Cellular pathology: Inflammation and Healing
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
127 Terms
What are the causes of chronic inflammation?
persistent infections
foreign bodies
autoimmune/immune-mediated conditions
repeated mechanical/chemical injury
What type of immunity is chronic inflammation a part of?
adaptive immunity
What immune cells are involved in adaptive immunity?
B & T lymphocytes
What are activated lymphocytes?
mediators of adaptive immunity and are often present in chronic inflammation
What do CD4+ helper (Th) lymphocytes secrete?
cytokines
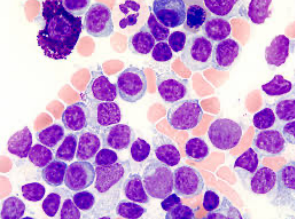
What does this image show?
lymphoplasmacytic inflammation
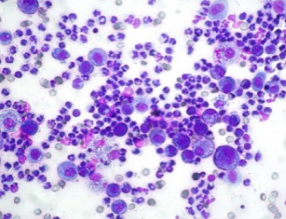
What does this image show?
suppurative chronic inflammation
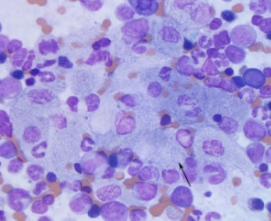
What does this image show?
granulomatous and granuloma formation
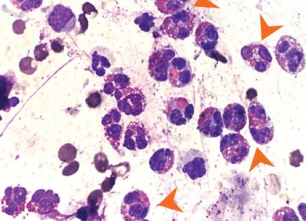
What does this image show?
eosinophilic chronic inflammation
What does chronic inflammation start as?
diffuse mononuclear infiltration
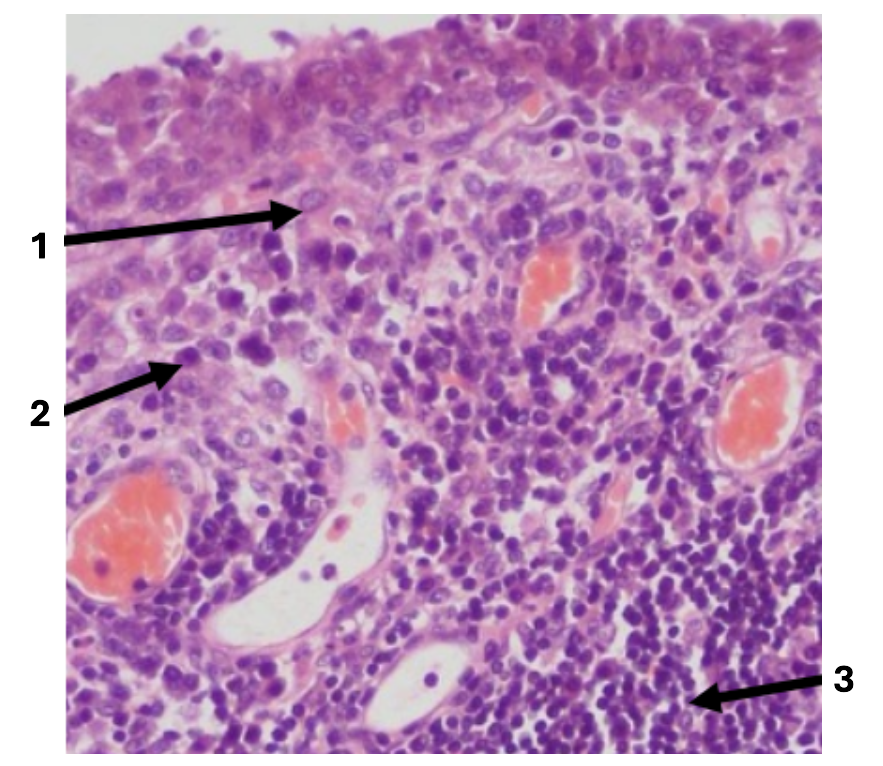
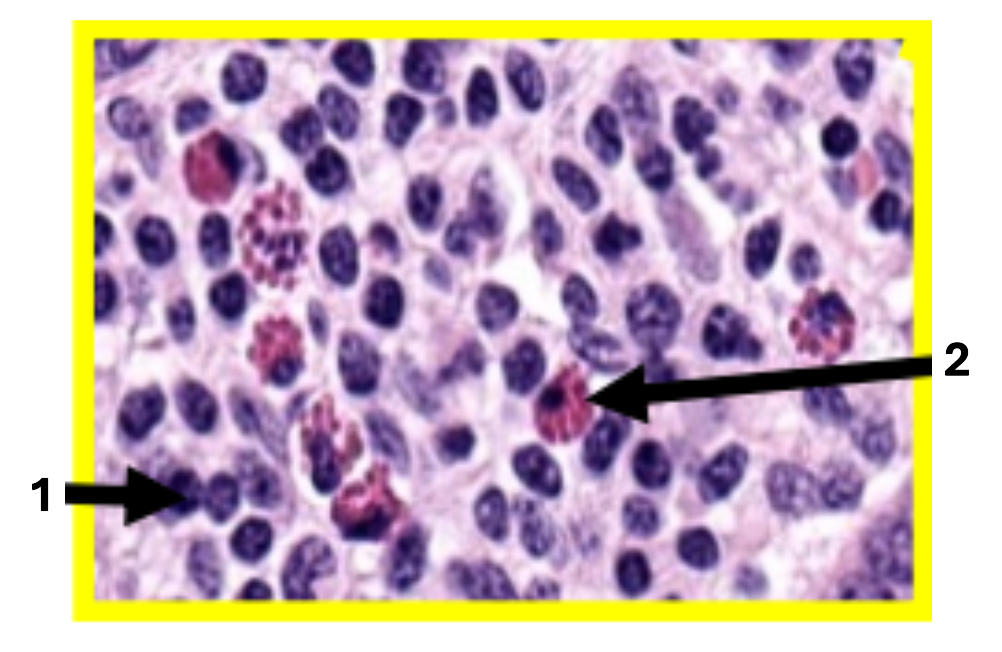
1
macrophage
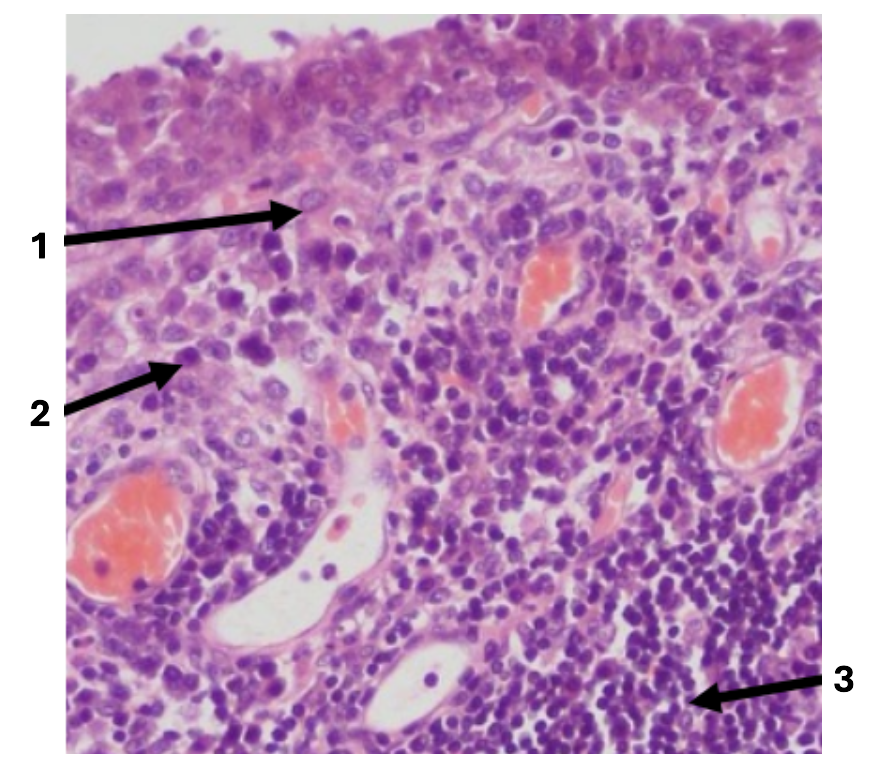
2
plasma cells
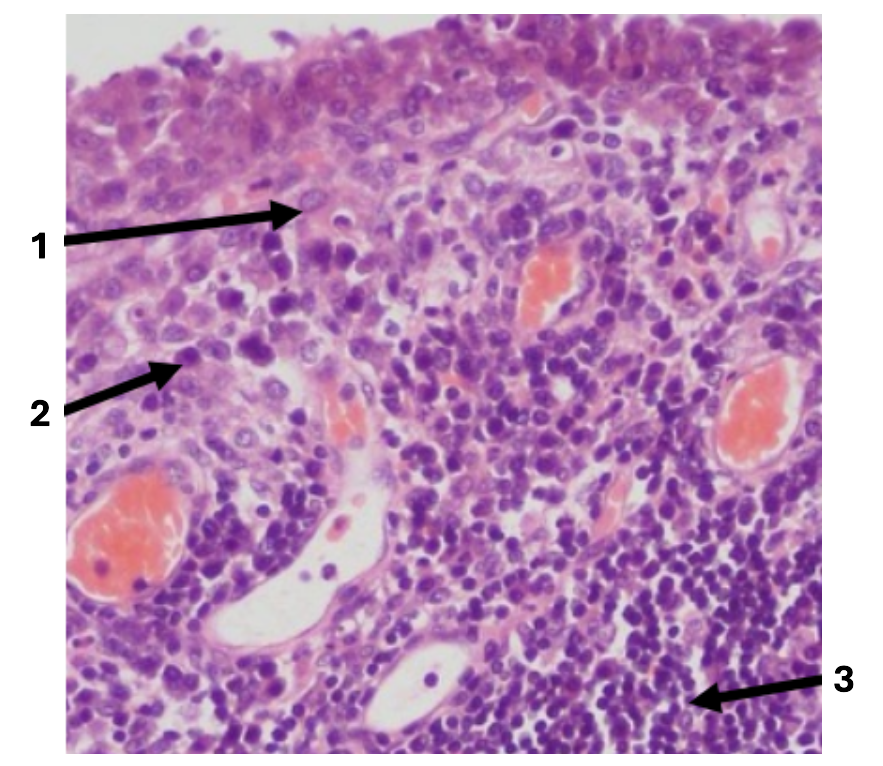
3
lymphocytes
What type of inflammation is common in chronic enteritis, thyroiditis & arthritis (autoimmune disorders)?
lymphoplasmacytic inflammation
In what conditions is lymphoplasmacytic inflammation common in?
chronic enteritis
thyroiditis
arthriti
What occurs during lymphoplasmacytic inflammation?
widespread lymphocyte & plasma cell infiltration
may form lymphoid follicles
What would you see looking at lymphoplasmacytic inflammation under the microscope?
dense mononuclear infiltrate
sometimes lymphoid follicle formation
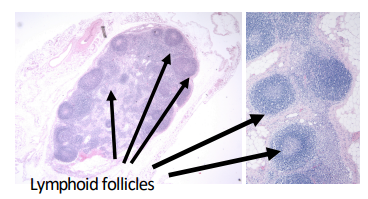
What does this image show?
thyroiditis in African green monkey
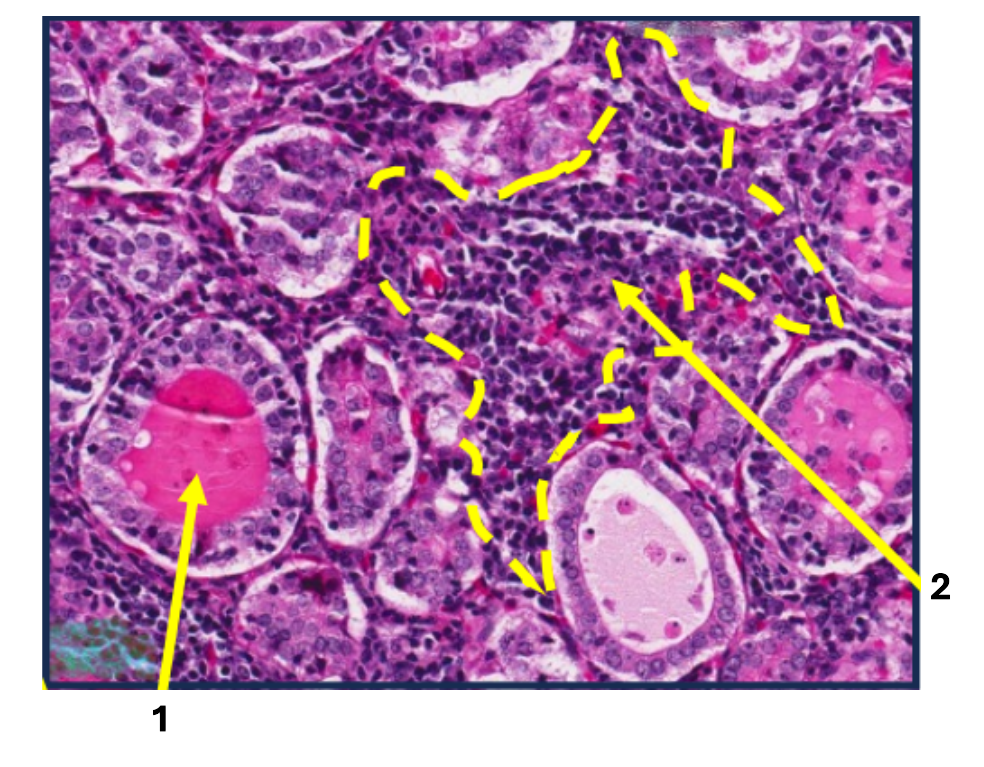
1
thyroid follicles
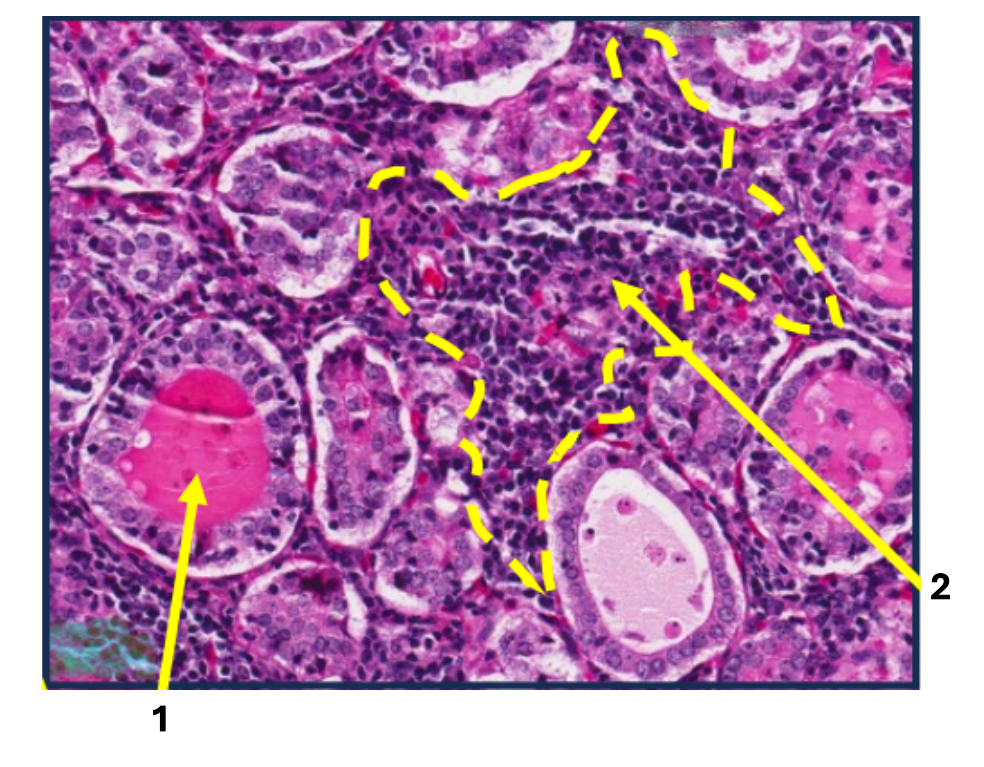
2
lymphocytes & plasma cells
What is the arrow pointing to?
lymphoid follicle
What are the features of suppurative chronic inflammation?
pus
encapsulated abscesses
persistent neutrophil recruitment & chronic mononuclear cells
Name examples of suppurative chronic inflammation
suppurative bronchopneumonia
purulent rhinitis
What are encapsulated abscessed?
fibrous wall surrounding pus
What can you see under a microscope with suppurative chronic inflammation?
central purulent core
fibrous capsule
peripheral mononuclear infiltrate
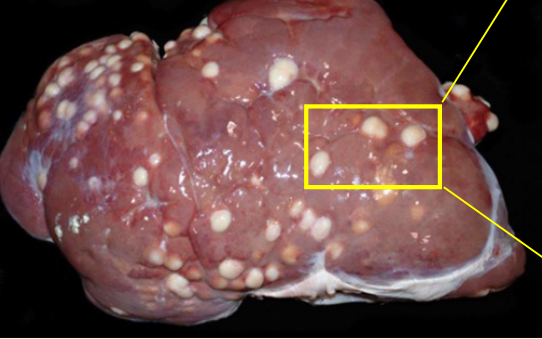
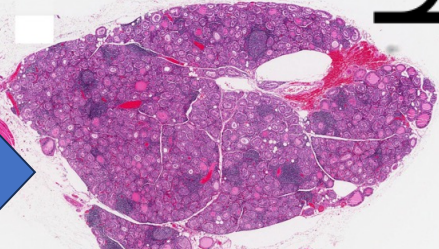
What does this image show?
liver abscesses in goat
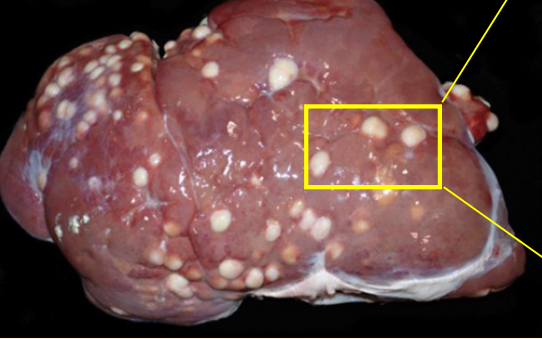
What type of chronic inflammation does this image show?
suppurative chronic inflammation
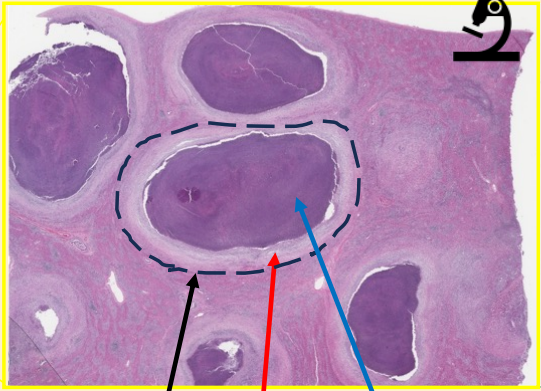
black arrow
abscess
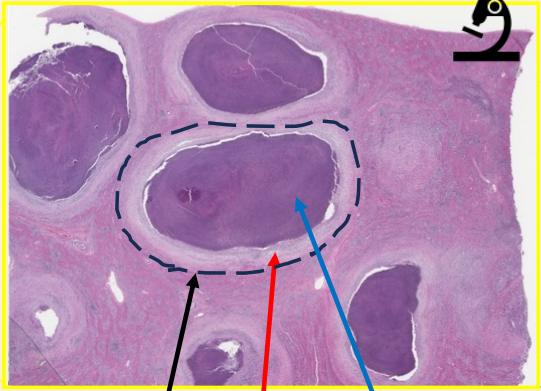
red arrow
capsule
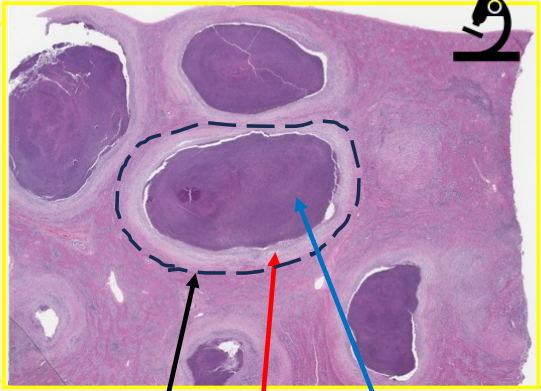
blue arrow
pus
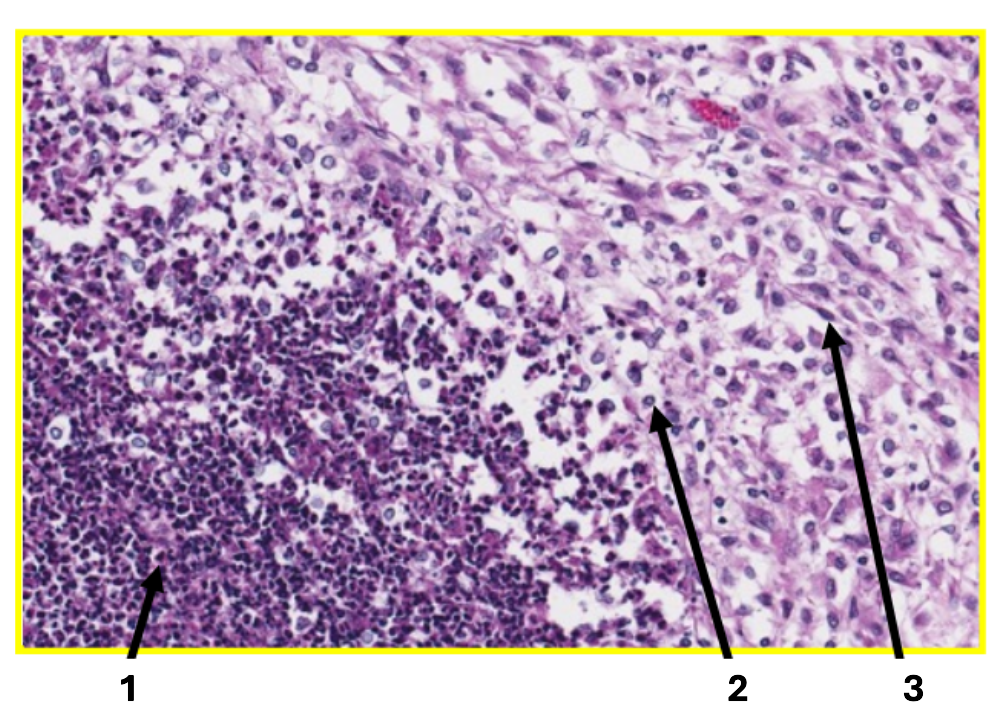
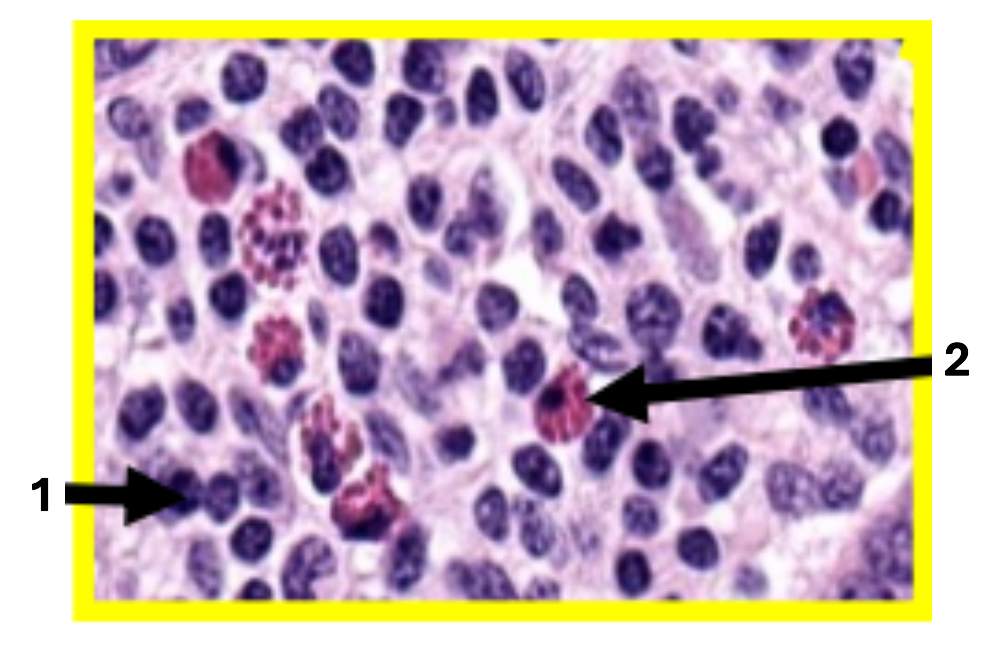
1
neutrophils
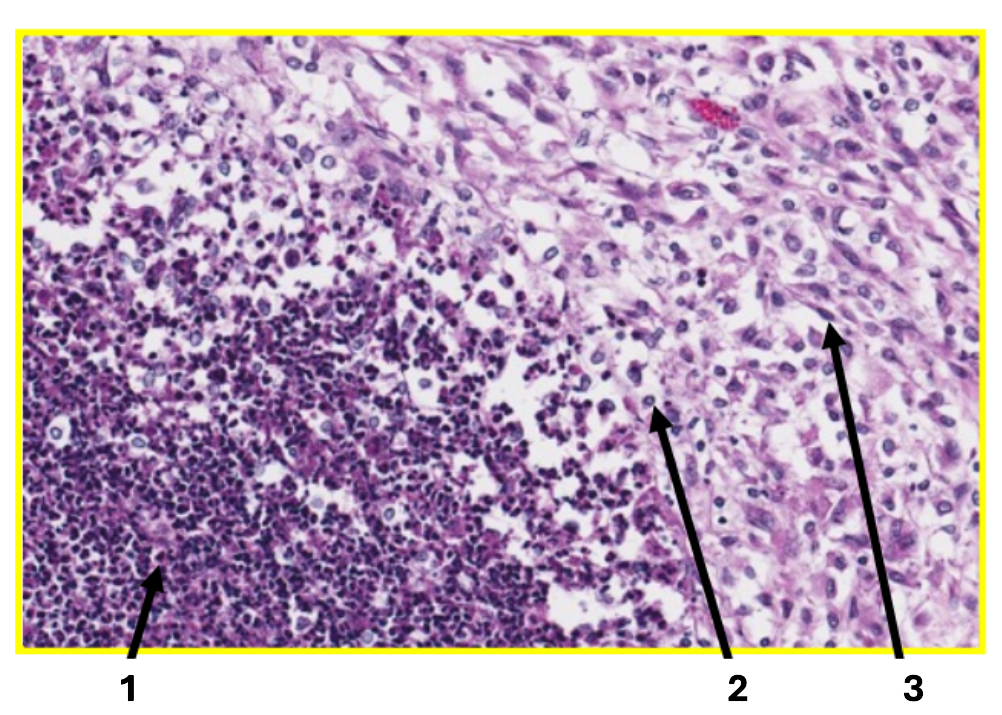
2
macrophages
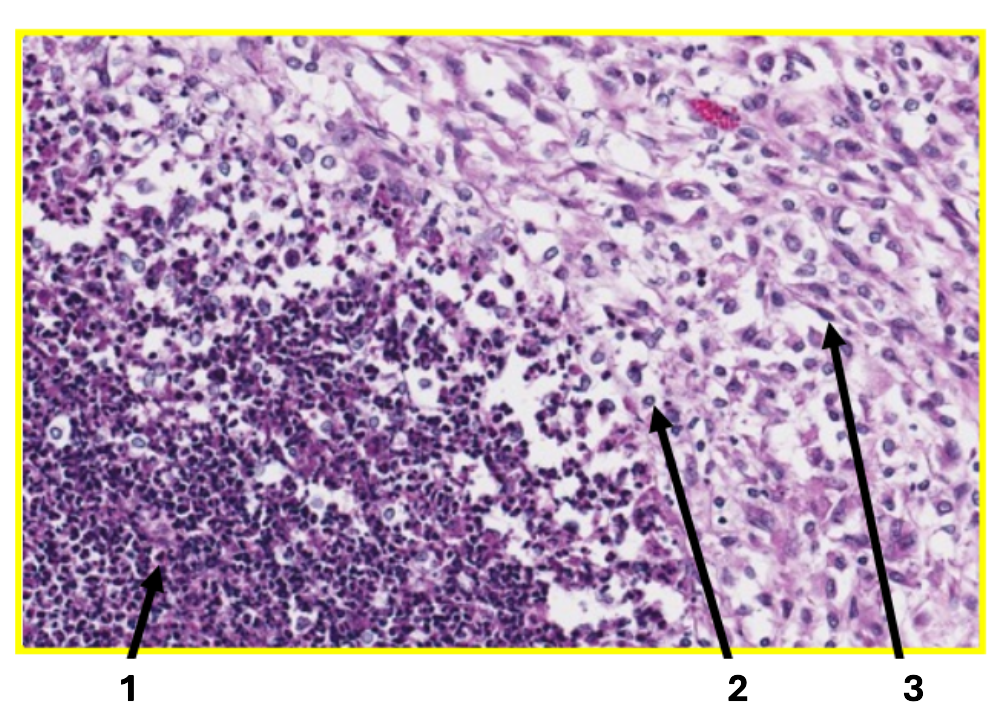
3
fibroblast
What is granulomatous inflammation made of?
macrophages & giant cells
What are common causes of granulomatous inflammation?
mycobacteria (bovine TB)
fungi (cryptococcus, histoplasma)
foreign material (suture granulomas)
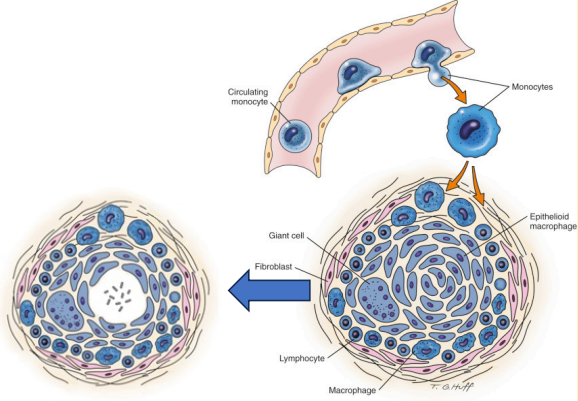
What does this image show?
granuloma structure/formation
What is the structure of a granuloma?
macrophages are dominant cells
surrounded by lymphocytes, plasma cells & fibrous capsule
central accumulation of degenerated cells/organisms/minerals
What food do granulomas look like?
soft cheese
How are granulomas formed?
macrophages engulf organisms
organism resists digestions, multiplies in macrophage
macrophage dies, engulfed by other macrophages
central caseous necrosis may mineralise
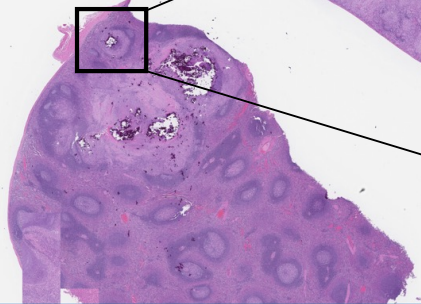
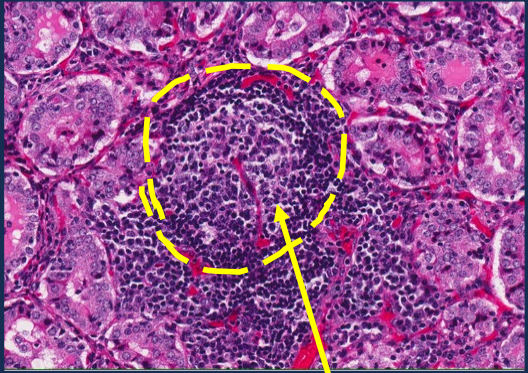
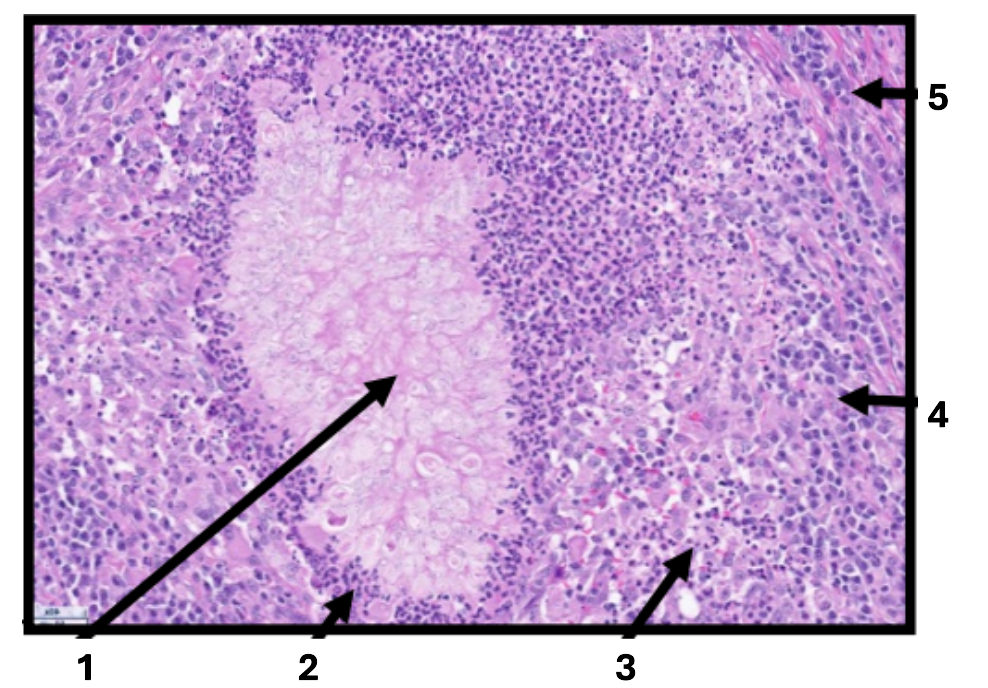
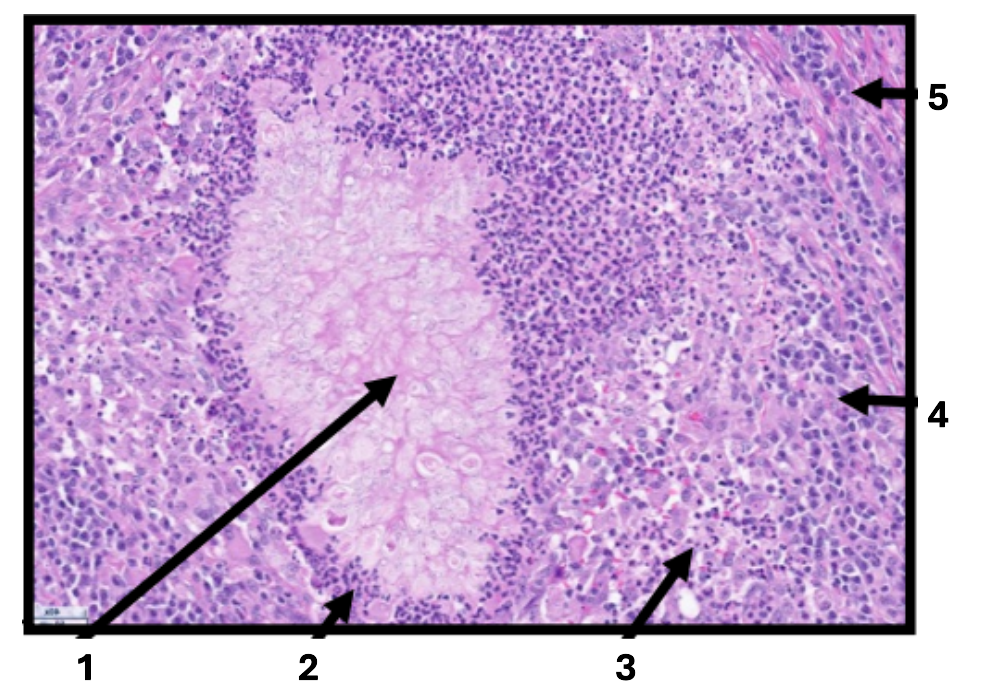
What does this image show?
macaque, spleen
1
degenerated core
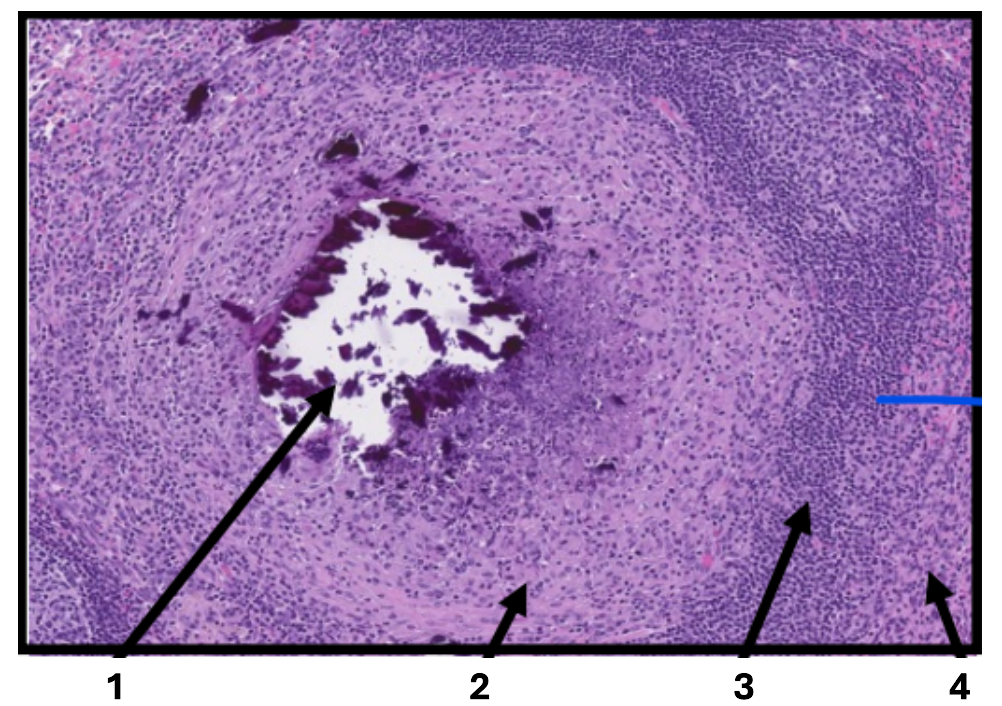
2
macrophages
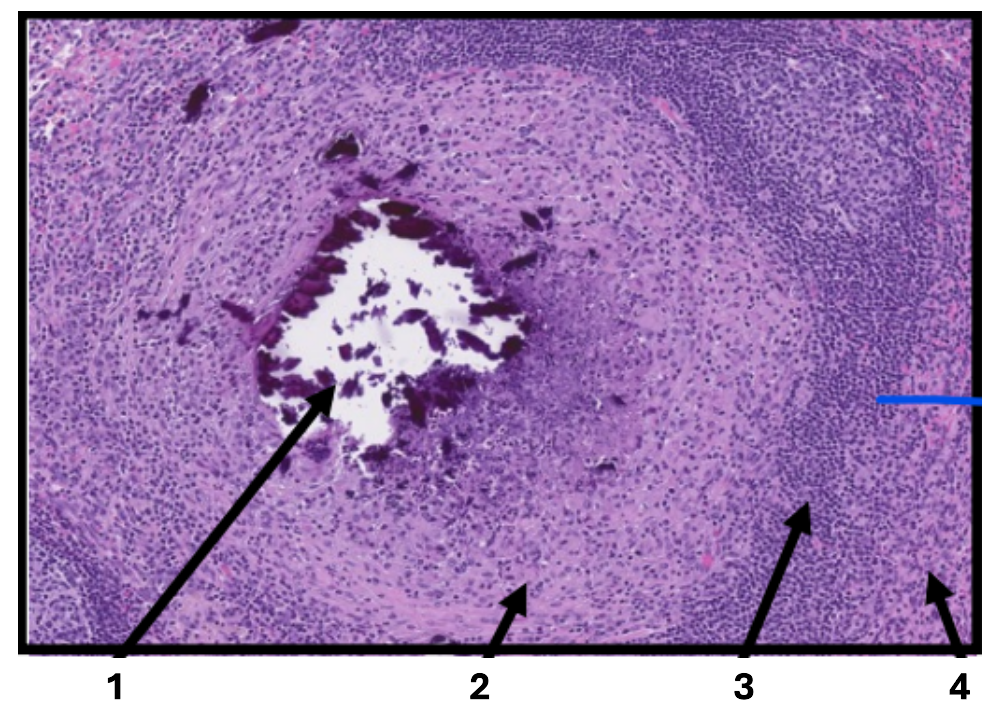
3
lymphocytes & plasma cells
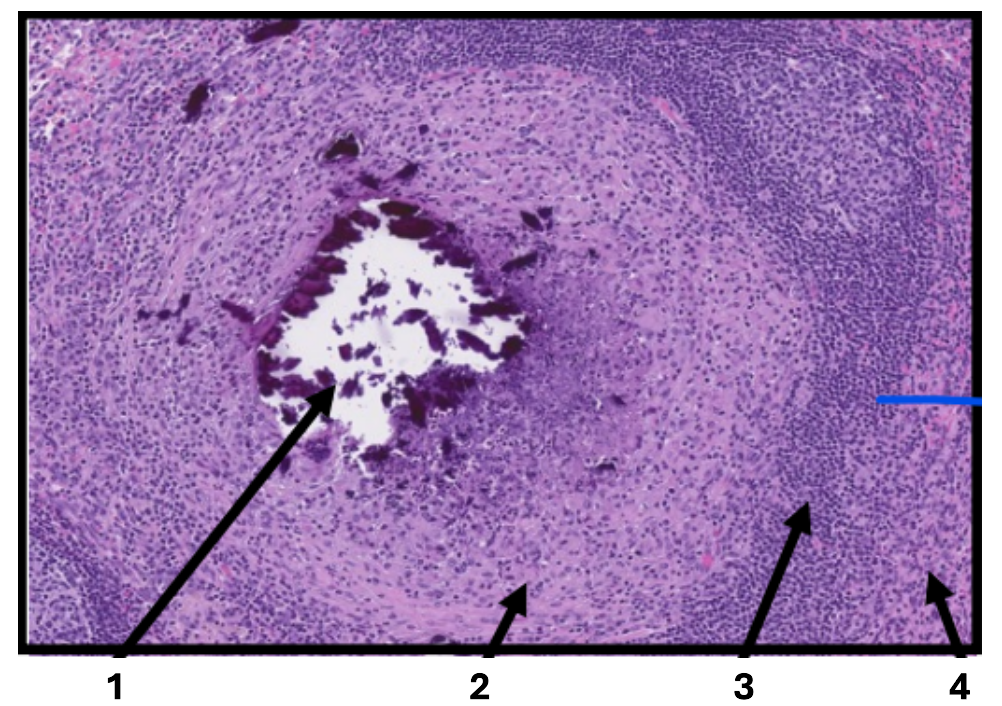
4
fibroblasts

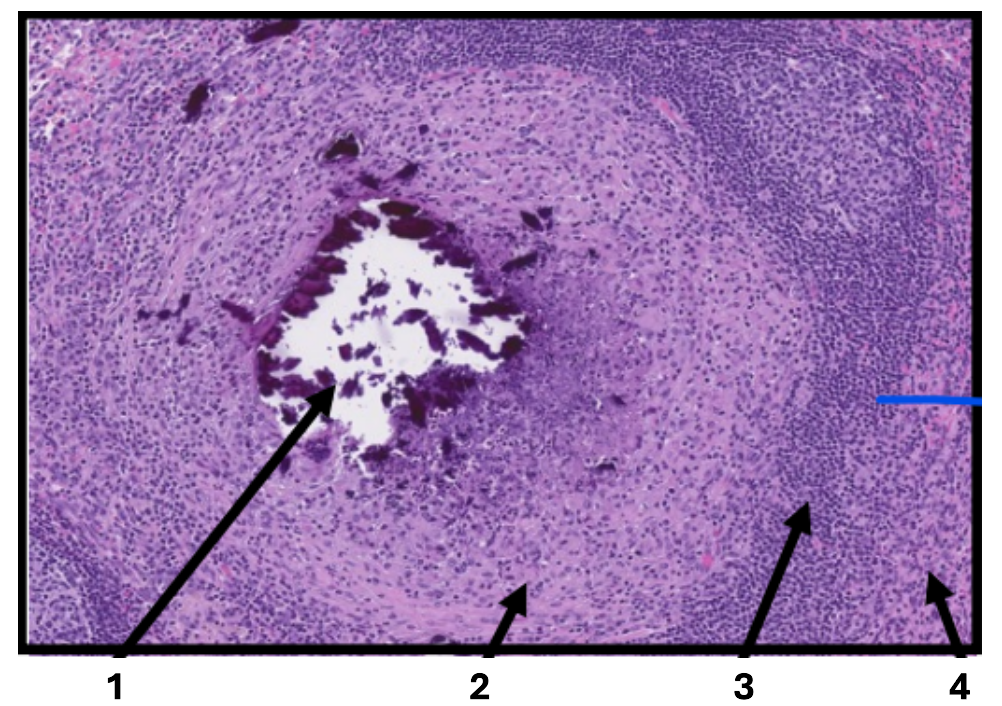
What does this image show?
horse, cutaneous mass
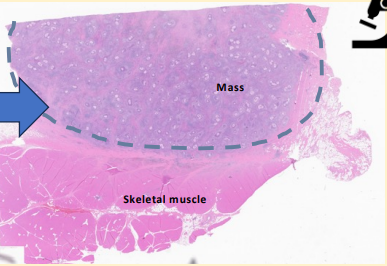
What does this image show?
pyogranuloma
1
fungi
2
neutrophils
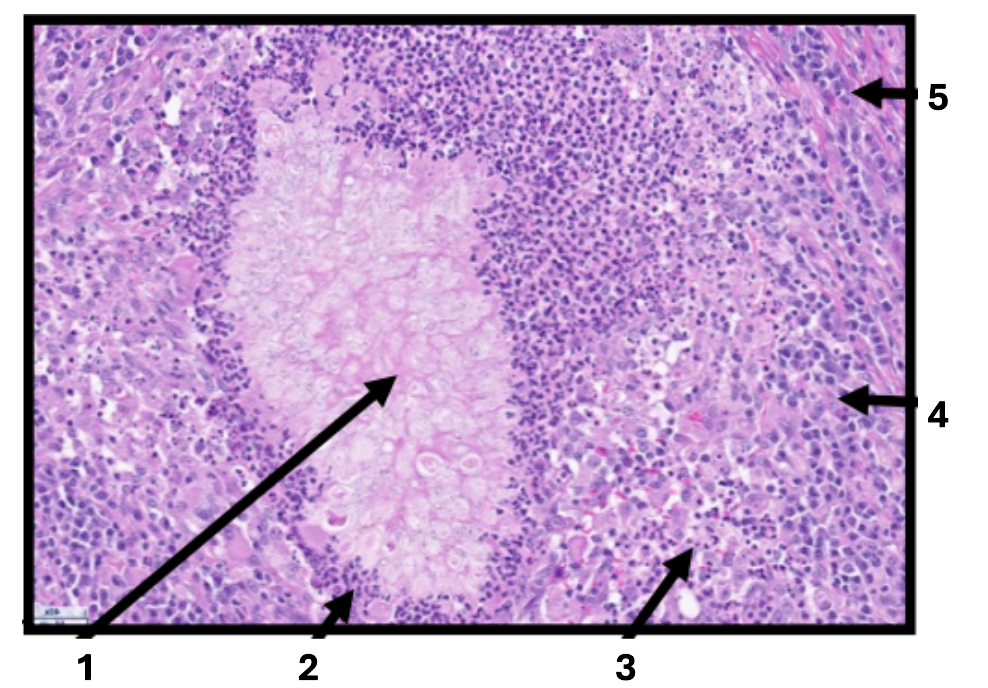
3
macrophages
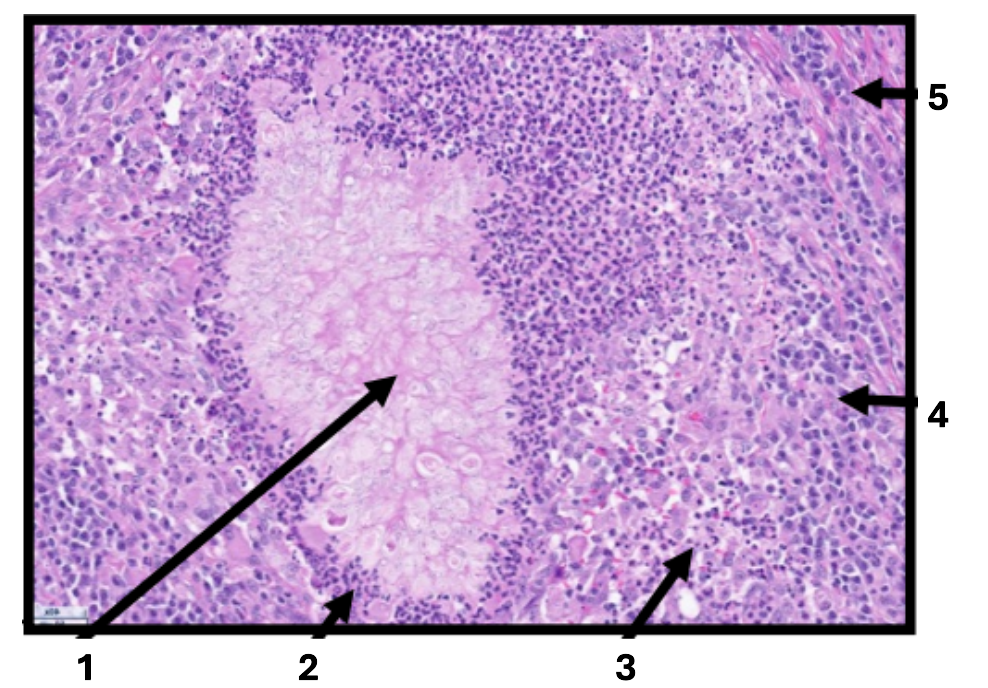
4
lymphocytes & plasma cells
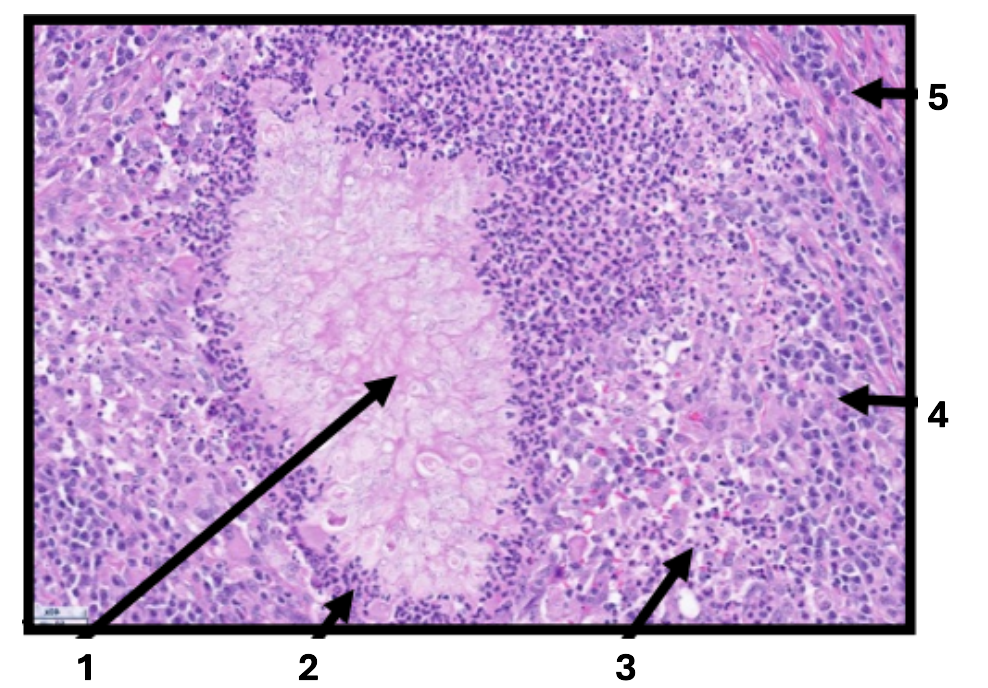
5
fibroblasts
What is eosinophilic inflammation?
chronic inflammation with predominance of eosinophils
What are common causes of eosinophilic inflammation?
parasitic infections
hypersensitivity
What features do you see under the microscope for eosinophilic inflammation?
bright eosinophil granules often mixed with mast cells and lymphocytes
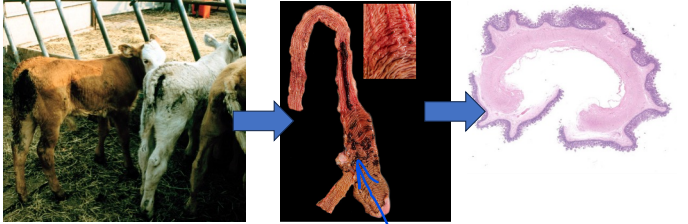
What does this image show?
beef cattle with coccidia
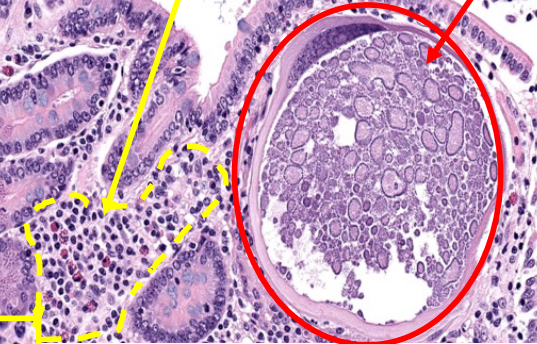
What is the yellow arrow pointing to?
inflammation
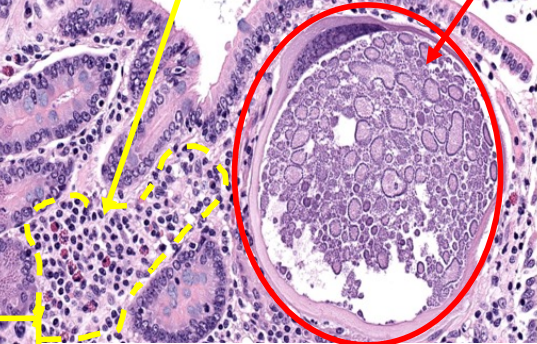
What is the red arrow pointing to?
coccidia parasite
1
lymphocytes & plasma cells
2
eosinophils
Define “chronic inflammation”
prolonged inflammation where tissue injury, attempted healing, and inflammation occur simultaneously
What are the pathological features of chronic inflammation?
infiltration by mononuclear cells
neutrophils & eosinophils
tissue destruction by inflammatory cells
Define “healing”
the body’s process of replacing damaged or lost tissue with new living tissue
What are the 2 main reactions in healing?
regeneration
repair
What is “regeneration”?
undamaged cells proliferate to replace specialised tissue
What is “repair”?
damage replaced by granulation tissue → scar formation
What are the 3 phases of healing?
inflammation
proliferation
remodelling
Does regeneration restore normal architecture and function to a tissue?
YES
Does repair restore normal architecture and function to a tissue?
NO
What does regeneration depend on?
cellular capacity to proliferate
Which cells proliferate and differentiate during regeneration?
tissue stem cells
What are labile cells?
cells that continuously proliferate at a certain rate
Name 4 examples of labile cells
squamous epithelium (of skin, mouth, vagina & cervix)
columnar epithelium ( of intestinal tract)
transitional epithelium (of urinary tract)
bone marrow cells
What are “stable cells”?
can proliferate but don’t normally do so
Name 3 examples of “stable cells”
liver hepatocytes
alveolar cells of lung
epithelium of kidney tubules
What are “permanent cells”?
neurons
skeletal & cardiac muscle
What is scar tissue made of?
connective (fibrous) tissue
When is scar tissue formed?
when there’s loss or limited proliferation of parenchymal cells & if the supporting structures of the tissue (stroma) are severely damaged
What does scar form from?
maturation of granulation tissue
What is granulation tissue?
network of new blood vessels and collagen that fills a wound
What phase may precede inflammation?
haemostatic phase
Why does the haemostatic phase occur?
if vasculature is injured
What happens during the haemostatic phase?
vasoconstriction
aggregation of thrombocytes → platelet plug
fibrin mesh formation → clot → scaffold for healing
What occurs during the inflammation stage?
initial stage where body sends cells to the injury site, causing symptoms like pain, swelling and redness as part of the natural healing response
What growth factors do M2 anti-inflammatory release?
Transforming Growth Factor (TGFB)
Endothelial Growth Factor (VEGF)
What do M2 macrophages do?
bridge inflammation & repair
What is proliferation?
new tissue (collagen & blood vessels) is laid down to replaced damaged area
tissue matrix is formed
reepithelization occurs at same time
What cells does proliferation involve?
epithelial/parenchymal cells
endothelial cells
fibroblasts
What do epithelial/parenchymal cells do during proliferation?
restore function
What do endothelial cells do during proliferation?
proliferate to form new blood vessels
What do fibroblasts do during proliferation?
lay down collagen that form the stroma or scar
What is proliferation controlled by?
cell cycle
What do growth factors do?
stimulate proliferation
What are growth factors produced by?
macrophages
epithelial cells
fibroblasts
During proliferation, what happens to epithelium adjacent to the wound?
undergoes activation and proliferation
During proliferation, what happens to the basement membrane?
provides scaffold to support cell migration into damaged area
angiogenesis
process of new blood vessel development from existing vessels
What happens to endothelial cells during angiogenesis?
endothelial cells grow from older intact blood vessels that branch out, form anastomoses with other vessels, and restore blood flow
What does granulation tissue contain?
proliferating fibroblasts
loose collagen
new blood vessels
scattered chronic inflammatory cells
What part of the wound does granulation tissue grow from?
base of wound
What size wound can granulation tissue fill?
ANY