Autoimmune Hemolytic Anemia (AIHA)
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Dx is determined from both the diagnostic tests and clinical evaluation of the patient
How is AIHA diagnosed?
Evidence of RBC destruction...
- increased retics
- increased unconjugated bili
- increased LDH
- decreased haptoglobin
If it is a true AIHA then you will also have the following lab results:
Compensated anemia
RBC production = RBC destruction
↑Retics, mild decrease in Hgb/Hct
Uncompensated anemia
RBC production < RBC destruction
↑ Retics > 3%, ↑ unconjugated bilirubin, ↑ total bilirubin, and ↑ LDH levels
↓Haptoblobin, ↓Hgb, ↓Hct
What are the different types of autoantibodies?
- Cold (benign and pathological)
- Warm
- Drug induced
When are autoantibodies usually found?
Generally found during routine testing as a positive DAT or positive auto control with an antibody ID panel
What are the most common reason's for a patient's DAT to be positive?
- Auto antibody
- Allo antibody
- Donor plasma antibody
- Maternal antibody
- Drug-related
- IVIG therapy or hypergammaglobulinemia
- Idiopathic
- Sample contamination
Standard laboratory tube testing will normally detect _________________ of IgG/RBC and ___________________ of complement/RBC
100-500 molecules of IgG
400-1100 molecules of complement
What are some significant factors that may cause someone to be affected or unaffected by AIHA?
- Thermal amplitude of antibody reactivity
- IgG subclass
- Amount of antibody bound to RBCs
- Ability of the antibody to fix complement
- Activity of the individual's macrophages
- Quantitative or qualitative change in the RBC membrane structure
What are the characteristics of cold reactive autoantibodies?
- May be reactive ≥ 30C
- Titer of ≥ 1000
- Strongly enhanced with albumin
- Common specificity for anti-I
- Capable of binding complement
- Clinically significant
- Associated with disease
What tests fo cold agglutinins often interfere with?
- ABO/Rh
- DAT
- ABSC
- Eluate
What are some methods that can be used to remove cold autoantibodies?
Patient has not been transfused in the last 3 months:
- Pre-warm Technique (IAT; No Enhancement Used)
Patient has been transfused within the last 3 months:
- Allo Adsorption
- RESt adsorption
What is the specificity of cold autoantibodies?
Anti-I
Anti-i
Anti-H and IH
Anti Pr, Anti-GD, and Anti- Sdx
Anti-M
Is specificity of cold autoantibodies considered clinically important?
Specificity is not considered clinically important.
Although development of specificities for integral components of the RBC membrane such as glycophorins or band 3 may be precursors for SLE or RA
Cold agglutinin syndrome, also called cold hemagglutinin disease (CHD) represents ________ of AIHA
18%
A _______________ study should be performed after identification of the CAA if the provider is suspecting CHD to confirm the thermal range of the cold antibody
thermal amplitude
RESt binds which antibodies?
anti-I and IH
Which pathological cold antibody is an IgG with a P antigen specificity and is Biphasic?
PCH (Paroxysmal Cold Hemoglobinuria)
What is the Donath-Landsteiner test?
1) Fresh serum specimen drawn and kept at 370 C until separated.
2) Add P+ RBCs at a 50% suspension to each tube
3) Incubate at indicated temperatures and times
4) After incubation, specs are spun down and examined for hemolysis
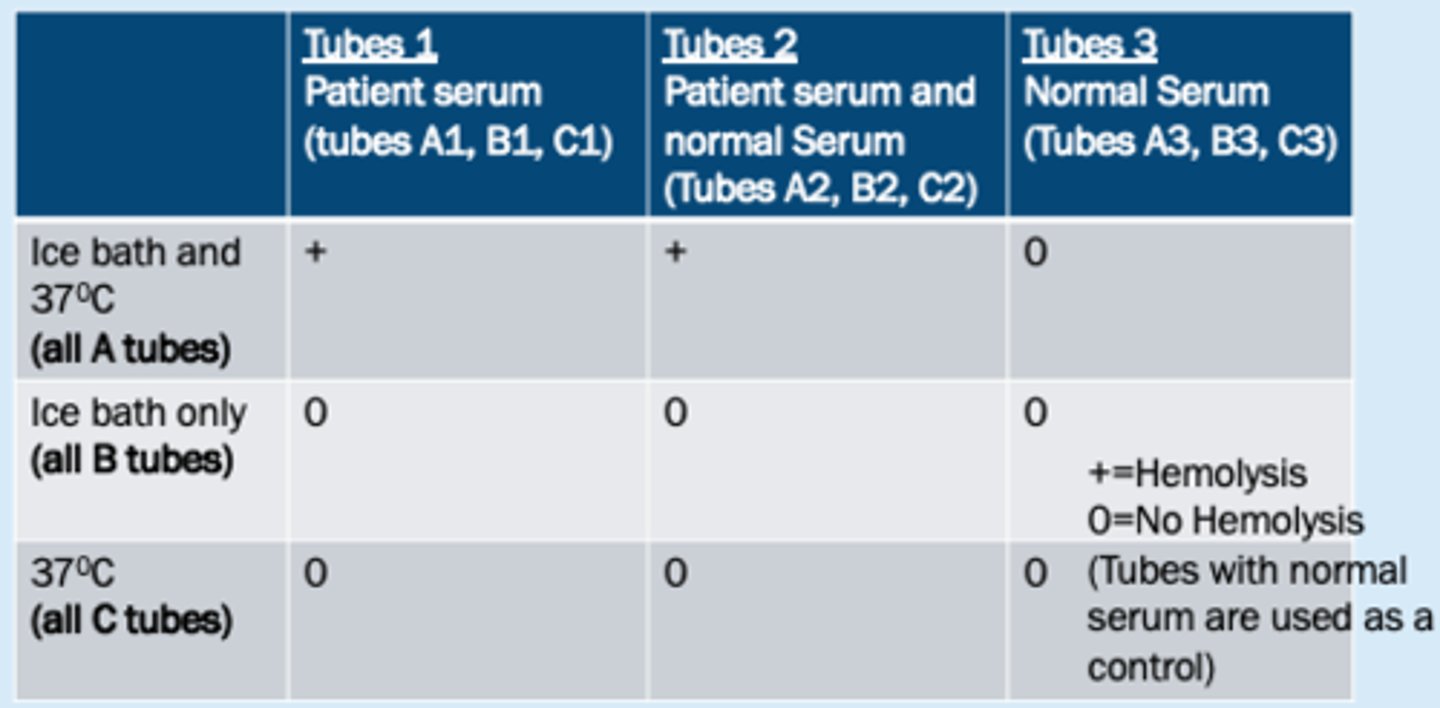
What specimen is required for the Donath-Landsteiner test?
serum (red top with no gel separator) maintained at 37C until serum separated from cells
-- has active C3 --
70% of AIHA is due to this type of reactive antibody
warm reactive antibodies
Are warm reactive autoantibodies clinically significant?
yes, all warm reactive antibodies should be reported to the physician due to the possibility of an underlying auto immune disease.
What are some causes of WAIHA
- infection
- surgery
- pregnancy
- underlying disease or secondary to a pathological disorder.
What are signs and symptoms of WAIHA?
- significant anemia
- pallor
- weakness
- dizziness
- dyspenea
- jaundice
- unexplained fever
80% of WAIHA cases demonstrating hemolytic anemia are caused by ________ antibody
IgG (IgG 1 and 3)
This antibody is IgG and reacts best at AHG
warm autoantibody
What are the serological characteristics of warm autoantibodies?
- IgG
- Reacts best at AHG
- Enhanced by enzymes
- React with high incidence RBC antigens and often have a general specificity within the Rh group (Mimicking antibody)
which autoantibody mimics allo antibodies to the Rh BGS?
warm autoantibodies
With which autoantibody should crossmatch's be avoided if at all possible?
WAA's
most crossmatches will be least incompatible
What drugs are used to treat WAA's?
- Corticosteroids
- IvIG
- Immunosuppressive drugs
Why do patient's with WAA's get a splenectomy as treatment?
If steroid therapy fails, a splenectomy decreases the production of antibody and removes a potent site of RBC damage and destruction
What are the 4 models of drug induced hemolytic anemia?
- Drug adsorption (penicillin type/hapten
mechanism)
- Immune complex (Quinidine, Phenacetin)
- Protein adsorption (Cephalosporin)
- Induction of autoimmunity (Methyldopa, Procanamide)
What are the steps of the drug adsorption mechanism of DIHA?
a. Drug binds to RBC membrane. It may act as a hapten
b. Drug induced formation of antibodies
c. Antibodies bind to drug on cell membrane
d. Extravascular hemolysis occurs. This may occasionally be severe.
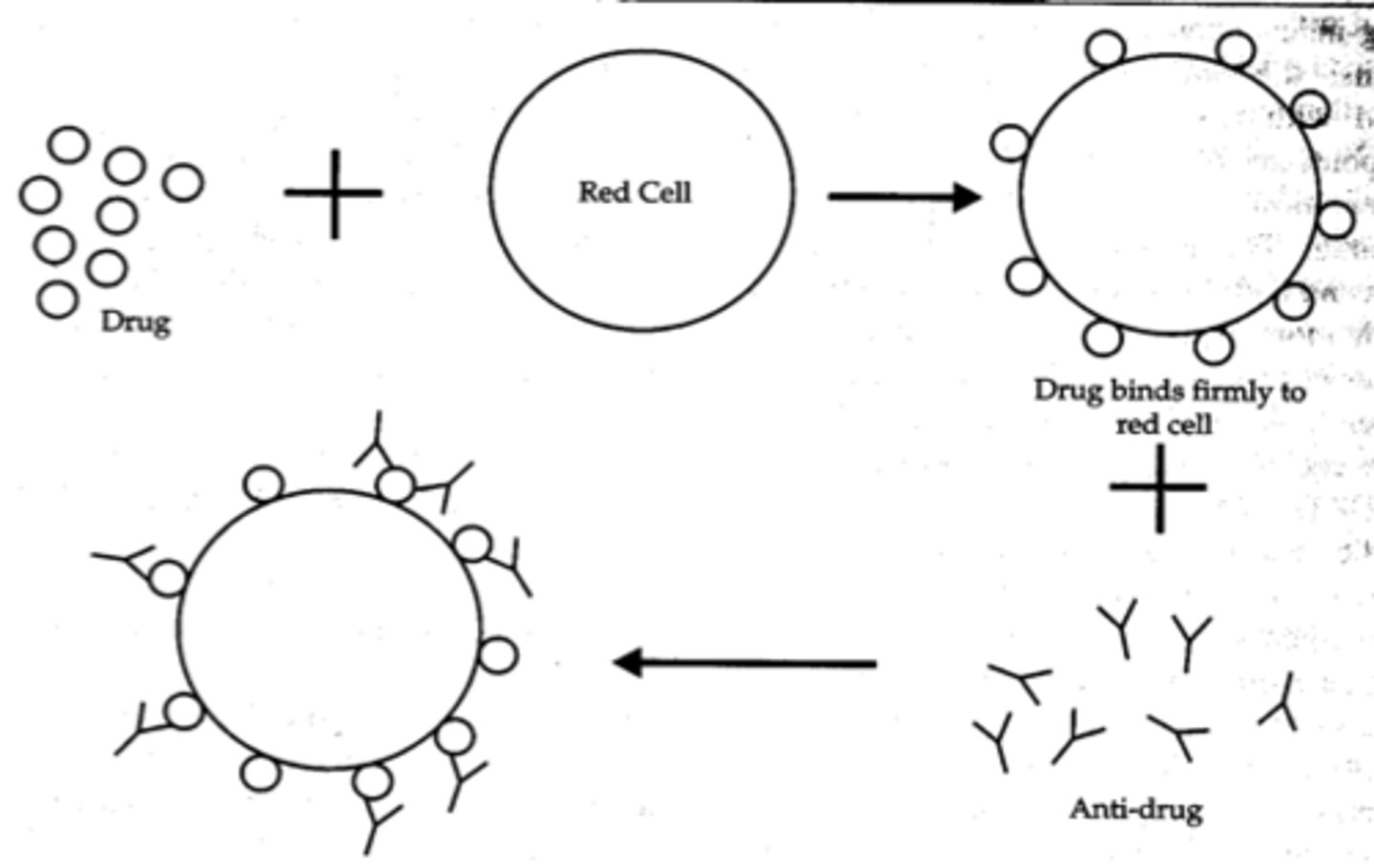
What lab findings are seen with the drug adsorption mechanism of DIHA?
+ DAT with IgG, serum or eluate only react with drug-treated red cells
What are the steps of the immune complex mechanism of DIHA?
1) Antibody forms tight complex with the drug; the "immune complexes" (IC's) circulate in the plasma
2) The IC's bind non-specifically to the red cell and cause C3 to bind.
3) The IC's then dissociate, leaving the cell coated with Complement, to hemolyze.
4) Cause intravascular as well as extravascular hemolysis
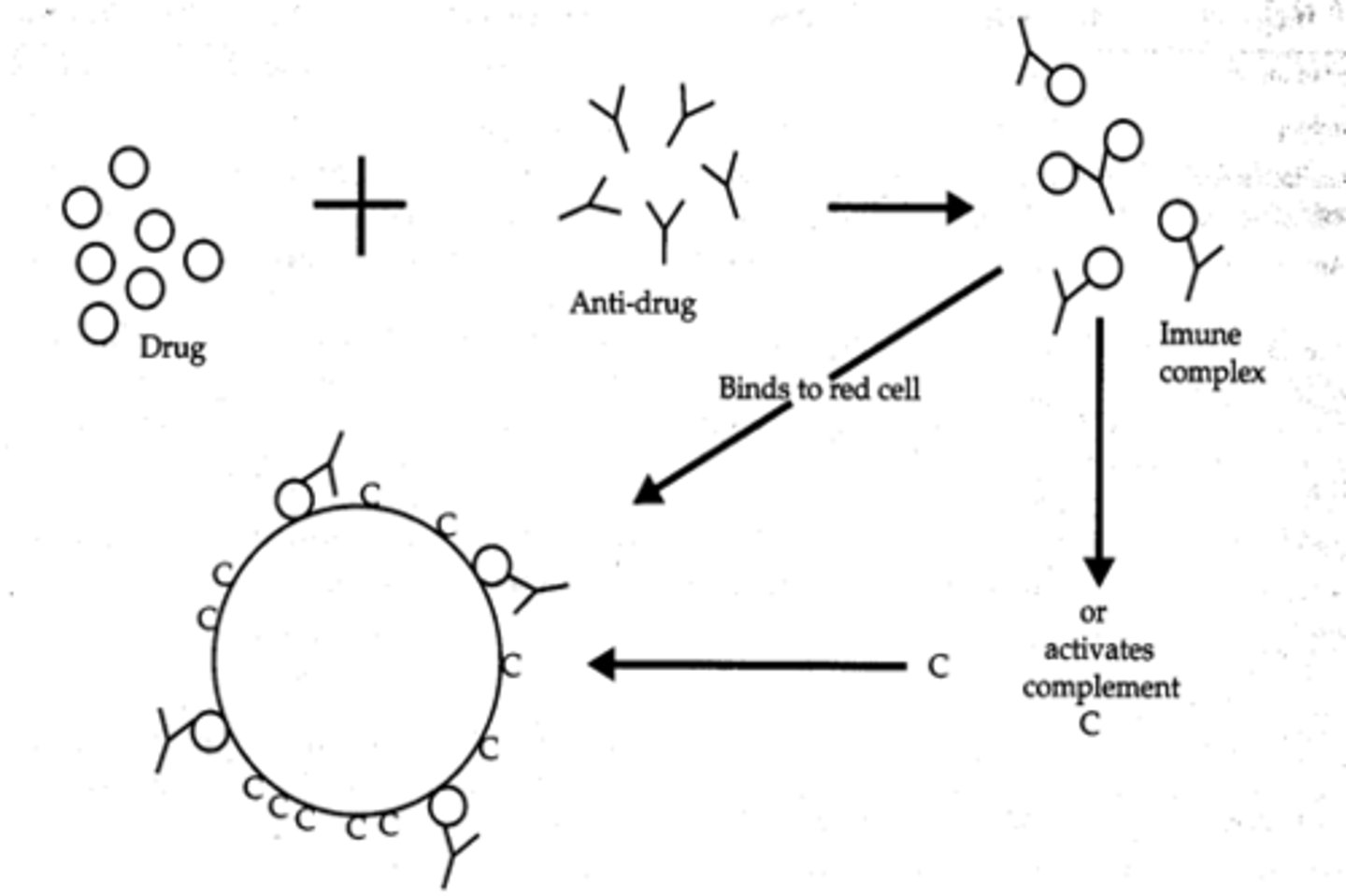
What lab findings are seen with the immune complex mechanism of DIHA?
+ DAT with C3 only usually. Screen or panel will only react if you incubate serum, DRUG, and cells
What are the steps of the protein adsorption mechanism of DIHA?
Drug coats the red cell, modifying the membrane so that other proteins (such as IgG, IgM, C3, albumin, etc) adsorb to the cell
- Clinical results will depend on amount of antibody / complement binding
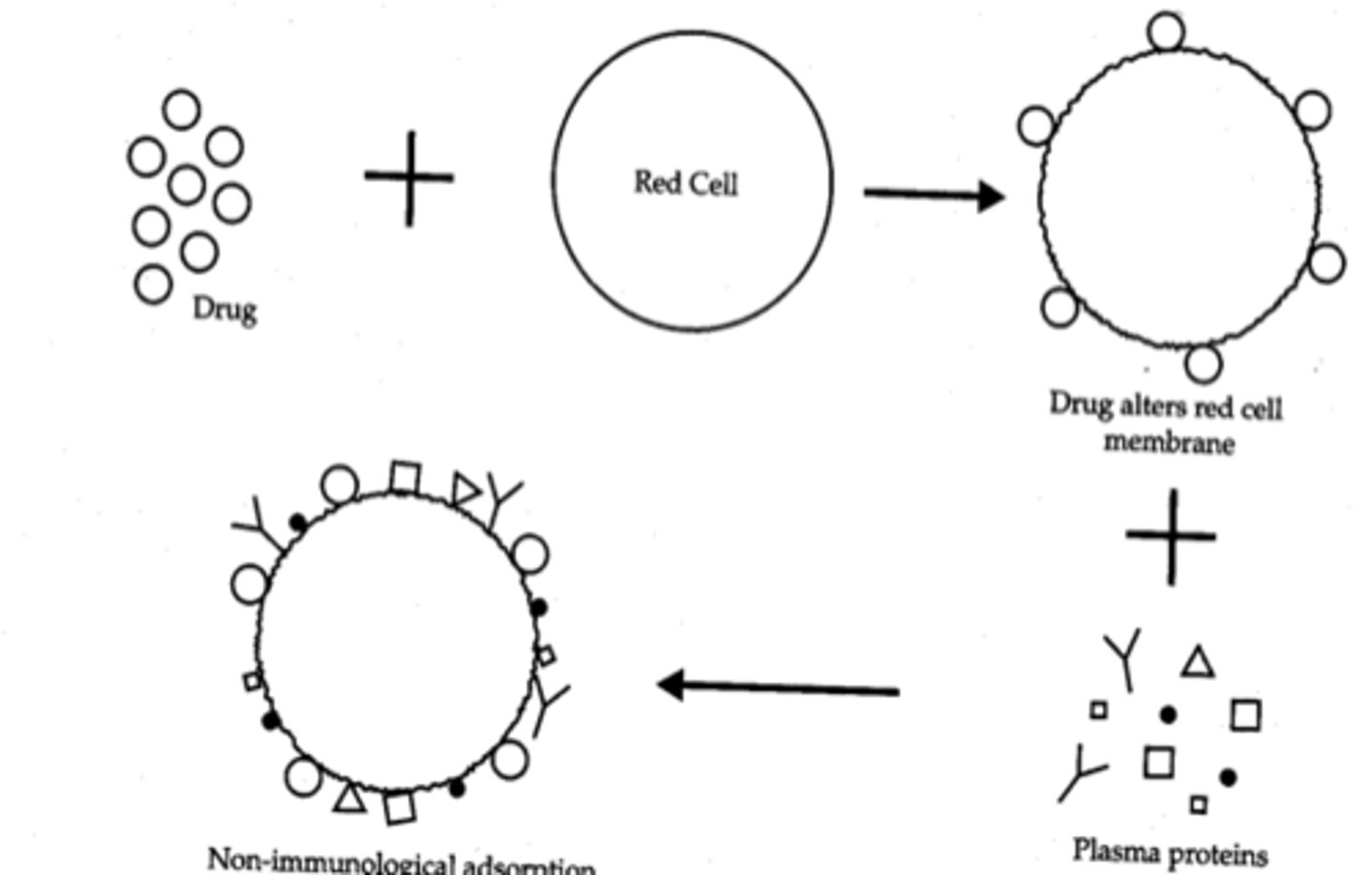
What lab findings are seen with the protein adsorption mechanism of DIHA?
+ DAT with IgG, C3
Negative screen, eluate negative
What are the steps of the induction of autoimmunity mechanism of DIHA?
Real autoantibodies appear to form, binding epitopes that are part of the red cell membrane. 2 possible reasons:
- Drug alters RBC membrane in some way (neoantigen, no longer recognized as "self")
- Drug down-regulates the normal T-suppressor cell function which allows overproduction of autoantibodies
What lab findings are seen with the induction of autoimmunity mechanism of DIHA?
Lab findings are indistinguishable from WAA as described above, usually with IgG only. (HISTORY)
What tests are done to investigate DIHA?
- DAT: Using anti-IgG and anti-C3
- Serum and eluate testing
- Test in presence of drug (immune complexes)
- Test with drug-pretreated cells (drug adsorption)
- Controls
Regardless of the cause of the autoantobody, your patient may need blood. If so, these considerations apply:
1.) Use the smallest amount of blood that can achieve the needed clinical result
2.) DON'T withhold transfusion just because the blood is "incompatible" in the tube!
3) Give ABORh compatible
Usually low risk of acute reaction even if don’t match a mimicking specificity