Chronic Kidney Disease
1/15
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
16 Terms
is CKD reversible? how is it defined and followed?
CKD is a clinical syndrome arising from irreversible progressive kidney injury evolving over the course of months to years
- syndrome: group of assoc signs and symptoms
- irreversible: process causes scarring in the kidney
- months to years: strict criteria is 3 months
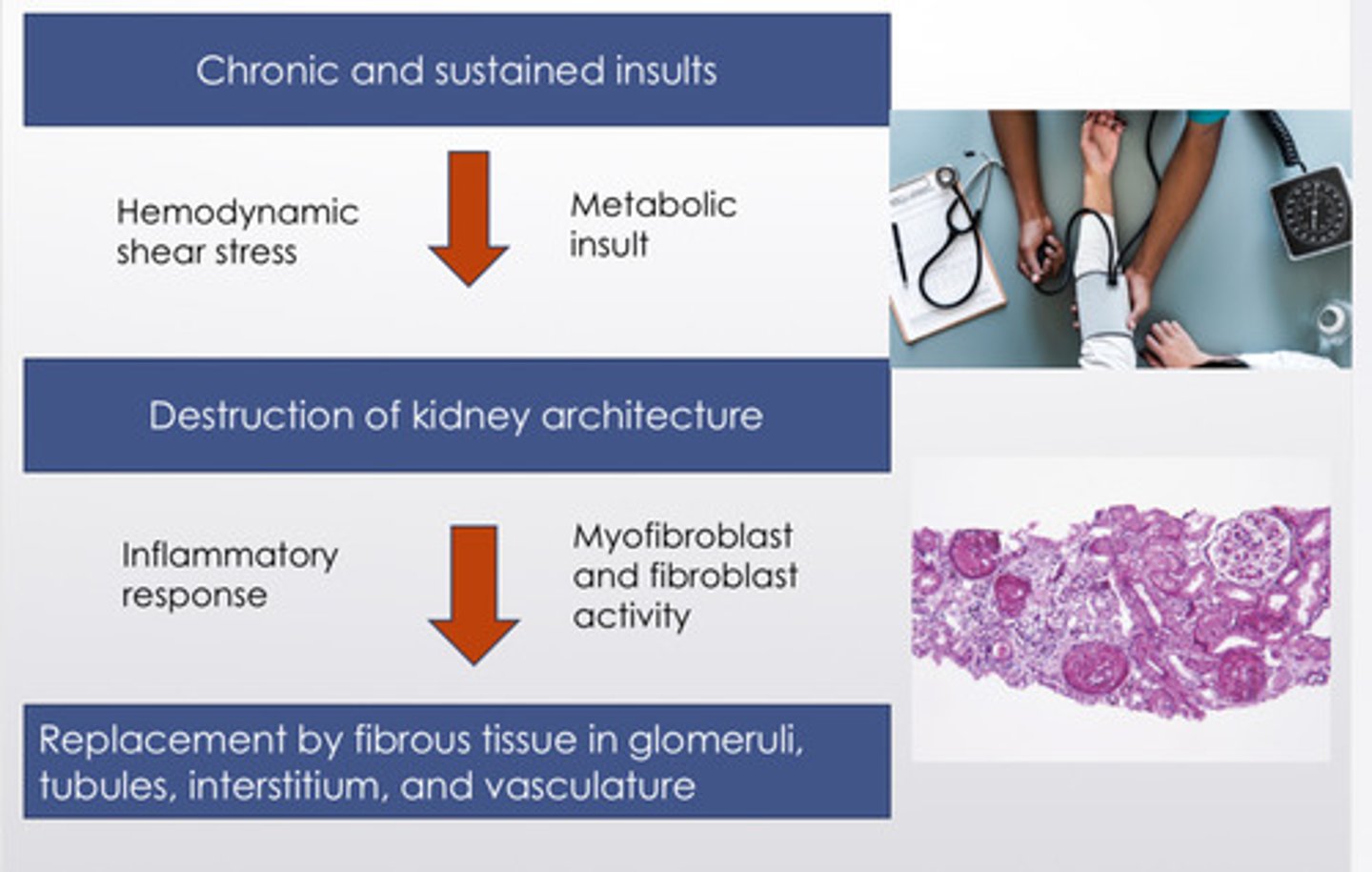
describe the pathway of chronic kidney damage (3)
chronic and sustained insults (hemodynamic shear stress, metabolic insults) ->
destruction of kidney architecture (inflammatory response, myofibroblast and fibroblast activity) ->
replacement by fibrous tissue in glomeruli, tubules, interstitium, and vasculature
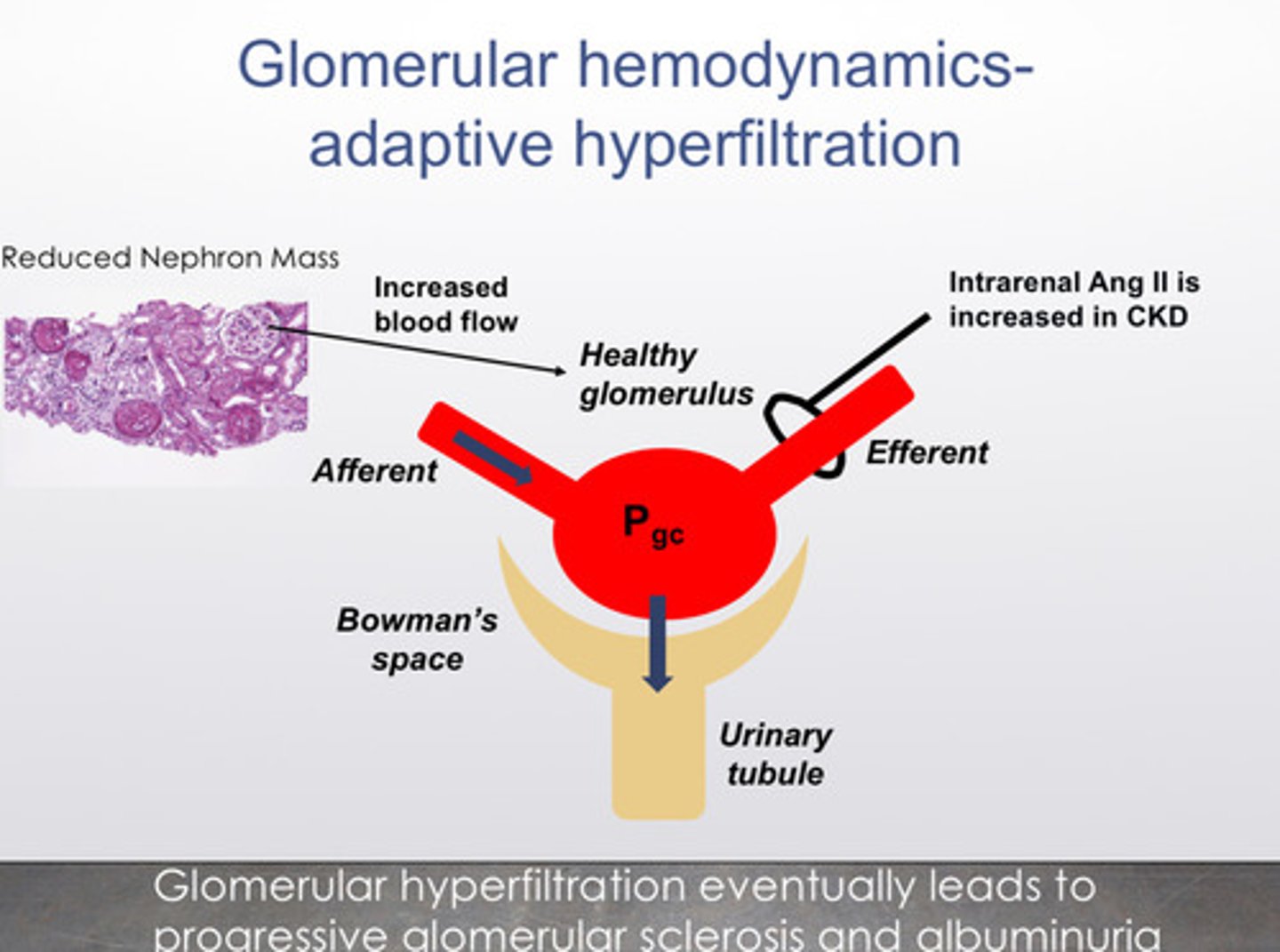
why does the damage progress over time?
1) this process continues even once the insults are well-controlled
2) fewer nephrons means that the remaining healthy nephrons see more blood flow, which increases glomerular capillary pressure
3) in CKD, intra-renal ang-II production increases —> hyperfiltration preserves GFR but lead to increased glomerular pressure and glomerulosclerosis
the bottom line: glomerular hyperfiltration eventually leads to progressive glomerular sclerosis and albuminuria
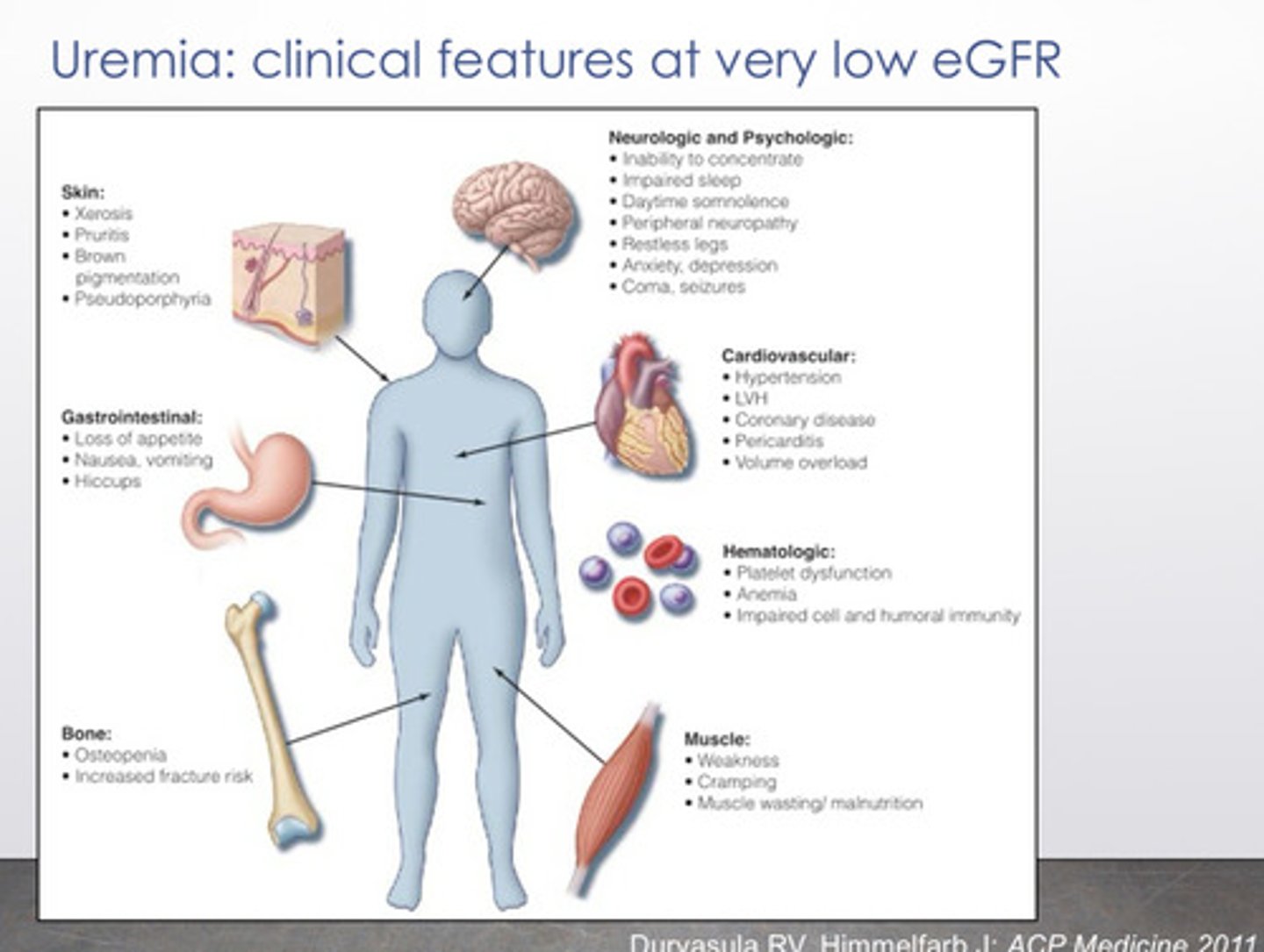
what are some signs and symptoms of people with severe CKD
1) skin: xerosis, pruritis, brown pigmentation
2) GI: loss of appetite, nausea, vomiting, hiccups
3) bone: osteopenia, increased fracture risk
4) neurologic/psychologic: inability to concentrate, impaired sleep, daytime somnolence, restless legs, anxiety, depression, coma
5) CV: hypertension, LVH, coronary disease
6) hematologic: platelet dysfunction, anemia, impaired cell and humoral immunity
7) muscle: weakness, cramping, muscle wasting/malnutrition
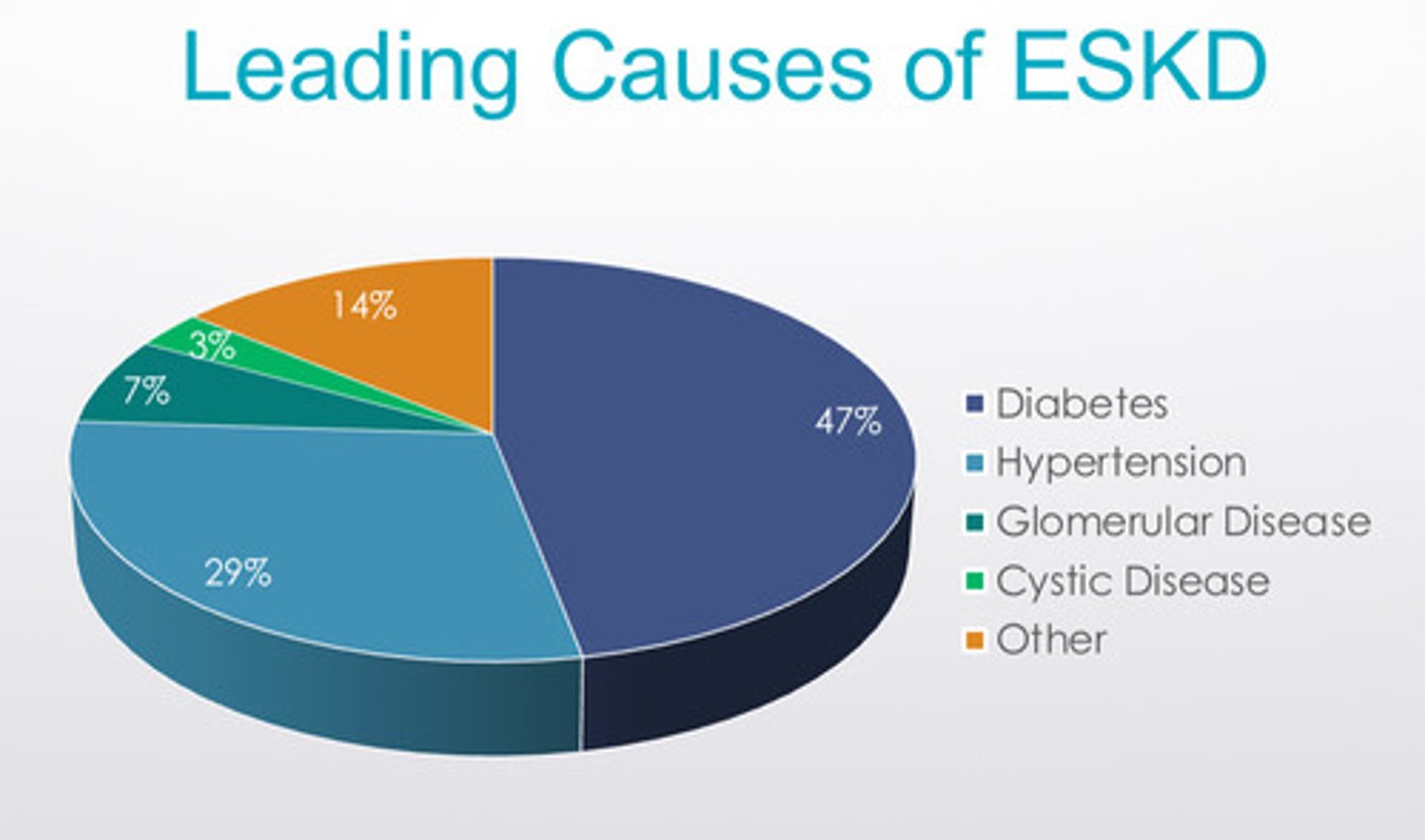
what are the 2 leading causes of CKD
1) diabetes
2) hypertension
some diseases can vary in their prognosis depending on _______ __________ that were useful to protect for some different disease
genetic mutations
what is albuminuria (aka proteinuria)
The presence of albumin in the urine.
under healthy conditions, the kidneys filter waste while remaining important proteins like albumin (mostly bc they are too large to cross the filtration barrier) in the bloodstream
why does albuminuria mark for kidney disease?
albuminuria means that the glomeruli are damaged, allowing the albumin to leak into the urine. the more albumin that appears in the urine, the more severe the kidney damage is likely to be
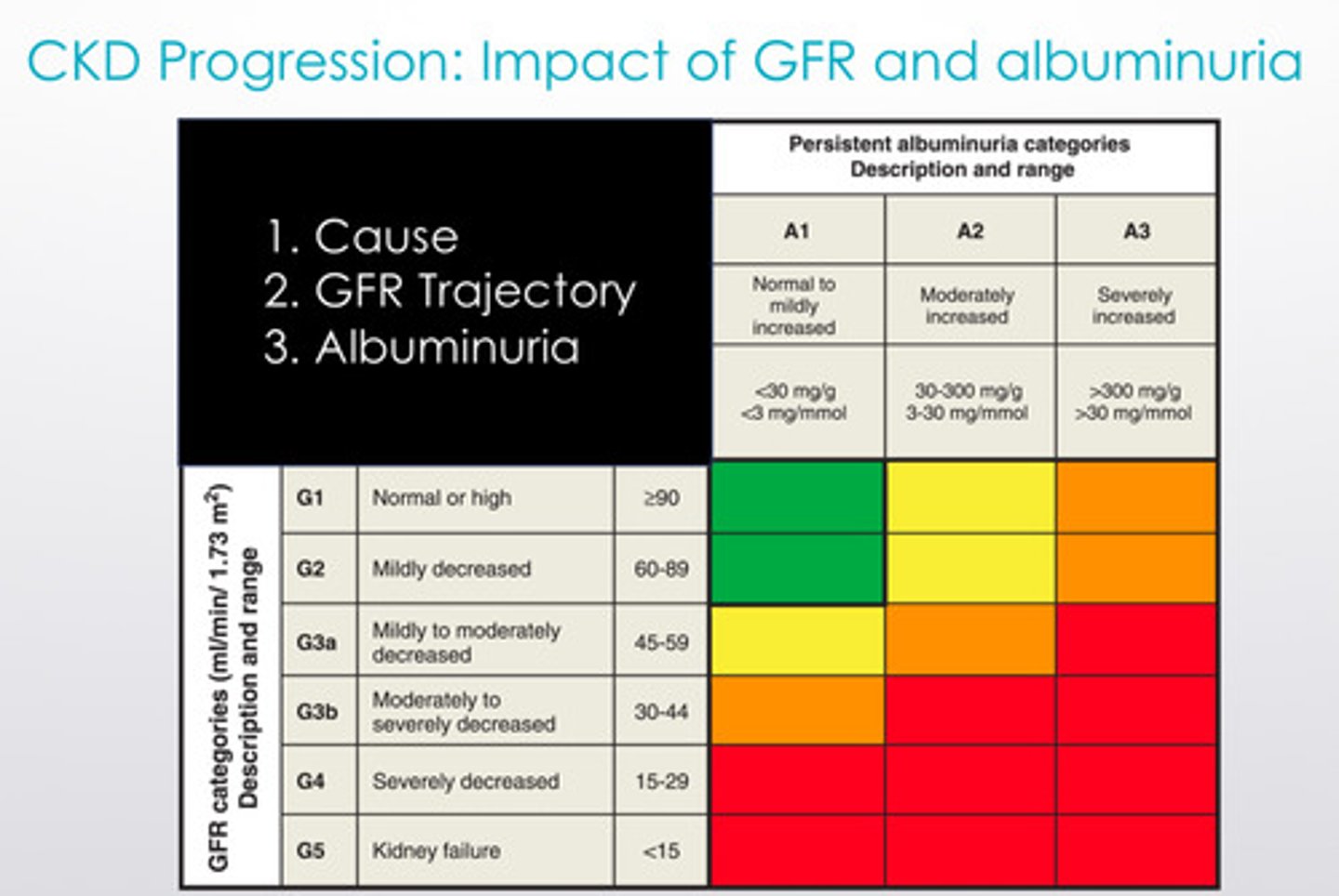
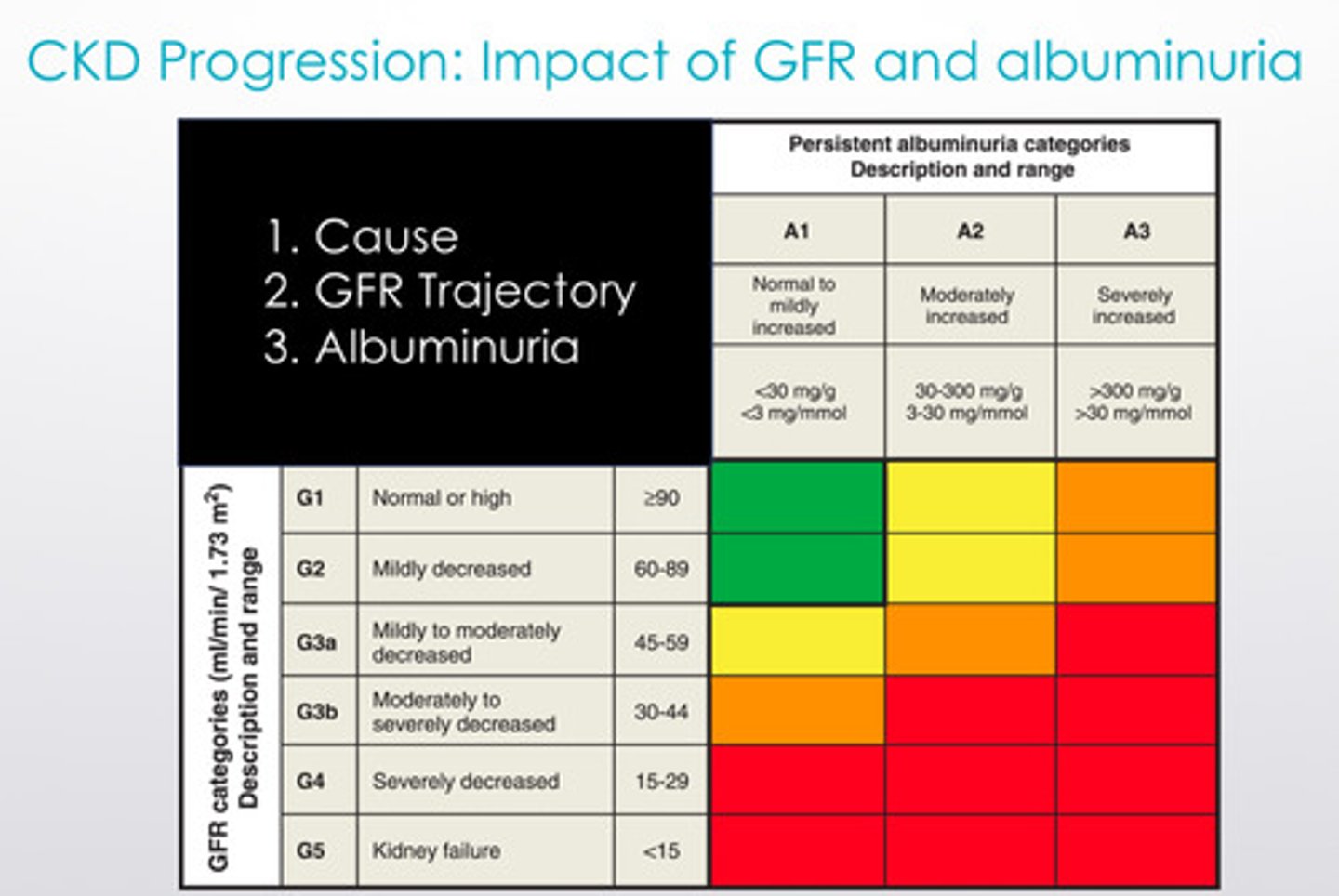
CKD progression is associated with the impact of what 2 things
1) decreasing GFR
2) increasing albuminuria
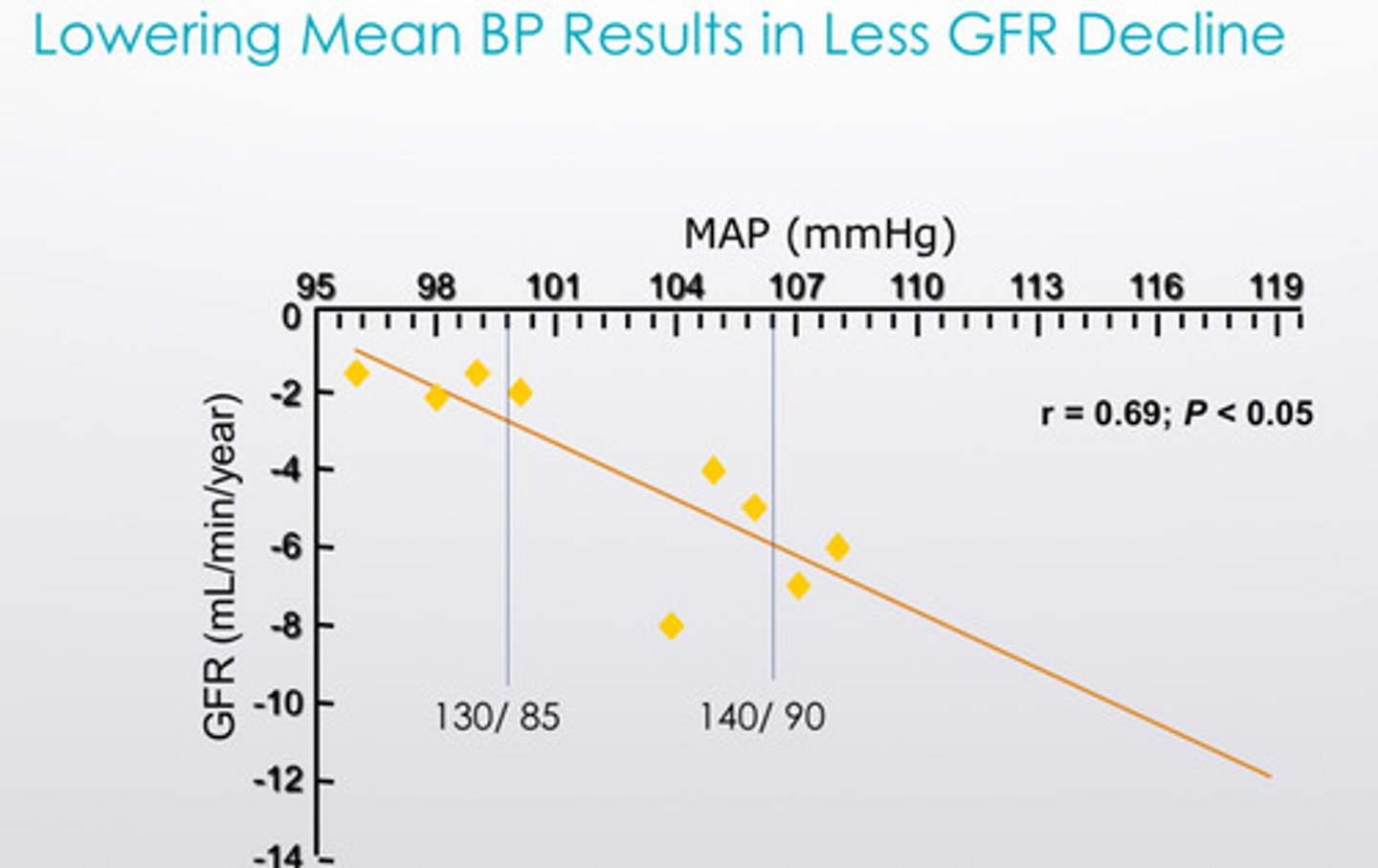
what is a tx strategy for slowing the progression of CKD?
lowering mean BP results in less GFR decline!
what are the medication categories that work best for this?
1) ang-II antagonists are first line therapy in management of HTN in proteinuric CKD (ACEI or ARBs can help prevent hyperfiltration)
2) SGLT2 inhibitors are also helpful in slowing the progression of proteinuric CKD to ESKD (end stage kidney disease)
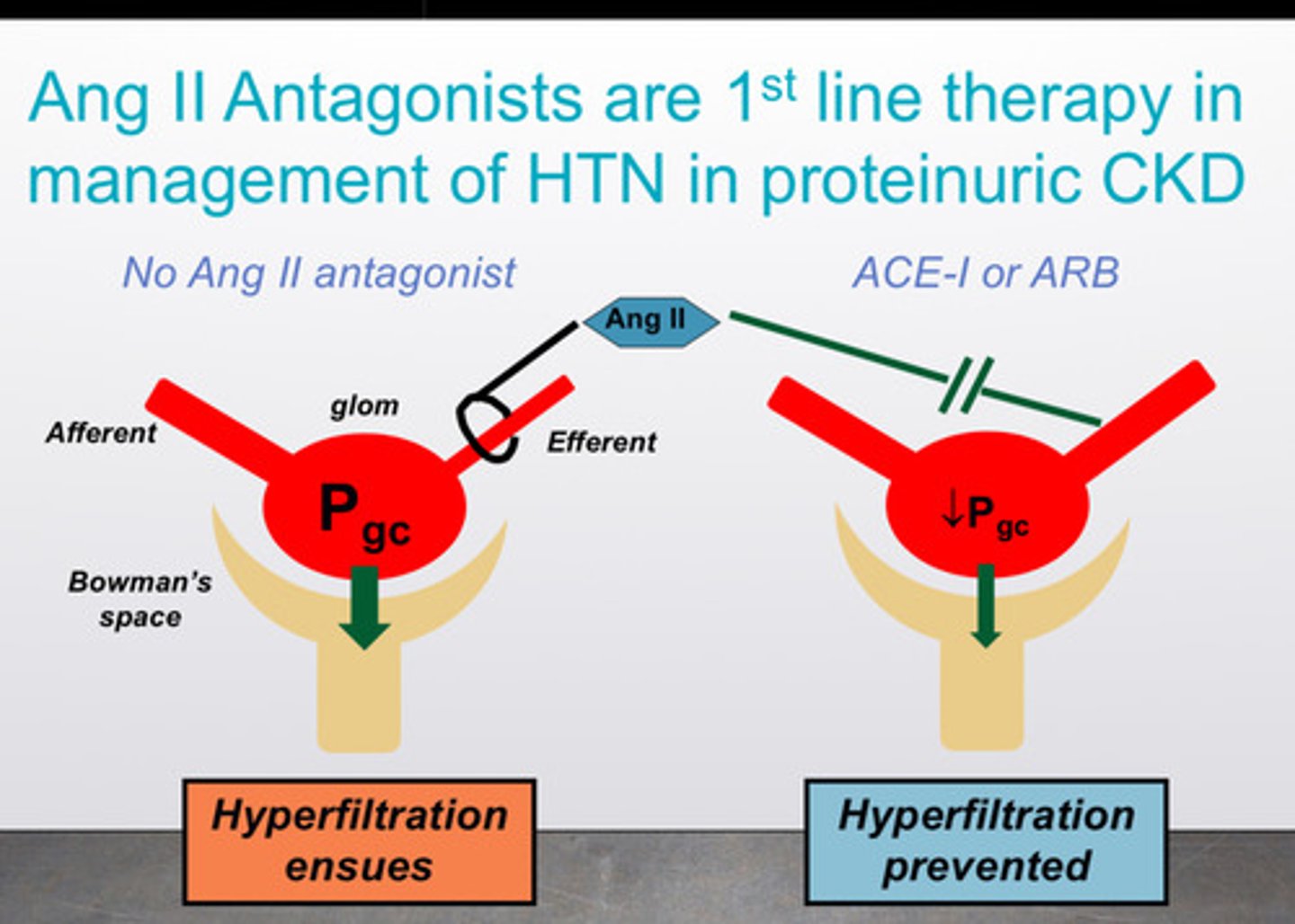
image of SGLT2 inhibitor action to slow progression of CKD

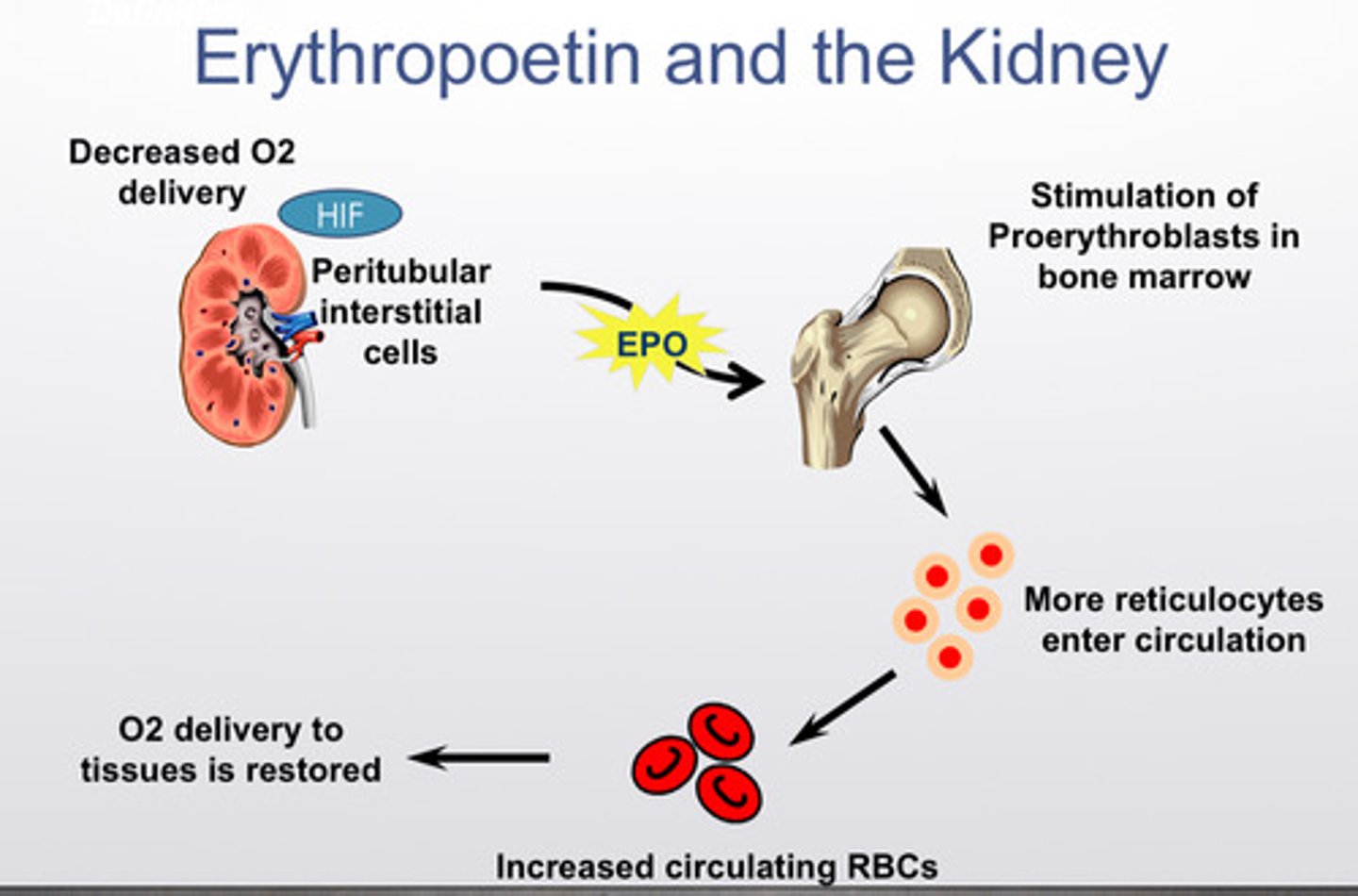
what are some treatments for the complications of CKD: anemia
tx is erythropoiesis stimulating agents, basically synthetic erythropoietin
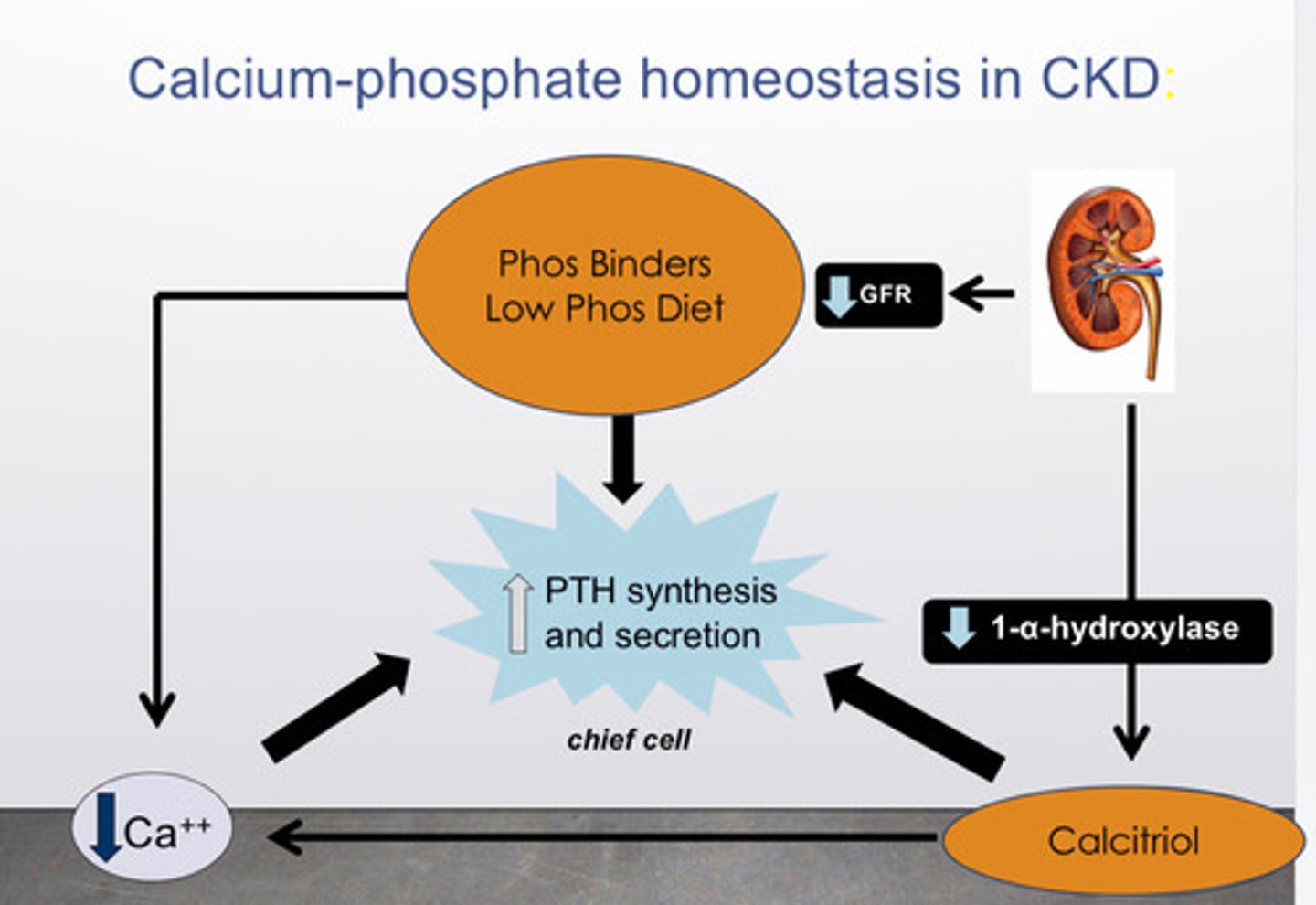
what are some treatments for the complications of CKD: high PTH
1) phosphate control via dietary phosphate restriction (avoiding foods high in phosphorus like dairy, nuts and phosphate binders
2) vitamin D supplementation with active vitamin D analogs (ex: calcitriol) to suppress PTH
what are some treatments for the complications of CKD: low VitD3 (cholecalciferol)
supplement with nutritional vitamin D
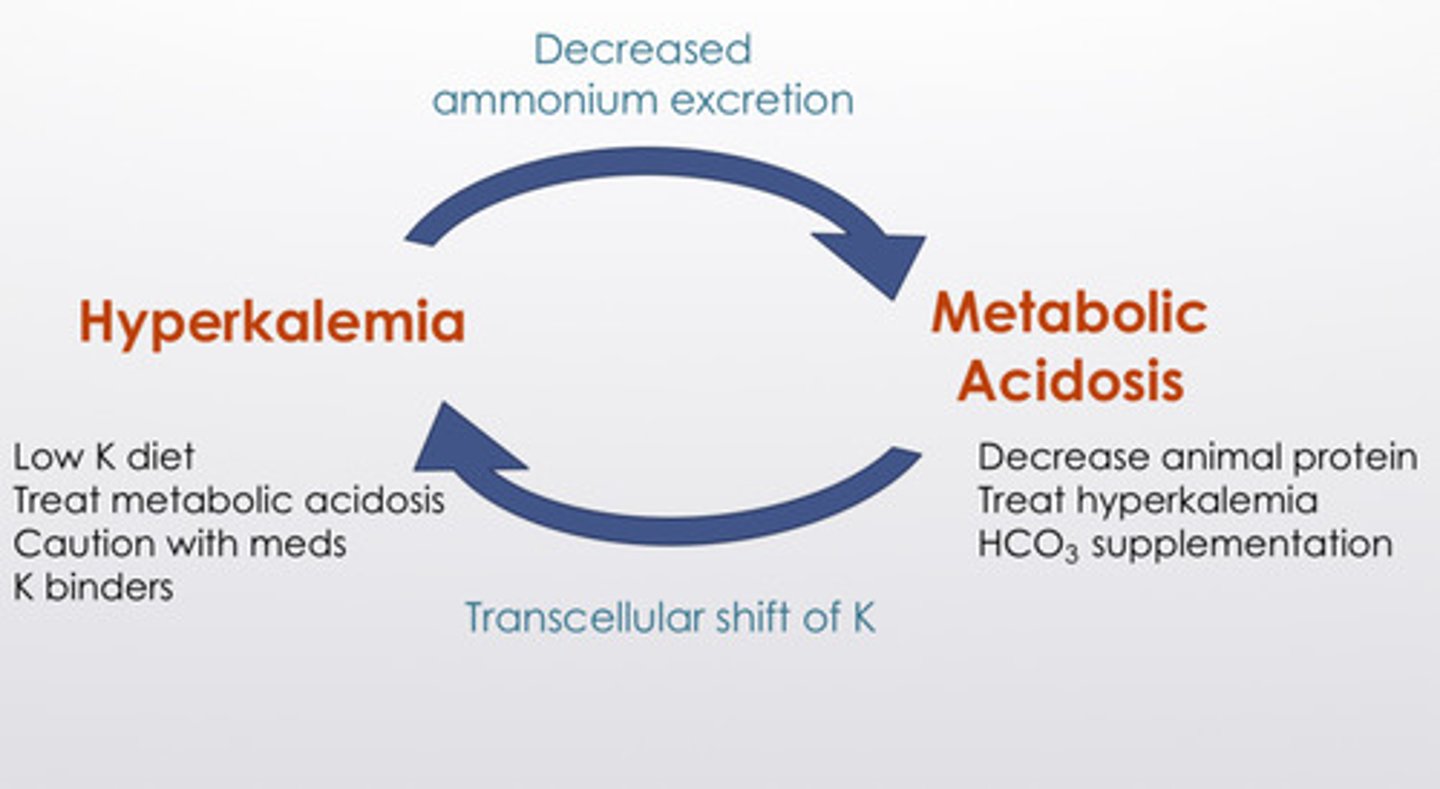
what are some treatments for the complications of CKD: hyperkalemia and metabolic acidosis
hyperkalemia: low K diet, treat metabolic acidosis, caution with medications, K binders
metabolic acidosis: decrease animal protein, treat hyperkalemia, HCO3 supplementation