Biological Basis for Understanding Psychotropic Drugs (Chapters 3, 4, & 5)
1/94
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
95 Terms
What are some things that could interact and produce a psychiatric disorder? No matter the cause, what happens to the brain?
Genetics
Neurodevelopment factors
Substances
Infections
Traumatic experiences
All interact and can produce a psychiatric disorder. No matter the cause, physical changes in the brain can result in disturbances in the patient’s mood and behavior
What are some of the responsibilities of the brain?
Maintenance of homeostasis
Regulation of the autonomic nervous system and hormones
Control of biological drives and behavior
Cycle of sleep and wakefulness
Circadian rhythms
Conscious mental activity
Memory
Social skills
Describe how the brain is responsible for the maintenance of homeostasis
The brain directs and coordinates the body’s response to internal and external changes
Various sensory organs relay information about the external world to the brain by peripheral nerves (sensations can be altered in psychotic disorders)
The brain controls skeletal muscles to respond to the external world; including the ability to initiate the contraction of muscles (including the diaphragm)
The brain also monitors internal functions
Receives information about blood pressure, body temperature, blood gases, and chemical composition of body fluids
Describe how the brain regulates the autonomic nervous system and hormones.
The autonomic nervous system and the endocrine system serve as links between the brain and cardiac muscle, smooth muscle, and glands of which the internal organs are composed
The brain influences internal organs by regulating hormonal secretions of the pituitary gland (master gland) which in turn regulates other glands
The hypothalamus secretes hormones called releasing factors which act on the pituitary gland to inhibit or stimulate the synthesis and release of pituitary hormones
Describe the hypothalamic pituitary adrenal axis (HPA axis).
Hypothalamus secretes corticotropin-releasing hormone (CRH)
CRH stimulates the pituitary gland to release adrenocorticotropic hormone
Adrenocorticotropin stimulates the cortex of each adrenal gland (located on top of the kidneys) to secrete the stress hormone cortisol
This is done in response to a variety of mental and physical stressors
How does the brain control biological drives and behavior?
Responsible for basic drives such as sex and hunger
Disturbances of these drives can be an indication of underlying psychiatric disorders such as depression
How does the brain control the cycle of sleep and wakefulness?
Various regions of the brain regulate and coordinate the entire cycle of sleep and wakefulness
Sleep pattern disturbances can occur in every psychiatric disorder
Psychotropic medications may interfere with the normal regulation of sleep and alertness (can cause drowsiness)
What is the circadian rhythm?
Fluctuation of various physiological and behavioral patterns over a 24-hour cycle, which influences:
Changes in sleep
Body temperature
Secretion of hormones such as corticotropin and cortisol
Secretion of neurotransmitters such as norepinephrine and serotonin
How does the brain control conscious mental activity?
All aspects of conscious mental experience and sense of self orientate in the activity of the brain
Conscious activity can be stream of consciousness, or can be more complex when applied to problem solving or interpretation
Can be distorted in psychiatric disorders
How does the brain influence memory?
Memory is the ability to retain and recall past experiences
When is the most common time for men and women to have a psychotic break?
Men: 18-25
Women: 26-32
Describe the composition of the brain and the three main functions:
Composed of 100 billion neurons
Neurons are nerve cells that conduct electrical impulses
3 main types of physiological actions:
Responding to stimuli
Conducting electrical impulses
Releasing chemicals called neurotransmitters
What is a neurotransmitter? What process are they apart of?
A chemical substance that functions as a neuro-messanger
Released from the axon terminal of the presynaptic neuron on excitation, then crosses the space (synapse) to the adjacent postsynaptic neuron where it attaches to receptors on the neuron surface
→ This interaction allows the activity of one neuron to influence the activity of other neurons (THIS IS WHAT MEDS TRY TO TARGET!)
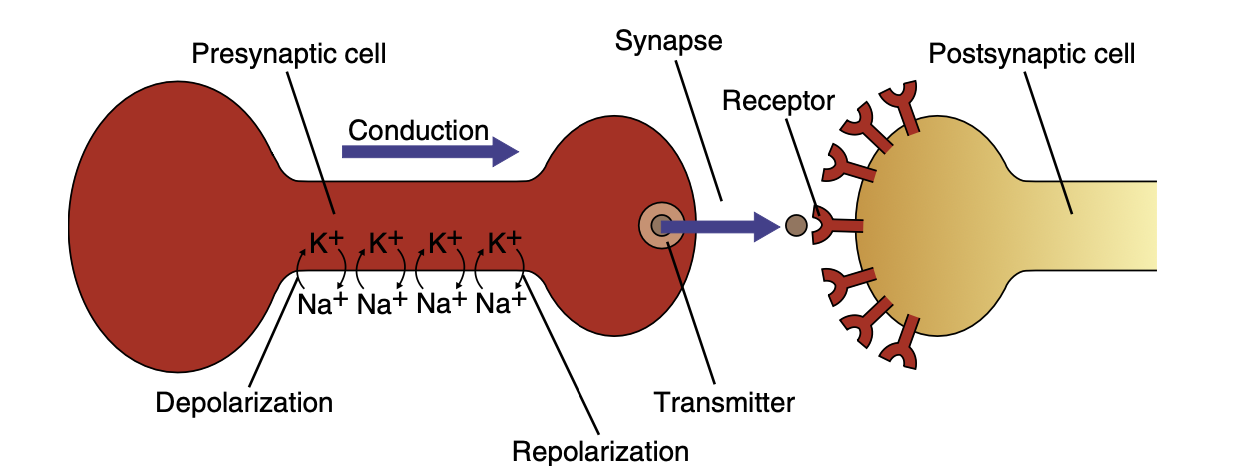
What happens after the neurotransmitter attatches to a receptor and exerts its influence on postsynaptic cells? What are the 2 ways that this happens?
Neurotransmitter is destroyed in one of 2 ways:
Enzymes: break down the neurotransmitter
Reuptake: taken back into the presynaptic cell from which they were originally released
Describe sodium and potassium in relation to neurons
Inward flow of sodium
Outward flow of potassium
What are the 3 main properties of neurotransmitters?
The chemical must be found in the pre-synaptic vesicles and must be released when the neuron is stimulated
The chemical must be inactivated after release (the most common mechanism of action is the re-uptake of the chemical by the pre-synaptic membrane, or the second being destruction by an extracellular enzyme)
If the chemical is applied exogenously (through medication) at the post-synaptic membrane, the effect will be the same as when the pre-synaptic neuron is stimulated
Describe the cholinergic neurotransmitter acetylcholine
Found in the cerebral cortex, hippocampus, limbic structures, and basal ganglia
More widespread in peripheral NS than CNS
Involved in sleep, arousal, pain perception, movement and memory
Decrease in acetylcholine can cause what diseases?
Alzheimers (decrease in acetylcholine-secreting neurons)
Huntington’s disease
Parkinson’s
Myasthenia Gravis (decrease in acetylcholine receptors)
What enzyme eats away at acetylcholine?
Acetylcholinesterase
Axons normally have slippery outer part, but this is destroyed by the enzyme
Causes the neurons to stick together and get all twisted up
Body forgets how to do things because signals aren’t fully sending
Describe the monoamine neurotransmitter norepinephrine
Found in the thalamus, hypothalamys, limbic system, hippocampus, cerebellum and cerebral cortex
Influences mood, cognitiion, perception, locomotion, sleep, arousal, cardiovascualr functioning
Plays a role in anxiety disorders
Antidepressants block the reuprake of norepinphring into the pre-synaptic cell or inhibit monoamine oxidase from metabolizing it
What disorders are associated with a decrease in norepinephrine?
Depression
What disorders are associated with an increase in norepinephrine?
Mania
Anxiety states
Schizophrenia
Describe the monoamine neurotransmitter dopamine
Found in the frontal cortex, limbic system, basal ganglia, thalamus, posterior pituitary and spinal cord
Involved in the control of complex movements, motivation, cognition, and regulating emotional responses
Many drugs of abuse (cocaine, amphetamine) cause dopamine release, suggesting a role in what makes things pleasurable *inside the brain, there is a development of more receptors that NEED to be filled = make it hard to come off of them)
Disorders associated with decreased dopamine
Parkinson’s disease
Depression
Disorders associated with increased dopamine
Schizophrenia
Mania
Describe the amine neurotransmitter serotonin (5-HT)
Found in the hypothalamus, thalamus, limbic system, basal ganglia, cerebral cortex, cerebellum, and spinal cord
Influences sleep and arousal, libido, appetite, mood, aggression, pain perception, coordination, and judgement
Plays a role in mood and probably delusions, hallycinations and withdeawl of schizophrenia
Involved in temperature regulation and pain control system
LSD acts as a serotonin receptor sites
Anitdepressants block its reuptake at the presynamtic cell
Disorders associated with decreased serotonin
Depression
Describe the amine neurotransmitter melatonin
Further synthesis of serotonin that is produced in the pineal gland
Induces pigment lightening effect on skin cells and regulates reproductive function in animals
Role in humans unclear
Implicated in the sleep-wake cycle and seasonal affective disorder
What is the most amount of melatonin that a person needs?
0.5 mg!!!!! That’s it!
Describe the neurotransmitter amino acid gamma-aminobutyric acid (GABA)
Found in the hypothalamus, hippocampus, cortex, basal ganglia, spinal cord and retina
A major transmitter for post-synaptic inhibition in the CNS
Involved in the slow down of body activity
Drugs that increase GABA, such as benzodiazepines, are used to treat anxiety and sleep
Diseases associated with decreased GABA
Anxiety
Schizophrenia
Mania
Hunington’’s disease
Describe the neurotransmitter amino acid glutamate
Found in all cells of the body and in the CNS where it si stored in synaptic vesicles and used as a neurotransmitter
Implicated in schizophrenia and may cause cell death in strokes and Hungington’s disease
Diseases that result from increase in glutamate
Psychosis
Diseases that result from decrease in glutamate
Prolonged increased neurotoxic
Neurodegeneration in Alzheimer’s disease
Improvement of cognitive performance in behavioral tasks! (which is good!)
Depression
Schizophrenia
PTSD
Describe the peptide neurotransmitters: endorphins and enkephalins
Distributed in the CNS
Their effect is generally inhibitory
The opiates morphine and heroin bind to endorphin and enkephalin receptors on pre-synaptic neurosn, blocking th erelease of neurotransmitters and thus reducing the pain
Describe the peptide neurotransmitter Substance P
Found in the spinal cord, brain, and sensory neurons associated with pain
Generally excitatory
Blocking the release of substance P by morphine, leads to a reduction in pain
Involved in the regulation of pain and possibly mood and anxiety
Describe the brainstem
Most primitive area of the brain
Connects directly to the spinal cord
Central to the survival of all animals by controlling heart rate, breathing, digestion, and sleeping
Ascending pathways that prokect to the cerebrum are known as the limbic system
What is the limbic system?
Plays a crucial role in the emotional status and psychological function using norepinephrine, serotonin, and dopamine as its neurotransmitters
Describe the hypothalamus and its function
Small area above the brainstem that plays a vital role in:
Controlling basic drives, such as hunger, thirst and sex
Linking higher activities (thought and emotion) to the functioning of internal organs
Processing sensory information that is then sent to the cerebral cortex
Regulating the sleep and wakefulness cycle and the ability of the cerebrum to carry out conscious mental activity
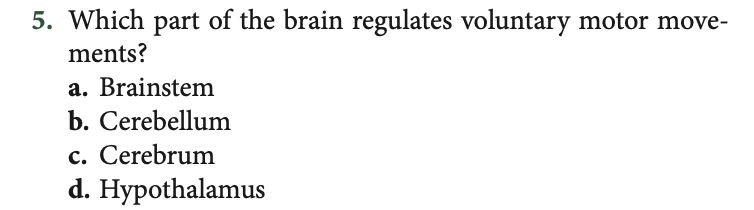
Describe the cerebellum and its function
Located behind the brainstem where the spinal cord meets the brain
Receives information from the sensory systems, the spinal cord, and other parts of the brain then regulates voluntary motor movements of skeletal muscles
Plays a crucial role in coordinating contractions so movement is smooth and directed
Involved in balance and equilibrium
Describe the cerebrum and its function s
On top of surrounding brainstem
Responsible for mental activities and a consious sense of being
Responsible for consious perception of the external world, our body, emotional status, memroy, and control of skeletal muscles
Responsbble for lanugage and communication
Surface of the cerebrum is the cerebral cortex, which has 4 major lobes
Consicous sesnsation and initiation of movemnt = frontal lobe
Sensation of touch = parietla lobe
Sounds = temporallobe
Vision = occipital lobe
What are the pockets of gray matter deep within the cerebrum?
Basal ganglia: involved in movement regulation
Amygdala and hippocampus (part of limbic system): involved in emotions, learning, memory, and basic drives
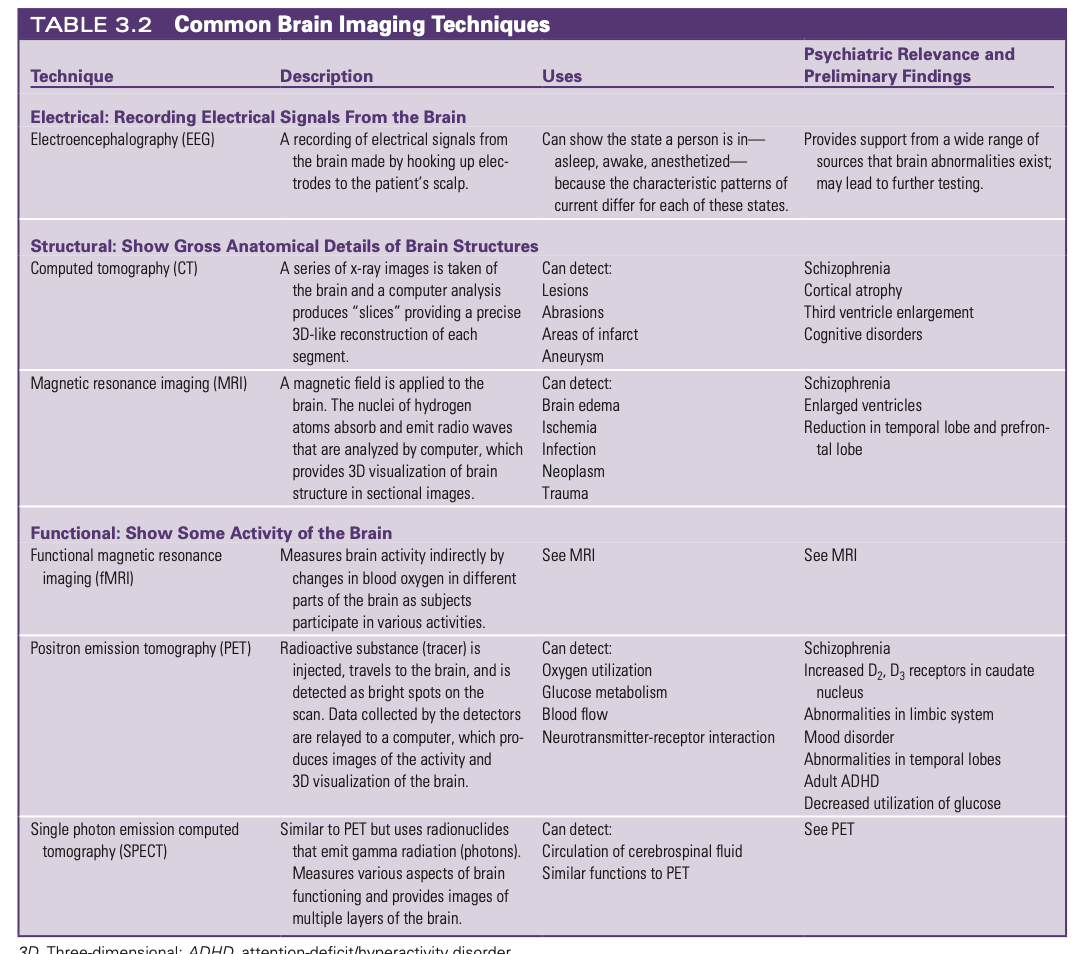
How can we visualize the brain?
Structured imaging techniques
Computed tomography (CT)
Magnetic resonance imaging (MRI)
Functional imaging techniques
Positron emission tomography (PET)
Single photon emission computer tomography (SPECT)
What does pharmacodynamics refer to?
Biological and physiological effects of the drug on the body
Drug action
Responses
*Dose related!
What does pharmacokinetics refer to?
Movement of a drug through the body (actions of the body on the drug!) ADME
Absorption
Distribution (how it’s distributed through the body)
Metabolism (liver transformation)
Excretion (kidney excretion)
*Also includes the half-life and dosing of medications
Benzodiazepines
Anti-anxiety and hypnotic medications
GABA is the major inhibitory (calming) neurotransmitter in the CNS
Benzos promote the activity if GABA
Possess anti-anxiety, hypnotic (sleep inducing, anticonvulsant, amnestic (loss of memory) and muscle relaxant properties
5 examples of Benzodiazepines
“-PAM”
Diazepam (Valium)
Clonazepam (Klonopin)
Alprazolam (Xanax)
Loreazepam (Ativa)
Temazepam (Restoril) - helps with sleep!
What is important to remember about benzodiazepines?
High risk for addiction
Short term use only to calm down
Do not use for more than 2 weeks
Side effects of benzodiazepines
Sedation
Ataxia
Anterograde amnesia
If combined with other CNS depressants, can cause respiratory depression and death
Z-Hypnotics
Short-Acting Sedative-Hypnotic Sleep Agents
Selectivity for GABA receptors
Possess hypnptic and amnestic effects without the antianxiety, anticonvulsant, or muscle relaxant effects of benzodiazepines
Examples of Z-hypnotics
Zolpidem (Ambien)
Zalepon (Sonata)
Eszopiclone (Lunesta)
What is important to remember about Z-hypnoics?
Controlled substances but less tolerance and dependence than benzodiazepines
Short half lives and no active metabolites compared to benzodiazepines
Start dosage low then slowly increase for best effect
Side effects of z-hypnotics
Bitter taste upon awakening
Complex sleep-related behaviors (sleepwalking, driving, cooking, etc)
CNS depressant use can increase side effects
Melatonin receptor agonists
Anti-anxiety and Hypnotic drugs (relax and sleep)
Melatonin is a naturally excreted hormone by the pineal gland at night as part of the normal circadian rhythm
Examples of melatonin receptor agonists
Ramelteon (Rozerem) is a melatonin receptor agonist and acts similar to endogenous melatonin
Buspirone
Treatment of generalized anxiey disorder
Side effects: dizziness, headache, nausea
Buspirone (BuSpar): people want fast results, but takes 2-3 weeks for it to work; people won’t get addicted!
Best anti-anxiety med because the least amount of side effects
Doxepin
Doxepin (Silenor) is the low dose formulation of a tricyclic antidepressant (TCA)
Approved for insomnia characterized by difficulty falling alssep
DO NOT TAKE IF ON A MONOAMINE OXIDASE INHIBITOR
Orexin Receptor Antagonists
Orexins (neuropeptide procied in the hypothalamis) promote wakefulness
Suvorexant (Belsomra) and Lemborexant (Daybigo) are orexin receptor antagonists
Used for insomnia
CONTRAINDICATEDIN NARCLEPSY
Controlled substance
What are the irst line drugs for longterm treatment of anxiety and depression disorders
Antidepressant medications, NOT benzodiazepines (these should be short term only)
How do SSRIs work?
Selective Serotonin Reuptake Inhibitors
Block the reuptake of serotonin by makign the meurotransmitter availabel in synapse
Examples:
Fluoxetine (Prozac) - people will take this for a long time, then it will stop working
Sertaline (Zoloft)
Paroxetine (Paxil)
Citlopram (Celexa)
Escitlopram (Lexapro)
Fluvoxamne (Luvox)
BOLDED MEDS ARE BEST ONES! BUT MOST EXPENSIVE
First line medications for treatment of major depressive disorder and anxiety disorders
Common side effects: nausea, restlessness, jitterieness, sleep disturbances, sexual dysfinction
What are the most common side effect of psychotropic medications:
Nausea
Vomiting
Weight gain
Low libido
Dizziness
Constipation
Blurred vision
Norepinephrine and Serotonin Specific Antidepressants
Mirtaxapine (Remeron)
Engnaces norepinpehrine and serotonin neurotransmission
Side effects: sedation, appetite stimulation, weight gain
Commonly given for insomnia
Serotonin-norepinephrine reuptake inhibitors
Increase both serotonin and norepinephirine in the synapse by reuptake
Venlafaxine (Effexor)
Desvenlafaxine (Pristiq)
Duloxetine (Cymbalata)
Levomilnacipran (Fetzima)
Treatment of major depssive disorder and anxiety disorders
More likely to ause sweating
Dose depednet increased in BP and hR due to norepinephine reuptake blockade - MONITOR BP AND HR!!!
Pain reduction
Monoamine Oxidase Inhibitors
Class of antidepressants that are rarely used today
Last-line agents
Phenelzine (Nardil)
Isocarboxazid (Marplan)
Tranylcypromine (Parnate)
Selegiline (Emsam)
Metabolized monoamines, including serotonin, norepinpehinr, and dopamine → Inhibit MAO, and increase synaptic levels of these neurotransmitters → antidepressant effects
What medications should be avoided if a patient is taking an MAOI?
SSRI & Busprione & Psychostimulants
Can lead to serotonin syndrome!!!!!!! Patient will become vasoconstrictive → HIGHER BLOOD PRESSURE BAD CAN DIE BC OF HYPETENSIVE CIRSIS
What food should someone taking an MAOI not consume?
Tyramine in protein-based foods: aged cheeses, pickled or smoked fish, wine ALL BAD!!!
What is the gold standard mood stabilizer for bipolar disorder?
Lithium
Narrow therapeutic index
Must monitor levels regularly
Dehydration, med interactions, decreased renal function can all increase lithium levels
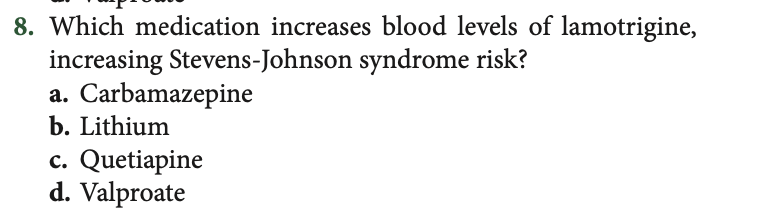
What are some anticonvulsant medications that are also mood stablizers?
Carbamazepine (Tegretol, Equetro): second line agent for manic or mized episodes
Lamotrigine (Lamictal): maintencance therapy for bippoalr disprder, used for bipolar depression
Valproate (Depakote): manic episodes with biplar disorder, useful for rapid cycling
Anticonvilsant properites derive from the lareration of electrical conductivity in menbranes
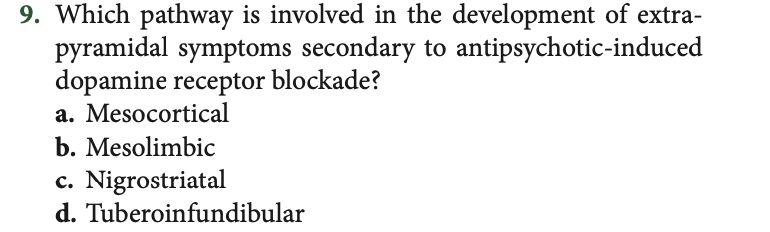
First generation antipsychotics
Strong antagonists (blocking agents)
Bind to D2 receptors
Block attatchement of dopamine
Reduce dopaminergic transmission
Agnists of receptors for:
Acetylcholine
Norepinephrine
Histamine
Second generation antipsychotics
Bind to dopamine receptors in the limbic system
Preferntially over dopamine receptors in neostrital areas of the basal ganglia
Decreased motor side effects
Target both the psotive nd negative symptoms of schizophrenia
Antangoisnts for serotninin and dpaine receeptors
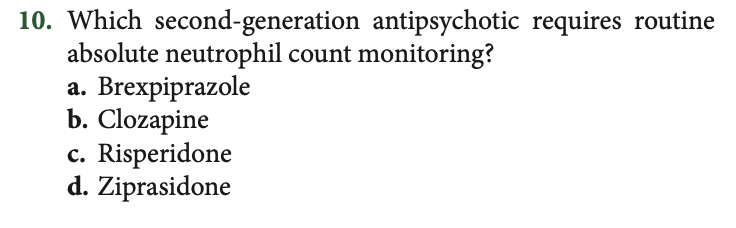
Common second-generation antipsychotic drugs
Clozapine (Clozaril)
Risperidone (Risperdal)
Olanzapine (Zyprexa)
Ziprasidone (Geodon)
Aripiprazole (Abilify) - MOST COMMON
Paliperidone (Invega)
Medication treatment for Alzheimer’s disease
Prevent or slow strucutral degeneration
Cholinestease inhibitors slwo the rate of memory loss
NMDA receptor agntagnonists
Examples:
Tacrine (Cognex)
Donepezil (Aricept)
Galantamaine (Razadyne)
Revastigmine (Exelon)
Memantine (Namenda)
Medication treatment for attention-deficit.hyperactivity disorder
Psychostimulants are first line treatment
Sympathomimetic amines that act by blocking the reuptake of norepinephrine and dopamine
Examples:
Methylphenidate (Ritalin)
Dextrosmphetamine (Adderall)
Atomoxetine hydrochloride (Strattera)
Major concerns of herbal medicine
Potential long-term effects
Nerve damage
Kidney damage
Liver damage
Possibility of adverse chemical reactions with other substances and conventional medications
CORRECT ANSWER: C
CORRECT ANSWER: A
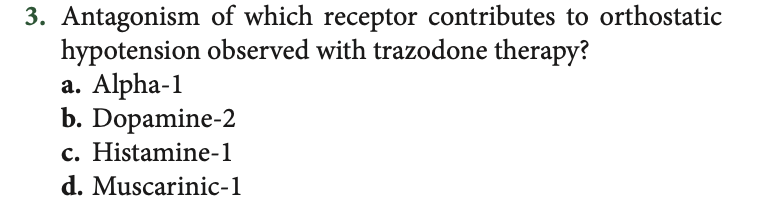
CORRECT ANSWER: A
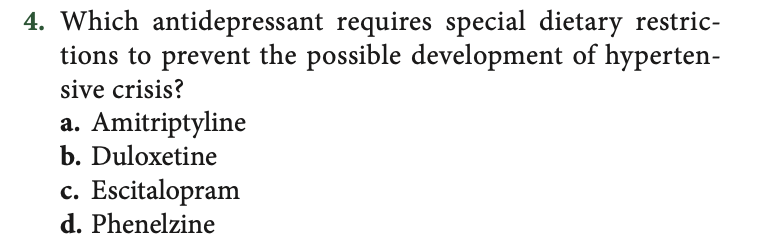
CORRECT ANSWER: D
CORRECT ANSWER: B
CORRECT ANSWER: A
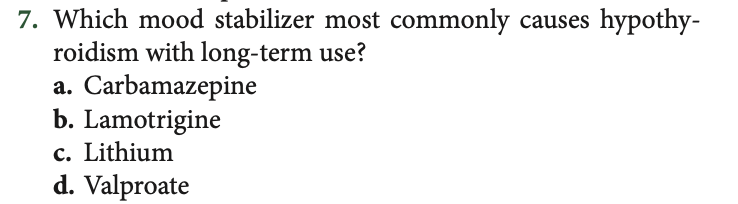
CORRECT ANSWER: C
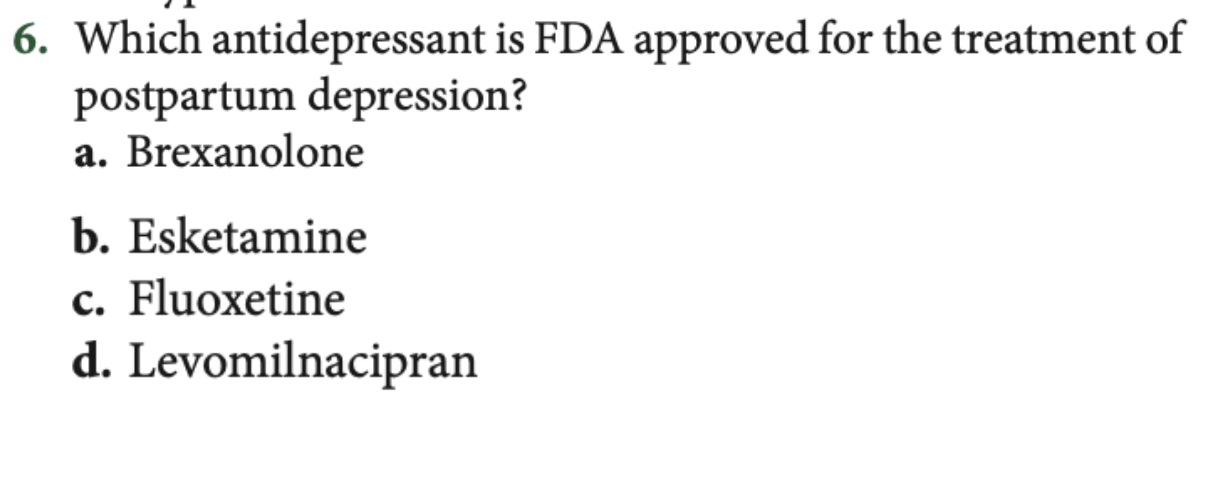
CORRECT ANSWER: D
CORRECT ANSWER: C
CORRECT ANSWER: B
Name and describe six functions of the brain
Circadian rhythm: regulating sleep and wake cycle
Motor functioning: regulate skeletal muscle coordination and contraction
Vital functioning: heart rate, respirations, blood pressure
Emotions, learning, memory
Basic drives and regulates hormones
Cognitive functioning
What is a neurotransmitter?
A chemical substance that functions as a neuromessenger, interacts with other neurons to release chemicals and conduct electrical impulses, and respond to stimuli.
How does the neurotransmitter dopamine affect mental illness?
Dopamine: Involved with the integration of emotions and thoughts. Involved in decision making.
Decrease → Parkinson’s and depression
Increase → mania and schizophrenia
How does the neurotransmitter serotonin affect mental illness?
Serotonin: Involved in sleep regulation, hunger, mood states, pain perception, aggression, and sexual behavior
Decrease → depression
Increase → serotonin syndrome
Give two examples of SSRIs. When are they used? What are some of the side effects?
Lexapro: used to treat depression and generalized anxiety
Side effects: GI upset, weight gain, decreased libido, constipation
Zoloft: used to treat depression and generalized anxiety
Side effects: dry mouth, weight gain, decreased libido
Describe mood stabilizers.
Class of drugs used to treat symptoms associated with bipolar disorder.
What are two examples of mood stabilizers, and when are they used?
Lithium: for bipolar disorder
Seroquel: for mood stabilizer and anti-psychotic
Describe first and second-generation antipsychotics. What are their side effects?
First generation: decrease dopamine activity in CNS; reduce positive symptoms - have more side effects than second generation!
Second generation: dopamine and serotonin antagonists - reduces positive and negative symptoms - fewer and better-tolerated side effects!
A nurse administers a medication that potentiates the action of GABA. What effect would you expect?
a. reduced anxiety
b. improved memory
c. more organized thinking
d. fewer sensory perceptual alterations
Correct answer: A!!
GABA receptors = related to anxiety!!!
What is a possible side effect of Buspirone?
Dizziness
If psychotropic drug block muscarinic receptors, what will the patient complain of?
Dry mouth
Blurred vision
Urinary retention
Constipation
Tachycardia