Auer and Stick Chapter 6: Metabolism and Nutritional Support of the Surgical Patient
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
How long can a horse with a BCS 4-5/9 tolerate food deprivation?
3-4 days
How are energy demands met during the period of starvation prior to surgery?
Energy demands are met by glycogen reserves, with little effect on overall metabolism
Body Condition Score 1
Poor: Animal extremely emaciated. Spinous processes, ribs, tailhead, hooks, and pins projecting prominently. Bone structure of the withers, shoulders, and neck easily noticable. No fatty tissue can be felt.
Body Condition Score 2
Very thin: Animal emaciated. Slight fat covering over base of spinous processes, transverse processes of lumbar vertebrae feel rounded. Spinous processes, ribs, tailhead, hooks, and pins prominent. Withers, shoulder, and neck structures faintly discernible.
Body Condition Score 3
Thin: Fat buildup about halfway on spinous processes, transverse processes cannot be felt. Slight fat cover over ribs. Spinous processes and ribs easily discernible. Tailhead prominent, but individual vertebrae cannot be visually identified. Hook bones appear rounded but easily discernible. Pin bones not distinguishable. Withers, shoulder, and neck accentuated
Body Condition Score 4
Moderately thin: Negative crease along back. Faint outline of ribs discernible. Tailhead prominence depends on conformation; fat can be felt around it. Hook bones not discernible. Withers, shoulder, and neck not obviously thin.
Body Condition Score 5
Moderate: Back level. Ribs cannot be visually distinguished but can be easily felt. Fat around tailhead beginning to feel spongy. Withers appear rounded over spinous processes. Shoulders and neck blend smoothly into body.
Body Condition Score 6
Moderate to fleshy: May have slight crease down back. Fat over ribs feels spongy. Fat around tailhead feels soft. Fat beginning to be deposited along the sides of withers, behind shoulder, and along the sides of the neck
Body Condition Score 7
Fleshy: May have crease down back. Individual ribs can be felt, noticeable filling of fat between ribs. Fat around tailhead is soft. Fat deposited along withers, behind shoulder, and along the neck
Body Condition Score 8
Fat: Crease down back. Difficult to feel ribs. Fat around tailhead very soft. Area along withers filled with fat. Area behind shoulder filled in flush. Noticeable thickening of neck. Fat deposited along inner buttocks.
Body Condition Score 9
Extremely fat: Obvious crease down back. Patch fat appearing over ribs. Bulging fat around tailhead, along withers, behind shoulders, and along neck. Fat along inner buttocks may rub together. Flank filled in flush
Pure Protein/Calorie Malnutrition
A decline in blood glucose concentration occurs with food deprivation; insulin levels fall and energy demands are initially met via glycogenolysis which increases the breakdown of liver glycogen stores
As starvation progresses, glycogen is mobilized within other tissues, including muscle
Lipid mobilization is triggered by alterations in insulin or glucagon levels and the activity of hormone-sensitive lipase
As glucose becomes limited, many body tissues begin to rely on fatty acid oxidation and the production of ketone bodies as energy sources
Glycerol produced from lipid degradation, lactate from the Krebs cycle, and amino acids from muscle tissue breakdown continue to be used for gluconeogenesis to provide energy to glucose-dependent tissues (CNS and RBCs)
Increases in circulating levels of growth hormone, glucagon, epinephrine, leptin, and cortisol, and deceases in insulin and thyroid hormones Afferent stimulus for the hypothalamic response to starvation which increases the drive to eat and decreases energy expenditure
Body survives primarily on fat stores, sparing lean tissue
Metabolic Response to Injury
The metabolic response to injury is characterized by an increased metabolism and the onset of a catabolic process leading to excessive breakdown of tissue proteins
Metabolic state results from a complex interaction of inflammatory cytokines (IL-1, IL-2, IL-6, TNF-a, and interferon-y) released at the site of injury or inflammation, circulating hormones released in response to stress and injury (hypothalamic-pituitary-adrenal axis), and neurotransmitters (sympathoadrenal axis)
Infusion of cytokines including IL-6 and TNF-a results in stimulation of corticotrophin, cortisol, epinephrine, and glucagon, leading to an increases in the resting metabolic rate and lipolysis
TNF-a activation of nuclear factor kappa (NFk)-B results in stimulation of proteolytic pathways
Afferent nerve activity and brain stimulation may cause autonomic nerve stimulation with direct effects on hormone secretion and hypothalamic-pituitary activation, increasing the activity of cortisol, catecholamines, growth hormone, aldosterone, and antidiuretic hormone Prolonged elevation of cortisol is associated with onset of insulin resistance
Despite decline in food intake, hepatic gluconeogenesis continues and rapid protein catabolism develops There is an increased mobilization of stored fuels and metabolic cycling, resulting in heat production and energy loss Insulin resistance develops and hyperglycemia may occur despite the absence of food intake
Increase in lean tissue breakdown, visceral organ dysfunction, impaired wound healing, and immunosuppression
Nitrogen losses during catabolic response may be as high as 20-30 g/day versus 4-5 g/day in an adult human experiencing PPCM
Nutrition supplementation will not completely reverse the processes occurring during metabolic stress As long as tissue injury persists, catabolic processes are maintained
Hyperglycemia has been shown to negatively impact immune function and may increase the risk of late infection Control of blood glucose with a goal of avoiding severe hyperglycemia without risking hypoglycemia is recommended
What is the principal source of energy in pure protein/calorie malnutrtion?
Fat
What is the principal source of energy in severe metabolic stress?
Skeletal muscle
Total Energy of Feedstuff
Digestible energy (DE) and non-digestible energy
Digestible Energy
Metabolic energy (used to provide energy) + lost of nonmetabolizable energy (gases produced and urea excreted in the urine)
Amount of Digestible Energy Needed to Meet the Maintenance Energy Requirements of the Normally Active, Nonworking Horse (DEm)
BW (kg)
1 Mcal = 1000 kcal
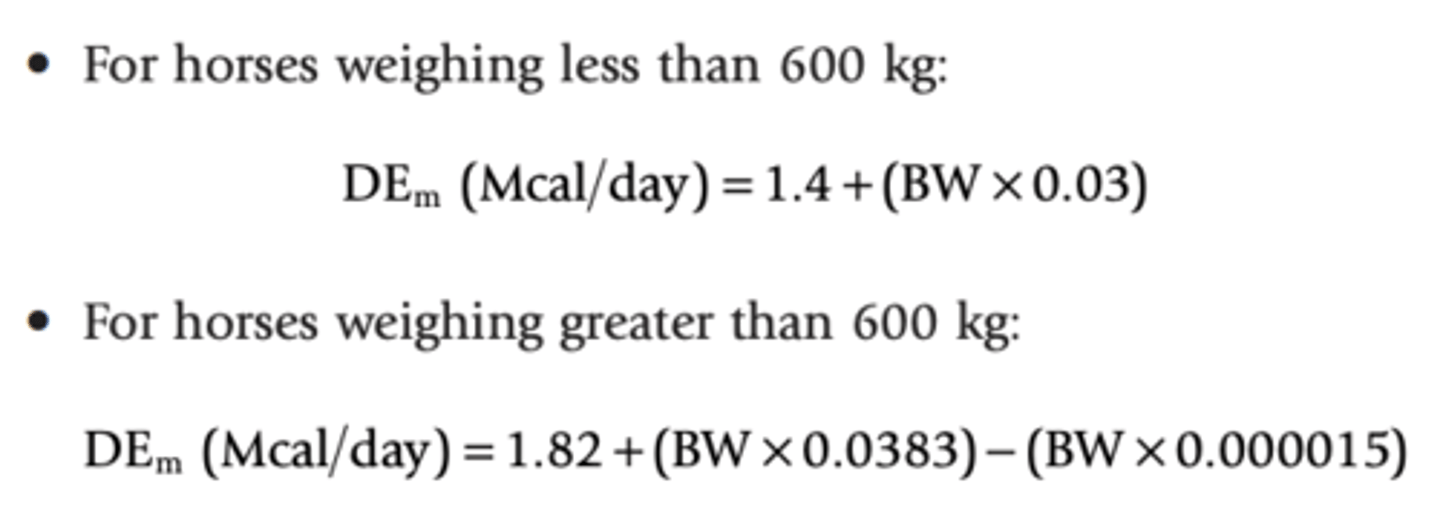
What can DEm be estimated as?
Approximately 33 kcal/kg/day
What can affect DEm?
Age
Size
Physical condition
Amount and type of activity
Environmental factors
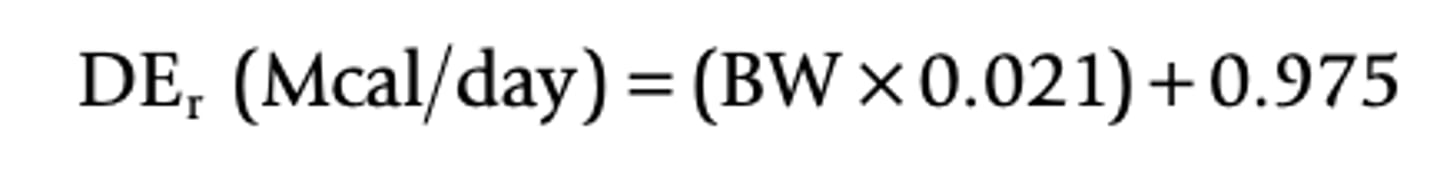
Resting Energy Requirement (DEr)
Amount of energy required for maintenance (neither weight gain nor weight loss) of the completely inactive animal
Approximately 70% of the Dem
Resting Energy Requirement Equation
When do energy requirements in the pregnant mare increase?
Energy requirements in the pregnant mare do not significantly increase until late gestation
What are the energy requirements of the pregnant mare in the last 3 months gestation?
Estimated to be 1.1, 1.13, and 1.2 times the DEm in the last 3 months of gestation
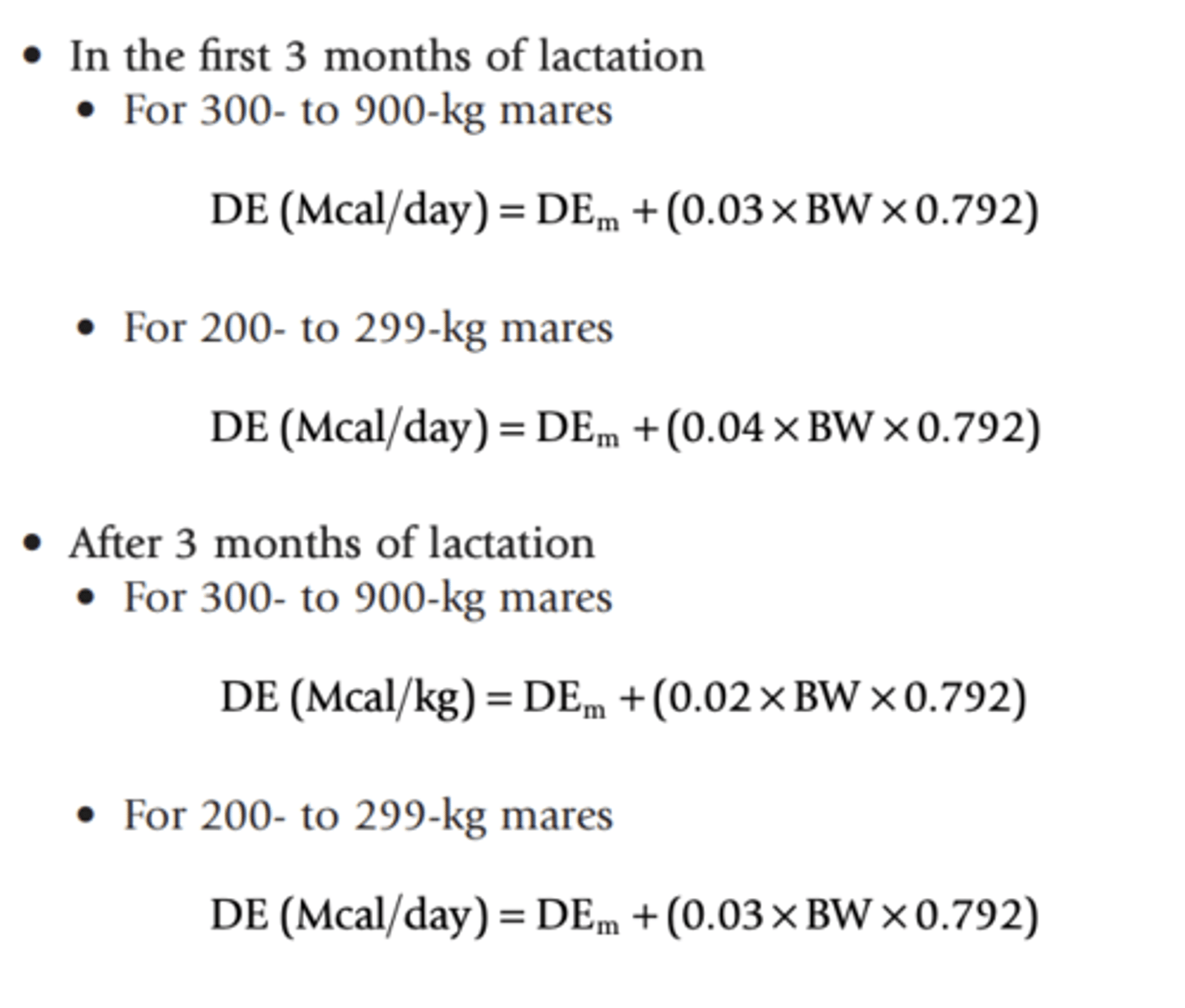
When do energy demands peak during lactation?
Peak over the first 3 months and then decline toward weaning
DE During Lactation Equations
What is an acceptable target when estimating the energy requirements of the majority of surgical patients?
DEr
How much energy does mare's milk have?
Between 500 and 600 kcal of energy per liter
How much does a healthy, 1 week old neonatal foal drink?
20-30% of its body weight in milk per day
What is the resting metabolic rate in a healthy sedated foal?
45-50 kcal/kg/day
Nutritional Supplementation for Sick Recumbent Foals
Start nutritional supplementation for sick recumbent foals at DEr and if tolerated, gradually increase to growth requirements over a shorter time that might be used to increase the adult animal's caloric intake
If using mare's milk or a milk replacement of similar caloric content, DEr, would equate to feeding the equivalent of 10% of the foal's body weight per day This is sufficient for the first 12-24 hours, but additional nutritional support would be required to ensure adequate intake for healing and growth
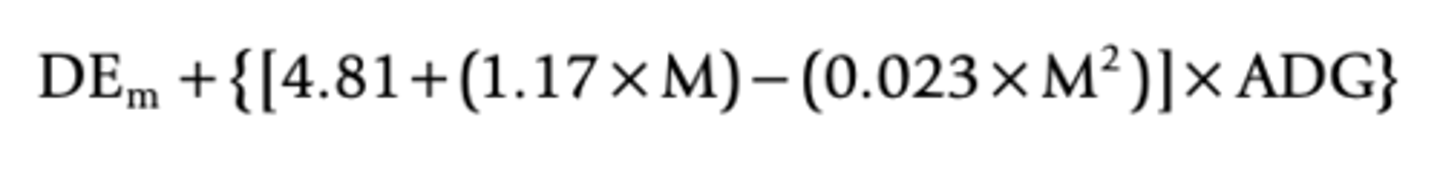
DEm for Weanling and Growing Horses
M - months of age
ADG - average daily weight gain (kg)
Protein Requirement Formula in the Adult Horse
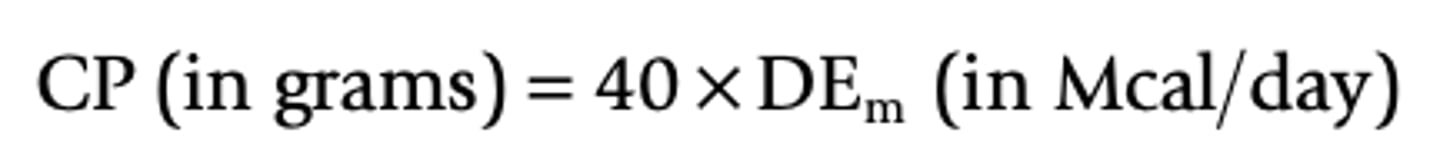
What can protein requirement in the adult horse be estimated as?
0.5-1.5 g of protein per kilogram of the horse's body weight per day
Fat Soluble Vitamins
A, K, D, E
Water Soluble Vitamins
B vitamins, C
Where are Vitamin K and all the B vitamins except niacin synthesized?
Synthesized by the microbial population in the horse's large colon and cecum
What vitamins are produced by the horse?
Vitamin D, Vitamin C, and niacin
What vitamins must be ingested?
The precursors to vitamin A, B-carotene, and vitamin E must be ingested
Enteral Nutrtion
Enteral nutrition increases total hepatosplanchnic blood flow in healthy patients, resulting in greater oxygen delivery to the mucosa
Enteral nutrition maintains functional and structural integrity of the gut; the absence of enteral nutrition causes mucosal atrophy, increased gut permeability, and enzymatic dysfunction in critically ill human patients
Enteral nutrition is a trophic stimulus for the GI tract both directly via the presence of nutrients and indirectly via stimulation of trophic hormones such as enteroglucagon
Enteral nutrition has a protective effect against bacterial translocation across the ischemic intestinal wall
During the hypermetabolic, catabolic state seen with injury or illness, many amino acids, such as glutamine, become conditionally essential Glutamine is an important fuel for lymphocytes, hepatocytes, and mucosal cells of the gut
Concerns about strength and diameter of anastomotic sites after surgical resection and about the risk of leakage if enteral feeding is introduced prematurely are not valid Enterally fed dogs had higher bursting pressures at colonic anastomotic sites and better wound collagen synthesis than unfed controls
Fiber is beneficial in increasing colonic blood flow, enzymatic activity, colonic mucosal cell growth, and absorption
Early Enteral Nutrition (EEN)
Initiation of enteral feeding within 48 hours after surgery
EEN significantly decreased morbidity and length of stay when compared with delayed enteral nutrition and PN
EEN has been shown to blunt the hypermetabolic and catabolic responses to injury in several human and animal models
What is the stomach volume of an adult 450 kg horse? What volume should feedings not exceed.
The stomach volume of an adult, 450 kg horse is approximately 9-12 L and a feeding should not exceed 6-8 L
When instituting enteral feeding, what is the maximum of the calculated requirements that should be fed during the first 24 hours?
When instituting enteral feeding, particularly in a patient with prolonged anorexia, feed a maximum of 50% of the calculated requirements during the first 24 hours
Parenteral Nutrition
Carbohydrates are commonly provided with 50% dextrose solutions that contain 1.7 Kcal/mL
Isotonic lipid emulsions contain principally safflower and soybean oils, egg yolk phospholipids, and glycerin, and come in 10% and 20% solutions
Amino acid preparations are available in several concentrations, 8.5% and 10% most common
Although not ideal, providing calories with dextrose infusions alone is a simple and inexpensive method to supply limited nutritional support to a postsurgical patient for a brief period (2 days) before transitioning to oral nutrition or more complex PN
Some vitamins can be given orally (Vitamins C and E) or added to crystalloid solutions (B vitamins)
The addition of lipids to PN is beneficial to patients with persistent hyperglycemia or hypercapnia because it reduced the dependency on glucose as the principal energy source
The amount of fat use will depend on the amount of carbohydrate provided, with fat storage occurring in the presence of excess carbohydrate calories
What should be used when calculating parenteral nutrition volumes for adult animals?
DEr should be used when calculating PN volumes for adult animals, but protein requirements should be based on maintenance needs or estimated using 0.5 to 1.5 g protein per kg BW/day
What should the ratio of nonprotein calories to nitrogen be in the final parenteral nutrition solution?
At least 100:1
What percentage of the non-protein calories should you use lipids to provide?
30-40%
What should the initial infusion rates of parenteral nutrition be?
Initial infusion rates should provide approximately 25-50% of the calculated requirement during the first 24 hours, if tolerated, the rate of infusion can gradually be increased over the next few days to provide 100% of the calculated requirement
Complications of Parenteral Nutrition
Hyperglycemia
Hyperammonemia
Hyperlipemia
Elevation of serum urea nitrogen
Thrombophlebitis
Sepsis
Lipid Infusion Complications
Allergic reactions
Hyperlipemia
Alterations in liver function
Fat embolism
Thrombocytopenia
Coagulopathies
Alterations in cellular immunity