Chapter 18: Urinary system and acid base balance
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
77 Terms
What are the functions of the urinary system?
Elimination of wastes, water balance, regulation of PH
What is true metabolic waste?
Substances produced from metabolic processes that are toxic to the body and need to be eliminated, such as urea, creatine, and uric acids.
What organ is the most powerful long-term regulator of blood pH
The kidneys
What is the normal range of urine pH
4.5 to 8.0
How do the kidneys respond to excess hydrogen ions (acidosis
By actively secreting H⁺ ions into the urine, lowering urine pH
How do the kidneys respond to excess base (alkalosis
By excreting excess bicarbonate, raising urine pH
What is the role of the lungs in acid-base balance?
They regulate blood pH by controlling the amount of CO₂ exhaled.
What chemical equation summarizes the lungs' role in pH regulation?
CO₂ + H₂O ⇌ H₂CO₃ ⇌ H⁺ + HCO₃
What happens to the reaction above during acidosis (too much H⁺)?
It shifts left, forming CO₂ and H₂O, which are then exhaled to reduce acidity
How does breathing faster help correct acidosis
It removes more CO₂, shifting the equation left and reducing H⁺ in the blood
What happens if a person breathes too slowly (hypoventilates
CO₂ accumulates, shifting the reaction right, increasing H⁺ and causing acidosis
What condition results from too much CO₂ due to impaired respiration
Respiratory acidosis.
What condition results from excessive loss of CO₂ due to hyperventilation
Respiratory alkalosis
What type of acidosis is commonly seen in people with renal failure?
Metabolic acidosis.
What effect does eating acidic or basic foods (e.g., lemons, TUMS) have on the urinary system
The kidneys adjust acid/base excretion to maintain homeostasis regardless of diet
What is the normal pH of arterial blood
Around 7.4, which is slightly basic
What are the three major contributors to blood pH
Hydrogen ions, bicarbonate ions, and carbon dioxide
How does CO₂ affect blood pH
CO₂ combines with water to form carbonic acid, which increases H⁺ and lowers pH
What is the equation representing the acid-base buffer system in blood
CO₂ + H₂O ⇌ H₂CO₃ ⇌ H⁺ + HCO₃⁻
What role does bicarbonate (HCO₃⁻) play in pH regulation
It acts as a base, binding excess H⁺ to decrease acidity
What is an acid in terms of hydrogen ions?
A substance that donates H⁺ ions to a solution
What is a base in terms of hydrogen ions
A substance that binds or removes H⁺ ions from a solution.
What does pH measure?
The concentration of free hydrogen ions (H⁺) in a solution
What is the pH scale range
From 0 (very acidic) to 14 (very basic); 7 is neutral
What pH range is optimal for most biological enzymes
Between 6–8 (except stomach enzymes like pepsin, which prefer pH 2)
What is a buffer
A substance or system that minimizes changes in pH by neutralizing excess acids or bases
What is GFR (glomerular filtration rate)?
The amount of filtrate produced per minute by the kidneys
What happens if GFR is too high or too low?
High GFR: essential substances pass without reabsorption.
Low GFR: wastes may be retained due to excessive reabsorption
How does the body regulate GFR and reabsorption
Through mechanical (arteriole size) and chemical (hormonal) controls.
What triggers the release of ADH?
Dehydration or high blood solute concentration
What does ADH do
Increases water reabsorption in the kidneys, decreasing urine volume
What substances inhibit ADH
Caffeine and alcohol.
What does aldosterone do
Increases Na⁺ reabsorption and K⁺ secretion in the kidneys
What is the effect of aldosterone on urine and blood
Decreases Na⁺ in urine, increases K⁺ in urine; raises blood Na⁺ and blood pressure
What is the relationship between Na⁺ and K⁺ under aldosterone
Saving Na⁺ causes the body to lose K
What is tubular secretion?
The process by which substances that were not filtered out initially are added to the filtrate from the blood, mainly at the distal convoluted tubule
Where does tubular secretion primarily occur
In the distal convoluted tubule (DCT), but it can occur along the entire renal tubule
What types of substances are commonly secreted into the renal tubule
Potassium ions (K⁺), hydrogen ions (H⁺), and organic substances like drugs (e.g., penicillin).
What is the main purpose of tubular secretion
To eliminate waste and maintain pH balance and proper ion concentrations
What transport mechanism is primarily used in tubular secretion
Active transport
What is tubular reabsorption
The process of reclaiming water and useful solutes from the filtrate back into the blood
Where does the majority of reabsorption occur?
: In the proximal convoluted tubule (PCT
What are the two limbs of the loop of Henle, and what do they do?
The descending limb allows water reabsorption, and the ascending limb reabsorbs solutes like Na⁺
What happens if glucose is found in the urine
It indicates a condition like Diabetes Mellitus, where glucose levels exceed the renal threshold.
What is the renal threshold (tubular maximum
The maximum amount of a substance that can be reabsorbed by the kidneys
How much filtrate is reabsorbed during urine formation?
About 99% is reabsorbed; only about 1% leaves the body as urine
What processes are involved in tubular reabsorption
Diffusion, osmosis, and active transport
What are the peritubular capillaries
Capillaries that surround the renal tubules and collect reabsorbed substances to return them to the bloodstream
What are the three main steps in urine formation?
Filtration, reabsorption, and secretion.
Where does filtration occur in the nephron
In the glomerulus
What is the functional unit of the kidney?
The nephron
What creates the pressure that drives filtration in the glomerulus
The afferent arteriole is larger than the efferent arteriole, creating back pressure
What substances are filtered out of the blood during glomerular filtration?
Water, glucose, sodium ions, waste metabolites—anything smaller than proteins or blood cells
What substances do not get filtered during glomerular filtration
Proteins, red blood cells, white blood cells, and platelets
What is the fluid called immediately after filtration occurs
Filtrate
Approximately how much filtrate is produced daily
About 48 gallons
How much urine is typically excreted per day
About 1 liter or 1/4 gallon.
What are the two parts of the nephron’s anatomy?
Renal corpuscle (glomerulus and Bowman's capsule) and renal tubular system
What structure surrounds the glomerulus like a koozie around a can
Bowman's capsule.
What are the parts of the renal tubular system
Proximal convoluted tubule (PCT), loop of Henle, distal convoluted tubule (DCT), and collecting duct
What feature of the PCT increases its reabsorption capacity
Apical microvilli forming a brush border
What are the two limbs of the loop of Henle
Descending and ascending limbs
What is the main function of the loop of Henle in juxtamedullary nephrons
To create concentrated urine
How does the DCT differ from the PCT in appearance
The DCT has fewer and more spaced-out microvilli, lacking a brush border
What do the collecting ducts drain into
Minor calyces at the renal papillae
What is the pathway of urine after the collecting ducts?
Minor calyces → Major calyces → Renal pelvis → Ureter → Urinary bladder → Urethra
What are the two urethral sphincters and what are they made of?
Internal urethral sphincter (smooth muscle, involuntary) and external urethral sphincter (skeletal muscle, voluntary).
What arteries supply blood to the kidneys, starting from the aorta
Renal artery → Segmental arteries → Interlobar arteries → Arcuate arteries → Interlobular arteries → Afferent arteriole
What capillary networks follow the efferent arteriole
Peritubular capillaries and vasa recta.
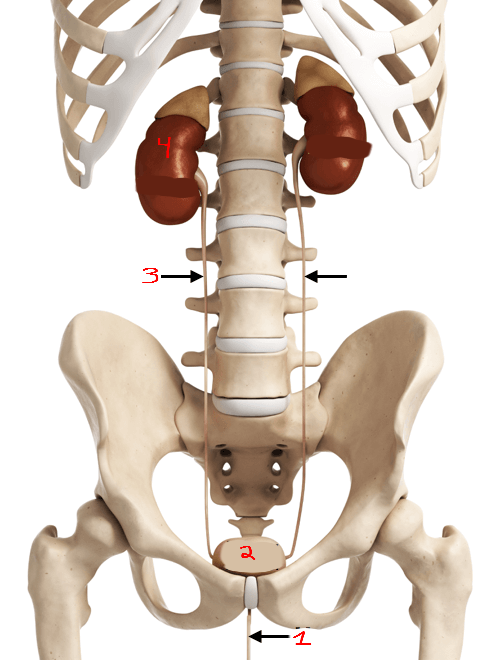
What is #1?
Urethra
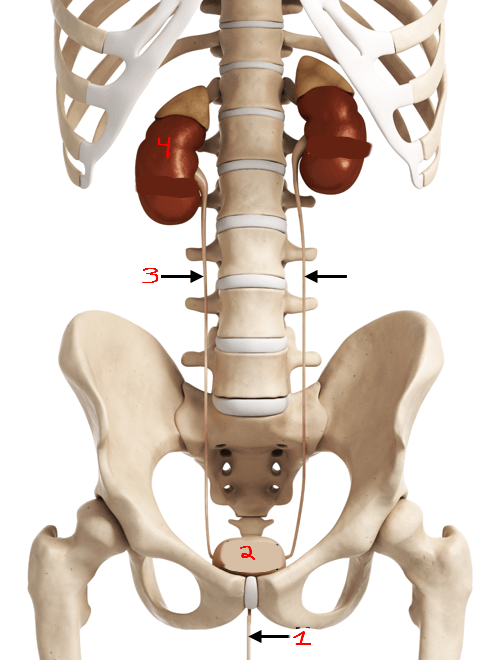
What is #2?
Bladder
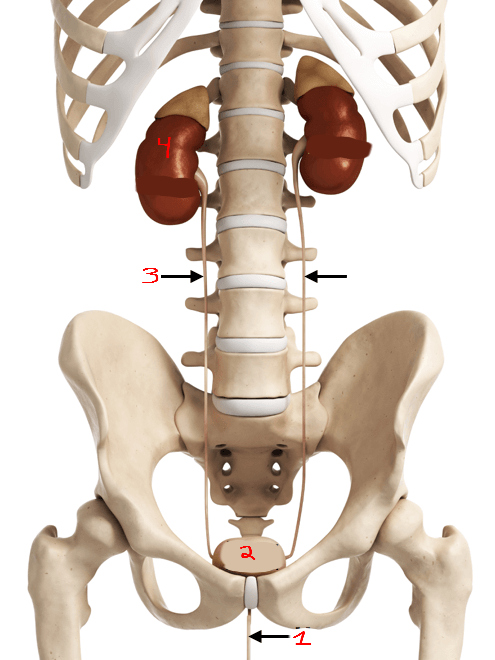
What is #3?
Ureter
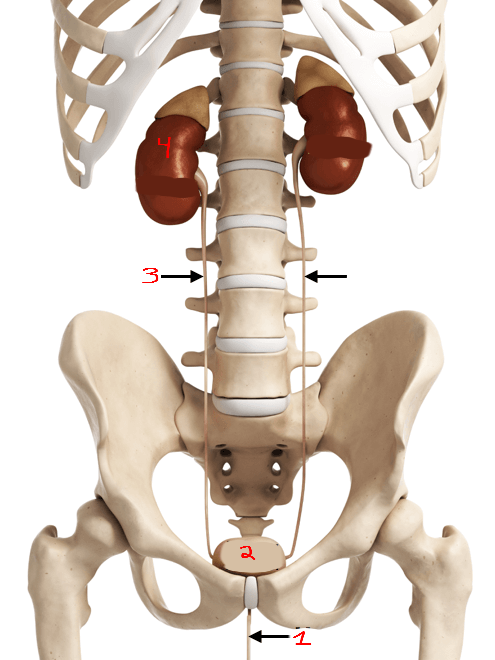
What is #4?
Kidneys
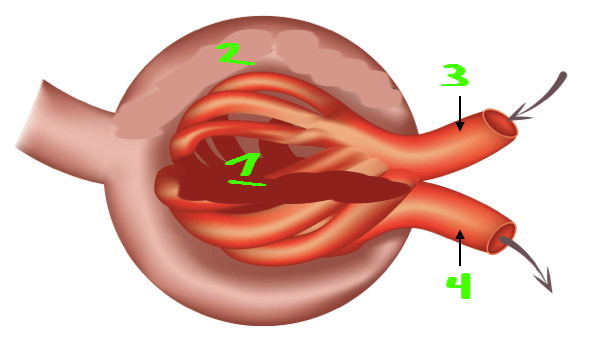
What is #1?
Glomerulus
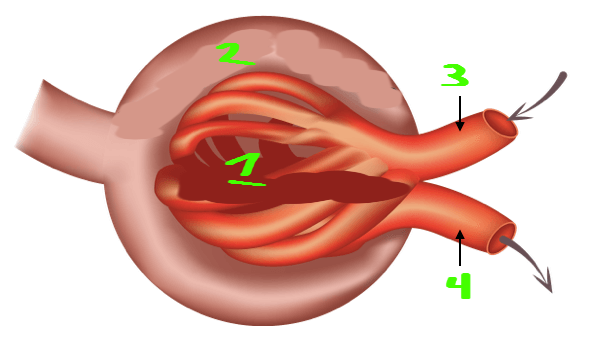
What is #2?
Bowmans capsule
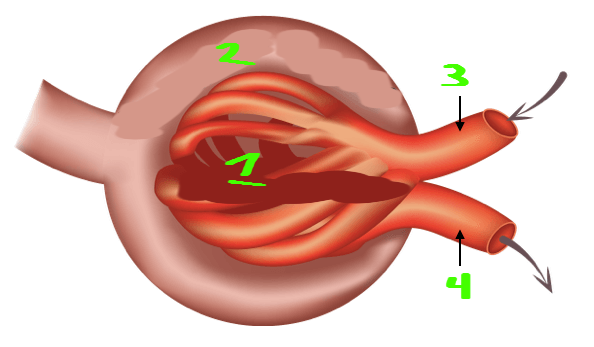
What is #3?
Afferent arteriole
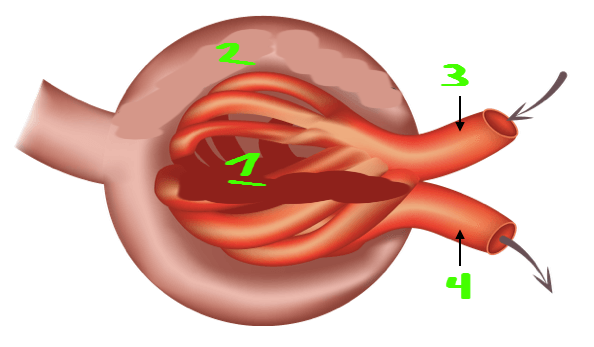
What is #4?
Efferent arteriole