M3.7 -Exchange surfaces and breathing
1/130
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
131 Terms
how come diffusion alone is enough to supply the needs of single-celled organisms?
The metabolic activity of unicellular organisms is usually low
so O2 demands and CO2 production of the cell are low
The SA:V of the organism is large.
so the distance which substances have to diffuse over is short
why do larger organisms need specialized exchange surfaces?
bigger organisms = smaller SA:V
distance that substances need to travel from outside to reach the cells at centre of the body get longer
so it is impossible to absorb enough O2 through the available SA to meet needs of the body
high metabolic demands
need lots of O2 for cellular respiration
lots of waste products produced that need to be removed
Is metabolic activity higher in unicellular or multicellular organisms?
multicellular
Features of an efficient exchange system
large SA:V
good blood supply/ ventilation »» CG
Short diffusion distances
why is an increased Surface Area important for efficient gaseous exchange?
increases the area over which gases and other substances can be transported into and out of the organism, via diffusion and active transport.
example of large SA
(to increase rate of diffusion)
root hair cells - plants
villi - small intestine
folded membranes -mitochondria
why are thin layers/walls/short distances important for efficient gaseous exchange?
distances which substances diffuse over are short
so rate of diffusion is faster and more efficient
as particles do not have to travel as far
examples of thin layers
(to increase rate of diffusion)
alveolar walls- lungs
villi - small intestine
why is a good blood supply/ steep concentration gradient important for efficient gaseous exchange?
steeper CG = Faster diffusion
good blood supply means substances are constantly delivered to and removed from exchange surface
so more efficient exchange
examples of good blood supply
(to increase rate of diffusion)
alveoli - lungs
gills - fish
villi- small intestine
why is good ventilation important for efficient gaseous exchange?
creates steep CG
create a high partial pressure (of oxygen in the alveoli.)
examples good ventilation
(to increase rate of diffusion)
alveoli- lungs
gills- fish
(flow of water carrying dissolved O2)
why do large organisms/ mammals have a high metabolic rate?
they are active
maintain their body temperature independent of the environment
what does the mammalian gaseous exchange system consist of?
nasal cavity
trachea
bronchus
bronchioles
alveoli (lungs)
Passage of air flow through the body
NASAL CAVITY - inhalation
TRACHEA - continues below larynx
BRONCHUS - trachea divides (forms left bronchus and right bronchus)
BRONCHIOLES - bronchi divide into smaller tubes
ALEVOLI - main site of gas exchange
features of the nasal cavity
Large SA and good blood supply
hairy lining
moist surfaces
importance of the large SA and good blood supply in the nasal cavity
Warms the air to body temp
» so air entering lungs is similar temp to body temp
Ensures appropriate exchange of carbon dioxide and oxygen,
To prevent diseases.
importance of the hairy lining in the nasal cavity
secretes mucus to trap dust and bacteria
this protects delicate tissue from irritation and infection
(provides additional humidity to the inhaled air)
importance of moist surfaces in the nasal cavity
increases humidity of incoming air
reduces evaporation from exchange surfaces
ensures cilia do not dry out and continue functioning
features of the trachea
strong, flexible cartilage
ciliated epithelial cells
goblet cells
importance of cartilage in the trachea
prevents collapsing of trachea
structure of cartilage in trachea and importance of that structure
rings of cartilage
rings are incomplete so food can easily move down the oesophagus behind the trachea
importance of ciliated epithelial cells in trachea
cilia beat and move the mucus along
move any trapped dirt and microorganisms away from lungs
where does most of the wafted mucus from the cilia end up?
into the throat
swallowed and digested
what effect does cigarette smoke have on cilia?
stops cilia beating
paralyze the cilia and eventually destroy them
what causes ‘smokers cough’
toxins destroy cilia
cilia are less effective at keeping lungs clear
coughing attempts to remove mucus from lungs
importance of goblet cells in trachea
secrete mucus onto lining of trachea
to trap dust and microorganisms
(that have escaped the nose lining)
where are goblet cells located?
between and below the epithelial cells
features of bronchi (bronchus)
similar structure to trachea
but
narrower in size
feature of bronchioles
smaller bronchi but no cartilage rings
walls of smooth muscle
lined with a thin layer of flattened epithelium
clusters of alveoli at the end
importance of smooth muscle in bronchioles
smooth muscles contract - bronchioles constrict
smooth muscles relax - bronchioles dilate
This changes the amount of air reaching the lungs
importance of thin layer of flattened epithelium in bronchioles
makes gaseous exchange possible
permits rapid diffusion of oxygen and carbon dioxide.
features of alveoli
thin flattened epithelial cells
collagen and elastic fibres
large SA:V
good blood supply
coated in lung surfactant
diameter of alveoli
200-300 μm
what is elastic recoil of the lungs?
The rebound of the lungs
after having been stretched by inhalation
importance of flattened thin epithelial cells in alveoli
single epithelial cell thick
short diffusion distance
between the air in the alveolus and the blood in the capillaries
diffusion rate much faster more efficient
importance of elastic fibres in alveoli
allow alveoli to stretch during inhalation
as return to resting size, air is squeezed out
» elastic recoil
what are elastic fibres in the alveoli composed of?
elastin
how many alveoli are there per adult lung?
300-500 million
what is the alveolar SA for gaseous exchange in the two lungs combined?
50-75m²
why is a large SA of the alveoli essential for gaseous exchange in the lungs?
speeds up diffusion because gases have more area over which to diffuse.
otherwise without the alveoli, the lungs would not be big enough for
amount of oxygen needed to diffuse into the body
How many capillaries supply the millions of alveoli in each lung?
280 million capillaries
importance a good blood supply in the alveoli
constant flow of blood through capillaries
» brings CO2 and carries off O2
maintains a steep CG for CO2 and O2
between air in the alveoli and blood in the capillaries
so rate of diffusion is faster
importance of lung surfactant in the alveoli
keeps alveoli inflated
prevents alveoli from collapsing
reduces surface tension at the air-liquid interface in the alveoli
allows O2 to dissolve in water before in blood
»increases rate of diffusion
define surfactant
substance which reduces tension and helps substances dissolve in water
what is the lung surfactant composed of? (chemical mixture)
phospholipids
hydrophilic proteins
hydrophobic proteins
where is the lung surfactant found?
coats the surfaces of the alveoli
what happens if surface tension is too high?
alveoli can’t expand anymore
lung collapse
unable to breathe in
what creates surface tension?
alveolar walls lined with thin film of water
tension from the forces acting on the liquid surfaces
function of the rib cage
protects vital organs in the thoracic cavity
assists in respiration
supports the weight for the upper extremities
how many types of rib are there?
true ribs
false ribs
floating ribs
what are true ribs?
1-7 ribs are true ribs
they articulate directly with sternum by costal cartilages
what are false ribs?
( vertebrochondral ribs)
indirectly articulate with the sternum
their costal cartilages are attached to the costal cartilage of the seventh rib
8,9,10 are false ribs
what are floating ribs?
do not articulate with the sternum at any point
11, 12 are floating ribs
structure of ribs, rib cage
basket-like structure
expansible and semi-rigid
twelve pairs of ribs
formed from ribs - corresponding attachments to sternum and vertebral column
protects lungs and heart » 2 vital organs
what happens to external intercostal muscles during inhalation?
contract
what happens to the ribs during inhalation?
move upwards and outwards
what causes the ribs to move upwards and outwards during inhalation?
the diaphragm and external intercostal muscles contract
what happens to the diaphragm during inhlation?
contracts
flattens
lowers
what happens to the internal intercostal muscles during inhalation?
relax
what happens to the volume of the thorax during inhalation?
increases
why does the pressure in the thorax decrease during inhalation?
volume of thorax increases
so pressure decreases
pressure and volume are inversely proportional at a constant
During inhalation, how does the air pressure in the thorax compare to atm?
pressure in thorax reduced to below atmospheric air
causes a pressure gradient
so air from outside moves inwards - down a pressure gradient
equalises pressure inside and outside chest
what happens to the alveoli during inhalation?
they stretch
Describe the process of inspiration
external intercostal muscles contract whereas the internal ones
relax
cause the ribs to raise upwards, outwards
The diaphragm contracts, flattens.
the intercostal muscles and diaphragm cause the volume inside the thorax to increase
thus lowering the pressure inside the thorax
» below ATM
difference between the pressure inside lungs and ATM creates a pressure gradient
causing the air to enter the lungs (thru nasal cavity etc)
» until pressure inside and outside lungs is equalised
is Inspiration an energy using process?
yes - active phase of ventilation
Is expiration an energy using process?
no - Expiration is passive in the normal individual during quiet breathing
what allows expiration to be a passive process?
elastic recoil of the lungs
relaxation of inspiratory muscles
energy stored in the elastic lung tissue during inspiration being sufficient.
what happens to the diaphragm during expiration?
relaxes
moves upwards
creates resting dome-shape
what happens to external intercostal muscles during expiration?
relax
what happens to internal intercostal muscles during expiration?
contract
what happens to the ribs during expiration?
move down
inwards
under gravity
what happens to the elastic fibres in the alveoli during expiration?
return to normal length
elastic recoil
why do alveoli shrink/ recoil during expiration?
to expel CO2 out of the lungs
what happens to the volume of the thorax during expiration?
decreases
what pressure changes take place in the thorax during expiration?
pressure inside thorax increases
to above atm
creates a pressure gradient
so air from inside is pushed outwards - down a pressure gradient
equalises pressure inside and outside chest
Describe the process of expiration
external intercostal muscles relax whereas the internal ones contract
cause the ribs to move downwards, inwards
The diaphragm relaxes, moves up, forms dome-shape.
the intercostal muscles and diaphragm cause the volume inside the thorax to decrease
thus increasing the pressure inside the thorax
» above ATM
difference between the pressure inside lungs and ATM creates a pressure gradient
causing the air to move out of the lungs (thru nasal cavity etc)
» until pressure inside and outside lungs is equalised
process of forced expiration
uses energy
internal intercostal muscles contract
pulls ribs down hard, fast
abdominal muscles contract
forces diaphragm to move up (dome-shape)
increases pressure in lungs rapidly
what happens to the cells lining the bronchioles during an asthma attack?
release histamines
what effect does histamine have during an asthma attack?
histamine chemicals cause epithelial cells to become
inflated and swollen
stimulate excess mucus production in goblet cells
smooth muscle in bronchiole walls to contract
» the airways narrow, fill with mucus, difficult to breathe
how is asthma treated/ helped?
relievers
preventers
where are asthma treating drugs delivered to in the body?
straight into the breathing system
using an inhaler
how do relievers work in treating asthma?
give immediate relief from symptoms
they attach to active sites
on cell surface membranes of smooth muscle cells
in the bronchioles
makes them relax and dilate the airways
how do preventers work in treating asthma?
they are often steroids
taken every day
to reduce sensitivity of lining of the airways
what does lung surfactant consist of?
phospholipids
hydrophilic proteins
hydrophobic proteins
when do alveolar cells produce lung surfactant in babies during pregnancies?
alveolar cells do not produce enough lung surfactant
until the 30th week of pregnancy
why is lung surfactant a concern in premature babies?
if baby is premature
(born before 37 weeks)
they alveolar cells may not have produced enough surfactant yet
so due to not enough surfactant
the alveoli collapse with each breath
as they collapse , damaged cells collect in the airways
leads to death
why can’t premature babies produce lung surfactant?
due to the immature development of type II pneumocytes
In what ways can the capacity of the lungs be measured?
A peak flow meter
Vitalographs
A spirometer
what is a peak flow meter?
show the amount and rate of air that can be forcefully breathed out of (and therefore into) the lungs (PEF)
useful quick measure
when is a peak flow meter often used?
in Asthma patients
» monitor how well lungs are working
» helps to diagnose Asthma
what is PEF (peak expiratory flow)?
amount and rate of air that can be forcefully breathed out of the lungs.
how to interpret results of a peak flow meter?
When a patient is well their PEF is higher
when the airways are narrow (as in asthma) » PEF is lower.
what is a vitalograph?
(more complex peak flow meters)
measures the FEV in 1 second » (FEV1)
measures FVC
produces graph, plots volume against time
what is FEV1 ?
Forced expiratory volume (in 1 second)
volume of air (in litres) exhaled in the 1st second during forced exhalation
after maximal inspiration.
what is FVC?
Forced vital capacity
volume of air that can be forcibly exhaled
from lungs
after taking the deepest breath possible
how to interpret vitalograph?
If the FVC and the FEV1 are within 80%
results considered normal
normal ratio value for the FEV1/FVC ratio is 70%
what is a spirometer?
measures different aspects of lung volume
investigate breathing patterns
how well lungs are functioning
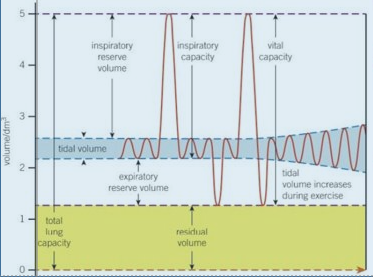
spirometer readings