Derm 2025 Pruritus and Itch drugs
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
66 Terms
Pruritis is the most ___.
It manifests as:
common dermatological skin problem of dogs and cats
manifests as scratching, chewing, licking, biting, and rubbing
The most common diseases that INDUCE pruritus are:
1) ectoparasite infestations
2) skin infections
3) allergies
Sarcoptic mange is quite contagious in dogs and a zoonotic disease. Lesions are primarily caused by the species:
Sarcoptes scabiei var. canis
Due to hypersensitivity to the lesions caused by Sarcoptes scabiei var. canis what are clinical signs patients may experience?
erythema and crust papules that are moderately to very pruritic.
lesions can be found on the face, ear margins, convex ears, sternum, and lateral aspects of limbs (a disease of extensor surfaces)
If the index of suspicion is high even though no mites were found it is appropriate to administer an acaricidal therapy to confirm diagnosis. What does this treatment consist of?
4 weekly lime sulfur, amitraz, or organophosphate dips
OR selamectin spot on treatment every 2 weeks for at least 3 treatments
OR you can also use off label treatment with isoxazoline class one weekly for 4 weeks
environmental treatment is recommended as well
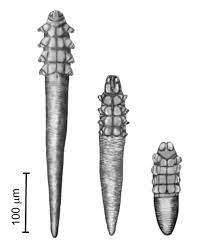
Pruritic inflammatory demodicosis is caused by a unique long bodied parasites called:
Demodex injai or long bodies Demodex canis
Cheyletiella, Lice, Trombiculids, and Otodectes can all cause ___ but only two can cause scaling of the skin
all cause pruritus
and Cheyletiella and extraauricular Otodectes causes:
True or false: Cheyletiella is zoonotic
True!
Pruritus is caused by active infection of ___ but hypersensitivity mechanisms (to their toxins) are also suspected to be involved.
Staphylococci
Always consider that majority of superficial pyoderma cases in dogs are due to __. Treatment for topical bacterial infections are:
due to underlying disease
combination of topical antiseptic/antibiotics with or without systemic antibiotics
Aside for bacteria, ___ is another common cause of pruritus and dermatitis in dogs. It will often colonize the skin secondary to other diseases. The pruritus could be related to inflammation or hypersensitivity mechanisms.
Malassezia (yeast)
Flea allergy dermatitis is caused by
Clinical signs include:
various hypersensitivity mechanisms directed against antigens of flea saliva
papules, pruritus, and secondary lesions on dorsolumbar area and hind legs
Treatment and control of flea allergy dermatitis is
using short-term coritcosteroid therapy and flea control
Oclacitinib and lokivetmab is also a good option
In the past, the term Atopic Dermatitis has been used for “a genetically predisposed inflammatory and pruritic skin disease with characteristic clinical features that is associated with IgE most commonly directed against environmental allergens. However, the new classification specifies it as:
a hereditary typically pruritic and predominantly T cell driven inflammatory skin disease involving interplay between skin barrier abnormalities, allergen sensitization, and microbial dysbiosis.
ALD and AD are different because ALD is used to classify
disease with the same clinical distribution as that of AD, but in which allergen-specific IgE cannot be demonstrated by usual methods.
Cutaneous adverse food allergies (AFRs) manifest as multiple diagnoses like food induced urticaria, pruritus without lesions, otitis alone, or in some dogs, atopic dermatitis. This means AFRs represent a ___ diagnosis
etiological
Do all dogs with AD have signs triggered by particular foods?
No (the prevalence between studies varies from 15 to 25% of AD dogs).
When do clinical signs of AD usually develop?
Early, most often before 3 yrs of age
Name 3 breeds at high risk of AD development
Golden retrievers, labradors, boxers
Give 3 examples of acute lesions of AD
Erythematosus macules, patches, and papules
What other clinical sign is commonly seen in dogs with food-induced AD?
Digestive signs such as vomiting, diarrhea, or soft stools.
How is AD diagnosed?
Based on suggestive clinical signs, history, and exclusion of other pruritic skin diseases.
List 3 of Favrot’s 2010 criteria for canine atopic dermatitis
Onset of signs under 3 years of age
Dog living mostly indoors
Glucocorticoid-responsive pruritus
chronic or recurrent yeast infections
Affected front feet
Affect ear pinnae
Non-affected ear margins
Non-affected dorso-lumbar area
How many criteria must be satisfied to establish a sensitivity of 85% and a specificity of 79% to differentiate dogs with AD from dogs with chronic or recurrent pruritus without AD.
A combination of 5 criteria must be satisfied
If a patient is being evaluated using Favrot’s 2010 criteria and meets a combination of 6 criteria, what effects does this have on the sensitivity and specificity of this test?
adding a 6th parameter increases the specificity to 89% but decreases the sensitivity to 58%
Are intradermal testing and allergen-specific IgE serology diagnostic tests for canine AD?
No, they are often positive in normal dogs
These tests should only be done AFTER a dog is diagnosed with AD to see what allergens they react to
When should intradermal testing and allergen-specific IgE serology be done?
Only to determine to what the dog has IgE hypersensitivity for later implementing allergen avoidance strategies or pursuing allergen-specific immunotherapy
Who should perform allergy testing and immunotherapy?
Dermatology specialists, unless you obtain additional training in this area.
Describe the therapeutic approach guidelines established by the International Task Force on Canine Atopic Dermatitis
The medications currently most effective in reducing chronic pruritus and skin lesions are topical and oral glucocorticoids, oral ciclosporin, oral oclacitinib, and, where available, injectable recombinant interferons. Allergen-specific immunotherapy and proactive intermittent topical glucocorticoid applications are the only interventions likely to prevent or delay the recurrence of flares of AD.
What type of clinical signs might patients with food allergens have?
Recurrent, year-round clinical signs and sometimes additional GI signs (soft stools, vomiting, diarrhea, increased fecal frequency)
What should all dogs with nonseasonal canine AD undergo?
1 or more dietary restriction-provocation trials to determine whether food allergens contribute to clinical signs
What is the current “gold standard” method for identifying food allergy in animals?
to observe improvement of canine AD clinical signs when the animal is fed a novel protein diet followed by recurrence of clinical signs when rechallenged with a previously fed food.
What is a novel protein usually combined with?
A carbohydrate
Name 3 examples of commercial novel protein source diets
RC Ultamino (feather protein), Purina Elemental (amino acid based diet) and RC Kangaroo/Potato
What is the minimum duration of a novel diet trial?
6 weeks
How long may some cases continue to improve on a novel diet?
Up to 8 to 12 weeks, depending on the resolution of clinical signs
What additional clinical signs influence the length of time required to feed the novel diet?
Severe skin inflammation, pruritus, ear infections, and superficial pyodermas
these must be controlled before improvement can be seen
What other hypersensitivities do most dogs with food allergies have?
Environmental or flea allergies
How can GI upset be avoided when introducing and rechallenging with a novel diet?
By initially mixing the old and new food (30/70%, then 50/50%) before complete transition to new or old food
When should adjunctive treatments be discontinued for patients with food allergy dermatitis in an ongoing food trial?
when the treatment resolves all concurrent clinical signs of pruritus and infection within 6-10 weeks of diet trial
If a patient is undergoing a novel protein diet trial and has completed their adjunctive therapies showing clinical signs have resolved, how long should the patient be maintained only on the novel food after discontinuing the adjunctive treatments?
for the following 2-3 weeks
What should happen if the clinical signs of pruritus and skin/ear infections do not recur during the 2-3 weeks on the novel food? This is after adjunctive treatment has been discontinued.
The patient is good to be rechallenged with the old diet
What is expected in dogs with food allergy after rechallenging with the old diet?
A relapse of clinical signs within 14 days.
What are the most common causes of canine AD in practice?
Environmental allergens from dust mites and pollens
What is likely most common allergen in atopic dogs?
House dust mite glycoproteins
What is the best course of action to help alleviate canine AD signs related to dust mites?
Reducing the number of mites and their allergens in the household
frequent and thorough pet mattress and environmental washing and vacuuming.
What is the sole causal treatment for environmental-induced canine AD?
Allergen immunotherapy (AIT), also known as desensitization or hyposensitization
How is AIT administered?
By administering gradually escalating quantities of relevant allergens subcutaneously or sublingually until immunologic tolerance to the allergens is established and relapses of canine AD signs are prevented.
What are the molecular and cellular mechanisms of AIT?
They include early mast cell and basophil desensitization effects; an induction of interleukin-10-secreting inducible regulatory T and B cells; regulation of IgE and IgG4 production; and inhibition of responses from eosinophils, mast cells, and basophils in the affected tissues.
What is considered the gold standard for in vivo challenge for patients undergoing AIT?
intradermal allergen injection
In vivo and in vitro assessments are options for patients opting for AIT. How do results of in vitro assessments of allergen-specific IgE (serum allergy testing) vary?
results very between laboratories, and no standardization exists for this test
Is AIT effective in every atopic dog?
No, but within 12 months approximately 50% and 80% of dogs with canine AD exhibit an improvement in clinical signs and/or a decrease in use of symptomatic medications, respectively.
What type of drugs should be given temporarily during AIT administration? What is their purpose?
Anti-inflammatory/anti-itch drugs
to maintain a good quality of life until AIT is judged to be effective
What do activated cells in the immune network up and downregulate that causes inflammation in canine AD?
various modulators, cytokines, chemokines that promote pathology in food and environment-induced canine AD skin lesions
How long does it take for symptomatic intervention to resolve clinical signs in dogs with food induced atopic disease on a diet trial?
6-10 weeks
Give an example of an approach to manage canine AD
Daily, intensive systemic and topical glucocorticoid administration for a few weeks until clinical signs are resolved “get control” followed by intermittent topical glucocorticoids twice weekly to previously affected areas, with a goal of suppressing subclinical inflammation “keep control”
How do glucocorticoids work?
they are fast-acting medications that deactivate many inflammatory cells and reduce inflammatory/itch mediators
What are the adverse effects associated with prolonged systemic glucocorticoid use?
PU/PD, polyphagia, muscle and skin atrophy, bacterial and fungal infections, demodicosis, and iatrogenic hyperadrenocorticism
Name two examples of medium-potency glucocorticoid sprays.
Triamicinolone acetonide (Genesis) and a diester hydrocortisone aceponate (Cortavance)
What is a highly potent diester steroid available as a cream?
Mometasone furoate
How should topical steroids be applied to clear localized skin lesions?
Daily application for 2-4 weeks
After clearing localized skin lesions, how should topical steroids be used?
Intermittent use of the same product (2-3 times per week) on the previously affected skin, even if visible lesions have disappeared.
When are short-acting oral glucocorticoids recommended?
If canine AD signs are too extensive to be controlled with only topical formulation, then short-acting oral glucocorticoids are recommended in conjugation with topical steroids.
What glucocorticoid-antihistamine combination can be used to reduce the adverse effects and dose of oral glucocorticoids?
Temaril-P (trimeprazine 5mg/ prednisolone 2mg)
What is the effect of antihistamine trimeprazine?
It seems to potentiate the low dose of prednisolone, achieving a steroid-sparing effect
What medications may help avoid adverse effects associated with long term systemic glucocorticoids?
steroid-sparing agents