Exotics Diseases/Conditions
1/129
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
130 Terms
Rabbit
Lagomorphs
Strict herbivores, fiber-rich diet Caecotrophy
Specialized dentition, continuously growing
Hing-gut (caecal) fermentation
Huge variety of breeds - different haircoat, external ear anatomy, body size
Lifespan 8-10 y
Social - should live in bonded pairs

Ferret
Carnivore (hypercarnivore) - need high protein diets
Domesticated from wild polecats (Mustela putorius)
Sexual dimorphism (males are larger)
Females are seasonal induced ovulators
Lifespan 6-8 y
Some variety of colour morphs (sable, albino, etc)

Guinea Pig
Rodents
Strict herbivores
Hystricomorphs - all teeth continuously growing
Hind gut fermentation (caecum) - mostly anaerobic gram +ve gut flora
Caecotrophy
Lifespan 5-6 y
Some variety of hair colour, length (hairless varieties as well)
Very social - should live in groups

Chinchillas
Hystricomorph Rodents - all teeth continuously growing
Strict herbivores
Adapted to cold, dry environments
Very dense haircoat
Lifespan 8-10 y (likely more)
Some variation in hair colour
Can fur or tail slip if roughly handled

Rats
Rodents
Myomorphs - only incisors grow continuously
Omnivores
Require relatively dry, well ventilated environments
Very social - should live in same-sex groups
Smart - need environmental enrichment
Lifespan 2-3y
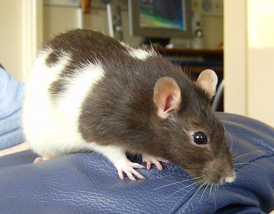
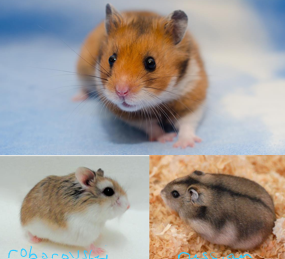
Hamsters
Myomorph Rodents - only incisors grow continuously
Omnivores
3 common species kept as pets - Syrian, Roborovski, Russian
Solitary, non-social
Frequently kept as a children’s first pet
Lifespan 1-2 y
Frequently bite when handled
Degus
Hystricomorph rodents
Increasing popularity as pets
Small (180 – 350g)
Social
Hind-gut fermenters + coprophagy
Strict herbivores
Elodont dentition
Similar diet to Chinchillas
Lifespan 5-6y
Can tail slip, difficult to restrain

Gerbils
Most common species kept = Mongolian gerbil (Meriones unguiculatus)
Desert adapted species
Social
Myomorph rodents
Lifespan 3-5y
Ventral scent gland
Pelleted diet
Can also slip their tail

African Pigmy Hedgehog
Insectivores
Arid areas of central and East Africa
Nocturnal
Spikes and typical curling behaviour
Solitary
Self-anointing/anting
Very large enclosures w/ hiding places
T = 22-32oC
Offer dry food, some vegetables and insects
Lifespan 5-6y

European Hedgehog
Insectivores and other invertebrates
Western Europe
Nocturnal
Hibernate during winter months
Wild populations declining in the UK

Bearded Dragon
Pogona vitticeps
Medium-size lizards (400-700g)
Omnivores to herbivores as they mature
Terrestrial/dry environment - basking temp 33-40oC, lower end temp 27oC, UV-B exposure essential (vitamin D/calcium metabolism), UV-A (behaviour)
Kept as a single pet
Some variation in colour
Lifespan 8-12y

Leopard Gecko
Eublepharis macularius
Small lizards (60-100g)
Insectivores
Terrestrial/dry environment - 22-33oC, UV-B exposure essential (vitamin D/calcium metabolism), UV-A (behaviour), hiding places w/ high humidity
Kept as single pet
Huge variation in colour/pattern
Lifespan 10-12y
Can shed their tails or skin when handled
Very delicate skin

Tortoises
Several species commonly kept - Horsfield’s (Agrionemys horsfieldii), Greek (Testudo graeca), Hermann’s (T. hermanni)
All strict herbivores
Small to medium sized
Terrestrial temperate to dry environment - 24-38oC, UV-B exposure essential (vitamin D/calcium metabolism), UV-A (behaviour)
Very long lifespans (up to 80y)
Some individuals routinely hibernate
Can be kept in groups or single

Cornsnake
Pantherophis guttatus
Small to medium size snakes
Strict carnivores (rodent prey)
Terrestrial environment - 21-30oC, UV-B exposure essential (vitamin D/calcium metabolism), UV-A (behaviour)
Lifespan 15-20y
Should be kept single
Huge variety of colour morphs

Budgie
Melopsittacus undulatus
In the wild, feeds on a variety of seeds.
As pets - balanced seed mixes, pellets, some greens
Very social and easy to breed
Appropriate cage size/design
Environmental enrichment - perches, toys, bathing
Variation in size/plumage
Lifespan 7-15 y

African Grey Parrot
Psittacus erithacus
Medium size (350-500g)
Feeds on variety of fruits, seeds and berries, pellets, mix vegetables/fruit, calcium supplements + UV-B?, UV-A for behaviour
Appropriate cage size/design
Environmental enrichment - perches, toys, bathing
Social interactions
Lifespan 20-30y

Domestic Chicken
Gallus domesticus
Most are ex-battery egg-laying hens
Mixed indoors (coop with perches + nesting boxes) and outdoors
Diet - commercial pellets, some grains/vegetables, insects/invertebrates, grit
Kept in all female groups +/- 1 male
Several breeds
Lifespan5-12y

Rabbit Vaccinations
Myxomatosis
Viral Haemorrhagic Disease 1 and 2
First dose from 5 weeks old, yearly booster
Ferret Vaccinations
Distemper (use dog vaccine but with sterile saline, not solvent) - first dose at 12 weeks, yearly booster
Rabies - travelling ferrets, first dose at 12 weeks, 18 month boosters
Anaphylactic vaccine reactions - 5-25 mins after any vaccine, hyperaemia, vomiting, hypersalivation, occasionally diarrhoea, dyspnoea, cyanosis
Treatment - adrenaline, diphenhydramine (can give prior to vaccine), dexamethasone, supportive care
Bird Vaccinations
Pigeons - avian pox, paramyxovirus
Canaries - avian pox
Poultry - can use commercial vaccine schedules
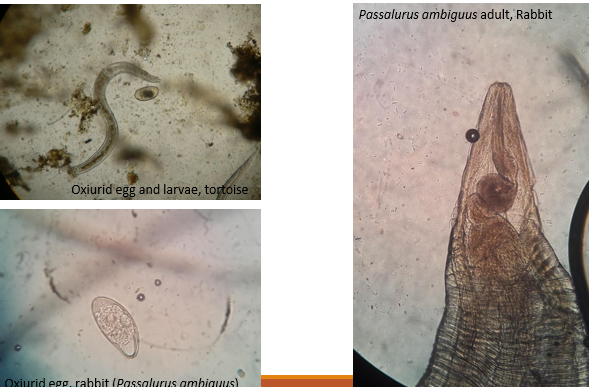
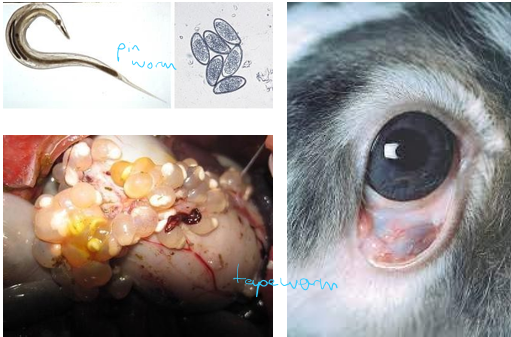
Oxyurids (pinworms)
Reptiles, rabbits, rodents
Considered commensals, but numbers increase in immunosuppressed patients
Treat if high egg count, ill patient - any wormer except Ivermectin
Ciliates
Commensals/low pathogenicity in Tortoises, herbivore lizards
Significant on other species
Detected with direct wet mounts

Wormers
Praziquantel - tapeworms, oral, injectable, spot-on
Oxfendazole - nematodes, oral
Fenbendazole - oral, toxicity (immunosuppression) in rabbits and birds
Ivermectin/Selamectin/Moxidectin - nematodes, external parasites, injectable, oral, spot-on, toxic to chelonians, skinks, and some snakes
(Moxidectin for heartworm prevention in ferrets)
External Parasite Control
Fleas - rabbits or ferrets, Imidacloprid
Flystrike - rabbits in summer, Cyromazine
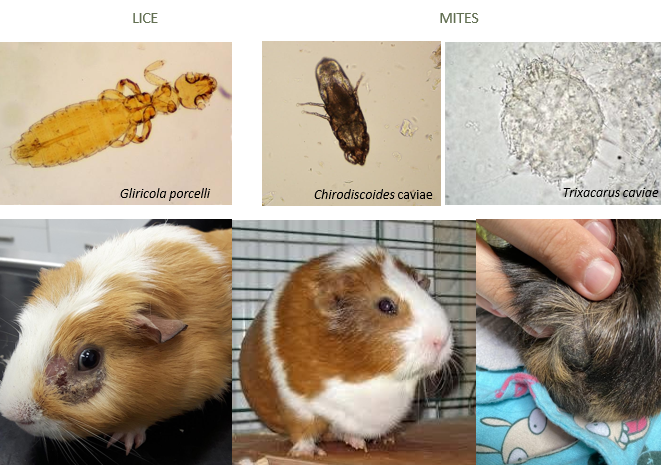
Lice/mites - rodents in groups or rabbits, Ivermectin etc
Feather lice - some birds in groups, Permethrin powder/spray
Neutering Exotics
Rabbits, male guinea pigs, male rats
Guinea pigs and rodents have increased risk of anaesthesia and post-op complications
Female ferrets can stay in oestrus indefinitely → hyperoestrogenism → bone marrow suppression and aplastic anaemia
Neutering ferrets not recommended - gonads provide negative feedback to hypothalamus and suppresses adrenal function (androgen production, affects circadian rhythm/photoperiod)
Deslorelin implants for ferrets - apply every 18-24 months
Anaesthesia Considerations for Birds
Susceptible to hypothermia
Most species not domesticated - peri-anaesthetic stress
Small species have difficult venous access and monitoring limited
Uncuffed ET tubes - complete partially overlapping tracheal rings
Pigeons and ducks have a lot of tracheal mucus - can block ET tube
No diaphragm - reduced ventilation in dorsal recumbency as pectoral muscle weight on ribs
Air sacs compressed by effusions, enlarged organs, fat deposits
Have higher oxygen demands
Higher HR
Higher BP (90-180mmHg)
Renal portal system may affect drug administration and distribution
Fasting pre-op not advised in <500g patients, 2-4 hours for larger
African Grey Parrots especially prone to hypocalcaemia
Sedation / Anaesthesia for Birds
Midazolam and Butorphanol - reverse with Flumazenil
Alfaxalone (propofol limited as only IV)
Atropine - only in bradycardia/CPR situations (<30s window)
Sevoflurane usually preferred over isoflurane (slower induction, hypocalcemia, arrhythmias, hypertension)
Analgesia for Birds
Meloxicam
Carprofen
Gabapentin
Butorphanol
Tramadol
Buprenorphine
Fentanyl
(flunixin, ketoprofen, dicofenac - toxic)
Lidocaine or Bupivicane for local anaesthesia
Emergency Drugs for Birds (if crashed)
Atropine
Adrenaline
Dextrose
Emergency Presentations of Birds
Dyspnoea
Non-specific illness
Trauma/bleeding
Reproductive - egg binding, egg yolk coelomitis
Neurological - seizures, paresis/paralysis
Regurgitation
Prolapses
Anaesthesia Considerations for Reptiles
Hepatic portal system - drug administration/distribution altered
Diving reflex in aquatic reptiles - R to L shunt and bypassing pulmonary circuit, hold breath so don’t breath in gas anaesthesia
Hypoxia increases respiratory rate
Uncuffed ET tubes
Chelonians have gular movements (olfactory) - don’t confuse with RR
Fasting 2-3 hours for most, 1-2 days for snakes and chelonians
Sedation/Anaesthetics for Reptiles
Midazolam and Dexmedetomidine
Alfaxalone / Propofol
Isoflurane
Ketamine (snakes)
(Atipamezole/Flumazenil reversal)
Atropine (chelonians breath-holding)
Analgesia for Reptiles
Methadone
Tramadol
Morphine
Meloxicam
Lidocaine or Bupivicaine
(butorphanol has no analgesic effects)
Emergency Presentations of Reptiles
Trauma
Prolapses - bladder, cloacal, false
Reproductive
Neurological - stargazing, loss of righting reflex, tremors
Most ‘emergencies’ are chronic cases or unnoticed disease that recently decompensated
Anaesthesia Considerations in Exotic Mammals
Prey animals - stress
Hypoxia and breath holding common - obligate nasal breathers
Prone to hypothermia
IV access limited in most
ET tube placement difficult, uncuffed, lidocaine spray, or V-gel
Fasting not advised - don’t vomit, ferrets prone to hypoglycaemia
Difficult to monitor if small
Sedation / Anaesthesia for Exotic Mammals
Midazolam and Butorphanol
Ketamine and Medetomidine
Sevoflurane
Alfaxalone
Analgesia for Exotic Mammals
Meloxicam
Carprofen
Buprenorphine
Tramadol - questionable if works
Gabapentin
Maropitant
Lidoaine or Bupivicaine
Emergency Presentations of Rabbits
Gut stasis - fluids, analgesia, prokinetics (metoclopramide), feeding, supportive care
Trauma - fractures, bite wounds
Respiratory - URT, pneumonia, heart disease, neoplasia
Neuro - seizures, paresis/paralysis, sudden and progressive head tilt
Haematuria with straining
Sudden blepharospasm, buphthalmia, or exophthalmia
Flystrike

Emergency Presentations of Ferrets
Trauma
Frequent vomiting >24h
Non-specific illness with anorexia >24h
Neuro - seizures, ataxia, collapse, paralysis
Dyspnoea

Emergency Presentations in Rodents
Gut stasis
Dyspnea - especially Guinea pigs
Trauma
Neuro – seizures, collapse, paralysis
Non-specific illness
Urogenital - bleeding and straining/vocalizing, dystocia
Abnormal perineal discharge - ‘wet tail’, diarrhoea, intestinal prolapse etc
Myxomatosis in Rabbits
Leporipoxvirus
Naturally infects wild rabbits, spreads to domestic
Clinical Signs - eyelid thickening and purulent eye discharge, nodules on ears/lips/nares/eyelids/external genitalia, occasionally pneumonic signs, infertility, death by starvation and secondary infections
Treatment - euthanasia advised, stick isolation, risk of carriers
Vaccination and avoid wild rabbit contact

Shope Fibroma in Rabbits
Different Leporipoxvirus
Induces self-limiting fibromas/fibromatosis
Cross-immunity against Myxomatosis
Viral Haemorrhagic Disease (VHD) in Rabbits
Calicivirus - two strains
Highly infectious - urine, faeces, aerosols, biting insects
High mortality rates
Causes necrotising hepatitis, DIC, acute liver failure, fibrinous thrombi, haemorrhage, organ failure, death in 3-4 days
Clinical signs - fever, increased RR, collapse, hypotension, neuro signs, haemorrhages (not always)
<4 week old rabbits resistant to infection
Diagnosis - PCR, PM and histology
Treatment - euthanasia
Vaccination
Papillomatosis in Rabbits
Can refer to:
Shope papillomavirus - SCC-like neoplasia
Oral papillomavirus - benign wart-like growths, self-limiting
Ano-rectal papillomatosis - not viral induced, cauliflower masses that bleed easily

Pasteurellosis in Rabbits
‘Snuffles’
Pasteurella multocida - several strains, primary pathogen in immunosuppressed rabbits, secondary pathogen in abscesses
Produces endotoxin
Transmitted by direct contact and aerosols
Clinical Signs - rhinitis, pneumonia, genital infections, wounds and abscesses, dacryocystitis, otitis media/interna (head tilt), eye discharge if affecting lacrimal duct
Diagnosis - deep nasal swab for c&s, PCR
Treatment - isolate, antibiotics, supportive care

Treponema paraluiscuniculi in Rabbits
‘rabbit syphilis’
Genital infection - vertical and sexual transmission
Nodules, crusting lesion that can ulcerate on vulva/prepuce/lips/nostrils
Diagnosis - histology with special silver stains
Treatment - penicillin SC (never oral beta-lactams in rabbits)
Bacterial Enteritis in Rabbits
Several possible pathogens
Tyzzler’s disease - 6-12 wo rabbits, diarrhoea, sudden death, intestinal fibrosis/stenosis and liver necrosis if chronic
Clostridial Endotoxaemia - overgrowth of Clostridium spp producing Iotatoxin, due to starch rich diets (caecum overload), stress, oral antibiotics (beta-lactams, -mycin)
Others - Salmonella, E coli, Campylobacter etc
Treatment - fluids, high fibre and low sugar/starch diet, antibiotics (fluoroquinolones, metronidazole), analgesics, cholestyramine (reduces toxin absorption), maropitant

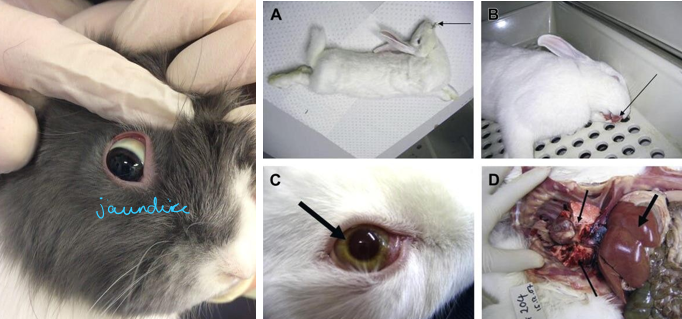
Coccidiosis in Rabbits
Intestinal - mixed Eimeria spp, often if young or in groups, diarrhoea ± blood, weight loss
Hepatic - Eimeria stiedae, diarrhoea and weight loss, hepatomegaly, jaundice, higher mortality
Treatment - Toltrazuril, TMP and sulphonamides, supportive care, diet managment, reduce stress
Intestinal cases become immune
Hepatic cases have chronic changes

Tapeworms in Rabbits
Rabbits are intermediate hosts - carry larval forms (not detected on faecal samples)
Cysticercus pisiformis - peritoneal cavity, liver
Coenurus serialis - SC tissues
Echinococcus granulosus
Mites in Rabbits
Psoroptes cuniculis - ear mites
Cheyletiella parasitovorax - skin mites
Leporacarus gibbus - fur mites
Diagnosis via skin scrapes, hair plucks
Frequently secondary to grooming problems (dental disease, arthritis, spinal disease) or immunosuppression
Treatment - Selemectin, Moxidectin

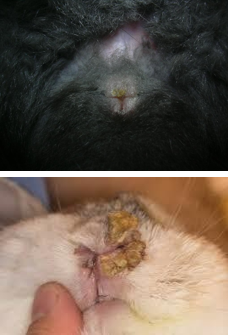
Flystrike in Rabbits
Maggots of Lucilia spp or Calliphora spp flies
Tail base and perineum most commonly affected
Risk factors - outdoors, high temps, soiled skin, overweight, difficulty grooming, uneaten caecotrophs
Very quick progression 3-4 days
Treatment - remove maggots and clip under sedation, Ivermectin SC, bathe in dilute iodine solution, dry area, analgesia, supportive care, treat underlying cause
Prevention - Cyromazine spot-on, good husbandry, hygiene, diet

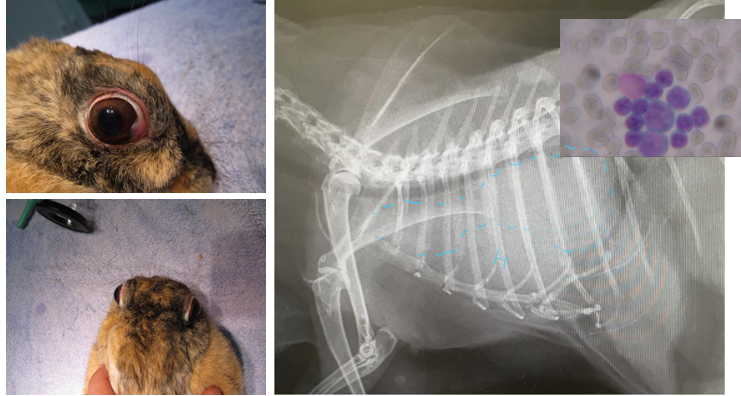
Encephalitozoonosis in Rabbits
Encephalitozoon cuniculi - microsporidia, intracellular, zoonosis
Most subclinical - clinical signs develop when infected cells rupture with spores
Transmission via inhalation, ingestion, vertical
Neurological presentation - head tilt, nystagmus, facial paralysis, paresis/paralysis, muscle weakness, seizures
Eye lesions - phacoclastic uveitis, lens opacity/rupture, cataracts
CKD - PUPD, urine scald, progressive weight loss
Diagnosis - serology IgM or IgG, PCR of urine (shedding intermittent)
Treatment - Fenbendazole, NSAIDs, fluoroquinolones or doxycycline, eye drops, midazolam if seizures, supportive care
Hair Matts in Rabbits
Long or densely haired breeds
Frequently have secondary bacterial dermatitis
Can be painful
Treatment - clip under sedation, analgesia, bathe skin, treat underlying problem

Bacterial Dermatitis in Rabbits
Most secondary to other conditions - urine scalding, skin fold dermatitis, epiphora/blocked tear ducts, dental disease and drooling, matted hair
Common isolates - S aureus, P multocida, P aeruginosa
Superficial to deep pyoderma, occasionally abscess formation
Painful
Treatment - Meloxicam, antibiotics, (don’t use steroids in rabbits, immunosuppression), hair clipping, keep dry, topical chlorohexidine, fusidic acid, silver sulfadiazine, correct risk factor

Pododermatitis in Rabbits
Avascular necrosis/pressure sores of plantar surfaces (can affect front paws too) - guard hairs not protecting
Painful
Risk factors - obesity, inactivity, inadequate flooring, loss of plantar guard hairs, concurrent conditions, contaminated bedding
Can get skin hyperkeratosis, secondary bacterial infections, osteomyelitis, osteoarthritis, displacement of superficial digital flexor tendon
Treatment - relieve pressure (bedding, bandaging, exercise), analgesia (meloxicam, gabapentin), antibiotics, keep clean and dry, surgery if chronic/abscesses/debride necrotic tissue, euthanasia

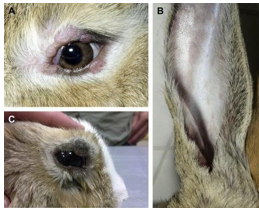
External Ear Disease in Rabbits
Easy build up of cerumen (wax) as kinked and narrow canal and ear base diverticulum (gap between tragus and annular cartilage)
Common Signs - head shaking, pruritus, discharge, increased cerumen, ear base swelling, facial paralysis (facial nerve in close proximity)
Common diseases:
Aural haematoma/oedema
Traumatic Lacerations
Neoplasia
Otitis externa - lop breeds, clean, often chronic, may need TECA etc

Urinary Disorders in Rabbits
Common - cystitis, uroliths, CKD, AKI
Common signs - weight loss, anorexia, gut stasis, pollakiuria/dysuria, pain when urinating, PUPD, urinary incontinence, haematuria, urine scald
Alkaline urine - calcium crystals normal
Limited capacity to excrete H+ so sensitive to systemic acidosis
Stress reduces renal blood flow
Calcium mainly regulated by the kidneys - excrete large amounts of Ca in urine as excess absorbed in GI tract
‘Sludgy urine’ in Rabbits
When calcium builds up in bladder
Can lead to cystitis, uroliths, incontinence etc
Common signs - dysuria/pollakiuria, painful urination, PUPD, incontinence, urine scalding, haematuria, abnormal urine
Treatment - analgesia, antibiotics, manage urine scald, clean bedding, increase exercise, increase water intake, reduce calcium intake, catheterise and flush bladder

Urolithiasis in Rabbits
Calcium carbonate, oxalate, phosphate
Predisposing factors - urinary obstruction, reduced water intake, reduced urine outflow, high calcium diet
Diagnosis - bloods (check renal failure), radiographs, ultrasound
Treatment - cystotomy, flush back to bladder, nephrectomy, analgesia, ACE inhibitors
Acute Kidney Injury in Rabbits
Many causes - congenital, infections, renal amyloidosis, urinary obstruction (sludge, urolith, etc), renal calcification (2ary to high Ca2+ blood levels), toxins, stress and reduced renal blood flow
USG isothenuric
Bloods - increased urea and creatinine and phosphate, normal calcium
Treatment - fluids, reduce stress, analgesia, treat underlying cause
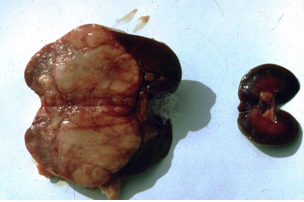
Chronic Kidney Disease in Rabbits
Many causes - congenital, infections, neoplasia, renal amyloidosis, E. cuniculi (nephritis, fibrosis), urinary obstruction (sludge, urolith, etc), renal calcification (2ary to high Ca2+ blood levels), toxins, stress and reduced renal blood flow, degenerative
Clinical Signs - PUPD, anorexia, weight loss
USG variable
Bloods - increased urea and creatinine, usually increased calcium and phosphate, anaemia
Treatment - fluids SC, increase water intake, ACE inhibitors, phosphate binders, treat main cause, low calcium diet
Vestibular Disease in Rabbits
Common neurological problem
Clinical Signs - head tilt, ataxia, paresis, rolling, facial nerve paralysis, nystagmus
Possible causes - E cuniculi, pasteurelosis, toxoplasma, neoplasia, head trauma
Peripheral disease - lesions on cochlea, middle ear or vestibular nerve, only horizontal and rotational nystagmus
Central disease - brainstem lesions, vertical/positional nystagmus ± intention tremors, hemiparesis, E cuniculi possible cause
Treatment - meloxicam, antibiotics, prochlorperazine (anti-vertigo), Fenbendazole if E cuniculi, exercise in padded environment, reduce stress, feeding, monitor for corneal ulcers
‘Floppy Rabbit Syndrome’
Generalised muscle weakness → paresis → paralysis
Many possible causes - neurological, hepatic lipidosis, hypokalaemia, toxicity, E cuniculi, myasthenia gravis, vitamin E/selenium deficiency
Self-limiting if not an above cause, 2-3 days with supportive care
Uterine Adenocarcinoma in Rabbits
Most common neoplasia in rabbits
Slow growing, locally invasive, ± distant metastasis
Clinical Signs - haematuria, palpation
Treatment - spay

Bile Duct Adenoma/Adenocarcinoma in Rabbits
Usually secondary to bile duct irritation and hyperplasia - Eimeria stiedae
Often incidental finding on ultrasound or PM
Could surgically remove if solitary mass
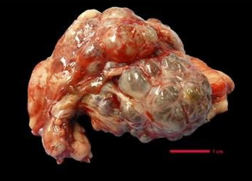
Embryonal Nephroma in Rabbits
Benign, slow growing
Not associated with renal dysfunction or failure
Often incidental finding of ultrasound or PM
Treatment - monitoring, nephrectomy
Lymphoma in Rabbits
Most cases not accompanied with leukaemia
Can affect any age group
Usually multicentric - including the dermis and eye
Non-specific clinical signs - weight loss, lethargy, palpable abdominal masses or lymph nodes
Diagnosis - cytology, ultrasound, radiography, haematology
Multiple chemotherapy protocols described
Thymoma in Rabbits
Clinical signs - respiratory changes, heart sounds muffled, bilateral exophthalmia
Can be difficult to differentiate from Thymic lymphoma
Diagnosis - radiography, ultrasound, cytology
Treatment - surgical, chemotherapy, radiotherapy
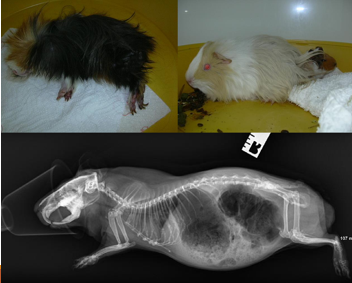
Diarrhoea in Guinea Pigs
Uncommon in adults - young/immunocompromised patients
Old males - faecal impactions secondary to loss of muscle tone on anal sphincter
Due to:
Diet - inadequate fibre/high simple carbohydrates
Bacterial infection - Tyzzer’s disease, salmonella, E coli, Yersinia
Dysbiosis/enterotoxaemia - after incorrect use of antibiotics, clostridial growth
Cryptosporidium wrairi
Eimeria caviae
Balantidium caviae
Hepatopathies
Dental Disease
Diagnosis - faecal flotation, faecal culture, bloods, abdominal US
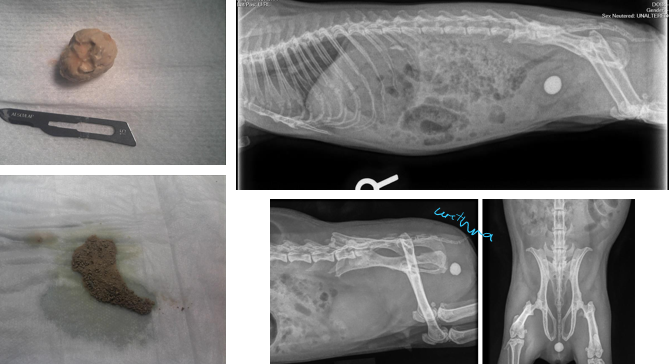
Urolithiasis in Guinea Pigs
Common
90% Calcium carbonate
Secondary cystitis and UTI is common
Frequently recurrent
Clinical Signs - haematuria, dysuria, pain/vocalisation during urination, anorexia, lethargy, hunched posture
Diagnosis - radiography, ultrasound
Treatment - <5mm can pass unaided, analgesia (meloxicam, maropitant), GA and flush/cystotomy, reduce calcium in diet, potassium citrate (urine acidifier)
Cystitis in Guinea Pigs
Often 2ary to urolithiasis
Same clinical signs as urolithiasis (without the uroliths)
Can be sterile or bacterial
Diagnosis - urinalysis +/- urine c&s, US scan, antibiotics (Marbofloxacin, TMP + sulfa), Meloxicam ± Maropitant
Ovarian Cysts in Guinea Pigs
Very common in older intact females
Serous cysts - non-functional, develop spontaneously, don’t respond to LH, only clinical signs if too large
Follicular cysts - follicles that fail to ovulate, hormonally active, respond to LH, variable clinical signs (non-pruritic flank alopecia, mammary gland hyperkeratosis)
If Clinical Signs - anorexia, lethargy, abdominal distension and discomfort, soft tissue mass palpable
Diagnosis - ultrasound
Treatment - hCG x2 14 days apart (follicular cysts), GA and spay, drainage of cysts (refill quickly)

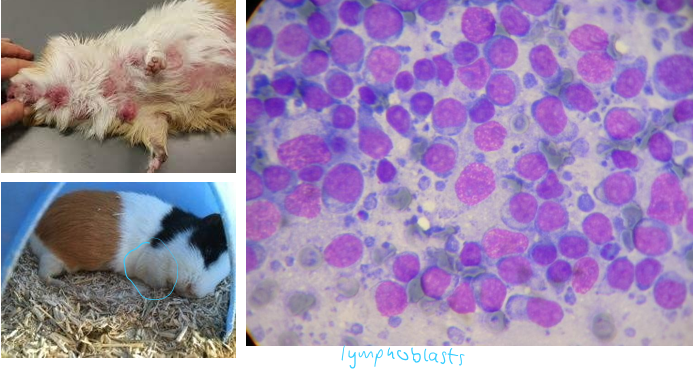
Lymphoid Neoplasia in Guinea Pigs
Common
3 forms - multicentric and highly malignant, epitheliotropic T cell, retroviral leukaemia
Diagnosis - cytology of peripheral lymph glands/skin, haematology, US scan
Treatment - Lomustine, L-asparaginase, palliative prednisolone, euthanasia
Poor prognosis
Skin Disease in Guinea Pigs
Mites/lice
Ringworm/Dermatophytiasis - crust lesions and alopecia, peri-ocular/nostrils, pruritis if secondary infection, zoonotic
Cervical lymphadenitis - Strep equi zooepidemicus, abscesses of cervical lymph nodes after oral abrasions, causes pneumonia, otitis media, septicaemia, surgical excision or lance and flush, antibiotics
Sebaceous lumps - old boars, rump and lower back, cysts/adenoma/trichoepithelioma/trichofolliculoma, surgical removal
Pododermatitis
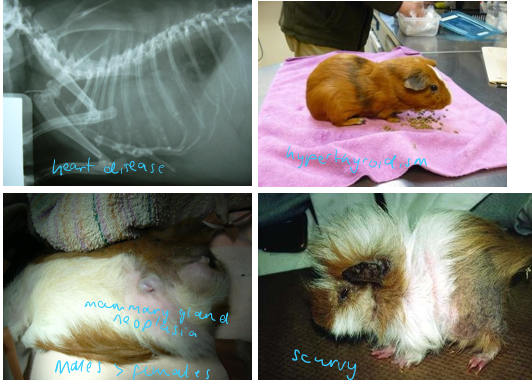
Other Conditions in Guinea Pigs
Hyperthyroidism
Hyperadrenocorticism
Insulinoma
Fibrous osteodystrophy
Hypovitaminosis C
Mammary gland neoplasia and mastitis
Pneumonia
Heart disease – most common pericardial effusion, DCM
Respiratory Disease Complex in Rats
URT infection - sneezing, nasal discharge, porphyrin staining around nostrils, noisy breathing
LRT infection - increased RR and effort, noisy breathing, crackles, muffled heart sounds
Risk if stress/immunosuppression, environmental e.g. cage ventilation
Due to:
Viral - Sendai virus, paramyxovirus
Bacterial - Mycoplasma pulmonis, Strep pneumonis, Cillia-associated Bacillus, Haemophilus spp
Fungal - Pneumocystis carinii
Diagnosis - clinical suspicion ± radiography
Treatment - antibiotics >3w (doxycycline, marbofloxacin, azithromycin), meloxicam, nebulisation, furosemide if secondary lung oedema
Mammary Gland Neoplasia in Rats
Most common neoplasia
Mammary fibroadenoma - most common, benign, associated with reproductive changes
Mammary adenocarcinoma - malignant
Treatment - surgical removal (mammary strip), spay, Cabergoline (prolactin antagonist) to slow progression, palliative, euthanasia
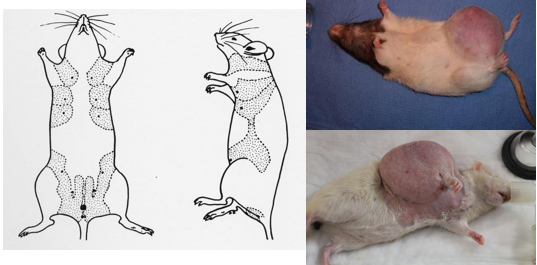
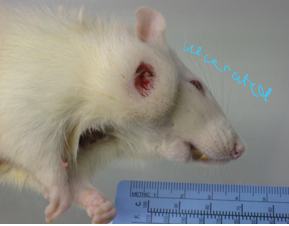
Zymbal’s Gland Tumours in Rats
Zymbal gland – specialized sebaceous gland on rat’s ear canal
Locally invasive carcinomas
Frequently mistaken for abscesses or ear infections
Often ulcerate
Treatment - palliative (surgical removal difficult/impossible)
Pituitary Adenomas in Rats
Neurological signs - paresis/paralysis on FLs, vision loss, ataxia
Progressive
Diagnosis - MRI or CT scan
Treatment - surgery not realistic due to location, Cabergoline, NSAIDs

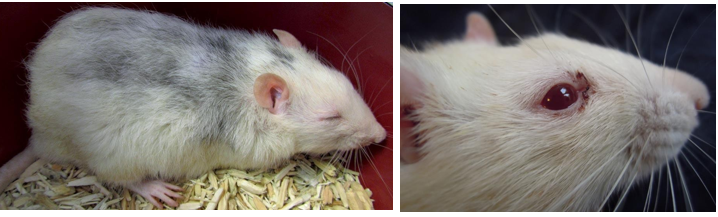
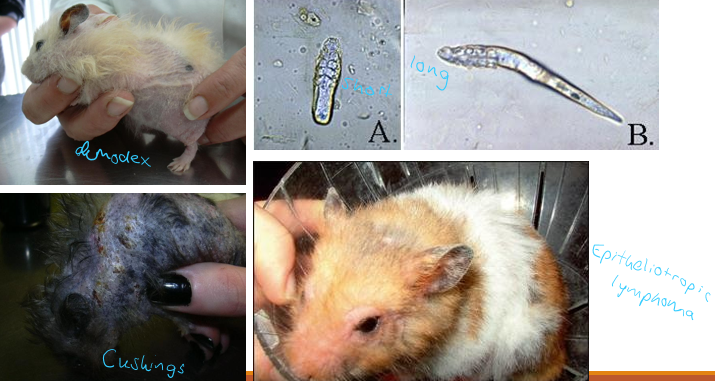
Skin Disease in Hamsters
Often present with alopecia, pruritus, masses, ulcers and scabs, inflamed area of skin
Stress/immunosuppression often a trigger
Demodex criceti, aurati - Ivermectin SC
Hyperadrenocorticism - look for PUPD, cortisol levels
Epitheliotropic Lymphoma - syrians, skin biopsy, prednisolone
Bacterial dermatitis
Hypothyroidism
Skin Abscesses
Skin Neoplasia - melanomas, fibromas, papillomas
Ringworm
Other external parasites - Ivermectin SC
Treatment - meloxicam, antibiotics (TMP + sulpha, marbofloxacin)
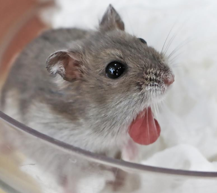
Everted Cheek Pouches in Hamsters
More common in dwarf species
Possible causes - food impaction, inflammation, abscess, neoplasia
Treatment - GA and examine, flush/clean, reposition, suture, ± NSAIDs, antibiotics
‘Wet tail’ in Hamsters
Enteropathies with diarrhoea
Due to:
Lawsonia intracellularis
Enterotoxaemia (Clostridium difficile) after inappropriate AB use
Tyzzer’s disease - C. piliforme
Diet - sudden changes, higher water content
GI parasites - protozoa, pinworms
Severe cases can lead to rectal prolapse +/- intussusception
Diagnosis - faecal mount, gram stain, culture, PCR
Treatment - supportive, SC fluids and glucose, thermal support, antibiotics, feeding

Hepatic Cysts in Hamsters
Occasionally found in older Syrian hamsters
Development defects of bile ducts
Clinical Signs - abdominal enlargement, dyspnoea, diffuse alopecia, lethargy, weight loss
Diagnosis - US scan
Treatment - surgical removal, cyst aspiration (US guided or intra-surgical), palliative care if multiple cysts present
Other Conditions in Hamsters
Dilated Cardiomyopathy
Atrial thromboembolism
Pyometra and endometritis
Uterine neoplasia
Bladder uroliths
CKD
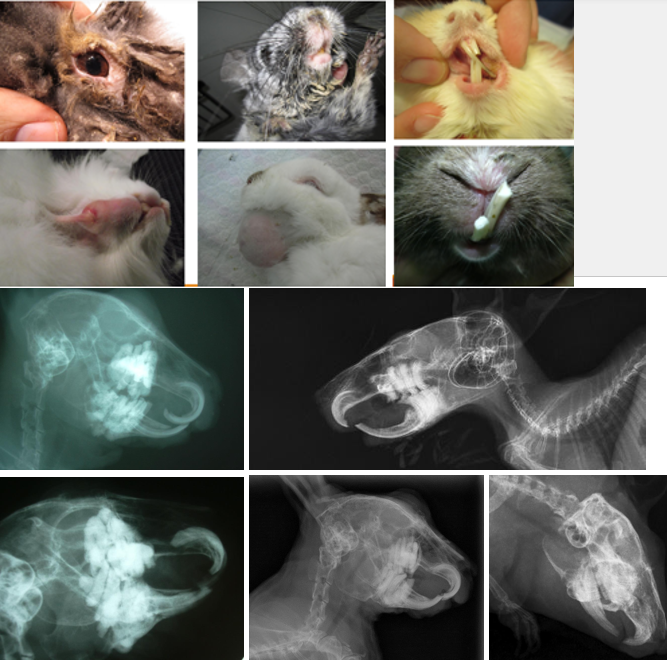
Dental Disease in Rabbits/Rodents
Risk Factors:
Lack of fibre and abrasive food items
Congenital malocclusion
Reduced chewing time/cycles
Trauma
Metabolic demands – e.g. pregnancy, lactation can affect dental growth
Hypovitaminosis D/Metabolic disease
General Clinical Signs - anorexia, selective appetite, weight loss, low BCS, unkept haircoat, gut stasis, excessive salivation, contact dermatitis on chin, lower neck and front paws
Molar Overgrowth Signs - epiphora and dacryocystitis, abscesses (mandibular, maxillary, retrobulbar)
Incisor Overgrowth Signs - obvious overgrowth, abrasions, wounds around lips
Diagnosis - oral exam (otoscope, rigid endoscope, ± GA), skull radiographs
Treatment - review husbandry and diet, more regular health checks, meloxicam, cranial nerve/splash block, surgical correction (crown reduction, incisor extraction), treat wounds and abscesses
Dacryocystitis in Rabbits/Rodents
Occlusion of lacrimal duct by overgrown upper molars/inflammation
Clinical Signs - contact periocular dermatitis, recurrent/chronic eye discharge
Diagnosis - radiographs
Treatment - long term Meloxicam, ± antibiotic eyedrops, lacrimal duct flush under sedation

Retrobulbar Abscessation in Rabbits/Rodents
Affects upper molars
Abscess leads to progressive exophthalmia
Ddx - intra-ocular disease (e.g. glaucoma), retrobulbar neoplasia
Diagnosis - radiographs
Treatment - abscess marsupialization, dental extractions, frequently requires enucleation

Distemper in Ferrets
Morbillivirus (same that infects dogs) - several strains
Almost always fatal in ferrets
Transmission - aerosols (respiratory secretions), direct contact with urine/faeces/skin, fomites
Clinical Signs - lethargy, anorexia, fever, erythema, hyperkeratosis and crusts on footpads/face, dyspnoea, tachypnoea, cough, muco-purulent conjunctivitis, paresis, ataxia, seizures
Diagnosis - unvaccinated, swabs for PCR or antigen detection, PM and histopathology
Treatment - often euthanasia, supportive care (meloxicam, antibiotics, hyperimmune serum from another ferret, vitamin A and C)
Prevention - vaccination, avoid contact with unvaccinated dogs/ferrets, routine cleaning/hygiene
Influenza in Ferrets
Transmission - aerosols (from owners)
Clinical signs - fever, URT signs, conjunctivitis, occasionally affects other organs
Diagnosis - antigen detection (availability?)
Treatment - usually self-limiting (5-7 days), supportive and meloxicam, antivirals
Aleutian Disease in Ferrets (ADV)
Parvovirus
Immunocomplex-mediated disease
Older ferrets (2-4 yo)
Can also infect Minks
Transmission - aerosols/direct contact with any body fluid
Clinical Signs - death without any clinical signs, chronic wasting disease, tremors, ataxia, paresis/paralysis, seizures, organ enlargement, anaemia, melena, dyspnea, weight loss
Diagnosis - low albumin, high gammaglobulin, low PCV, PCR, serum antibody
Treatment - supportive, immunosuppressive prednisolone/ciclosporin, melatonin implants (scavenge free radicals, stimulates antioxidant enzymes)
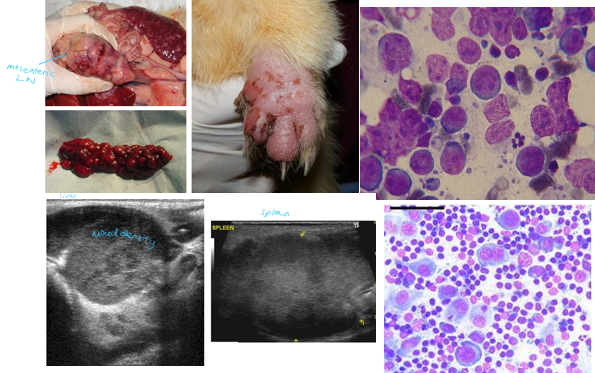
Lymphoma in Ferrets
Common
Types - T cell, B cell, Cutaneous epitheliotropic, gastric
Diagnosis - anaemia, hypoalbuminemia, hyperproteinaemia, hyperglobulinemia, ultrasound, cytology, biopsy
Treatment - chemotherapy (modified COP, CHOP, L-asparaginase), prednisolone, radioation
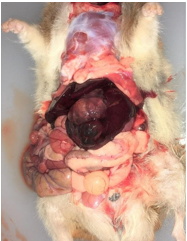
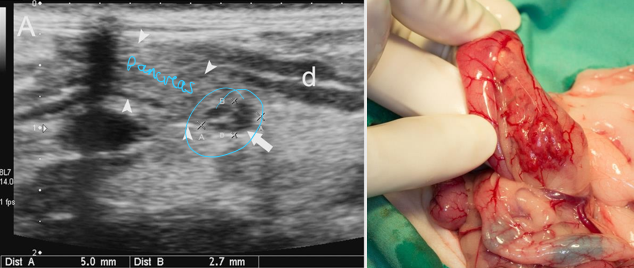
Insulinoma in Ferrets
Benign
Affects pancreatic β-cells (insulin production)
Unknown cause
Clinical signs - nausea/ptyalism, lethargy/weakness, ataxia, seizures, signs often resolve after being offered food
Diagnosis - hypoglycaemia (after 4h starving), plasma insulin concentration, ultrasound
Treatment - surgery (nodulectomy, partial pancreaectomy), dextrose, fluids with glucose, midazolam, prednisolone, diazoxide
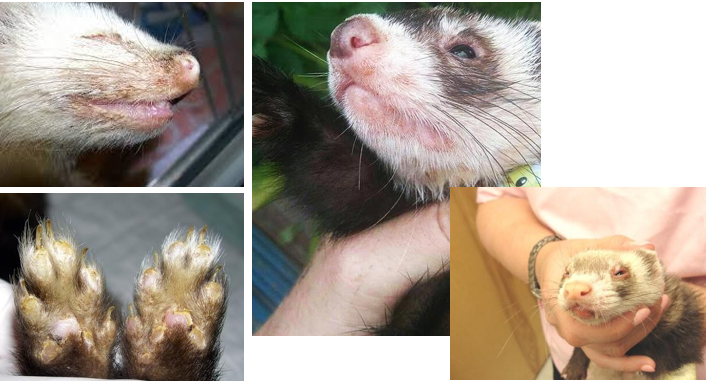
Adrenal Gland Disease in Ferrets
Hyperadrenocorticism (hyperaldosteronism / hyperadrenocorticism, hyperandrogenism)
Due to surgical neuter (removes negative feedback on adrenal cortex), abnormal photoperiod/circadian rhythms (gonadotropins are produced during hours of light), genetics
Clinical Signs - progressive symmetrical alopecia (starts at tail), pruritus, vulvar enlargement (spayed females), urinary blockage from prostate enlargement (males), sexual behaviour and typical odour (males)
Diagnosis - ultrasound, serum/plasma concentrations of hormones
Treatment - adrenalectomy, Deslorelin implants (suppress release of gonadotropins and adrenal gland stimulation)

Gastritis in Ferrets
Common
Clinical Signs - vomiting (vs regurgitation), anorexia, lethargy, melena (GI ulceration is frequent)
Due to - foreign bodies, toxin ingestion, NSAID treatment, Helicobacter mustelae infections, neoplasia, azotaemia/renal disease, other diseases can also cause nausea
Treatment - fluids, anti-emetics, frequent/small meals, highly digestible/high protein diet
Helicobacter mustelae in Ferrets
Chronic gastritis + mucosal ulceration
Triggered by stress
Possible progression to gastric adenocarcinoma / lymphoma
Ulceration → melena, severe anaemia, shock
Diagnosis - gastric wall biopsies ± PCR
Treatment - antibiotics (amoxicillin and metronidazole), bysmuth citrate, sucralphate, famotidine, omeprazole, fluids and supportive care

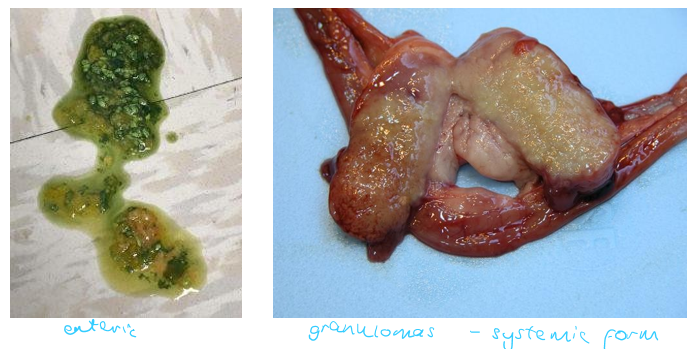
Diarrhoea in Ferrets
Difficult to differentiate between small or large intestinal diarrhoea
Short GIT transit time (3h) – frequent defecation
Due to:
Salmonella
Campylobacter
Ferret Coronavirus Enteric Form - green profuse, tylosin
Ferret Coronavirus Systemic Form - progressive pyogranulomatous inflammation, weight loss, abdominal masses
Rotavirus - kits, high morbidity and mortality
Distemper
Inflammatory Bowel Disease - lymphoplasmocytic infiltration, ± vomiting, ultrasound and biopsy, diet, prednisolone, azathioprine
Neoplasia
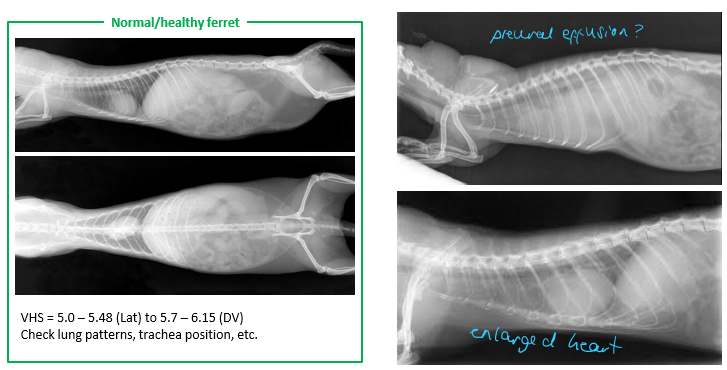
Cardiac Disease in Ferrets
Common - DCM, HCM, aortic valve regurgitation, myocarditis, neoplasia, heartworm
Ferrets <3yo
Clinical Signs - lethargy, exercise intolerance, weight loss, coughing, dyspnoea, ascites, organ enlargement, heart murmur, muffled heart sounds, arrhythmias, hind limb weakness (not related to thromboembolism), pulse deficits, hypothermia, HR180-250bpm, sinus arrhythmia
Emergency Management - O2 supplementation, sedation, furosemide, draining
Diagnosis - bloods, urinalysis, radiography, ECG, echo, heartworm testing, cardiac troponin I
Treatment - Furosemide, ACEi (Benzapril), Pimobendam, Spironolactone, Dilitiazem, Atenolol, pacemakers
Common Health Problems in Hedgehogs
Skin disease – alopecia/loss of spines, external parasites, ringworm, wounds, neoplasia
Oral and dental disease - weight loss, anorexia, excessive salivation, blood/pus discharge, tartar, periodontal disease, oral neoplasia e.g. SCC
Heart disease
Neoplasia
Wobbly Hedgehog Syndrome - demyelinating paralysis, ataxia, seizures, euthanasia
Enteritis and diarrhoea
Trauma - bites, RTAs, fractures
Orphaned hoglets
Malnourishment - wild hedgehogs in autumn/winter
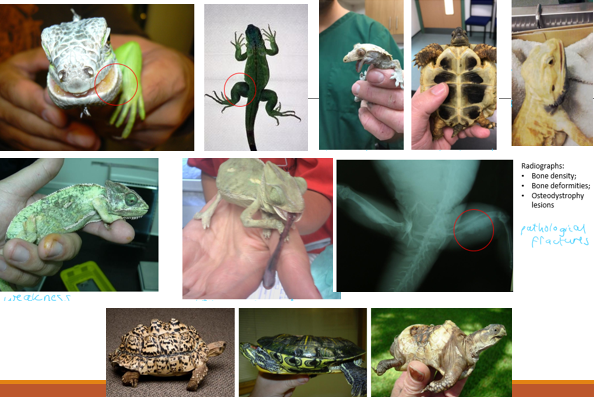
Metabolic Bone Disease in Reptiles
Due to - inadequate UV-B exposure, calcium deficiency, vitamin D3 deficiency, other conditions (e.g. CKD) affecting calcium metabolism
More common in young growing individuals, herbivore species
Clinical Signs - fibrous osteodystrophy lesions (swelling, lost calcium density), weakness, tongue paralysis, pliable jaw, soft shell, muscle tremors, seizures, abnormal shell shape, pathological fractures
Diagnosis - radiographs, biochemistry (Ca, P, renal function)
Treatment - vitamin D3, calcium gluconate, calcitonin, review husandary and diet
Hypovitaminosis A in Reptiles
Squamous metaplasia of different epitheliums
Terrapins and aquatic turtles, unbalanced diet
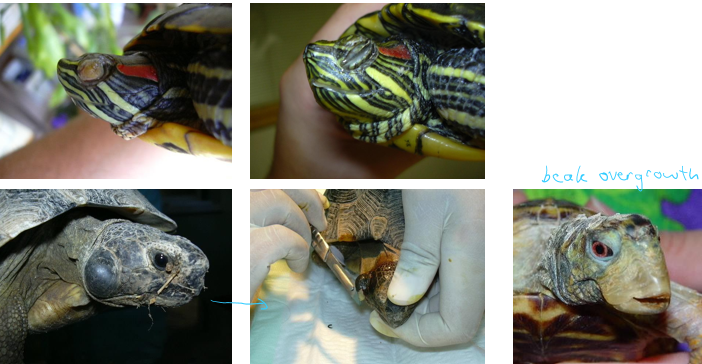
Clinical Signs - blepharitis, keratoconjunctivitis, overgrown nails and beak (chelonians), stomatitis, rhinitis, aural abscesses, retained shed
Treatment - vitamin A, surgical removal of conjunctival debris and aural abscesses, antibiotic eyedrops if eye lesions, review husbandry and diet