2. Diseases of the cornea- Keratitis, ulceration, perforation.
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
What are the five layers of the cornea?
Epithelium
Bowman's layer (not present in dogs and cats)
Stroma
Descemet's membrane
Endothelium
What is the limbus?
The transition zone between the cornea and sclera
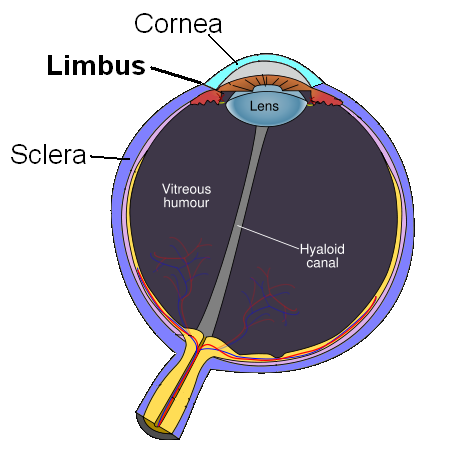
What is the significance of the limbus?
Richly vascularised (supplying nutrients to the avascular cornea)
Contains stem cells for epithelial regeneration
Dense network of nerves, lymphatics, and immune cells
What is the uvea?
The middle layer of the eye (vascular tunic) consisting of the iris, ciliary body, and choroid
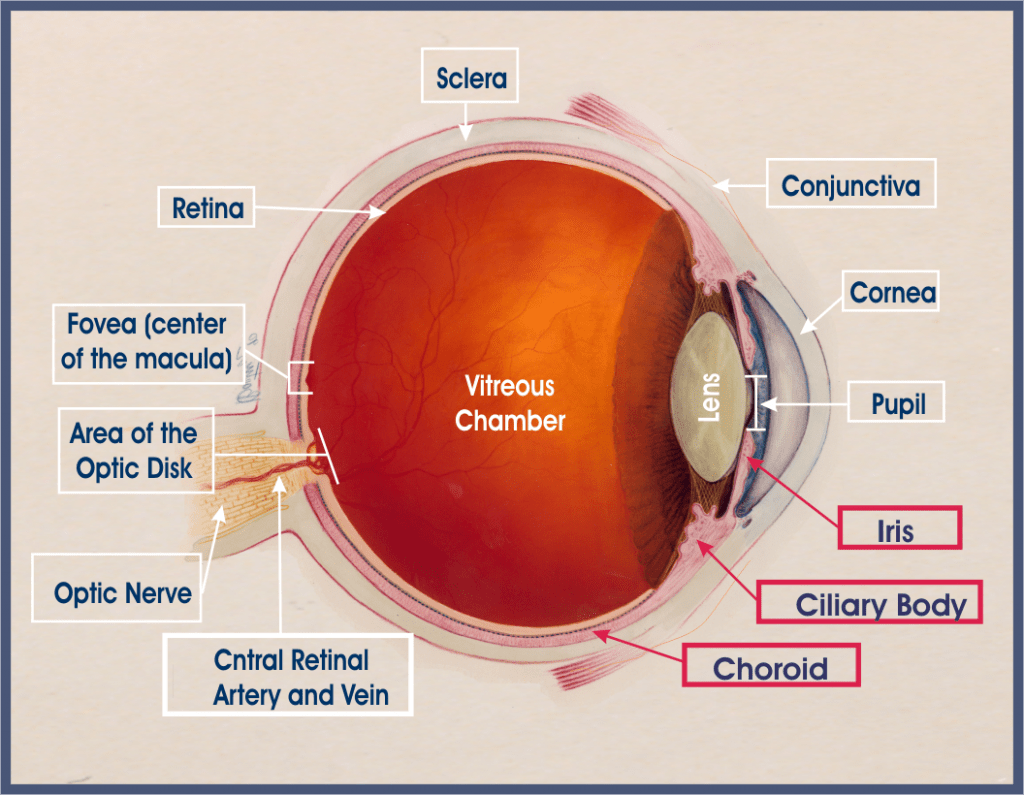
What are the functions of the uvea?
Regulation of intraocular pressure
Control of pupil size
Accommodation for near-vision
Nourishment of the retina
Absorption of excess light
What are some bacterial causes of keratitis?
Staphylococcus aureus
Staphylococcus epidermidis
Streptococcus pneumoniae
Pseudomonas aeruginosa
Chlamydia
Enterobacteriaceae
What are some viral causes of keratitis?
Canine herpesvirus 1 (CHV-1)
Feline herpesvirus 1 (FHV-1)
What are the general clinical signs of viral keratitis?
Punctate, dendritic or geographical corneal ulcers. They remain superficial if ulcerated.
Non-ulcerative appear as a circumferential ring of superficial corneal vascularisation with epithelial & subepithelial leukocyte infiltrate in the peripheral cornea.
What are the clinical signs of mycotic keratitis?
Ulcerative or non-ulcerative lesions. Candida infections often present as raised, yellowish-white, or greyish-white plaques or ulcerated lesions. Aspergillus infections are usually ulcerative with extensive stromal inflammation and melting

What are examples of non-ulcerative/superficial keratitis?
Pannus/chronic superficial keratitis
Pigmentary keratitis
Deep keratitis
What is pannus/chronic superficial keratitis/non-ulcerative keratitis?
A progressive, immune-mediated inflammatory condition affecting the cornea in dogs
What are the clinical signs of pannus?
Greyish-pink film on the eye progressing to corneal opacity due to cellular infiltration and vascularisation
What is pigmentary keratitis?
Deposition of pigment on the cornea secondary to chronic corneal irritation in dogs

What are the clinical signs of pigmentary keratitis?
Brown to black pigmentation on the cornea (starting at the limbus), corneal vascularisation, opacity, ulceration/erosions (in severe cases), ocular irritation, redness, tearing, squinting, and potential vision impairment/blindness if the central cornea is affected

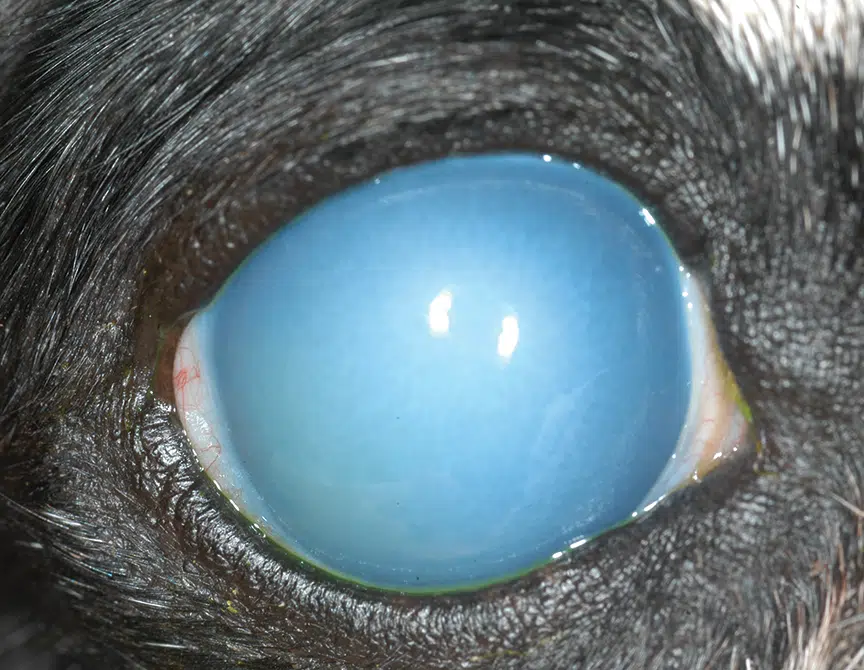
What are the clinical signs of deep keratitis?
Uveitis, corneal opacity ("blue eye"), and severe eye pain often disproportionate to clinical findings
How is keratitis treated?
Preventive ATB. Dexpanthenol gel (promote wetness). CSS (immune-mediated only if no ulceration is present), cyclosporin (immune-mediated), anti microbial/fungal etc- based on aetiology.
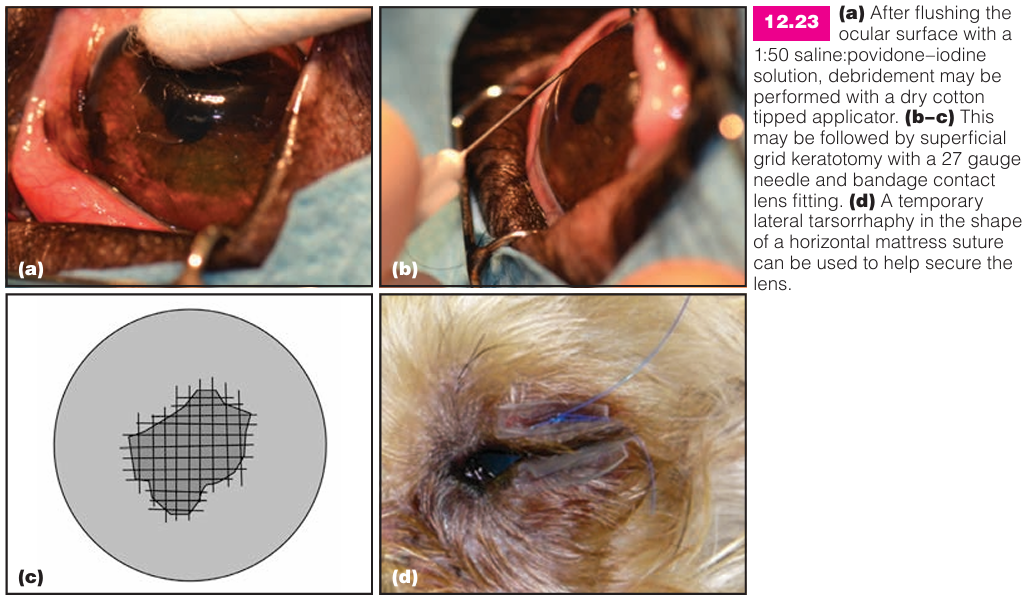
Grid keratotomy- needle scratch grid lines onto cornea, allowing healthy cell to grow → promote healing
Diamond burr debridement
What are the clinical signs of ulcerative keratitis?
Hyperlacrimation, blepharospasm, photophobia, conjunctival hyperaemia, corneal oedema, and potentially miosis with aqueous flare

How is ulcerative keratitis diagnosed?
Clinical signs and fluorescein stain retention by the corneal stroma

How is ulcerative keratitis treated?
Addressing the underlying cause
Topical antibiotics (gentamicin for G+, chloramphenicol for G-)
EDTA (protease inhibitor), topical atropine
Corticosteroids are contraindicated!
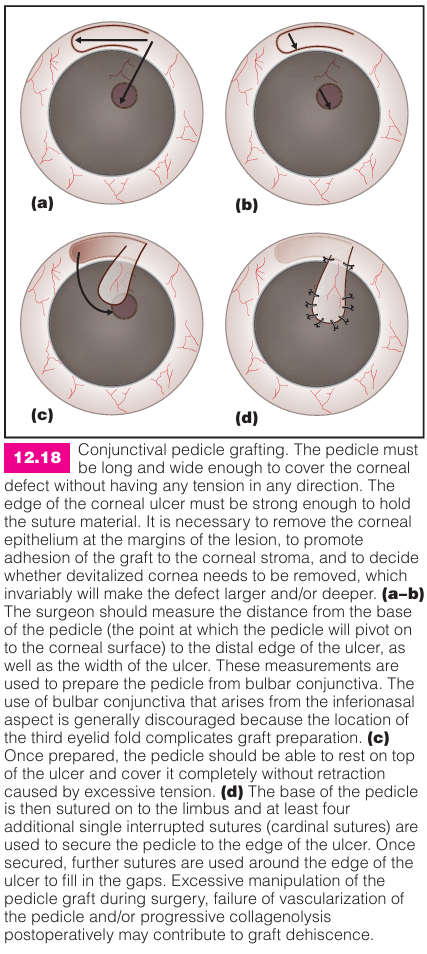
Pedicle grafts or corneal transplantations for deep ulcers
Grid keratotomy may be performed
What is a spontaneous chronic corneal epithelial defect/indolent ulcer/Boxer ulcer?
A superficial corneal ulcer with a non-adherent/peeled corneal edges. Recurrent uveitis may be present.

What is the aetiology of indolent ulcers?
Congenital, occurring spontaneously without trauma.

What are the clinical signs of indolent ulcers?
Blepharospasm, hyperlacrimation, conjunctival hyperaemia, eye discharge, ocular pain, corneal cloudiness, and sometimes visible defects or white spots on the cornea.
What are the differential diagnoses for indolent ulcers?
Traumatic ulcer, immune-mediated keratitis, infectious ulcer, and KCS.
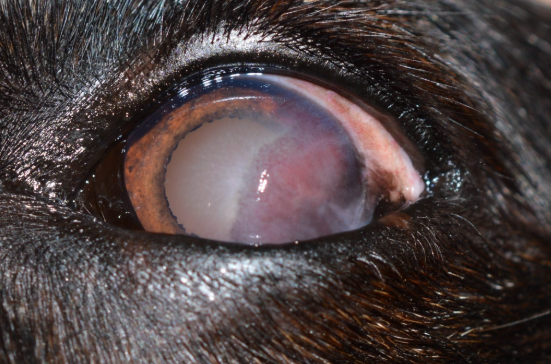
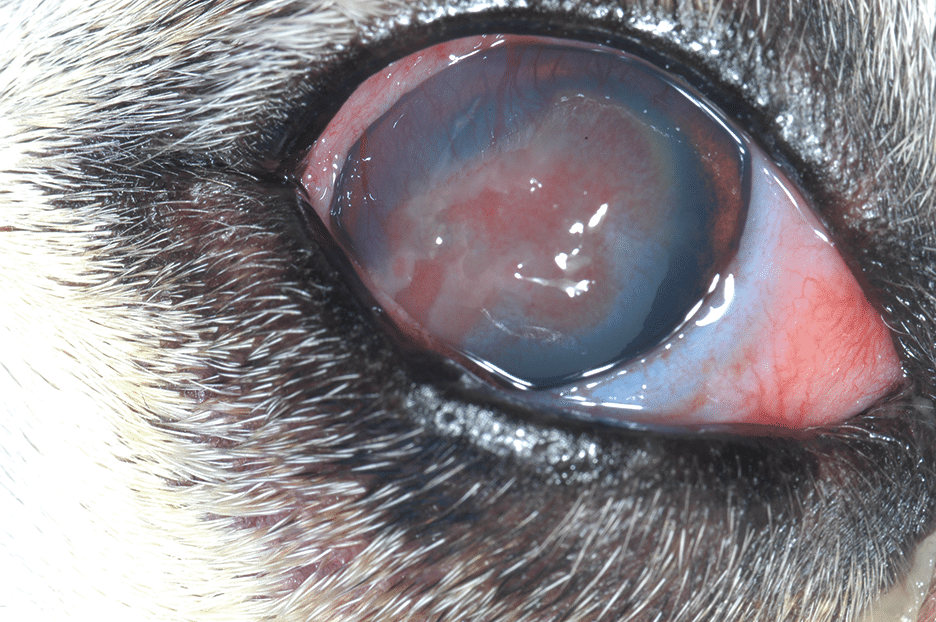
What is a melting ulcer?
Liquefaction of the corneal stroma by proteases produced by bacteria (e.g., Pseudomonas spp.), fungi, or inflammatory cells.
What are the clinical signs of melting ulcers?
Severe eye pain, redness, tearing, blurred vision, photophobia, eye discharge, and a white to yellow spot on the cornea that may have a mushy or gelatinous texture.

How are melting ulcers treated?
Topical and/or systemic antibiotics/antifungals
Topical anti-proteases (EDTA)
Lubricating eye drops
Antiviral drugs
Enucleation may be necessary in severe cases.
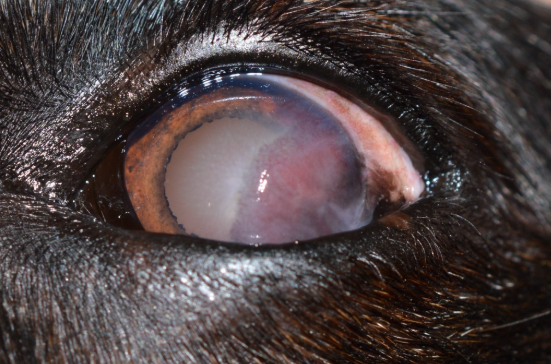
What are stromal abscesses?
A pocket of infection of corneal tissue that usually manifests as a light grey or soft pink haze in its early stages
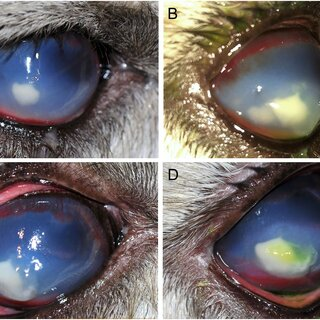
What is the aetiology of stromal abscesses?
Worsening of ulcers (rate of generation and protection mechanisms are unbalanced).
Can be due to eyelid abnormalities (ectopic cilia, entropion, irritants, trauma, immune-mediated, infection, dystrophy, precorneal tear film defects
What are the clinical signs of stromal abscesses?
Similar to ulcer but with the presence of yellow or white stromal infiltrate
How is a stromal abscess diagnosed?
Clinical signs
What is the treatment for stromal abscesses?
Topical: chloramphenicol, natamycin, atropine
Systemic: NSAIDs, trimethoprim, itraconazole
Surgery: debride, pedicle flap on penetrating keratoplasty
What is the aetiology of descetoceles and perforation?
Progression of deep corneal ulcers or trauma
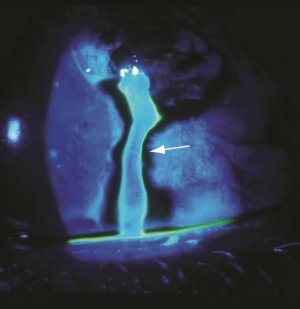
How are descemetoceles and perforations diagnosed?
Full eye examination. Fluorescein → Seidel test for presence of aqueous humour leakage from globe
What is an example of a neoplasm affecting the cornea?
Dermoid cyst
What are the clinical signs of a dermoid cyst?
Visible/palpable mass on the eyelid edge, usually near the lateral canthus, typically non-tender. May cause mild irritation or discomfort. Rarely, it may rupture causing acute inflammation and redness

How are dermoid cysts treated?
Surgical removal of abnormal tissue, including hair follicles, followed by lid margin closure.
Blepharoplasty may be needed for insufficient lid margin length
Sliding or grafting procedures may also be used for closure.
What is an example of a congenital defect affecting the cornea?
Persistent pupillary membrane
What is persistent pupillary membrane (PPM)?
A congenital defect involving remnants of foetal tissue in the pupil area. It can be iris-to-iris, iris-to-lens, or iris-to-cornea.
What are some surgical procedures for the cornea?
Superficial keratectomy
Keratoplasty/corneal grafting
Conjunctival flap
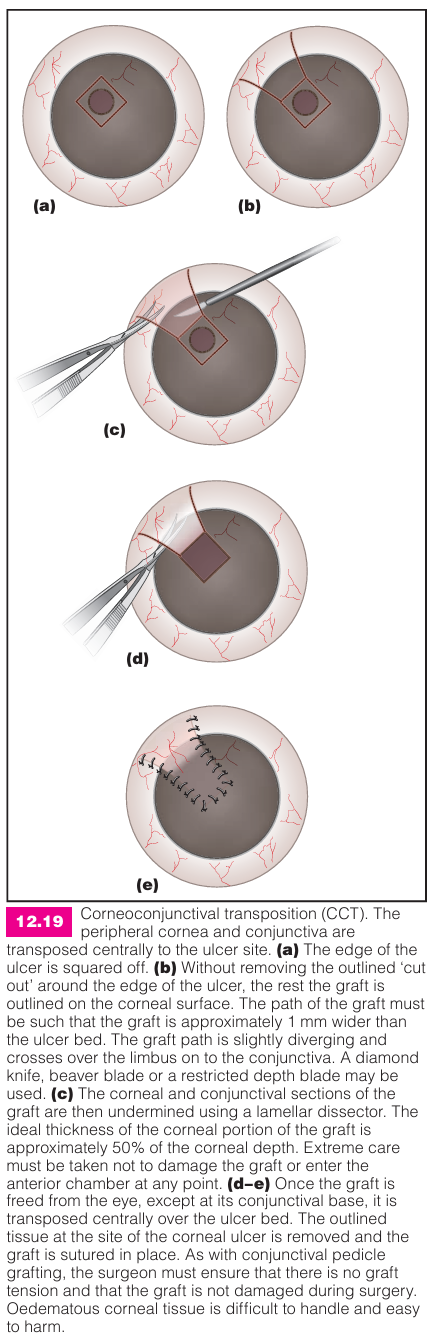
Corneoscleral transpositioning
What is a conjunctival flap?
A tissue covering used for deep or slow-healing corneal lesions.
What is corneoscleral transpositioning?
A corneal transplant using adjacent healthy corneal tissue and conjunctival tissue to cover the ulcer and provide structural support.
Why does the eye have an unpaired number of muscles?
Everything is paired except musculus retractor bulbi (unpaired)

What is an autoimmune cause for keratitis?
Pannus
Which breeds is keratoconjunctivitis sicca more common in?
Cocker spaniel and chihuahua
What methods can be used for diagnosis of KCS?
Schirmer Tear Test (under 8mm)
Fluorescein test