pubhlth 228 - week 3: economic evaluation
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
31 Terms
economic evaluation
objective way to compare alternative ways of using resources to improve health & choose to spend funds to produce max health benefits
what inspired economic evaluation?
motivated by projects during the depression era, and the intro of medicaid & medicare in 1965
why are economic evaluations important?
federal agencies (EPA & FDA) are required to conduct it to ensure good use of resources
BUT USPTF (united states preventive services task force) DOES NOT consider costs when making recommendations
considering how are different population groups affected
cost-analysis
focus only on program costs
efficacy or effectiveness analysis
focus only on program outcomes
cost-minimization analysis
programs have equivalent outcomes (compare program costs & outcomes)
cost-benefit analysis, measure, need, & result
how program outcomes are measured
program costs and benefits measured in money
no need for group comparison
results:
net benefit or net cost savings (benefit - cost)
cost-benefit ratio (benefit / cost)
cost-effectiveness analysis, measure, need, & results
program costs and benefits measured in health outcomes
non-monetary units
need comparison b/w groups
results:
cost per unit health outcomes (cost per additional year of life)
cost-utility analysis, measure, & result
program cost & benefits measured in health outcomes
measures health outcomes adjusted for quality of life
subset of cost-effectiveness analysis
result:
cost per quality-adjusted life year (QALY)
non-monetary units
measuring profit or success using human outcomes rather than money
net benefit or net cost savings
result of cost-benefit analysis
(benefit - cost) > 0 —> program worth implementing
ex: project costs 100 million & benefit 105 million —> net: 5 million
cost-benefit ratio
result of cost-benefit analysis
if (benefit / cost) > 1 —> the program is worth implementing
ex: project costs 100 million & benefit 105 million —> ratio 1.05
cost-effectiveness analysis health outcome/effect measures
natural measures: comparing 2 treatments for the same condition
patient-reported outcome measures: patient perspective of their own health
incremental cost-effective analysis
if additional benefits or health effects is worth the additional cost
decision on which program to use should be based on additional costs & benefits of 1 intervention vs another, not total or average costs and benefits
incremental cost-effectiveness ratio (ICER)
comparing costs & benefits QALY b/w 2 intervention strategies; focus on changes in cost & QALYs
incremental cost / incremental QALY
cost savings
under cost-benefit analysis
benefits measured as cost savings (ex: reduced costs due to illness or disease avoided)
how to measure benefits (cost-benefit analysis) - type of cost savings
direct costs (medical costs, supplies, expenses for services)
indirect costs (value of time or life lost due to illness)
external or intangible costs (externalities or pain)
how to measure benefits (cost-benefit analysis): direct & indirect
measure direct cost by observed $ outlay (receipts, invoices, or payroll)
measure indirect through productivity gains, $ value of health improvements, willingness to pay, revealed preference, & cost of illness studies
advantage & disadvantages of willingness to pay approach
advantage: based on the values people place
disadvantage: people not knowing enough & that healthcare affects your choices
revealed preference approach
under cost-benefit cost savings; indirect cost
“hidden price tag” & OBSERVING (not asking) what people do
ex: difference in home price reveals exactly how much homeowners are willing to pay for clean air
ex: time is an indirect cost of healthcare. if a patient spends 2 hours driving to a doctor, they haven't "lost cash," but they have lost time they could have used for something else
advantages & disadvantages of revealed preference
advantages: reflects real world limitations like income & time; unlike survey’s people give “socially acceptable answers”
disadvantages: ability to pay bias & gives more “weight” to preferences
advantages & disadvantages of cost-benefit analysis
advantage: money is easily understood by people, can evaluate merits, & diff health outcomes
advantage: all benefits must be measured in $, which can be difficult & ignore scale of program (large b/c ratio may represent small net benefits)
advantages & disadvantages of cost-effective analysis
advantages: no need to value human life in $ & can compare programs based on the cost of achieving health improvement
disadvantages: can’t evaluate “worth” of program implementation & difficult to compare programs w/ diff health measures/outcomes
advantages & disadvantages of cost-utility analysis
advantages: doesn’t treat ALL years of life saved as equal value (ex: someone in a coma); adjusts year based on individual preferences for diff health conditions (how much would they give up to avoid a specific condition
disadvantages: measurement difficulty; not representative of population
QALY formula
sum of each (years x designated health state preference)
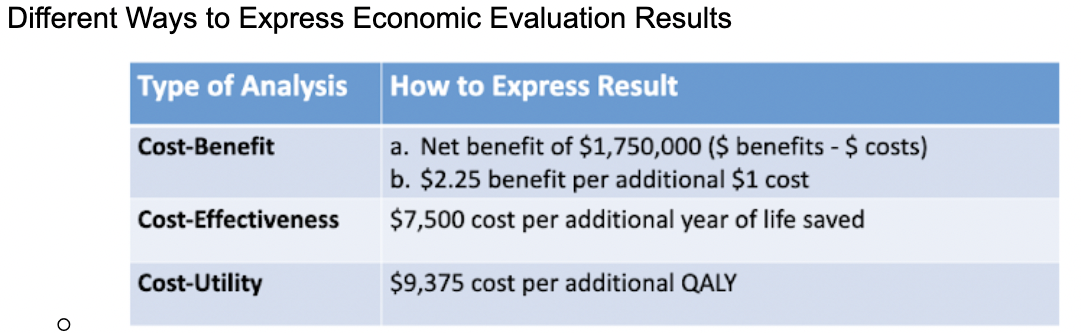
different ways to express economic evaluation results
should unrelated healthcare cost be included in c-e ratios? (ex: if evaluating a program to reduce cholesterol, should include medical costs of non-CHD health care (e.g., cancer, influenza, etc.)
economic perspective is all about all costs
most people exclude these costs