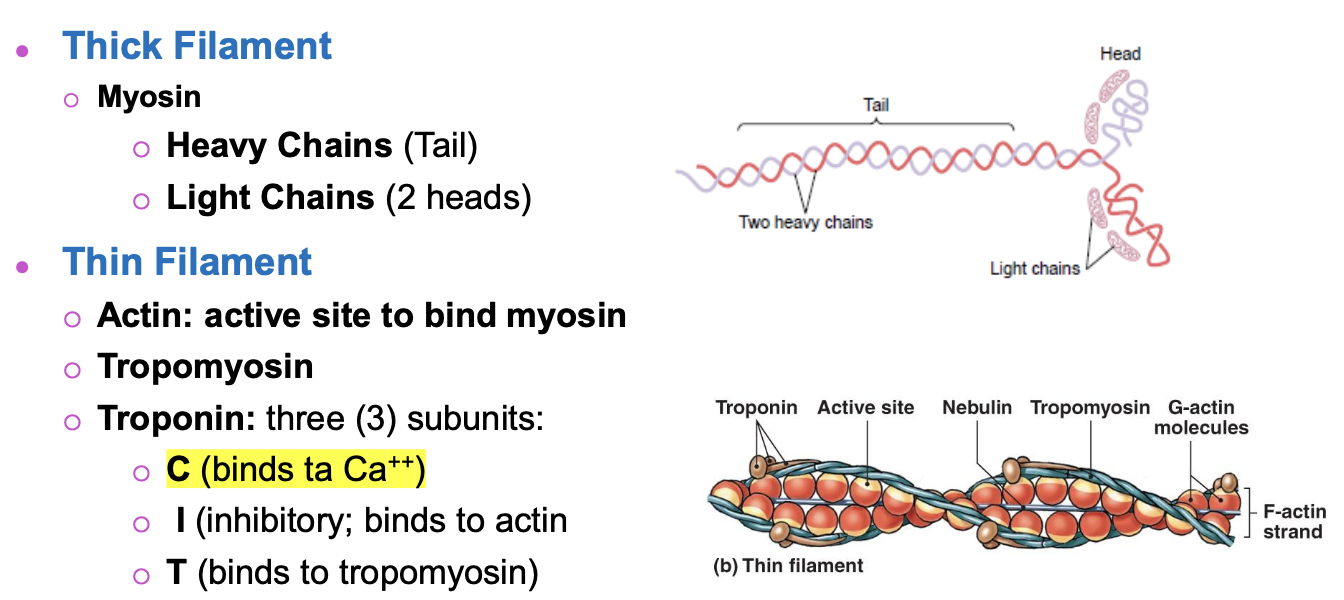
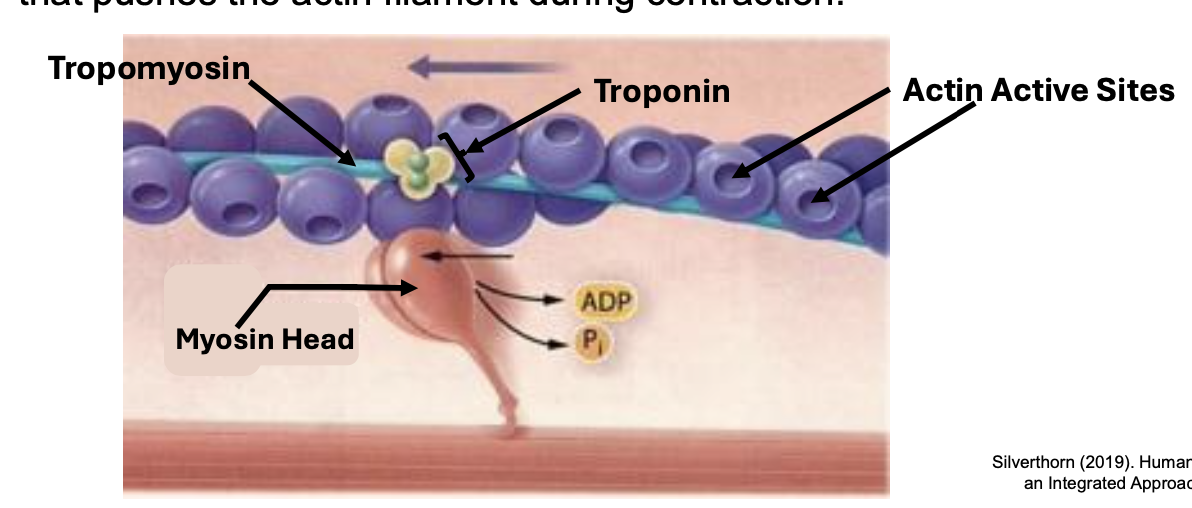
cross bridges between the thick and thin filaments
cross bridges are formed by the interaction of the myosin heads (thick filaments) to active sites in actin filaments (thing filaments), the movement of myosin cross bridges provides force that pushes the actin filament during contraction
Skeletal muscle motor unit
all skeletal muscle fibers are innervated by a neuron and a single motor neuron communicates with several muscle fibers, as more tension is needed more motor units are recruited
the synapse in muscle cells is called neuromuscular junction which is a chemical synapse as it involves neurotransmitter release from the neuron that binds the muscle receptors (at the motor end plate)
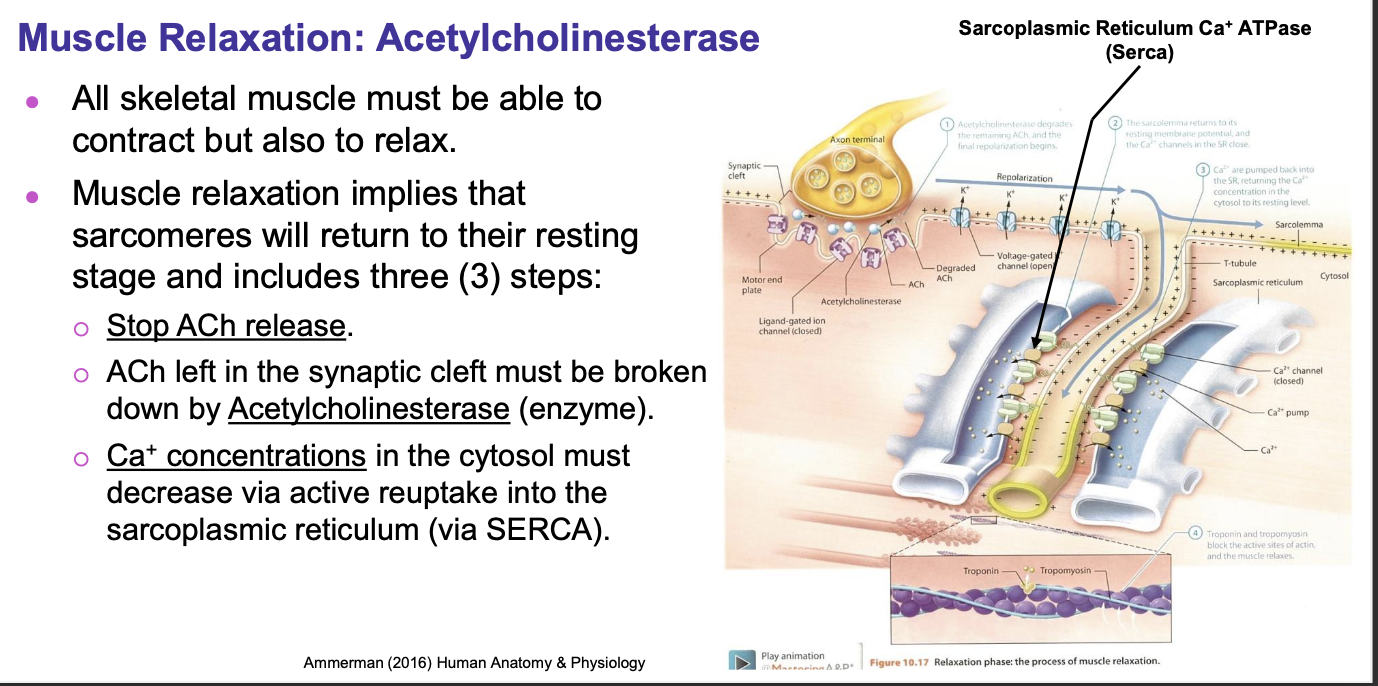
in order for the muscle to contract it must experience an action potential at the sarcolemma→ Acetyl Choline is released from the motor neuron into the synaptic cleft that is between the neuron and the muscle fiber, ACh binds to ligand-gated Na+ channels in the motor neuron end plate and allow Na+ to enter the muscle fiber, entry of Na+ will depolarize the sarcolemma
End plate potential for skeletal striated muscle: propagation and t-tubules
propagation: end-plate potential stimulates an action potential that will travel along the sarcolemma and down the t-tubules in a wave like pattern, depolarization of one area will depolarize other neighboring areas, stimulating the opening of other voltage-gated Na+ channels along the muscle membrane
T-tubules (transverse) are deep invaginations of the muscle cell membrane into the muscle fiber which contact the sarcoplasmic reticulum
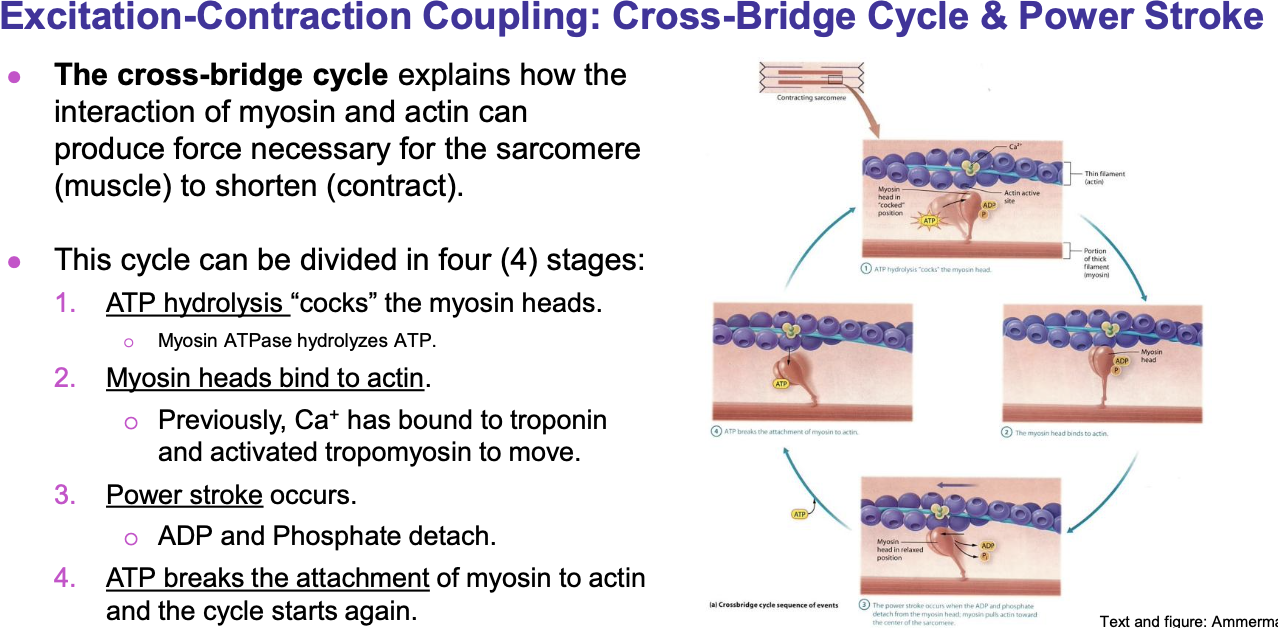
End plate potential for skeletal striated muscle: excitation-contraction coupling/calcium binding to troponin
end plate potential: the excitation-contraction coupling refers to the connection of the depolarization of the sarcolemma and the contraction of the myofilaments, the wave of depolarization drives deep into the muscle fiber thanks to the t-tubules, t-tubules are linked to the cisternae of the sarcoplasmic reticulum were Ca+ is stored (Ca+ is released into the cytoplasm when the depolarization wave runs through the t-tubules), muscle contraction requires many action potentials to occur repeatedly which Ca+ in the cytosol increased with each one. the increasing Ca+ concentration is key to the excitation process to the muscle contraction process, Ca+ binds to troponin and triggers the sliding mechanism in the muscle
tropomyosin curls around the thin filaments blocking the active sites of actin molecules, preventing myosin from binding, upon excitation of Ca+ ions bind to troponin C and initiates a mechanism that moves the tropomyosin away from the actin active sites
The cycle of cross bridge
muscle- tendon interaction
at the end of each muscle, interdigitating collagen fibers merge and contribute to a connective tissue bundle called tendon, each individual muscle fiber is connected directly to the tendon creating a pull on the tendon attached to the bone
Muscle relaxation
Muscle tone
refers to the flight tension of muscles which is involuntary activation of motor units by the brain and spinal cord (the CNS alternates which motor units to activate so all can rest), the contractions are not strong enough for movement but maintain posture and stabilize joints
Muscle injury: enzymes
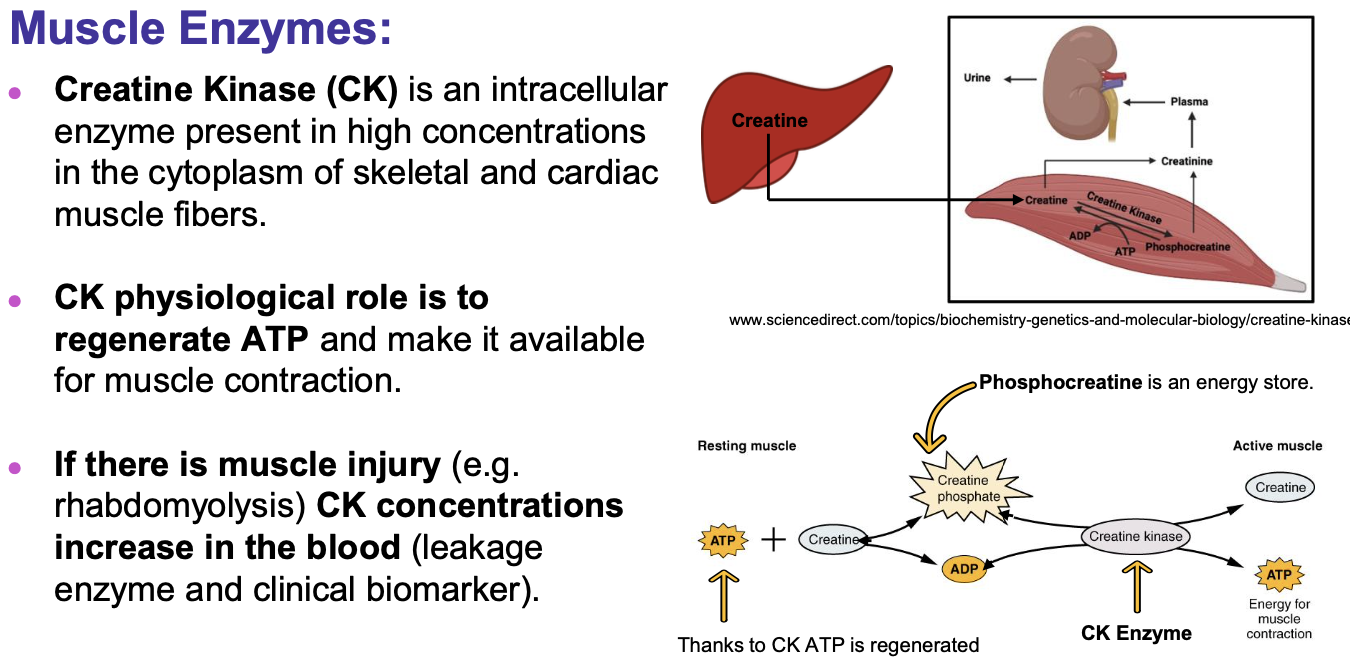
Ck: image above
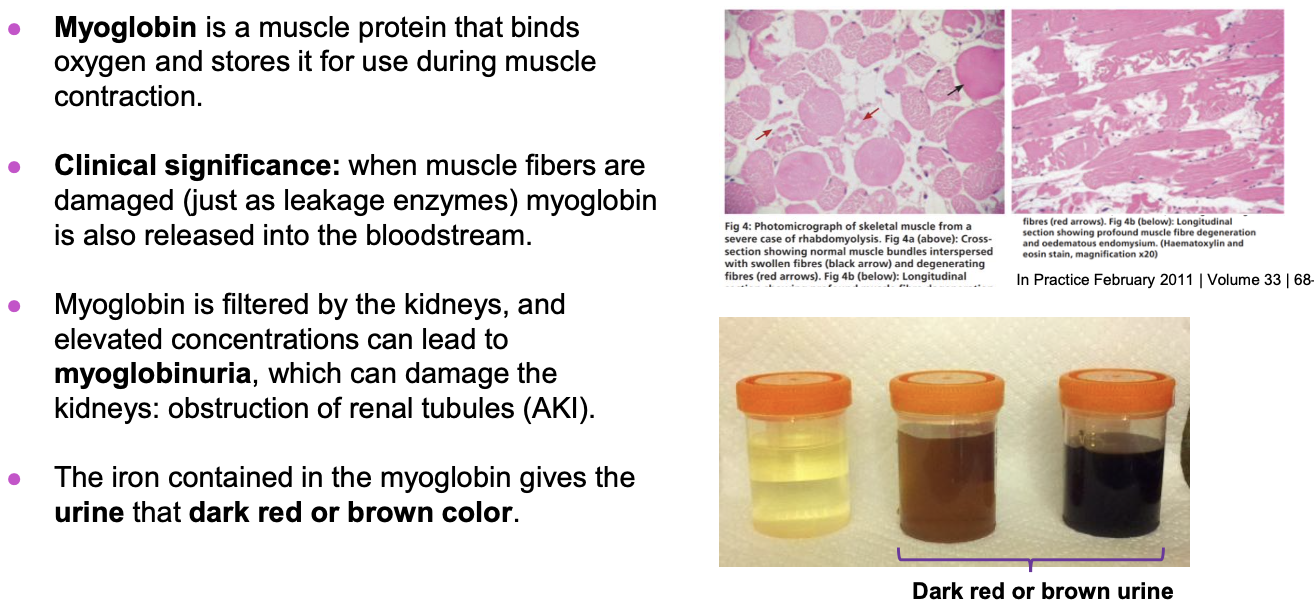
Myoglobin: muscle protein that binds oxygen and stores it for use during muscle contraction (if muscle fibers are damaged myoglobin is released in to the bloodstream which is filtered by the kidneys leading to myoglobinuria)