Spinal Cord Injuries Overview
1/33
Earn XP
Description and Tags
This set of flashcards covers key concepts related to spinal cord injuries, focusing on causes, symptoms, classifications, management, complications, and the psychological impact on patients.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
What is a spinal cord injury (SCI)?
An injury to the spinal cord, vertebral column, supporting soft tissue, or intervertebral discs caused by trauma.
What are the common causes of spinal cord injuries?
Motor vehicle crashes, falls, violence (predominantly gunshot wounds), and sports-related injuries.
What percentage of spinal cord injury patients are males?
78%.
What is the average age of injury for spinal cord injuries?
43 years of age.
What are the major causes of death in patients with SCI?
Pneumonia, pulmonary embolism, and sepsis.
What classifications exist for spinal cord injuries?
Primary injuries and secondary injuries.
What is complete spinal cord lesion?
Signifies loss of both sensory and voluntary motor communication from the brain to the periphery.
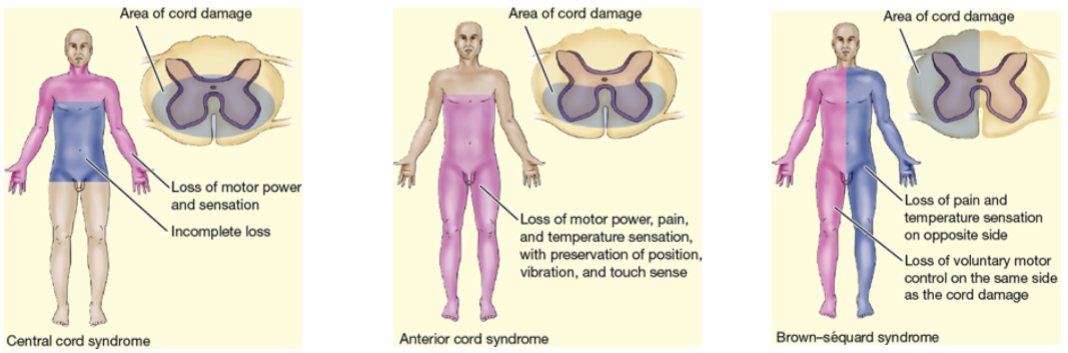
What symptoms characterize Central Cord Syndrome?
Motor deficits in the upper extremities, sensory loss more pronounced in the upper extremities, and variable bowel/bladder dysfunction.
What are the manifestations of Anterior Cord Syndrome?
Loss of pain, temperature, and motor function below the level of the lesion; light touch and vibration sensation remain intact.
What is autonomic dysreflexia?
An acute life-threatening emergency due to exaggerated autonomic responses to stimuli, characterized by severe headache and paroxysmal hypertension.
What is the major goal of management for spinal cord injuries?
Prevent secondary injury and observe for progressive neurologic deficits.
Define neurogenic shock in the context of SCI.
Loss of autonomic nervous system function below the level of the lesion, affecting vital organ function.
What is the role of early surgical intervention in SCI?
Early surgical stabilization may improve clinical outcomes by preserving neurologic function.
What occurs immediately after spinal cord injury to the bladder and bowel?
The bladder becomes atonic and cannot contract, leading to urinary retention.
What complications are common in patients with spinal cord injuries?
Pressure injuries, urinary tract infections, contractures, and respiratory infections.
What interventions can prevent venous thromboembolism (VTE) in SCI patients?
Anticoagulation therapy, range-of-motion exercises, anti-embolism stockings, and adequate hydration.
What is the importance of nutritional support in patients with SCI?
To prevent secondary complications, maintain immune function, and support repair of tissues.
How does spasticity affect patients with SCI?
Increased muscle tone and spasms can interfere with rehabilitation, ADLs, and quality of life.
What is the significance of a bowel training program for SCI patients?
To establish bowel evacuation through reflex conditioning and prevent complications like constipation.
What psychological challenges do patients with SCI face?
Grief, denial, anger, depression, and coping with changes in self-identity and functioning.
Spinal Cord Injury
• 294,000 persons in the United States live with disability from SCI
• Causes include MVAs, falls, violence (gunshot wounds), and sports-
related injuries
• Risk factors include young age, male gender, alcohol and drug use
• Major causes of death are pneumonia, pulmonary embolism (PE),
and sepsis
Pathophysiology of SCI
• The result of concussion, contusion, laceration, or compression of
spinal cord
• Primary injury is the result of the initial trauma and usually
permanent
• Secondary injury resulting from SCI include edema and
hemorrhage
• Major concern for critical care nurses
• Treatment is needed to prevent partial injury from developing into
more extensive, permanent damage
Manifestations of pf SCI
Complete - total loss of sensory and motor function below the injury site. Incomplete - preservation of some sensory and/or motor function below the injury site.
Assessment of the Patient with ACUTE SCI
• Monitor respirations and breathing pattern
• Lung sounds and cough
• Monitor for changes in motor or sensory function; report
immediately
• Monitor for bladder retention or distention, gastric dilation, and ileus
• Temperature; potential hyperthermia
• Assess for spinal shock
Spinal and Neurogenic Shock
Spinal shock
• A sudden depression of reflex activity below the level of spinal
injury
• Muscular flaccidity, lack of sensation and reflexes
Neurogenic shock
• Caused by the loss of function of the autonomic nervous
system
• Blood pressure, heart rate, and cardiac output decrease
• Venous pooling occurs because of peripheral vasodilation
• Paralyzed portions of the body do not perspire
A patient is just admitted to the hospital following
a spinal cord injury at the level of T4. A priority of
nursing care for the patient is monitoring for
a. return of reflexes.
b. bradycardia with hypoxemia.
c. effects of sensory deprivation.
d. fluctuations in body temperature.
bradycardia with hypoxemia. This is a common complication of neurogenic shock, which can occur after a spinal cord injury. It is crucial to monitor heart rate and oxygen levels, especially after high thoracic or cervical injuries.
Management of the acute Phase of SCI
• Pharmacological Therapy
• Respiratory Therapy
• Skeletal Reduction/Traction
• Surgical Management
Goals & interventions for the Patient with
SCI
Major goals may include:
• Improved breathing pattern and airway clearance
• Improved mobility
• Prevention of injury due to sensory impairment
• Maintenance of skin integrity
• Relief of urinary retention
• Improved bowel function
• Decreasing pain
• Recognition of and absence of complications
Possible complications for a patient with sci
•Venous thromboembolism
•Orthostatic hypotension
•Autonomic dysreflexia
Autonomic Dysreflexia
• Acute emergency!
• Occurs after spinal shock has resolved and may occur years after
the injury
• Occurs in persons with SC lesions above T6
• Autonomic nervous system responses are exaggerated
• Symptoms include severe pounding headache, sudden increase
in blood pressure, profuse diaphoresis, nausea, nasal
congestion, and bradycardia
• Triggering stimuli include distended bladder (most common
cause), distention or contraction of visceral organs (e.g.,
constipation), or stimulation of the skin
During assessment of a patient with a spinal cord
injury at the level of T2 at the rehabilitation center,
which finding would concern the nurse the most?
a. A heart rate of 92
b. A reddened area over the patient’s coccyx
c. Marked perspiration on the patient’s face and
arms
d. A light inspiratory wheeze on auscultation of the
lungs
Marked perspiration on the patient’s face and
arms. This may indicate autonomic dysreflexia, a potentially life-threatening condition, especially for patients with spinal cord injuries above T6.
Nursing Interventions for Autonomic Dysreflexia
• Place patient in seated position to lower BP
• Rapid assessment to identify and eliminate cause
• Empty the bladder using a urinary catheter or irrigate or
change indwelling catheter
• Examine rectum for fecal mass
• Examine skin
• Examine for any other stimulus
• Administer ganglionic blocking agent such as hydralazine
hydrochloride IV
• Label chart or medical record that patient is at risk for autonomic dysreflexia
• Instruct patient in prevention and management
A patient with an SCI at T5 begins to complain of a severe
headache and is diaphoretic and nauseated. Which nursing
interventions would be appropriate? SATA
A. Place the patient immediately in a sitting position
B. Lower the patient to a flat, side-lying position
C. Assess for bladder distention
D. Assess the rectum for a fecal mass
A. Place the patient immediately in a sitting position
C. Assess for bladder distention
D. Assess the rectum for a fecal mass.
Long-term Goals for the Patient with
Tetraplegia or Paraplegia
• Attainment of some form of mobility
• Maintenance of healthy, intact, skin
• Achievement of bladder management without infection
• Achievement of bowel control
• Achievement of sexual expression
• Strengthening of coping mechanisms
• Knowledge of long-term management
• Absence of complications