Immune System Lecture Worksheets 1 & 2 Bio 221
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
123 Terms
Study
Study
Study
Study
What are the 2 arms of specific immunity?
The two arms are cell-mediated immunity and antibody-mediated (humoral) immunity.
What is an antigen?
An antigen is any molecule that triggers an immune response by being recognized as foreign by the body.
What are the 2 types of T cells?
The two main types are Helper T cells (Th) and Cytotoxic T cells (Tc).
What arm of specific immunity involves the Tc cells?
Cell-mediated immunity involves Cytotoxic T cells (Tc).
Which type of T cell participates in both arms of specific immunity?
Helper T cells (Th cells) — they coordinate the immune response by activating B cells for antibody-mediated (humoral) immunity and Cytotoxic T cells for cell-mediated immunity.
What arm of specific immunity involves the B Cells?
Antibody-mediated (humoral) immunity involves B cells.
What is co-stimulation?
Co-stimulation is the second activation signal required for a lymphocyte (usually a T cell) to become fully active. It ensures that immune responses occur only when both antigen recognition and a confirming signal are present, preventing accidental or inappropriate activation.
Name the five classes of antibodies and give characteristics of each type.
IgG: Most abundant antibody in blood and tissues; crosses the placenta to protect the fetus and provides long-term immunity.
IgA: The secretory antibody, found in mucus, saliva, tears, and breast milk, protects mucosal surfaces from infection.
IgM: The first antibody produced during an infection; forms pentamers and is a strong agglutinator.
IgD: Surface receptor antibody, found on the surface of B cells; acts as a receptor to help activate B cells.
IgE: Involved in allergic reactions and defense against parasites; binds to mast cells and basophils.
Order of the most abundant antibody in the bloodstream to remember: George ate my deviled eggs.
How does the secretion of antibodies help fight disease?
Antibodies bind to antigens to neutralize pathogens, trigger phagocytosis, and activate complement proteins to destroy invaders.
What does an antigen presenting cell (APC) do?
An APC processes and displays antigens on its surface for recognition by T cells, initiating an immune response.
Give examples of APCs.
Examples include macrophages, dendritic cells, and B cells.
How are naive helper T cells activated?
A naïve T cell is a T cell that hasn’t encountered its specific antigen yet.
An antigen-presenting cell (APC) (like a dendritic cell or macrophage) captures a pathogen and shows a piece of it (the antigen) on a molecule called MHC II.
The T cell’s T cell receptor (TCR) recognizes the antigen on MHC II.
The TCR binds the antigen and then after is the co-stimulatory signal.
The APC also provides a co-stimulatory signal—think of it as a “green light” that says, “It’s okay to activate.”
✅ Both steps are required; without the co-stimulation, the T cell becomes inactive.
Helper T cells type 1 stimulate what type of cells?
Th1 cells activate Cytotoxic T cells and macrophages for cell-mediated immunity.
Helper T cells type 2 stimulate what type of cells?
Th2 cells activate B cells to become plasma cells and produce antibodies, supporting antibody-mediated (humoral) immunity.
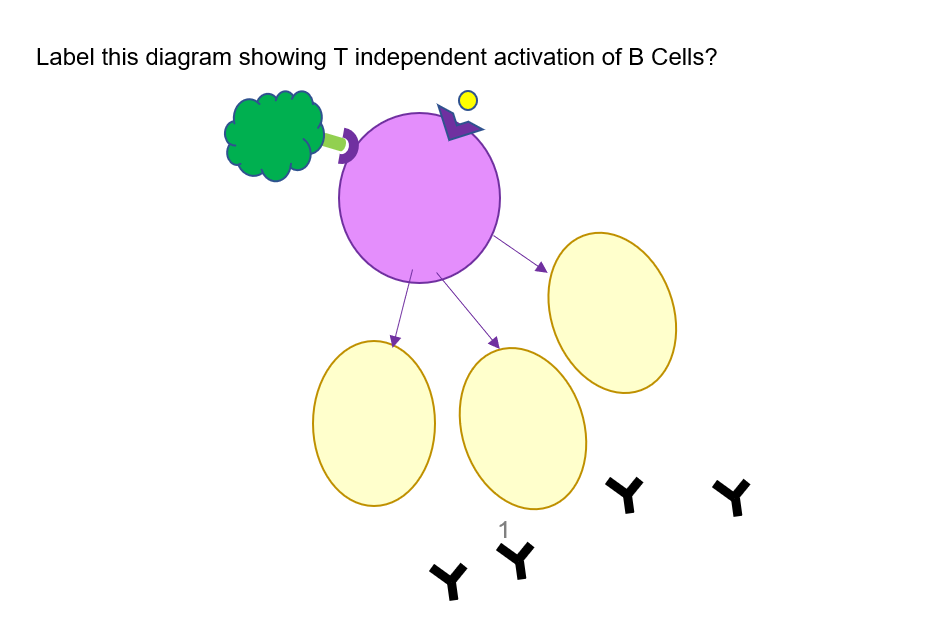
Distinguish between T independent and T dependent B cell activation.
T-Independent Activation:
B cells are activated directly by antigens without T cell help. The response is weak, short-lived, and does not produce memory cells.
T-Dependent Activation:
B cells require Helper T cell (Th) assistance for activation. The response is strong, long-lasting, and creates memory cells for faster future defense.
What type of T cell is involved in cell-mediated immunity?
Cytotoxic T cells (Tc).
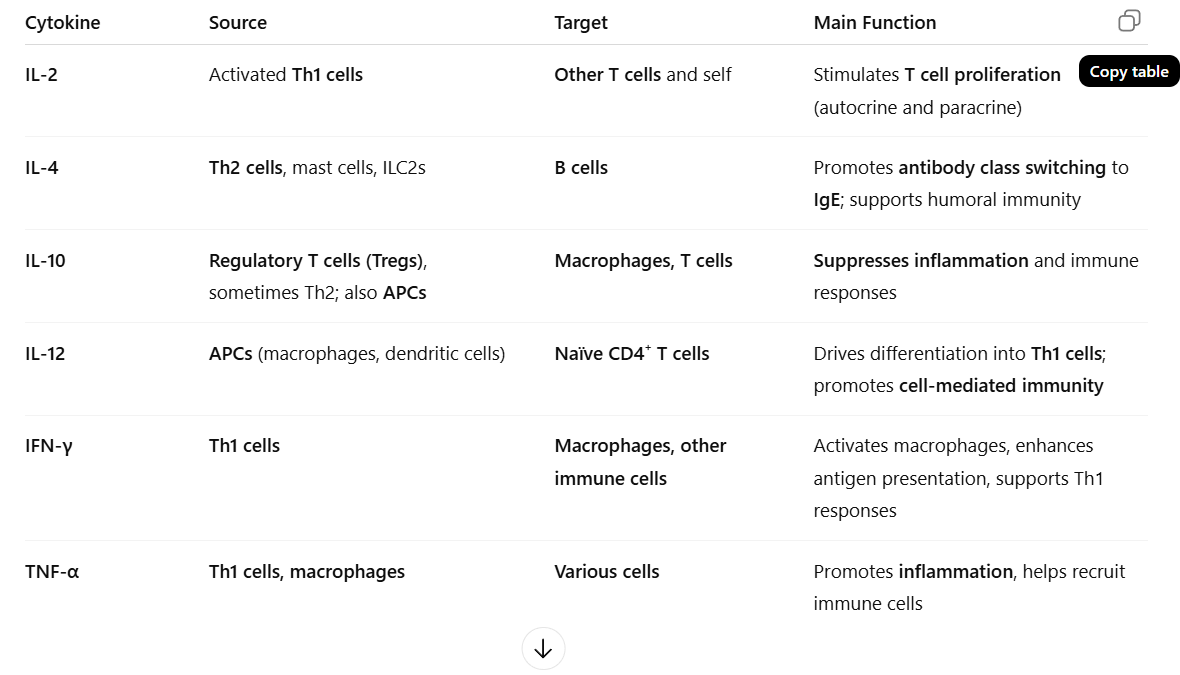
When are cytotoxic (Tc) T cells activated?
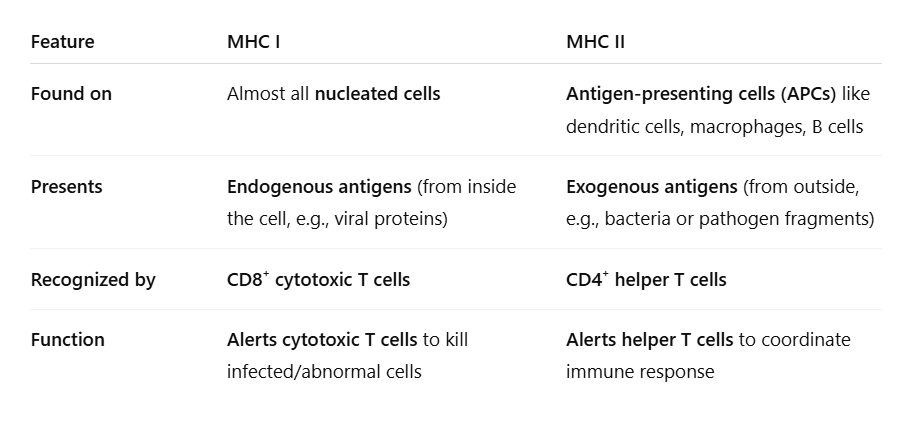
🧩 1. “Antigens are presented on MHC I molecules”
MHC I (Major Histocompatibility Complex I) is found on all body cells.
When a cell is infected (like by a virus) or becomes abnormal (like cancer), it displays bits of that foreign protein (antigen) on its MHC I.
This acts as a “red flag” to signal something is wrong inside the cell.
⚔ 2. “Cytotoxic T cells recognize this MHC I + antigen”
Cytotoxic T cells (CD8⁺) constantly check cells’ MHC I displays.
When they find a cell showing a foreign antigen on MHC I, they know that cell is infected or damaged.
🤝 3. “Helper T cells provide co-stimulation”
The Cytotoxic T cell doesn’t act alone — it needs confirmation from a Helper T cell (CD4⁺).
Helper T cells release cytokines (like IL-2) that give the “go signal” to fully activate the Cytotoxic T cell.
🚀 4. What happens after activation
The Cytotoxic T cell multiplies and begins killing infected cells by releasing perforin and granzymes
Infected cell → shows antigen on MHC I → Cytotoxic T cell detects it → Helper T cell confirms → Cytotoxic T cell becomes activated and destroys the infected cell.
What do cytotoxic T cells do to help get rid of a pathogen?
They destroy infected or cancerous cells by releasing perforin and granzymes that induce apoptosis (programmed cell death).
How do memory cells help us develop immunity?
Memory cells store information about specific antigens after an initial infection. During future exposures to the same pathogen, they trigger a faster, stronger, and more effective immune response.
Distinguish between a primary and secondary immune response in terms of antibody response.
Primary Response:
The primary response occurs after the first exposure to an antigen. It is slow, produces low levels of antibodies (mainly IgM), and does not yet form immediate memory.
Secondary Response:
The secondary response occurs after a subsequent exposure to the same antigen. It is faster, stronger, and longer-lasting, producing high levels of antibodies, mainly IgG, due to memory cells created during the primary response.
What is a vaccine?
A vaccine is a preparation containing weakened, inactivated, or partial antigens that triggers the immune system to produce memory cells and antibodies, providing protection without causing the actual disease.
What is the function of regulatory cells?
Regulatory cells (also called Regulatory T cells or Tₙₑg cells) help control and balance the immune response.
Their main functions are:
Prevent overreaction of the immune system after an infection has been cleared.
Suppress autoimmune responses — stop the body from attacking its own healthy cells.
Release inhibitory cytokines (like IL-10 and TGF-β) that reduce inflammation and calm other immune cells.
Do antigens have epitopes?
✅ Yes.
An epitope (or antigenic determinant) is the specific part of an antigen that is recognized and bound by an antibody or a B/T cell receptor.
One antigen can contain many epitopes, each triggering a different immune response.
Antigens are the whole molecules; epitopes are the smaller regions that the immune system actually detects and binds to.
Memory Tip:
🧠 Antigen = entire target; Epitope = specific “spot” the immune system locks onto.
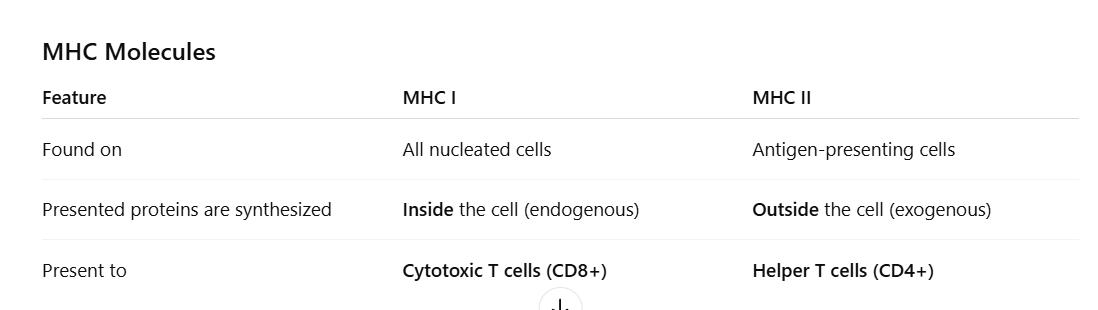
Label the diagram.
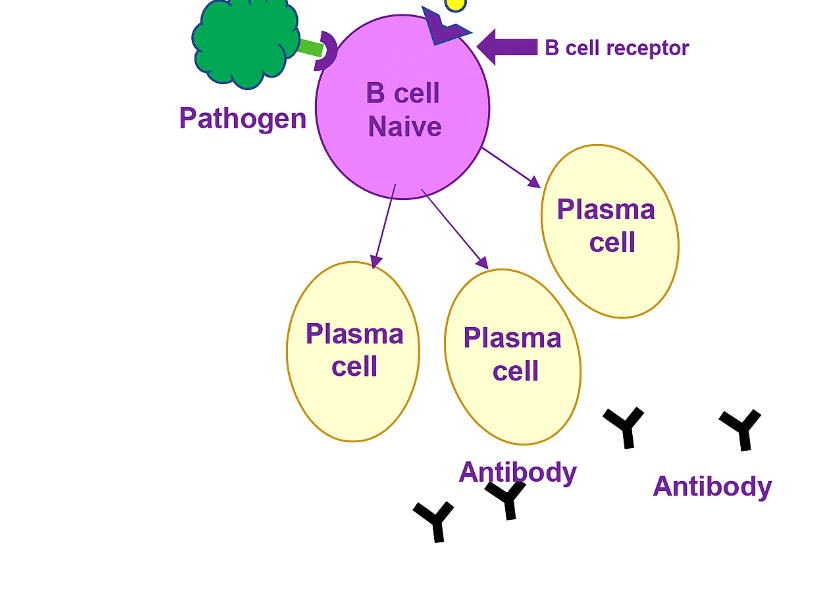
What are the steps for an activated B-cell?
Activation: A B cell binds to its specific antigen and receives activation signals from a helper T cell.
Proliferation: The activated B cell rapidly divides to form a clone of identical cells.
Differentiation: The cloned cells become plasma cells, which secrete antibodies specific to the antigen, and memory B cells, which provide long-term immunity.
CD40L + IL-4 (and other cytokines)" = Th2 costimulation for B cells. The actual molecule providing the activating signal is CD40L, but it only works because the B cell has CD40 to receive it.
What are naive cells?
Naive cells are immune cells (lymphocytes) that have not yet encountered an antigen. They are in a resting state, ready to respond upon first exposure to a specific pathogen.
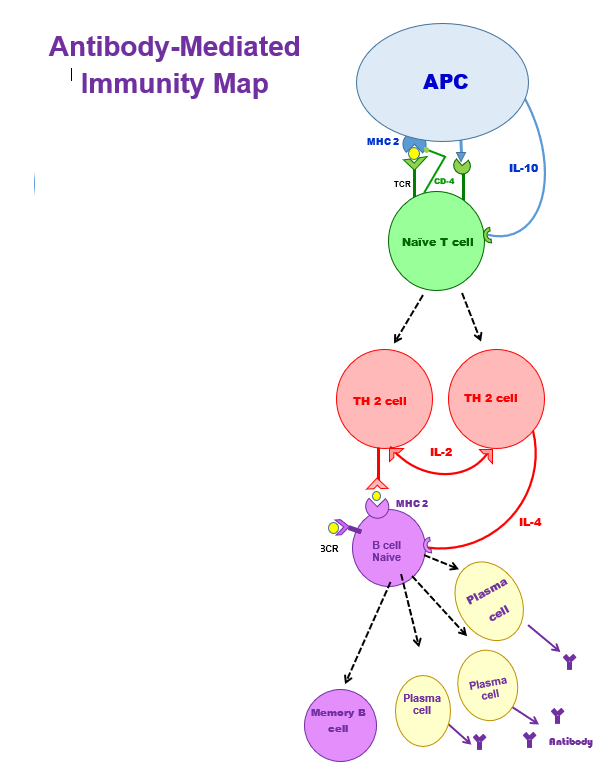
Study the antibody-mediated immunity map.
Antibody-Mediated (Humoral) Immunity – Stepwise
1. Antigen Presentation (APC → Naïve CD4⁺ T cell)
APC (like a dendritic cell) presents antigen on MHC-II.
The CD4 co-receptor on the T cell binds MHC-II, stabilising the interaction.
2. T Cell Activation
TCR binds the antigen-MHC-II complex.
CD28 on T cell binds B7 (CD80/CD86) on APC → costimulatory signal.
3. T Cell Differentiation
IL-4 from innate cells (mast cells, basophils, and ILC2s) creates initial Th2 cells, and Th2 then starts secreting IL-4 for naïve T cells to become Th2 cells.
Th2 cells secrete IL-4, creating a positive feedback loop → more Th2 differentiation.
Th2 cells also produce IL-2 to stimulate the proliferation of T cells.
4. B Cell Activation
Naïve B cell binds antigen via BCR and presents it on MHC-II.
Th2 cell recognizes antigen-MHC-II on B cell.
Costimulatory signal: CD40L (Th2) → CD40 (B cell).
CR3 (3CR) on B cell binds complement-coated pathogens → boosts activation.
5. B Cell Differentiation
Activated B cells become:
Plasma cells → secrete antibodies
Memory B cells → long-term immunity
6. Antibody Function
Antibodies bind, neutralize, and opsonize pathogens, enhancing their destruction.
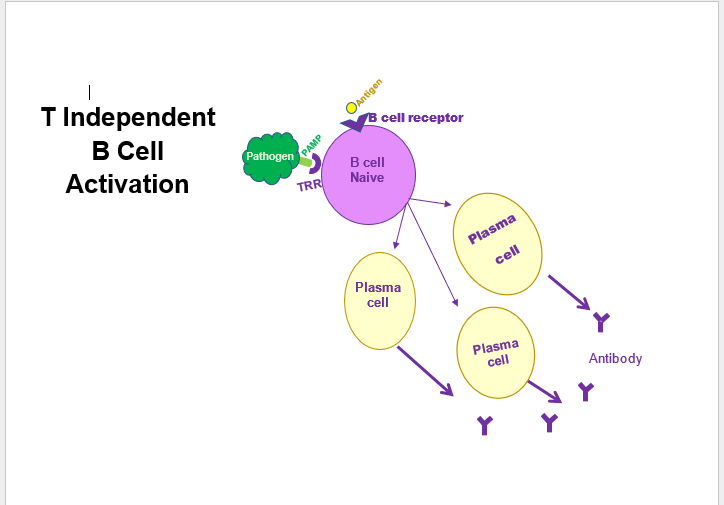
Study the T-independent B cell activation.
🧫 1. Pathogen binds directly to the B cell
A naïve B cell (a B cell that hasn’t encountered its specific antigen yet) has special receptors on its surface:
BCR (B cell receptor): recognizes a specific shape or molecule on the pathogen.
TLR (Toll-like receptor): recognizes general “danger” signals common to pathogens (like bacterial cell wall parts).
When both receptors are triggered, it’s a strong sign the pathogen is real — no need for a helper T cell.
⚡ 2. B cell becomes activated on its own
Normally, B cells need a Helper T cell (Th2) to confirm activation.
But in this case (like with bacteria or polysaccharide antigens), the B cell can self-activate because both BCR and TLR signals are strong enough.
This is called a T-independent activation.
🧬 3. B cell differentiates into plasma cells
Once activated, the B cell changes (differentiates) into a plasma cell — the “antibody factory” form of a B cell.
🎯 4. Plasma cells produce antibodies
These plasma cells start secreting antibodies that match the pathogen’s antigens exactly.
Antibodies then bind to and neutralize the pathogen or mark it for destruction by other immune cells.
🔁 Flow summary:
Pathogen → binds BCR & TLR on Naïve B cell → B cell activates (no Th cell) → becomes Plasma cell → releases Antibodies to fight the pathogen.
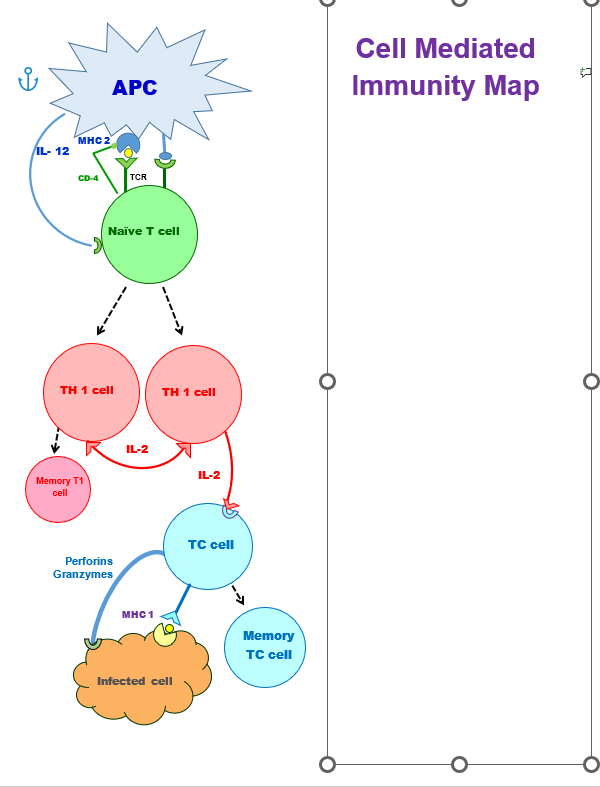
Study the cell-mediated immunity map.
Antigen Presentation
APC (dendritic cell, macrophage, or B cell) presents antigen on MHC-II.
Naïve CD4⁺ T cell recognizes the antigen via its TCR.
CD4 co-receptor binds MHC-II to stabilize the interaction.
Costimulatory signal: CD28 on the T cell binds B7 (CD80/CD86) on the APC.
Cytokine signal: IL-12 from the APC (or innate cells) drives Th1 differentiation.
2. T Cell Differentiation
Naïve CD4⁺ T cell → Th1 cell (driven by IL-12).
Th1 cells are key for cell-mediated immunity.
3. Cytokine Release and Function
Th1 cells secrete IL-2:
Autocrine effect: stimulates their own proliferation.
Paracrine effect: helps nearby T cells, including naïve or partially activated cytotoxic T cells (Tc cells), to proliferate and differentiate.
Other Th1 cytokines (bonus for context):
IFN-γ → activates macrophages and enhances antigen presentation.
TNF-α → promotes inflammation.
4. Cytotoxic T Cell Activation
Tc cells (CD8⁺ T cells) recognize infected cells via MHC-I + antigen.
Activation requires: IL-2 from Th1 cells (as a growth/proliferation signal).
Effector function: release perforin (forms pores) and granzymes (induces apoptosis) → kills infected cells.
5. Memory Formation
Some Th1 and Tc cells become memory cells → faster and stronger response upon re-exposure.
What are the main characteristics of IgG antibodies?
IgG is the most abundant antibody in blood and tissues. It crosses the placenta to provide passive immunity to the fetus and gives long-term protection after infection or vaccination.
What are the main characteristics of IgA antibodies?
IgA is found in mucus, saliva, tears, and breast milk. It protects mucosal surfaces by preventing pathogens from attaching and entering the body.
What are the main characteristics of IgM antibodies?
IgM is the first antibody produced in response to an infection. It forms pentamers (5 antibodies linked → lots of binding sites.), making it a powerful agglutinator (causes pathogens to clump together for easier elimination), and an efficient activator of the complement system.
What are the main characteristics of IgE antibodies?
IgE plays a role in allergic reactions and defense against parasites. It binds to mast cells and basophils, causing them to release histamine and other inflammatory mediators,
What are the main characteristics of IgD antibodies?
IgD is found on the surface of immature B cells, where it acts as a receptor that helps activate B cells during the immune response.
What are the key differences between antibody-mediated (humoral) and cell-mediated immunity?
1⃣ Helper T cell type:
Th2 → Humoral (antibody-mediated)
Th1 → Cell-mediated
2⃣ Main target:
Th2: Extracellular pathogens (bacteria, toxins)
Th1: Intracellular pathogens (viruses, infected cells, tumors)
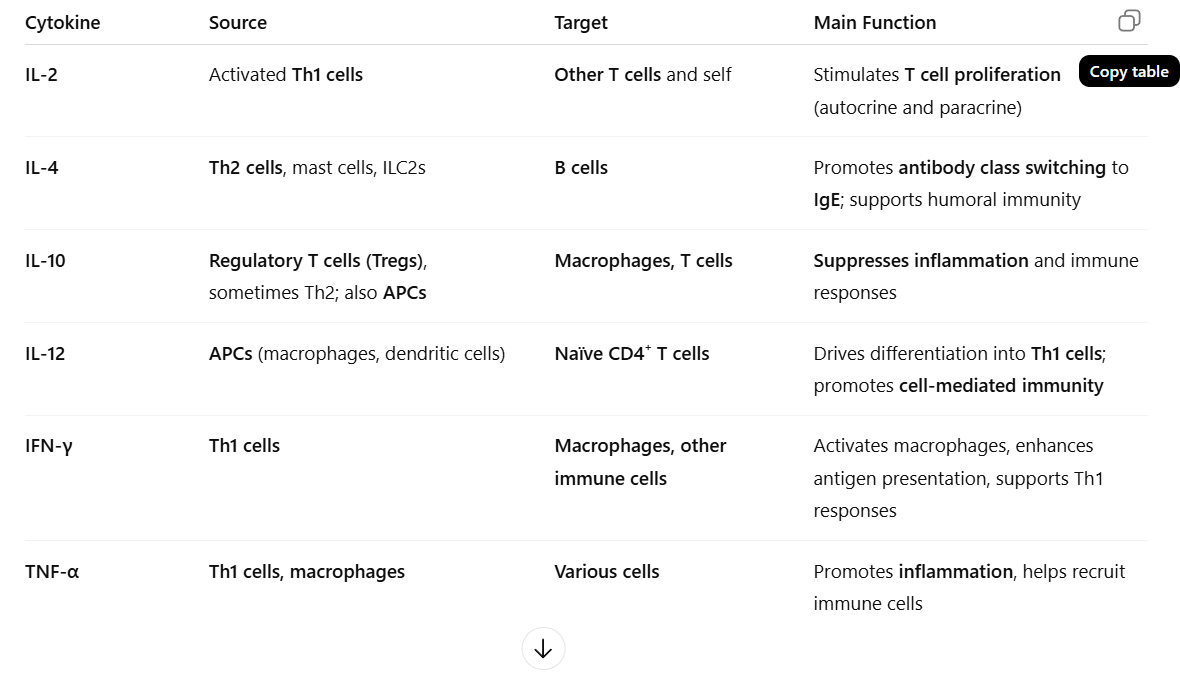
3⃣ Cytokines involved:
Th2: IL-10, IL-2, IL-4
Th1: IL-12, IL-2, IFN-γ
4⃣ Effector cells:
Th2: Activates B cells → Plasma + Memory B cells → Antibodies
Th1: Activates Tc (Cytotoxic T) cells → Kill infected cells
5⃣ Antigen presentation:
Th2: APC presents on MHC-II
Th1: Infected cell presents on MHC-I
6⃣ Final outcome:
Th2: Antibodies neutralize or tag pathogens
Th1: Tc cells destroy infected or abnormal cells
🧠 Easy Memory Tip:
“Th2 = B cells = Bodies = Antibodies (Outside)”
“Th1 = Tc cells = Terminate (Inside)”
What do cytotoxic T cells (Tc cells) trigger in infected or abnormal cells?
Cytotoxic T cells trigger apoptosis (programmed cell death) in infected, cancerous, or damaged cells to eliminate the threat.
What’s the difference between Helper T cells and Cytotoxic T cells?
Helper T (CD4⁺): Recognize antigens on MHC II, release cytokines to activate B and T cells.
Cytotoxic T (CD8⁺): Recognize antigens on MHC I, kill infected or abnormal cells directly.
Why are T cells considered the main part of the immune system instead of B cells?
T cells are the leaders and coordinators of the immune system:
Helper T cells (CD4⁺) release cytokines that activate B cells, cytotoxic T cells, and macrophages, guiding the entire immune response.
Cytotoxic T cells (CD8⁺) directly kill infected or cancerous cells, which antibodies can’t reach.
Without T cells, B cells can’t fully activate or make effective antibodies, and the immune system becomes disorganized (as seen in HIV).
B cells mainly make antibodies to target pathogens in body fluids, but they usually need Helper T cell (Th2) signals first.
✅ Summary:
T cells direct, regulate, and destroy, while B cells produce antibodies under their command — making T cells the central controllers of adaptive immunity.
What are the sources and actions of interleukin 1& 2?
IL-1 (Interleukin-1)
Source: Mainly macrophages and other antigen-presenting cells (APCs).
Actions:
Promotes inflammation (fever, vasodilation).
Activates helper T cells (CD4⁺).
Stimulates production of other cytokines.
IL-2 (Interleukin-2)
Source: Activated CD4⁺ helper T cells.
Actions:
Stimulates proliferation of T cells (autocrine and paracrine effect).
Activates cytotoxic T cells (CD8⁺) and NK cells.
What is the result of Tc cell docking with MHC I on a cell?
When a cytotoxic T (Tc) cell docks with MHC I presenting an antigen on a cell, it recognizes the antigen. After receiving activating signals (often from Th1 cells), the Tc cell kills the infected or abnormal cell, usually by inducing apoptosis using perforin and granzymes.
Compare T-independent and T-dependent B cell activation.
T-independent activation does not involve Helper T cells. The antigens are usually lipids or carbohydrates, no memory cells are formed, and this type of immunity develops after age 2.
T-dependent activation does involve Helper T cells (Th2). The antigens are usually proteins, memory cells are formed, and it can occur from birth.
Describe and give examples of natural vs. artificial and active vs. passive immunity.
Natural Passive Immunity: Transfer of pre-made antibodies from mother to child—IgG through the placenta and IgA through breast milk.
Artificial Passive Immunity: Injection of antibodies from an external source, such as antiserum or monoclonal antibodies.
Natural Active Immunity: The body develops its own immune response after infection, creating memory cells.
Artificial Active Immunity: Occurs after vaccination, where exposure to an antigen stimulates the immune system to build memory and protection.
Why is a vaccine considered artificial active immunity, and receiving antibodies artificial passive immunity?
A vaccine is artificial active because it’s man-made and causes your body to actively produce antibodies and memory cells.
Receiving antibodies is artificial passive because the antibodies come from an external source (like antiserum or monoclonal antibodies). Your immune system doesn’t make or remember them, so protection is immediate but short-lived.
What is the function of M cells in the gut?
M cells are specialized epithelial cells in the intestinal lining that bind and transport pathogens from the gut lumen to underlying macrophages.
The macrophages process the antigen and activate T cells, which in turn activate B cells to produce antibodies, especially IgA for mucosal immunity
What is the function of the immune system?
A group of organs and cells that defends the body against pathogens, removes damaged cells, absorbs nutrients, and identifies and destroys abnormal or cancerous cells.
What are the components of the immune system?
The immune system includes white blood cells (leukocytes), lymphatic vessels, lymph nodes, the spleen, thymus gland, bone marrow, and MALT (mucosa-associated lymphoid tissue). (non-encapsulated wbc)
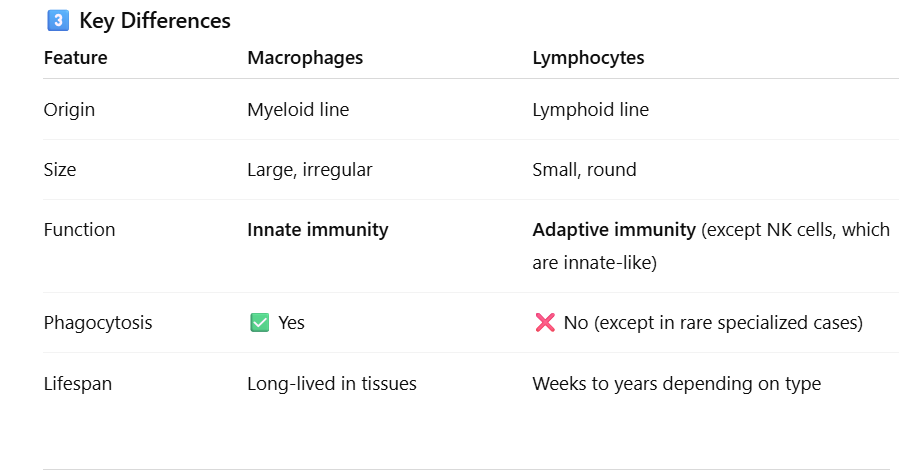
Name the 5 types of white blood cells and their basic functions.
Neutrophils (Innate) —-Phagocytose bacteria and debris.
Lymphocytes (Adaptive except for NK cells)—Include B cells, T cells, and NK cells; responsible for adaptive and innate immunity.
Monocytes (Innate)— Become macrophages; engulf pathogens and dead cells.
Eosinophils (Innate)—Attack parasites and modulate allergic responses.
Basophils (Innate)—Release histamine and heparin during inflammation and allergies.
What are the functions of the lymph vessels?
They transport lymph, return excess interstitial fluid to the bloodstream, and help move immune cells throughout the body.
What are characteristics of lymph vessels?
Lymph vessels have thin walls, valves to prevent backflow, and resemble veins in structure.
What are lymph nodes?
Lymph nodes are small, bean-shaped organs that filter lymph and house lymphocytes to initiate immune responses.
Approximately how many lymph nodes are in the body?
There are about 600 to 700 lymph nodes in the human body.
What fibers and cells are present in lymph nodes?
Lymph nodes contain reticular fibers that trap particles and white blood cells, including:
Lymphocytes (All adaptive T and B cells except for NK cells, innate) – Recognise and respond to specific antigens.
Macrophages (Innate)—Engulf and destroy pathogens and debris.
Dendritic cells (Innate) – Capture antigens and present them to lymphocytes to activate immune responses.
What is MALT?
MALT (mucosa-associated lymphoid tissue) is lymphoid tissue that protects mucosal surfaces—such as those in the digestive, respiratory, urinary, and reproductive tracts—from pathogens.
What are specific types of MALT?
Specific types of MALT include tonsils, Peyer’s patches in the small intestine, and the appendix.
What are the functions of the spleen?
The spleen filters blood, removes old red blood cells, stores platelets, and activates lymphocytes to initiate immune responses.
Distinguish between red pulp and white pulp.
The red pulp filters blood and removes old red blood cells, while the white pulp contains lymphocytes and initiates immune responses.
What is the function of the thymus gland?
The thymus gland is where T lymphocytes (T-cell) mature and differentiate, allowing them to function properly in immune responses.
What is the role of thymosin?
Thymosin is a hormone that promotes the development, helps naïve T cells become fully functional and able to respond to antigens and maturation of T cells.
Distinguish between nonspecific (innate) and specific immunity.
Innate immunity provides general, immediate defense with no memory, while specific (adaptive) immunity targets particular antigens and has memory for faster future responses.
→ “memory” refers to the immune system’s ability to remember a pathogen it has encountered before.
Name some components of the first line of defense.
The first line of defense consists of physical and chemical barriers such as skin, mucous membranes, tears, saliva, stomach acid, and normal microbiota that prevent pathogens from entering the body.
What are PAMPs and DAMPs?
: PAMPs (pathogen-associated molecular patterns) are molecules present on pathogens that signal infection, while DAMPs (damage-associated molecular patterns) are molecules released by injured or stressed cells to signal tissue damage.
What are PRRs (TLRs)?
PRRs, like Toll-like receptors (TLRs), are on immune cells and detect signs of infection or cell damage:
PAMPs: Pathogen-associated molecular patterns (from microbes)
DAMPs: Damage-associated molecular patterns (from injured cells)
When PRRs detect these signals, they activate the immune system to fight infection or repair damage.
Memory Tip: 🧠 PRRs = Immune “sensors” that detect danger
B cells and T cells – are the only ones that generally do not use PRRs for activation
What cells have PRRs?
Macrophages, dendritic cells, and neutrophils have PRRs, allowing them to detect PAMPs and DAMPs and initiate immune responses.
What happens when PRRs are activated?
When PRRs (Pattern Recognition Receptors) are activated, they trigger immune responses, including inflammation, cytokine release, and activation of other immune cells to fight pathogens or respond to tissue damage.
What are the symptoms of inflammation and name two vasodilators.
The symptoms of inflammation are redness, heat, swelling, pain, and loss of function. Two vasodilators that contribute to these symptoms are histamine and bradykinin.
What is margination and diapedesis?
Margination is when white blood cells stick to the walls of blood vessels at the site of infection.
Diapedesis is when these white blood cells squeeze through the vessel walls to reach the infected or damaged tissue.
What are the steps of phagocytosis?
Chemotaxis – The phagocyte moves toward the pathogen.
Adherence – The phagocyte binds to the pathogen, sometimes aided by opsonins.
Ingestion – The pathogen is engulfed into a phagosome.
Digestion – The phagosome joins with a lysosome to form a phagolysosome, where the pathogen is broken down.
Exocytosis – Waste materials are expelled from the cell.
What is an opsonin?
An opsonin is a molecule, such as an antibody or complement protein, that coats a pathogen, making it easier for immune cells to recognise and engulf, thereby enhancing phagocytosis.
What is complement?
Complement is a group of plasma proteins that enhance immune responses by destroying pathogens (lysis), coating them for easier engulfment (opsonization), and promoting inflammation.
Name the 2 ways complement is activated.
Classical Pathway: Triggered by antibodies bound to pathogens → starts a cascade → leads to opsonization, inflammation, MAC formation.
Alternative Pathway: Triggered directly by pathogen surfaces, no antibodies needed → same cascade and outcomes.
Key Difference: 🧠 Classical = antibody-dependent, Alternative = innate/direct.
Memory Tip: 🧠 “Classical needs a class (antibodies), Alternative acts automatically.”
Classical: The pathway starts when C1 complex binds to the Fc region of the antibody, not just any antibody contact.
What is the action of interferon, and what secretes it?
Interferons:
Interferons are proteins released by virus-infected cells that alert and protect nearby healthy cells.
Warn nearby cells to make antiviral proteins that block virus replication.
Activate macrophages and natural killer (NK) cells to destroy infected cells.
Help the immune system spot infected cells by increasing how well they display antigens. (Increases antigen presentation)
Slow the spread of viruses by creating an antiviral shield around neighboring cells.
Summary:
Interferons act as the body’s early warning system against viruses, helping to stop infection and activate other immune defenses.
What is the hypoferremic response?
The hypoferremic response is when the body reduces the amount of iron in the blood during infection to limit bacterial growth, since many bacteria need iron to survive. (The body binds up iron and iron-binding proteins; therefore, it’s less available for pathogens.)
What is a pyrogen, and how does its secretion improve immune response?
A pyrogen is a substance that causes fever, either from pathogens or immune cells. Fever speeds up immune cell activity and slows the growth of pathogens, enhancing the body’s defense.
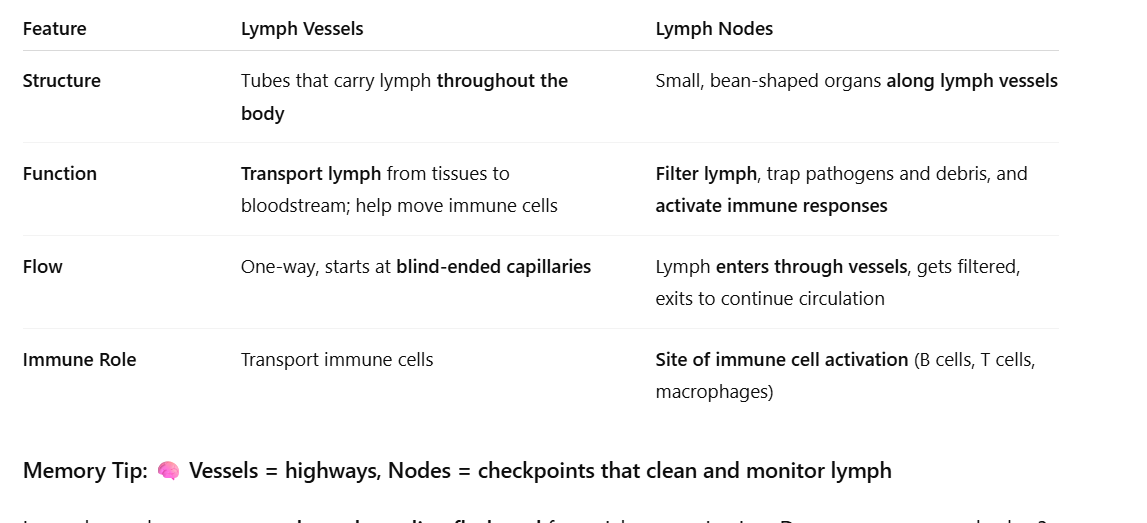
What are lymph vessels and what do they contain?
Lymph vessels are blind-ended tubes filled with lymph, a clear fluid derived from interstitial fluid.
How does lymph move through lymph vessels?
Lymph flows one way through vessels aided by valves, skeletal muscle contraction, and pressure changes during breathing.
What is the main function of lymph vessels?
They collect excess interstitial fluid from capillary beds and return it to the bloodstream.
Example: About 30 L of fluid is filtered from capillaries daily, 27 L reabsorbed, and 3 L recovered by lymph vessels as lymph.
What are the functions of lymph vessels?
Lymph vessels pick up excess filtered fluid from capillary beds, absorb fats from the intestines and transport them to the bloodstream, and expose lymph to white blood cells for immune monitoring.
Blood plasma leaks out of capillaries → becomes interstitial fluid → drains into lymphatic vessels → becomes lymph → returns to bloodstream near the heart. (The excess filtered fluid was blood plasma at first).
What are granulocytes and what are their types and functions?
Granulocytes are a type of white blood cell that contain granules in the cytoplasm.
Types:
Neutrophils
Most abundant WBC
Phagocytose pathogens (especially bacteria) and cellular debris
First responders in infections
Eosinophils
Red/orange-staining granules
Involved in allergic reactions and defense against parasites
Modulate inflammation
Basophils
Least abundant WBC
Release histamine → mediates allergic reactions
Release heparin → prevents local blood clotting
What are agranulocytes, and what are their types and functions?
Agranulocytes are white blood cells without visible cytoplasmic granules.
Types:
Monocytes – Become phagocytic macrophages and give rise to dendritic cells.
Lymphocytes—Carry out specific immune responses, including B cells, T cells, and NK (natural-killer) cells.
Where do granulocytes and agranulocytes come from?
All WBCs come from hematopoietic stem cells in the bone marrow.
Granulocytes (neutrophils, eosinophils, basophils) develop from myeloid progenitors.
Monocytes (agranulocytes) also come from myeloid progenitors.
Lymphocytes (B cells, T cells, NK cells) come from lymphoid progenitors.
Dendrtic cells from myeloid stem cells.
Memory Tip: 🧠 Myeloid → granulocytes, monocytes& dendritic cells; Lymphoid → lymphocytes
How much of the spleen is made up of red pulp?
Red pulp makes up about three-quarters (¾) of the spleen and is responsible for filtering blood and removing old red blood cells.
What are key features of the thymus gland?
The thymus gland shrinks with age (involutes) and secretes thymosin.
What is the difference between innate (non-specific) and adaptive (specific) immunity?
Innate (non-specific) immunity: Present at birth, works immediately, does not require prior exposure, responds the same way to all pathogens, and does not improve with repeated exposure.
Adaptive (specific) immunity: Develops after first exposure, is not effective at birth, targets specific pathogens, and improves with repeated exposure due to immune memory.
Which white blood cells perform phagocytosis?
The white blood cells that perform phagocytosis are:
Neutrophils – the first responders that rapidly engulf and destroy pathogens.
Monocytes/Macrophages – monocytes circulate in the blood and become macrophages in tissues, where they continue phagocytosis and present antigens to T cells.
Dendritic cells – specialized phagocytes that capture antigens and serve as antigen-presenting cells (APCs) to activate T cells.
What is the activation of complement?
When complement proteins in the blood are triggered by antigens or antibodies, they start a chain reaction that helps fight infections. This cascade:
Opsonizes pathogens: Tags microbes so immune cells can eat them more easily. (Tags pathogens — marks them so immune cells can eat them easily)
Triggers inflammation: Calls immune cells to the infection site.
Causes cell lysis: Forms the membrane attack complex (MAC) that pokes holes in microbes, killing them.
Memory Tip: 🧠 OIL = Opsonization, Inflammation, Lysis
What are the steps of second-line defense?
🛡 Second Line of Defense — Internal Battle
Goal: Destroy pathogens that slip past the first line (skin + mucous membranes).
⚔ Step-by-Step (Easier to Memorize)
1⃣ Pathogen Break-In
→ Germs enter tissues after breaking through skin or mucous membranes.
2⃣ Alarm Sounds (Inflammation Begins)
→ Damaged cells release histamine and other chemicals to signal danger.
3⃣ Vasodilation = Redness & Swelling
→ Blood vessels widen → more blood, fluid, and WBCs rush to the area.
4⃣ Phagocyte Migration (Chemotaxis)
→ Neutrophils and macrophages follow the chemical trail to infection.
5⃣ Phagocytosis = Eat & Destroy
→ Phagocytes engulf and digest pathogens using enzymes.
6⃣ Complement Activation
→ Complement proteins:
Opsonize (coat pathogens for easy eating)
Punch holes (membrane attack complexes)
7⃣ Fever & Antimicrobial Substances
→ Body temp rises to slow microbe growth.
→ Interferons & complement proteins block pathogen spread.
8⃣ Tissue Repair
→ Once pathogens are gone, inflammation decreases and healing begins.
What is the goal of the first line of defense?
To prevent pathogens from entering the body.
What are antigens, antibodies, and pathogens?
🦠 Pathogen
A pathogen is the whole disease-causing organism, like a bacterium, virus, fungus, or parasite.
It’s the invader that causes illness.
Example: The influenza virus (the flu) is a pathogen.
🎯 Antigen
An antigen is a specific molecule or structure on the pathogen that your immune system recognizes as “foreign.”
Usually a protein, sugar, or toxin on the pathogen’s surface.
It’s the target the immune system identifies.
Example: The spike protein on the coronavirus is an antigen.
🛡 Antibody
An antibody is a Y-shaped protein made by B cells (a type of white blood cell) in response to a specific antigen.
It binds exactly to that antigen like a lock and key, neutralizing the pathogen or marking it for destruction by other immune cells.
Example: Anti-spike antibodies bind to the coronavirus spike protein to block infection.
🧩 In short:
The pathogen is the invader,
the antigen is the recognizable part of that invader,
and the antibody is the weapon your immune system makes to fight it.
🦠 The pathogen is the burglar,
🎯 the antigen is the burglar’s fingerprint,
🛡 the antibody is the detective’s handcuff that fits that fingerprint perfectly.
Compare innate and adaptive immunity by giving an example of how each responds to a pathogen. Include whether the response has memory or not.
Innate Immunity (general, immediate, no memory)
Cut on your skin → neutrophils rush to the site to attack any bacteria.
Inhalation of dust containing microbes → macrophages in the lungs engulf and destroy invaders immediately.
Fever response to infection → body raises temperature to slow pathogen growth, regardless of the specific microbe.
Key: Works right away but doesn’t “remember” the pathogen.
Adaptive (Specific) Immunity (targets specific antigens, has memory)
Chickenpox infection in childhood → body produces antibodies and memory B/T cells. If exposed again, the immune system responds faster and stronger, preventing disease.
Flu vaccination → introduces antigens so memory cells are ready for future infections.
Allergy testing → adaptive immune cells react to a specific antigen that the body has seen before.
Key: Slower at first exposure but faster and stronger upon re-exposure.
What is lymph and what does it do?
Lymph is a clear fluid derived from interstitial fluid that circulates in the lymphatic system. It:
Transports immune cells to fight infections
Returns excess tissue fluid to the bloodstream
Carries fats from the digestive system
Memory Tip: 🧠 Lymph = tissue fluid + immune cells on the move
Are PAMPs and DAMPs PRRs? Explain the difference between them.
❌ No — PAMPs and DAMPs are not PRRs.
PAMPs (Pathogen-Associated Molecular Patterns): Molecules found on pathogens (e.g. LPS, flagellin, viral RNA).
DAMPs (Damage-Associated Molecular Patterns): Molecules released by damaged or dying host cells (e.g. ATP, HMGB1, uric acid).
PRRs (Pattern Recognition Receptors): Receptors on immune cells that detect PAMPs and DAMPs, triggering an immune response (e.g. Toll-like receptors, NOD-like receptors, RIG-I).
🧠 Summary:
PAMPs & DAMPs = signals
PRRs = sensors that recognize those signals.
What are the three types of barriers in the first line of defense?
Physical, Chemical, and Biological barriers.
What are examples of physical barriers in the first line of defense?
Skin: tough, waterproof shield
Mucous membranes: trap microbes
Cilia: sweep mucus and germs out of airways
What are examples of chemical barriers in the first line of defense?
Acidic pH (stomach, sweat, vaginal secretions) kills microbes
Lysozyme (in tears, saliva, mucus) breaks bacterial cell walls
Sebum and sweat have antimicrobial substances
What is an example of a biological barrier?
Normal flora (beneficial microbes) that compete with harmful bacteria for space and nutrients.
What’s an easy way to remember the first line of defense?
Think “Physical, Chemical, Biological” = Skin, Secretions, Symbiotic bacteria — your body’s first wall of defense.
What does lymph collect as it drains from tissues?
It picks up bits of bacteria, viruses, toxins, damaged cells, and sometimes cancer cells — giving a “snapshot” of what’s happening in tissues.
Where does lymph flow for immune monitoring?
Through lymph nodes, which act as immune checkpoints containing lymphocytes (B & T cells) and macrophages that inspect the lymph.