Exam 6 chickens, swine, pigmy goat, beef
1/145
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
146 Terms
Nose ring application
used to control bulls
insert in bulls 9-12 months of age
standing position in a chute under local analgesia
use self-piercing, non-rusting metal ring
inserted through the nasal septum about one inch from the tip of the nose
should not be used as the sole form of restraint

indications for dehorning in cattle
prevent operator injury
prevent livestock injury
ease of working animals
less space required for housing and feeding
treatment of disease conditions
correction of behavioral problems associated with dominance
reduce carcass condemnation due to bruising associated with horn injuries
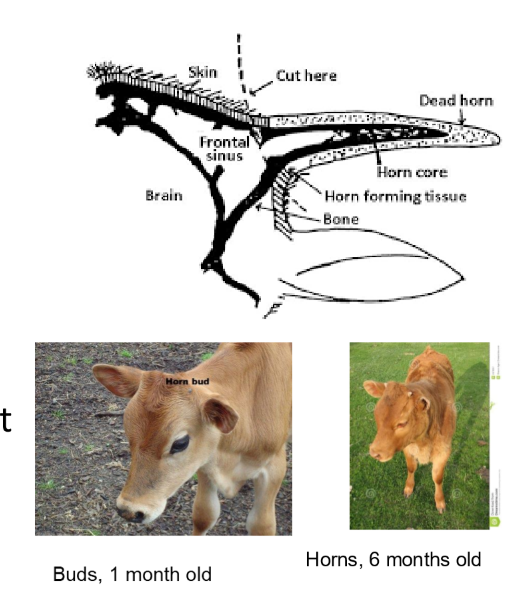
horn anatomy and growth
The horn grows from a modified skin epithelium (buds)
buds are not attached to the skull before 2 months of age
frontal sinus opens to the cavity of the horn at 4 months
restraint and analgesia with dehorning in cattle
head tray or similar restrait device
head tie to one side with halter
cornual nerve block (conrnual) branch of the lachrymal nerve) - 5ml of 2% lidociane using 20-22 g 0.5-1% needle
local infiltration around base of horn

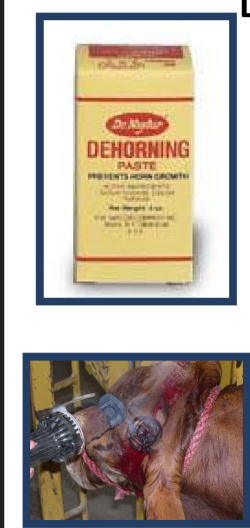
Disbudding in cattle
caustic paste / caustic chemical injection
pastes contain NaOH, KOH or CaOH
injectable contains CaCI
apply at <1 week of age
do not use in beef calves or in group housed calves cover the horn bud with duct tape
clip hair around horn bud, use gloves
post op NSAIDs
Electrothermal (hot iron)
butane-powered, rechargeable or corded
calves up to 2 moths old
hot iron must fit comfortably over horn bud
apply for 5-10 seconds, depending on the size of the calf
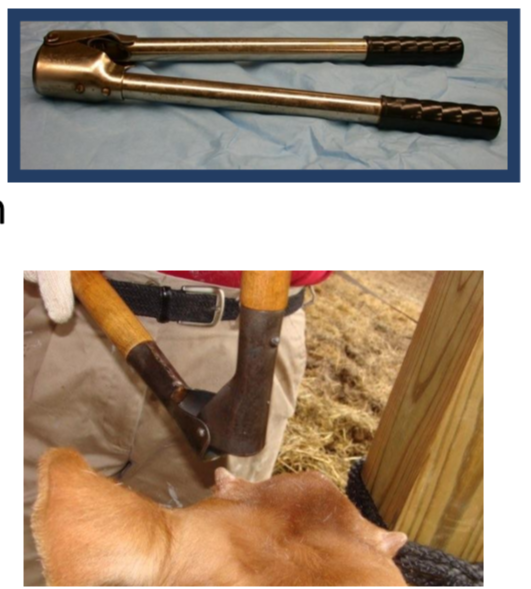
Barns dehorner
calves from 3 months to a year or more
remove 1-1.5 cm of skin at base
control hemorrhage
remove all pieces of bone frome horn
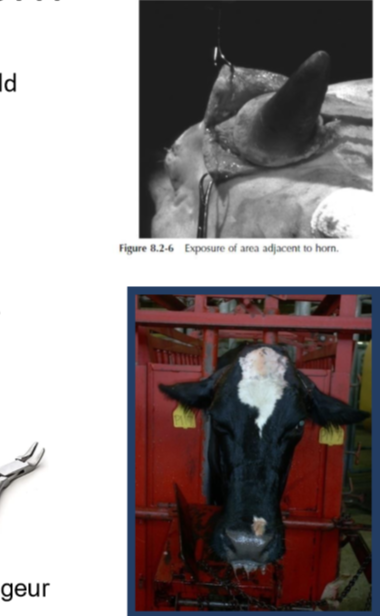
Dehorning in adult cattle
dehorning cattle with large size horns is not recommended - sinusitis, skull fractures, pain
keystone dehorner
used for large horns of heifers, cows, and bulls
good restrait
local analgesia
post operative NSAIDs

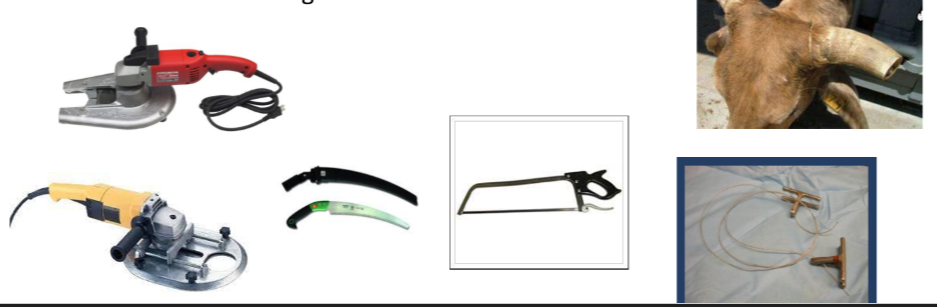
Horn tipping adult cattle
Adult cattle, bulls
cut distal 1/3 of the horn length
manual saw dehorners
electric saw dehorners
OB wire dehorning
cosmetic dehorn
preferred in animlas younger than 2 years old
show cattle to improve appearance of head
standing restraints, tranquilization, cornual nerve block
aseptic preparations
surgical removal of all germinal epithelium
use barn dehorner to cut horn from its base and bone rongeur to smoothen the bone edges
close skin the non absorbale, vertical mattress
remove skin sutures in 3 weeks
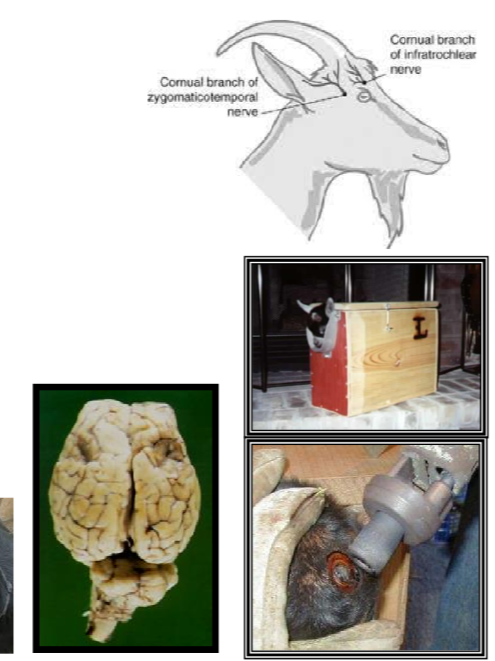
Disbudding goat kids
Electrothermal (hot iron)
Disbud kids before 2 weeks of age
restrain in a dehorning box
sedation/ analgesia
local block - ring block
nerve block conrual branch of the lachrymal nerve and infratrochlear branch of the ophthalmic nerve
post operative - NSAIDs, tetanus, antitoxin
complications
thermal meningitis
scurs and ingrown horns
Dehorning adult goats
Not recommended high risk of tetanus, sinusitis, myiasis, abortion, ketosis, and death
dehorning wound is difficult to close with sutures and takes months to heal
the goat looses social ranking
under GA
post op antibiotics, NSAIDs, bandage

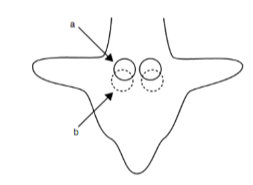
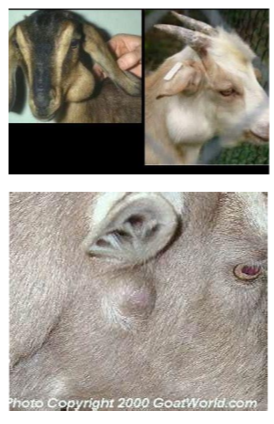
Descenting Goats
A view of the kid from the top of its head
(A) the area of applying the cauterizing unit for descenting
(B) the area of applying the cauterizing unit for dehorning
circles - surgical removal of glands under general anesthesia
Keratoconjuctivitis in sheep and goats
Chlamydophila percorum is the most common cause of pinkeye in sheep
Mycoplasma spp. also can cause pinkeye
very common
clinical signs: Epiphora, hyperemia, mucopurulent discharge, keratitis
history may indicate other problems in the herd: mastitis, polyarthritis, pleuropneumonia
Diagnosis: cytology, IFA, culture
treatment: topical antibiotics, systemic oxytetracycline, NSAIDs, protect the eye
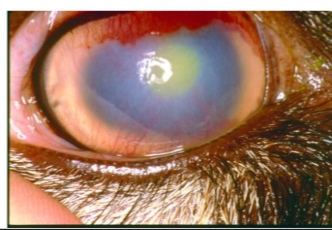
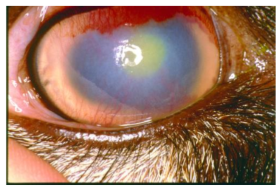
Infectious bovine keratoconjunctivitis
pink eye, contagious ophthalmais, New forest disease
occurs primarily during summer months
all breeds susceptible
Bos tauru » than Bos indicus
Herefords and Hereford crosses
younger > older
DDx - foreign bodies, trauma, MCF, IBR, listeria
Moraxella bovis: gram negative bacillus
newer strains emerged: M. bovoculi
recently discovered cause of IBK: Mycoplasma bovoculi
Neisseria spp can also cause IBK
transmitted by handlers, mechanical vectors (face fly, house fly, stable fly)
75% unilateral eye lesion
epiphora, blephrospasm, photophobia
mucopurulent eye discharge, corneal abscess, blindness in severe cases only
central corneal ulcer

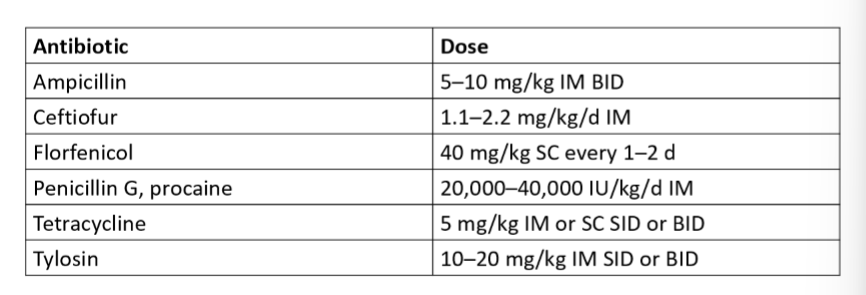
Infectious bovine keratoconjunctivitis treatment
Long-acting oxytetracycline (2 injections of 20 mg/kg, IM or SC at a 48 to 72 hour interval
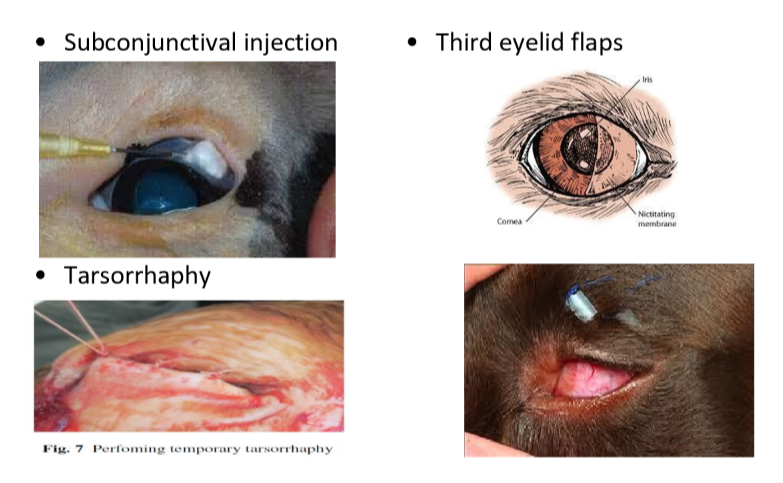
Subconjunctival injection with penicllin (2ml) with or without dexamtheazone (1mg or 0.5ml)
use 25g 5/8 needle
third eyelid flaps, tarsorrhaphy or eye patches
NSAIDs
prevention - vaccination, control flies
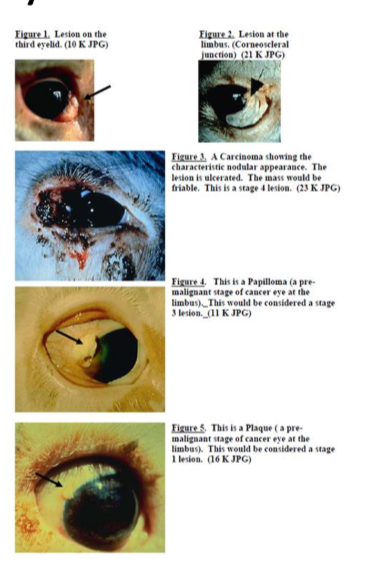
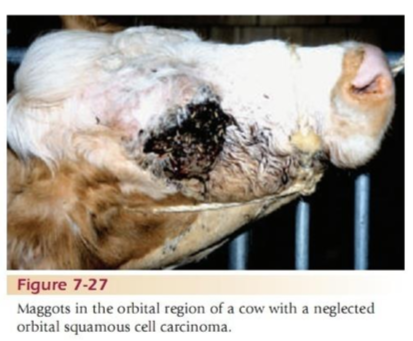
Squamous cell carcinoma (SCC) or “cancer eye”
Economic importance
very invasive locally
may metastasize to the local lymph nodes
predisposing factors:
sunlight, age
non pigmented eyelids and conjunctiva (white faced cattle)
Herefords, simmentals and Holestein - Friesians
most common areas for tumors: the limbus (junction of the cornea and the sclera) the third eyelid, and on the upper and lower eyelid margins
treatment
small lesions less than 2 cm
cryosurgery
eyelid wedge resection
third eyelid resection
larger lesions (5cm or more): Enucleation
invasive lesions: culling
prognosis: 40-50% recurrence rate
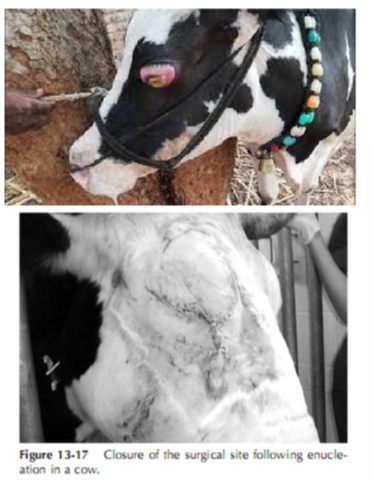
Enucleation
Surgical removal of the entire eyeball
indications
panophthalmitis
intra-ocular neoplasia
severe primary or secondary infection, eg infectious bovine keratoconjunctivitis
trauma or rupture of globe
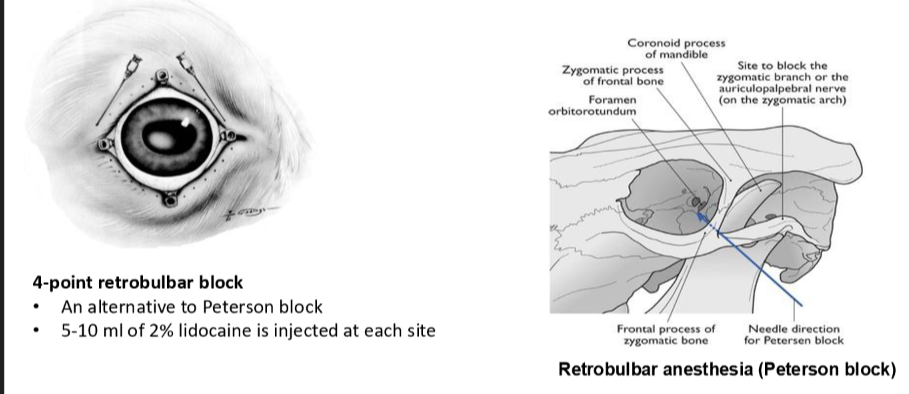
restraint and analgesia
standing or recumbent
sedation 10-20mg xylazine IV
eyelid aknesia - auriculopalpebral nerve block: needle inserted front of the base of the at the end of zygomatic arch
post op care
systemic antibiotics for 5-7 days
NSAIDs for 3 days
tetanus prophylaxis as required
remove sutures in 3 weeks
complications
failure or inability to remove all neoplastic tissue (SCC)
massive intra-orbital hemorrhage
abscess formation
excessive dead space
failure to appose the skin margin without excessive tension on sutures
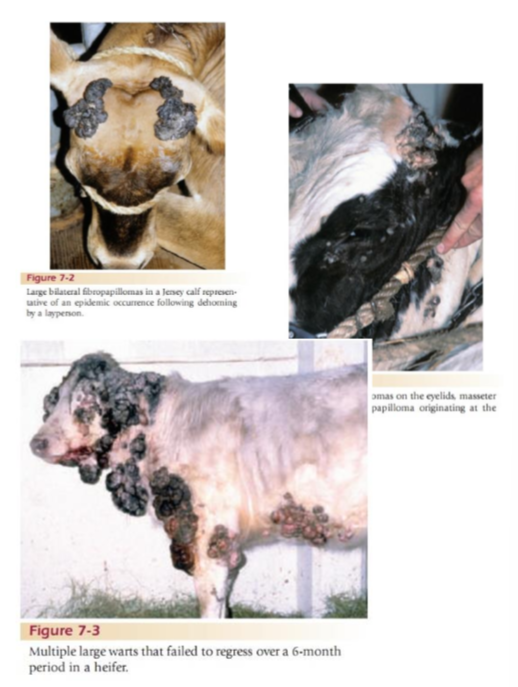
Papillomatosis (Fibropapillomas, warts)
Most common skin tumor in cattle
benign and self limiting
6 and 24 months old most at risk for warts
associated with dehorning, ear tagging, tattooing devices
lesions are cauliflower like, rough, or rusty
some appear flatter, gray and have a broad based skin attachment, others have a pedunculated base
head, neck, brisket and sometimes udder and teats and eyelids are mostly affected
treatment:
spontaneous regression within 1-12 months
large wards may be surgically removed and their bases cauterized chemically
cryosurgery
crushing is also used to remove wars and may stimulate the immune system
lithium antimony thiomalate 6% solution 15 mL by deep IM injection every other day 4-6 times
prevention:
commercial or autogenous vaccines should be repeated at 7 day intervals
in show animals it takes at least 4 to 6 weeks before vaccination cause warts to regress
disinfection of surgical instruments
Dermatophytosis (Ringworm)
club lamb fungus in sheep and goats
common in diary young calves in group housing during winter months
Trichophyton verrusconsum is the most common pathogen
infection by contact
zoonotic disease
treatment
remove crusts and debs
topical application of 7% iodine solution
topical application of chlorine bleach (1:10 dilution)
sun exposure: UV rays from sunlight aid healing

Club lamb fungus
treatment options
most effective treatment
prevention strategies
hygiene practices
avoid communal bathing areas
disinfect grooming tools and equipment regularly
early detection
isolate affected lambs promptly to prevent spread
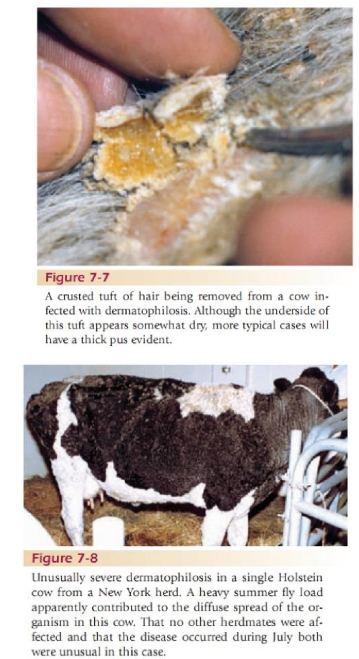
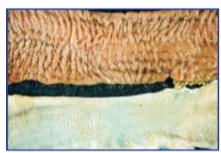
Dermatophilosis
Rain rot; Rain scald; Streptothricosis in cattle, goats, lamas; lumpy wool in sheep
Dermatophilus congolensis - gram positive, non acid fast, facultative anerobic actinomycete
moist environmental conditions and long hair coats predisposes to infection
animlas housed outside during rainy seasons
clinical signs - matted tufts of hair
zoonotic disease
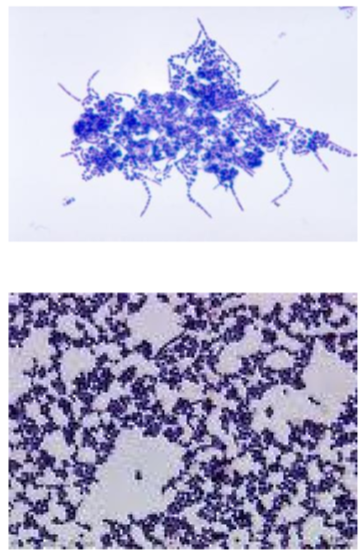
Diagnosis
bacterial smears
gram stain, new methylene blue, or Diff-Quik
parallel rows of gram positive cocci that look like railroad tracks or tramcar line
treatment
topical and systemic antibiotics
topical application of lime sulfur
keep animals dry
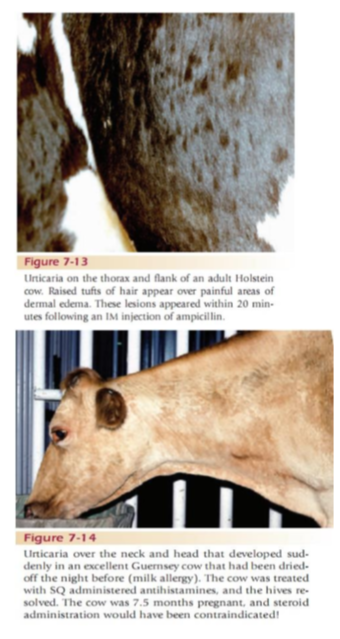
Urticaria and Angioedema
Hypersensitivity reactions
Urticaria (hives) appears as skin wheals or mucous membrane swellings as a result of dermal edema
Angioedema tends to imply larger swelling or plaques of edema that involve subcutaneous tissue
variety of drugs, feeds, and other stimuil may evoke hypersensitivity reactions
rapid onset
severe respiratory and cardiovascular signs
milk allergy is common in jersery cows at drying off
treatment
remove inciting cause
Antihistamines, NSAIDs with or without coricosteroids
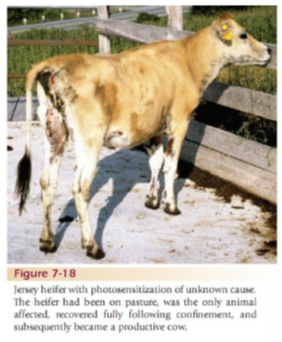
Photosensitization
Primary:
occurs when a photodynamic agent is either ingested, injected or absorbed through the skin
Examples: hypericin (St. John’s wort), fagopyrin (Buckwheat), furocoumarins (psoalens) from various toxic plants
Congential photosensitization resulting in aberrant pigment synthesis
bovine erythropoietic porphyria
bovine protoporphyria
secondary (hepatogenous) photsensitization
the most common type
impaired hepatic detoxification and excretion of the phototoxic agent phylloerythrin
hepatotoxic plants containing pyrrolizidine alkaloids
blue green algae
molds such as Aspegillus sp, fusarium sp, and pithomyces sp
Diagnosis
clinical signs - erythema and edema of hairless, nonpigmented areas of skin
evidence or history of exposure to photosensitizing agents or hepatotoxins
Evidence of liver damage, elevated SDH, GGT, ALP, direct bilirubin
prognosis is poor for cattle with hepatogenous photosensitization
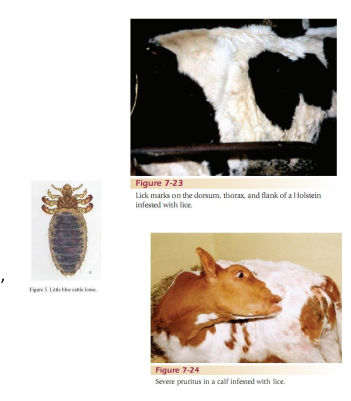
LIce
2 types
sucking lice - larger and take blood meals
biting lice - feed on dead skin and feathers
causes pruritus, restlessness, and excessive licking
blood loss anemia in calves
treatment
organochlorine, organophosphorus, pyrethroid, coumaphos, diazinon and permethrin
Ivermectin injectable gets sucking lice but not biting spp
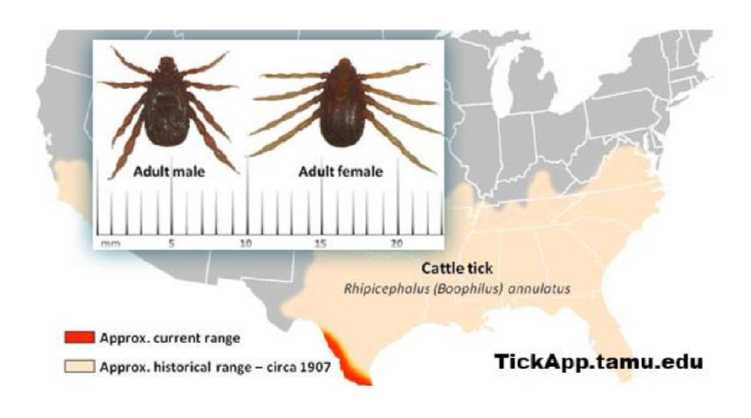
Ticks
2 types: soft and hard
inflammation, itching, and swelling at the site of the bite
anemia, weight loss, and even death
ticks can also create wounds that can become infected if not taken care of
spread diseases
Dermacentor - tansmits anaplasmosis
Cattle fever tick (Rhinpicephalus annulatus) - transmits babesia (reportable)
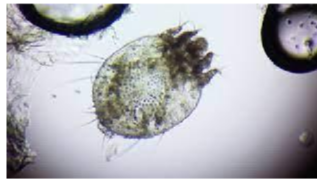
Mange
occur during colder months, in houses animals with close contact
causes skin irritation, hide damage, reduced gain
reportable in most states
several species
Psoroptes cuniculi - ear mites in sheep and goats
Chorioptes bovis - tail or foot or red mange, pruritic and nodular lesions, most common type of mange in cattle
Demodex - non pruritic nodular lesions containing the mite, cigar shaped mite
Diagnosis
microscopic examination of skin scrapes
scrape the edges of the lesion using scalpel
wet scraping with 10% potassium hydroxide
treatment
cattle
use approved products
injectable or pour-on formulations of doramectin, ivermectin, and moxidectin
2 to 3 topical treatments separated by 2-3 weeks
sheep and goats
hot lime sulfur spray or dip. treatment should be repeated every 12 days if needed
Obligatory or Primary Myiasis (Screwworm)
the fly larvae are completely parasitic
invade small skin wounds or mucus membranes
Eradicated in USA using the sterile male release program
occasional outbreaks in ares on Mexico border (Recently in Florida in Deer)
reportable disease

Facultative Myiasis
Blow fly strike or maggots
more common problem in sheep less in goats and cattle (breech region in sheep)
castration and tail wounds, clipping wounds, head wounds on fighting rams
open wounds that are infected and smelly attract flies (wound strike or maggots)
treatment
wound care
Larvicidal agents - ivermectin or organophosphates
prevention
shearing regularly before the summer: shearing controls outbreaks
crutching (ie wool is shorn between the legs and around the tial)
Mulesing (ie operation to remove folds of skin from the hindquarters of the sheep) welfare issue
topical application of quarternary ammonium, phenols, caustic soda or plastic clips on the hindquarter of sheep
proper care of surgical and traumatic wounds - Ivermectin given at time of sx provides residual protection for 16-20 days
insecticide sprays or ointments
vaccination
Hypodermiasis (Warbles, Grubs)
Warble or heel flies of cattle:
reported in sheep, goats, deer, humans, dogs, cats,
hide damage, decreased milk production, weight loss
decreased amount of feeding time due to irritation and gradding
entire life cycle is 1 year
larvae migrate to the submucosa of the caudal thirds of the esophagus
larvae reac the epidural adipose tissue between the dura mater and periosteum of the thoracolumbar vertebrae
treatment
treat cows between July 1 till end of October
to prevent adverse reactions cattle should NOT be treated between December and March
pour on products - ivermectin, moxidectin, organophosphates
adverse reactions
esophageal inflammation could choke
temporary or permanent paralysis
anaphylactic reactions are common

Sheep ked
not a tick but a wingless blood suckling fly
keds will bite humans producing painful result
spreadby contact; long wooled breeds are more susceptible
heavy infestation common in autumn and winter
loss of condition, anemia, irritation, biting and rubbing, damaged skin and low quality fleece
diagnosis by inspection of affected wooly areas looking for wingless fly
treatment using pour on products - ivermectin, moxidectin, organosphosphates

Pygmy goats as pets
Origin: West Africa
Introduced to the U.S. in the 1950s for research and exhibition
gained popularity as pets and livestock due to small size, friendly nature, anda adaptability
lifespan: 10-15 years

Pygmy goat internal parasites
types: GI nematodes, flukes, lungworms
clinical signs
weight loss, poor growth, anemia, poor hair coat, submandibular edema (bottle jaw,) diarrhea
specific signs (coughing from lungworms)
risk factors: environmental conditions, stocking density
diagnosis fecal exmiantion, fecal egg count

treatment of internal parasites in goats
administer only when clinical signs are evident. avoid overuse
assess anemia severity using FAMACHA
combination treatments are more effective than single drug treatments in reducing the survival of resistant worms, especially if used early
examples: albendazole + levamisole
monitor drug efficacy using fecal egg count
consider breeding for inherent resistance
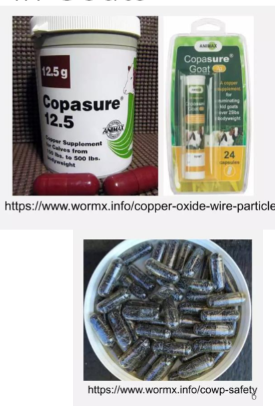
Copper oxide wine particles (COWPs):
COWPs are tiny copper oxide rods
used as a supplement to reduce barber pole worm infections in sheep and goats
best used selectively for animals showing clinical signs of hemonchosis (FAMACHA score 4)
combination treatment examples:
Albendazole + COWPs
Levamisole + COWPs
decision-making tools for deworming:
FAMACHA system: specifically for blood feeding parasites like barber pole worm
five point check
eye: check for anemia
jaw: look for bottle jaw
back: assess body conditon score (BCS)
tail: observe for dags
coat: inspect for coat condition
happy factor
performance indicators: use average daily gain and or milk production
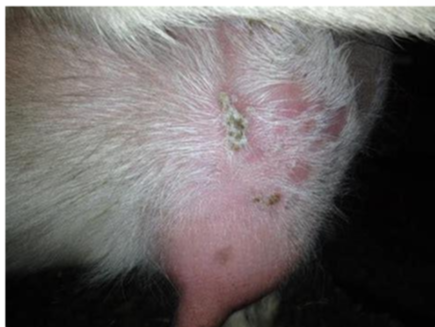
psoroptic mange (ear mange)
Caused by P. cuniculi
typically infests the ears of goats but can spread to the head, neck, and body
clinical signs: scaling, crusting, inflammation, alopecia, ear scratching, head shaking, and rubbing of ears and head
prognosis is good with appropriate treatment
treatment
ivermectin, moxidectin or eprinomectin
Coumaphos, toxaphene, lime sulfur and phosmet
repeat treatment at least twice 5 to 7 days aprat
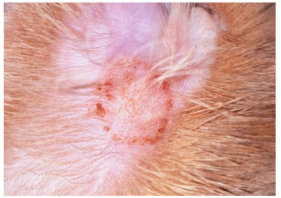
Chorioptic mange
C. caprae
lesion distribution: scrotum, distal limbs in sheep; lower limbs, abdomen, hindquarters in goats
clinical signs: alopecia, erythema, excoriation, crusting; pruritus, restlessness.
treatment
ivermectin, moxidectin or eprinomectin
repeat treatment at least twice, 5 to 7 days apart
Demodectic mange
D. caprae
lesion distribution: face, limbs, back; severe folliculitis, secondary pyoderma
diagnosis: deep skin scraping; examination of exudate for mites
treatment: ivermectin, moxidectin, or eprinomectin
repeat treatment at least twice 5 to 7 days apart
Lice
Clinical signs: pruritus, alopecia, anemia, skin damage, loss of condition, decrease in production (both milk and wool)
treatment:
Coumaphos
malathion
injection of avermectin anthelmintics
avermectin are useful in treating sucking lice but have limited efficacy against biting lice
repeat treatment at least twice 5 to 7 days apart
Dermatophilosis (Streptothricosis, Lumpy wool disease, rain scald, rain rot)
causative agent: Dermatophilus congolensis baterium
transmission: through carrier animals, biting insects, abrasion, and moisture
predisposing factors: skin damage, moisture, weakened immune system
clinical signs: papules and pustules coalesce, forming “paintbrush lesions”
diagnosis: gram stain, histopathology, culture
treatment:
topical agents like iodine
oxytetracycline
prevention: maintain dry conditions, good nutrition and control ectoparasites; vaccines have limited effectiveness

Staphylococcal Dermatitis
Nonpruritic lesions on head and face
alopecia, papules, crusts, erosions or ulcers, exudation, erythema, hyperpigmentation, thickening of the skin.
diagnosis: culture, histopathologic examination
treatment:
Antibiotics
wash affected skin with iodine or chlorhexidine shampoo
topical antiseptic
antibiotic ointment (Oxytetracycline/polymyxin B)
prevention: prevent facial injuries, control fly populations, isolate affected animals
Dermatophytosis (Ringworm)
Caused by Trichophyton verrucosum
infection by contact
zoonotic disease
treatment
remove cruts and debris
topical application of 7% iodine solution
topical application of chlorine bleach (1:10 dilution)
sun exposure: UV rays from sunlight aid healing
Bacterial pneumonia
Pasteurella multocida, Mannheamia hemolytica, Mycoplasma spp
symptoms: fever (>104F) coughing, nasal discharge, difficulty breathing, weakness, death
Diagnosis:
auscultate the lungs for abnormal lung sounds such as crackles or wheezes
thoracic radiographs
collect a tracheal wash sample for bacterial culture
treatment: antibiotics, NSAIDs, supportive care
prevention: good nutrition, sanitation, proper ventilation, vaccination
Viral pneumonia
Parainfluenza type 3 (PI3)
member of the paramyxovirus family
clinical signs: coughing, nasal discharge, fever rare
diagnosis: virus isolation
treatment: supportive
prevention: vaccination with live intranasal vaccine may reduce disease incidence
Adenovirus:
clinical signs: mild, severity increases with secondary bacterial infection
diagnosis: virus isolation or paired serology samples
treatment: supportive
prevention: vaccination with live intranasal vaccine may reduce disease incidence
respiratory syncytial virus (RSV):
clinical signs: anorexia, fever, conjunctivitis, cough, tachypnea, tachycardia
diagnosis: necropsy findings, observation of syncytial cells on histopathologic examination, immunoperoxidase staining
treatment: supportive
prevention: use of a commercial cattle monovalent modified live virus vaccine against RSV
Caprine Herpesvirus:
linked to rhinitis, vulvovaginitis, abortions
may induce mild rhinitis, tracheitis
diagnosis by PCR
treatment: supportive
control: emphasize environmental and stress management
Keratoconjuctivitis
caused by Chlamydophila spp, and Mycoplasma spp
very common
clinical signs: Epiphora, hyperemia, mucopurulent discharge, keratitis
history may indicate other problems in the herd: mastitis, polyarthritis, pleuropneumonia
diagnosis: cytology, IFA, culture
treatment:
topical antibiotics
oxytetracycline
NSAIDs
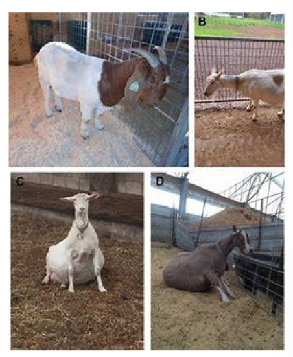
Caprine arthritis encephalitis (CAE)
caused by: Lentivirus
clinical signs: progressive paresis in kids, arthritis in adults, agalactia, chronic weight loss
transmission: vertical (colostrum, milk) and horizontal (blood, mucus)
diagnosis by serologic testing (ELISA, AGID) PCR
treatment: pain medications
prevention:
isolate kids immediately after birth
feed kids pasteurized colostrum
test kids for CAEV every 6 months and cull positive animals
biosecurity - new additions should be quarantined and tested within 60 days of arrival
chemical disinfection of equipment using phenolic and quaternary ammonium compounds.
Paratuberculosis (Johne’s Disease)
Caused by Mycobacterium avium paratuberculosis
transmission: vertical (colostrum, milk) fecal-oral, in utero, milk
clinical signs: weight loss, submandibular edema, weakness; diarrhea less common
diagnosis: fecal PCR testing, necropsy (enlarged lymph nodes, thickened intestine)
treatment: no cure
prevention:
maintain a closed herd
kidding area cleanliness
vaccinations
there is no vaccine approved for goats
USDA-approved vaccine for cattle is effective in reducing the risk for shedding in lactating herd
Caseous lymphadenitis (CL; cheesy gland)
Caused by: Corynebacterium pseudotuberculosis
transmission: skin breaks, contact with pus, contaminated fomites
forms: internal (chronic weight loss) and external abscesses
diagnosis: radiographs, culture, or serologic testing (SHI test)
antimicrobials (intralesional and or systemic)
treatment is extra-label; strict adherence to withdrawal times is required
systemic antibiotics
long term procaine penicillin G and Rifampin have shown some success
tulathromycin reaches effective concentrations in walled-off abscesses
drainage and isolation
environmental decontamination
strict biosecurity measures
vaccination: there is no vaccine licensed for goats
sheep vaccine - not 100% effective but reduces disease prevalence and incidence
shearing precautions
environmental hazard reduction remove barbed wire and such
Clostridium tetani infection (tetanus)
an anaerobic spore forming bcterium found in soil and manure
clinical signs
lockjaw
muscle spasms, especially in neck, limbs, and back
sawhorse stance
difficulty breathing
seizures and possible death
Diagnosis: based on clinical signs and history of injury
treatment:
tetanus antitoxin, antibiotics (penicillin/tetracycline)
muscle relaxants, sedatives
supportive care
prevention
vaccination (tetanus toxoid)
proper wound care
prognosis: poor
Pregnancy toxemia
Cause: high energy demand late in pregnancy, especially with multiple kids
clinical signs and diagnosis:
neurological signs such as depression, recumbency, tremors, star-gazing, incoordination, circling, and teeth grinding
confirmed by detecting increased urine and blood ketone concentrations
treatment
in early cases
oral propylene glycol 2-3 ounces twice daily
B vitamins, calcium borogluconate
transfaunation
feed energy rich diet
severe cases in late gestation require C-section, IV fluids with dextrose and B vitamins
prevention:
avoid excessive weight gain early in pregnancy
increase grain in final month
provide low stress environment
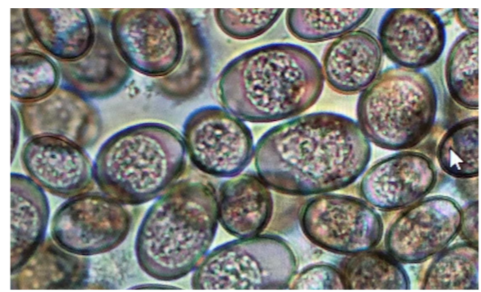
Coccidiosis in the neonate
clinical signs: thin kids, diarrhea, sudden death around ~3 weeks old.
diagnosis: fecal flotation test to detect oocysts of Eimeria spp
treatment:
amprolium
decoquinate
benzeacetonitrile compounds
parenteral sulfadimethoxine
oral sulfadimethoxine
oral sulfadimidine
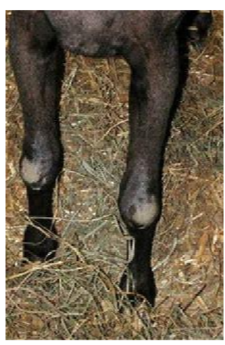
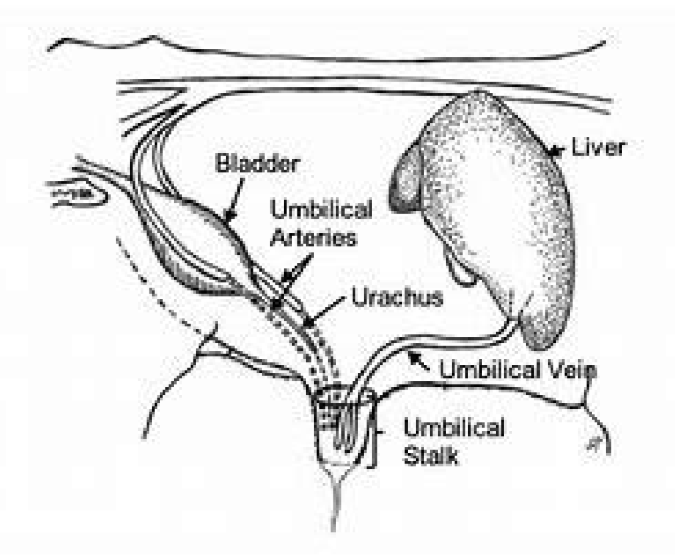
Navel ill and septic joint
cause: infection of the umbilicus
clinical signs: swollen umbilicus, swollen joints, reluctance to move, failure to gain weight
treatment:
systemic antibiotics: Florfenicol or tylosin
joint lavage with saline solution
intra-articular injection of antimicrobials (Ceftiofur, penicilli, amikacin)
regional limb perfusion of antibiotics (ceftiofur, penicillin, amikacin)
surgical removal of the umbilicus
prevention: Dip umbilicus with 7% iodine immediately after birth; maintain a clean birthing area
Contagious ecthyma (sore mouth)
cause: orf virus
clinical signs: painful lesions around mouths of kids, on teats of does; may lead to anorexia and starvation
transmission: direct contact, fomites
treatment:
parenteral antibiotics
topical antibiotics
repellents and larvicides to prevent myiasis
NSAIDs for pain
supportive care
prevention: vaccine is live and should only be administered if the disease is present

Polio
causes:
primary: Thiamine deficiency, sulfur toxicity
secondary: excessive grain, rumen acidosis, improper feeding
clinical signs:
stargazing, circling, head pressing, blindness, nystagmus, convulsions, death in 24-72 hours if untreated
treatment:
thiamine: 0.25cc/10pound body weight, 3-4 times daily
prevention:
diet: high roughage, low concentrate
avoid moldy feeds, excessive carbs
supplementation: thiamine, probiotics, brewers yeast
Resuscitation of kids following dystocia
they may look normal initially but crash 2-4 hours later
need to be aggressive in therapy
if depressed: measure bicarb and correct deficit or use BD of 10
soludelta-dortef (1 mg/lb) injection
consider oxygen even if no respiratory difficulty and normal color
dehydrated, non-diarrheic (septic, hasnt nursed): hypoglycemic
if <8% dehydrated, mild depression, still walking: 150-250 mls oral calf electrolytes without bicarb
If >8% dehydrated, depressed, recumbent: correct fluid deficit with balanced electrolyte solution
follow up with milk
Castration
castration of males reduces offensive odor
should be delayed to allow musculoskeletal development
early castration (before 3 months) hinder penile development and urethral diameter leading urolithiasis
aseptic techniques, proper pain management and post-operative care are essential for animal well being
surgical castration under general anesthesia is preferred
complications can include hemorrhage, infection, and tetanus
dystocia goats
causes: fetal malpositioning, fetal disproportion, multiple fetuses, incomplete cervical dilation (ringwomb), uterine inertia, and uterine torsion.
C-section common in pygmy goats
ringwomb
failure of the cervix to adequately dilate resulting in dystocia
causes:
late gestation hormonal imbalance
nutritional factors
genetic predisposition
treatment
early intervention
IM administration of estrogen
followed by SQ hourly xytocin (10 units)
manual dilation: gradual manual dilation with adequate lubrication after the second oxytocin dose
most effective treatment: Cesarean section for rapid and successful resolution
Foot rot goats
cause:
Fusobacterium necrophorum and Dichelobacter nodosus
wet and muddy conditions promote infection
overgrown hooves increase susceptibility
signs
lameness, swelling, pain, reluctance to walk
necrotic lesions in the interdigital space with a foul odor
diagnosis: clinical signs physical exam
treatment
systemic antibiotics: penicillin streptomycin or oxytetracycline
foot bathing in formalin or zinc sulfate
prevention
quarantine new animals before flock introduction
maintain dry and clean barns
regular hoof trimmig and foot care
provide balanced nutrition with essential minerals
goat hoof trimming
untrimmed hooves are prone to developing lameness, splayed toes, and foot rot
hooves are trimmed regularly preferably every 4 to 6 weeks
hoof care
conduct regular foot baths, especially during wet seasons to maintain hoof health

Deworming program for goats
conduct regular fecal exams (every 3-4 months) to monitor parasite load
deworm strategically based on fecal egg counts
rotate pastures to reduce exposure to parasite eggs and larvae
deworm 3 to 4 times annually (every 3-4 months)
deworm does before kidding and during the last month of pregnancy
goat vaccination program
Core vaccinations
CDT (Clostridium perfringens type C + D and tetanus)
vaccination for does
vaccinate 30 days before giving birth
administered as two shots 3-4 weeks apart
vaccination for kids
from vaccinated does
first dose at 5-6 weeks of age
booster 3-4 weeks later
from uncertain vaccinated history does
first dose at 7-21 days of age
booster 3-4 weeks alter
option to give tetanus antitoxin at birth or castration
optional vaccinations
caseous lymphadenitis vaccine if CL is common in the area
rabies if there is a risk or it is required by local laws
Foot trimming swine
indications
to prevent lameness and ensure proper locomostion
to treat overgrown hooves, cracks, or foot infections
done as needed typically every 6-12 months in mature pigs or when lameness is oberved
procedure
restrain using a chute, sling, or sedation
use hoof shears, a rasp, or an angle grinder
remove overgrown hoof material carefully avoiding damage to sensitive tissues
treat any visible lesions, cracks, or infections with antiseptics or anibiotics

Tusk trimming (boars)
to prevent injuries to handlers, other pigs, or sows during breeding
every 6-12 months, depending on the growth rate
use a wire saw, bolt cutters, or an electric grinder
restrain with sedation
trim the tusks just above the gum line, avoiding damage to the pulp cavity to prevent pain or infection
disinfect tools before and after use
apply antiseptic to the trimmed area
Tail docking
to prevent tail-biting which can lead to infections and abscesses in pigs
perform tail docking within the first 3-7 days of life
use sterilized equipment such as a sharp cutter, scissors, or a cauterizing device
leave about 1-2 cm of tail to minimize nerve damage
apply an antiseptic to prevent infection
docking tails too short lead to rectal prolapse
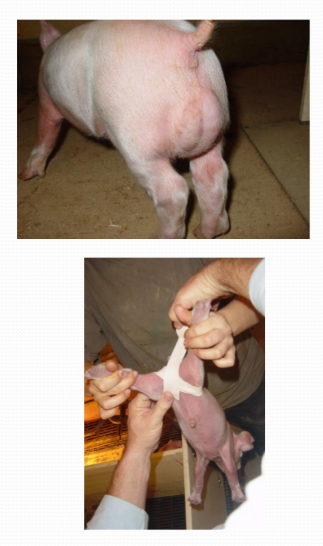
Needle tooth removal
to prevent injuries to littermates and sows udder during nursing
perform within the first 24-48 hours of life
use sterilized sharp clippers or grinders to clip the sharp tips of the 8 needle teeth (corner deciduous incisors and canines)
avoid clipping too close to the gum to prevent damage and infection
disinfect tools between litters to prevent disease transmission
OHE
performed in pot belly pigs
indications
to prevent unwanted pregnancies
to prevent ovarian and uterine tumors
therapeutic treatment of chronic uterine infection tumors
age 6-8 weeks optimal
linea alba incision
use 3 clamp vessel ligation technique
subcuticular closure
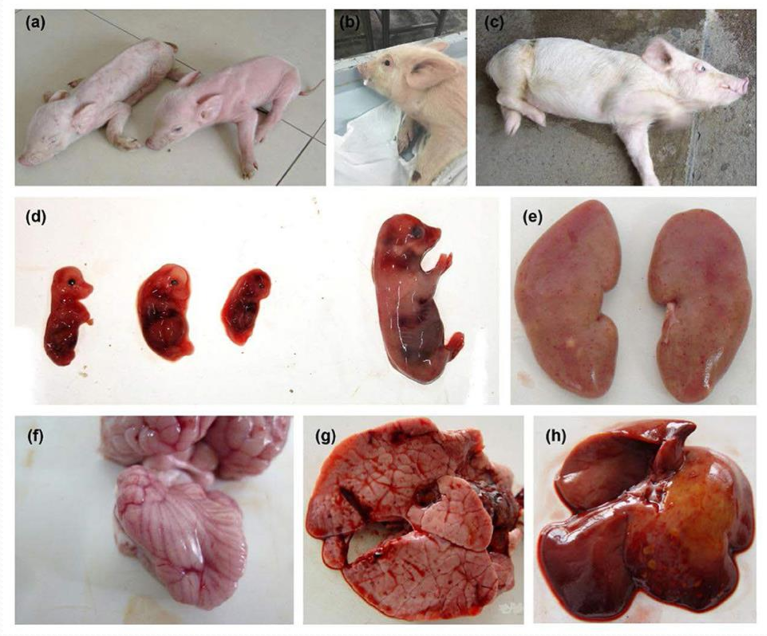
Pseudorabies (Aujeszky’s disease)
herpes virus
affcts all ages
clinicals signs
suckling piglets: sudden death
growers and weaned piglets: nervous signs
tremors, incoordination, dog-sitting, paddling, convulsions, coma and death
finishing and adults; respiratory signs
sows: reproductive failure
clinical symptoms:
giving birth to weak piglets
foaming at the mouth
severe neurological disorders
aborted fetus
hemorrhagic spot on the renal cortex
cerebral hemorrhage and congested meninges
pulmonary hemorrhage
liver with mulitple small focal areas of necrosis
Swine influenza
clinical symptoms:
fever, coughing, pneumonia spreading rapidly, rapid return to normality within 7-10 days
reproductive failure: return to estrus, abortions, reduced litter size, infertility in boars
Epidemiology:
endemic in most herds
intermittent bouts of respiratory disease and infertility
Diagnosis: virus isolation in nasal swabs, serology
prevention strategies: biosecurity measures, vaccination
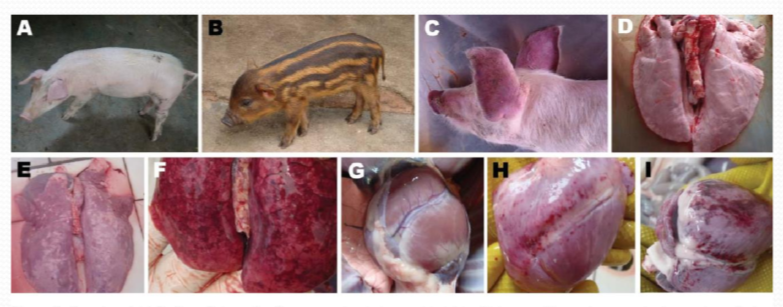
Porcine reproductive and respiratory syndrome (PPRS)
affects all ages
causes significant economic loss
clinical symptoms:
pneumonia in weaners:
mild coughing
sneezing
increased respiratory rates
death rate up to 15%
reproductive failure in sows
late term abortion
premature birth
prolonged anoestrus
agalactia
clinical signs and lesions
normal duroc crossbred pig
normal wild boar
red discoloration in ears of a domestic duroc crossbred pig infected with PPRS
normal lung
pulmonary hyperplasia and consolidation in wild boar infected with PPRS
normal heart
cardiac hemorrhages and edema in a wild boar infected with PPRS
Mycoplasma pneumonia (enzootic pneumonia) pigs
endemic in most herds
clinical presentation
acute pneumonia: fever, cough, respiratory distress, high mortality across all ages
chronic cases: prolonged cough and breathing difficulty (thumps)
lung lesions: consolidation of the anterior, cardiac, intermediate, and anterior diaphragmatic lung lobes
diagnosis methods
PCR (polymerase chain reaction) serology
treatment: medicated feed
prevention strategies
maintain an EP disease-free herd
implement biosecurity measures
vaccination
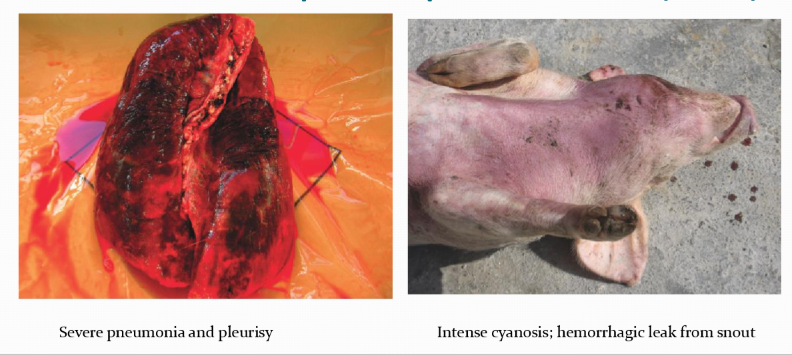
Actinobacillus pleuropneumonia (APP)
affects pigs 8 to 16 weeks of age
respiratory distress
cyanosis of the ears
sudden death with hemorrhage from the nose (dxx bacillus anthracis)
diagnosis
bacterial culture from lesions
PCR
serology (ELISA)
treatment
antibiotic injections
medicated feed or water for the rest of the herd
prevention
biosecurity measures
vaccination
medicated feed
Greasy pig disease (Exudative epidermitis; Staphylococcus hyicus)
affects all ages
septicemia and toxemia cause death
dark patches of flaky, greasy skin lesions
diagnosis - bacterial culture
treatment - antibiotic injection, spray affected pigs several times with 10% bleach, chlorhexidine or dilute iodine
prevention - biosecurity, autogenous vaccine

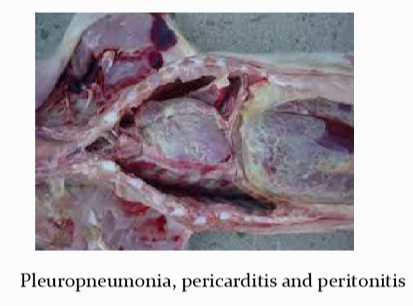
Glassers disease (Haemophilus parasuis)
anthrax-like disease with high mortality and sudden death in sows and suckling pigs
Young growing pigs - meningitis, middle ear infection, pleuropneumonia, pericarditis and peritonitis
diagnosis - bacterial culture
treatment - antibiotics injections, medicated feed or water for the rest of the herd
prevention - biosecurity, autogenous vaccine, medicated feed.
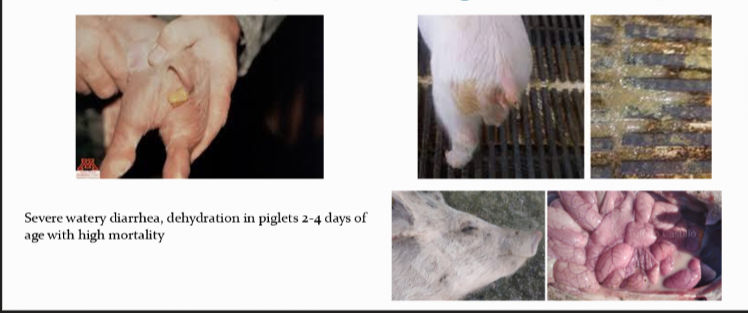
Colibacillosis (Enterotoxigenic E. coli)
severe watery diarrhea, dehydration in piglets 2-4 days of age with high mortality
older pigs are not affected
inflammation of the small intestine with watery, yellow, content
the stomachs of dead piglets is full of milk
diagnosis - bacterial culture from feces or rectal swabs
treatment - antibiotic injection, oral electrolytes, mediated feed for the herd
prevention - hygiene in maternity, all in / all out system, autogenous vaccines, commercial vaccines
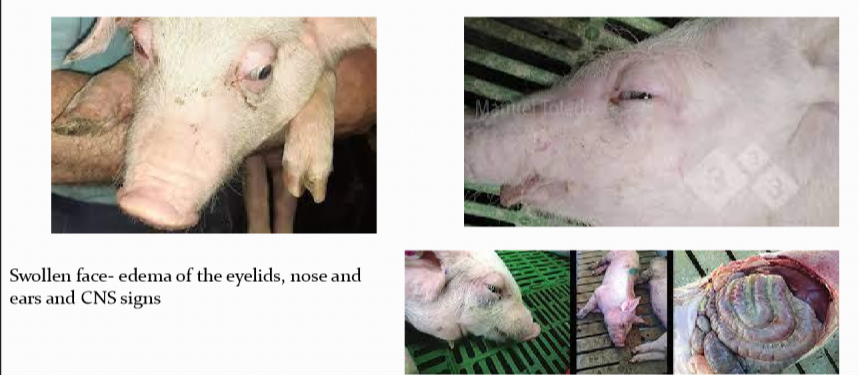
Edema disease
caused by hemolytic E coli that produce Shiga toxin 2e (stx2e also known as verotoxin 2e or VT2e)
affects wearner pigs (days to few weeks after weaning)
associated with dietary changes overfeeding poor hygiene
swollen face edema of the eyelids, nose, and ears
CNS signs - dullness, blindness, head pressing, lateral recumbency, paddling leg movement, coma, death
diagnosis - detect stx2e in feces by ELISA, culture of E. coli that are positive for stx2e and f18 antigens
treatment - antibiotic oral or injection
prevention - improve hygiene, medicated feed, oral vaccination
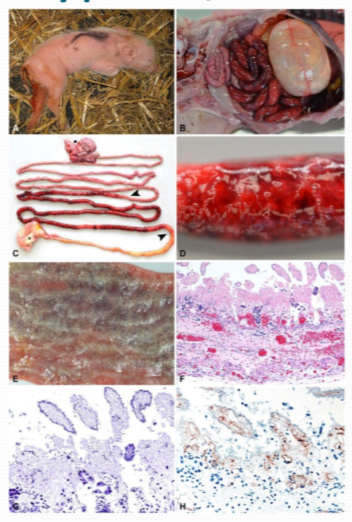
Enterotoxemia C. perfingens
bloody diarrhea and death in piglets hours to few days in age
hindquarters are soiled with bloody feces
pasty pink diarrhea
diagnosis - bacterial culture, demonstration of the beta toxin in the intestinal contents by ELISA
treatment - medicated feed, oral electrolytes, antitoxin
prevention - hygiene, medicated feed, vaccination
Clostridium difficle enteritis (neonatal tyflocolitis)
yellow pasty to watery diarrhea in piglets less than 7 days of age
the colon is swollen with edema and the contents of the lage intestine is pasty to watery and yellow
diagnosis - toxin detection by PCR or ELISA
treatment - medicated feed, oral electrolytes antitoxin
prevention - hygiene, vaccination, medicated feed

Salmonella choleraesuis
all ages are affected
necrotizing enterocolitis with rectal strictures
septicemia/endotoxemia, cyanosis
diagnosis - bacterial culture, serotyping by PCR
treatment - isolation of affected animals injectable antibiotics, oral electrolytes
prevention - biosecurity, medicated feed, vaccination
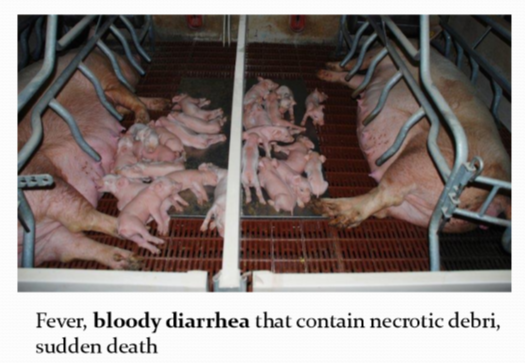
Swine dysentery - brachyspira hyodysenteriae
colitis with watery, bloody diarrhea and death in growers and finishers
diagnosis - bacterial culture from feces, fecal smear, PCR on feces
treatment - antibiotics injection or oral
prevention - biosecurity, medicated feed for the herd, no vaccines

Ileitis
4 forms
Porcine intestinal adenopathy (PIA)
regional ileitis (RI)
necrotic enteritis (NE)
proliferative hemorrhagic enteropathy (PHE; bloody gut) - Massive bleeding into the small intestine, pale pigs, black tarry feces, sudden death
lesions - hose-like thickening of the mucosa of the terminal ileum
transmissible gastroenteritis (TGE)
coronavirus
diarrhea and vomiting across all age groups
severe watery diarrhea and more mortality in younger pigs
lesions - distension of the small intestine with foamy, yellow, odoriferous fluid and milk curds. the intestinal wall is very thin and transparent
improve immunity in pregnant sows and gilts by feeding them guts and gut contents of dead piglets
Streptococcus porcinus (Jowl abscesses)
purulent lymphadenitis of head and neck in weaners and finishers
external drainage of purulent exudate
diagnosis - bacterial culture
treatment - antibiotic injections
prevention - biosecurity

Leptospirosis
sows and gilts - abortions, stillbirths infertility
weaners and growers - jaundice, acute death
tx - medicated feed
prevention - biosecurity, vaccinaiton

Brucellosis
females - infertility, late-term abortions, stillbirths, weak piglets, vulval discharges
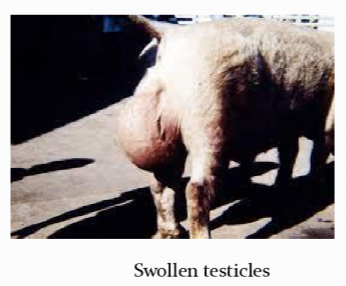
boars - swollen testicles, infertility
treatment - none
prevention - biosecurity no vaccine for swine
Iron toxicity
muscle necrosis and death within 24 hours after iron injection
acute lameness within 2 hours after iron injection
injection site become dark and swollen
heavy breathing, pale
lesions - muscles appear pale due to necrosis of the muscle fibers, myocardial infarction

Cryptorchidectomy
retained testicles (ridgelings, one-nutters)
important in show barrows due to mounting behavior
very helpful to know which side is retained if animal is unilaterally castrated
NEVER do a unilateral castration on a cryptochid and leave the undescended testicle
testicle usually located dorsally between inguinal canal and kidney
make 2-3 incision on a abdomen of pig on side of retained testicle
feel for testicle within abdomen and exteriorize
ligate spermatic cord
close abdomen
Scrotal hernias
hereditary condition ~1% incidence in industry
often found at time of castration
ddx - hydrocele, scirrous cord, hematoma
treatment
taping method: 1 inch elasticon tape around legs in figure 8 pattern after castration (puts pressure on inguinal rings) remove tape in 4-5 days
surgical correction
needs to be performed prior to castration
umbilical hernias / infected navels
hernias often start with umbilical infection or abscess
not hereditary
only repaired in valuable animals
Disease organisms get to other farms by one of three ways 90% of the time what are those 3 things
Vehicle
poultry equipment
people
airborne transmission is not really a thing
What does every poultry place has no matter what
Coccidiosis

What are the 3 foot baths
1st soapy water
2nd disinfectant
3rd soapy water
The development of an infectious disease depends on three variables:
resistance of the bird
virulence of the disease organism
dosage of the organism
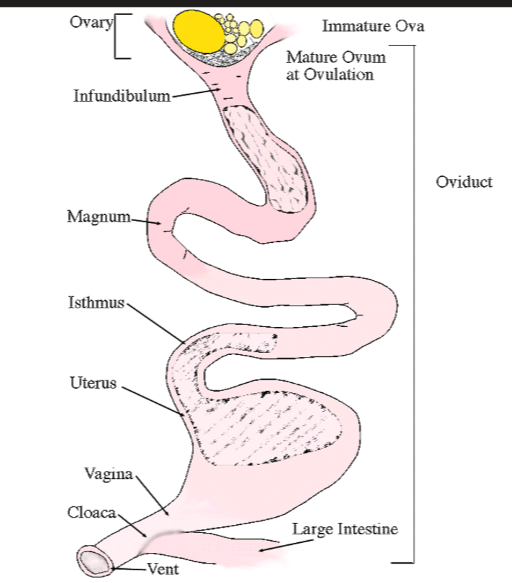
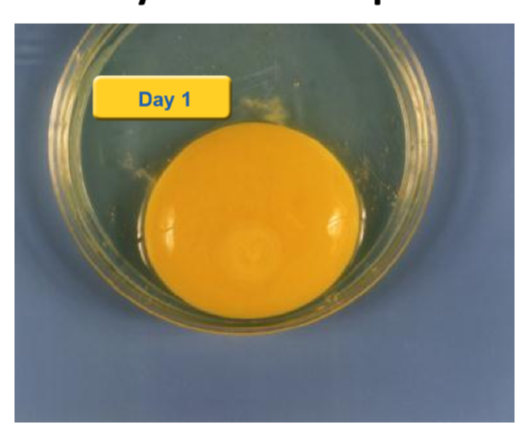
what is the egg really for?
support the development of the chicken embryo
why is nutrient make-up ideal?
it must contain everything needed from fertilization until after chick hatches
why developed as a food for humans
cheap protein source
ideal protein make-up
tastes good
where does fertilization of the egg occur
Infunidbulum
with the light method when do you know if the egg is fertilized or not
if the yolk is high then not fertilized
if fertilized the yolk would be at the bottom by the albumen
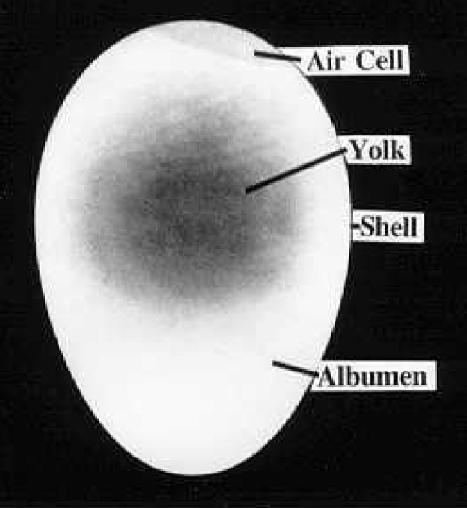
What does it look like in the yolk if it was fertilized
appearance of a donut look in the embryo
appearance of tissue development
infectious bursal disease
an acute very contagious viral disease of young chickens characterized by destruction of immature lymphocytes in the BF and to a lesser extent in other lymphoid organs
recognized in all poultry-producing areas of the world
one of the most important diseases in concentrated broiler producing areas (often not recognized subclinical form)
resistant to disinfectants and environmental factors
can persist for months in contaminated houses
transmission of infectious bursal disease
virus shed in feces
feed, water, litter become contaminated
infection by ingestion of virus
easily transmitted (mechanically) between farms
subclinical form of infectious bursal disease
infection of susceptible chickens less than 3 weeks of age:
no clinical signs, but permanent and severe immunosuppression
more economically important form
majority of field infections are subclinical
clinical form of infectious bursal disease
infection of susceptible chickens 3-6+ weeks of age:
sudden onset, rapid increase in mortality
clinical signs include ruffled feathers, diarrhea, vent pecking, dehydration, trembling, depression, transient immunosuppression
infectious bursal disease lesions
initially, the BF is swollen 2 to 4 days after infection
appears inflamed, edematous and hyperemic, possibly hemorrhagic
at 5 days bursa is normal in size
after 5 days the BF diminishes in size rapidly (atrophies) grey in color
hemorrhages may be present in thigh and pectoral muscles
kidneys may be swollen
severe cases - all follicles affected simultaneously
less severe cases - scattered follicles affected spread to other follicles