Imaging the retina
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
What are the different methods of retinal imaging?
- photography
- widefield imaging
- autoflourescence
- angiography (FA and ICG)
- OCT
What is the advantage of taking a retinal photograph with the eye dilated?
- increased contrast
- increased quality
How many degrees can a standard camera allow for capture?
~20 to 50 degrees images of the retina
how many degrees can a wide field camera allow for capture?
up to 200 degrees images of the retina
What are retinal photographs used for?
- to detect, diagnose and monitor eye conditions (e.g., AMD, retinal detachment, retinal vascular diseases etc.)
Filter to view blood vessels
- red free , able to see more vessels
what is a pseudo wide field image?
- taking multiple fundus photographs using different fixation points but there can be problems aligning the photographs with each other
Standard Wide field imaging degrees
30-50 degrees
45 degrees in some extent
What is the optos machine?
- wide field imaging
- scanning laser system
- uses 2 wavelengths which penetrates the retina at different depths
- can obtain a 130 degree field image (good for documenting peripheral pathologies)
- pupil dilation not required but advised to obtain the best image
- an optional 488nm blue laser can be used for fluorescein angiography
What are the 2 lasers of the optos machine?
532nm green laser: penetrates retina only and allows the viewing of the retina and anterior RPE
633nm red laser: penetrates through the choroid and allows viewing of the posterior RPE and choroid
- the red and green images are superimposed to produce a pseudo colour image
What are the optics of the optos machine?
- uses an ellipsoid mirror to create images of the peripheral retina
- ellipsoid mirror contains 2 focal points
- laser of the optos is directed through one of the focal points, while the patients eye is positioned so that the second focal point is located inside the patients eye creating a large scan angle
- if the patient has steady fixation and a dilated pupil, imaging out to the ora serrata is possible
Optos vs standard fundus photograph
- optos able to image 200 internal degrees
- whereas standard is 5-15%
What is retcam?
- wide field imaging
- used in neonates and is the standard screening tool for retinopathy of prematurity in the UK
- can obtain a 130 degree field image
research findings of the screening of diabetic retinopathy 1991
introduced imaging of DR in the retinal periphery by obtaining seven standard fields.
By combining these 30-degree images, a montage visualizes about 75 degrees of retina.
research findings of the screening of diabetic retinopathy filberg 2003
They reported that ultra-wide-field imaging had poor sensitivity and specificity compared to clinical examination in the diagnosis of diabetic retinopathy.
research findings of the screening of diabetic retinopathy wessel 2012
Ultra-wide-field fluorescein angiography imaged:
3.9x more nonperfusion,
1.9x more neovascularization,
3.8x more panretinal photocoagulation than the conventional seven standard fields.
In fact, in 10% of eyes, ultra wide-field imaging demonstrated peripheral retinal pathology that was not seen with traditional fundus photographs.
What are limitations of optos
Not possible to image the entire peripheral retina.
Optos assumes that it can gain a 200-degree internal image
based on the assumption that the radius of curvature of the eye is 11mm and that the ora serrata is located at an internal angle of 230 degrees
False colour image can be hard to interpret and a high level of training is required to obtain good images
Low resolution in the posterior pole, unlike a standard fundus camera or other imaging systems (OCT, confocal SLO)
Fails to image the superior or inferior peripheral retina more frequently than the temporal or nasal retina (lids).
Other image artefacts are introduced by IOLs + clarity of the ocular media
Image distortion therefore the measurement distances displayed on an image may not correspond to the actual dimensions of the eye
How is retinal photographs taken
Non invasive but needs dilation sometimes
Retinal photographs colour
Pigmentation changes - haemorrhages , drusen,detachments and alterations in pallor
Monochromatic images - retinal photographs
useful for assessing the superficial retinal vasculature
as it provides a much improved contrast of vessels compared to their surrounding tissue.
Retinal photographs- colour to chromatic
can provide some information on
relative location (depth) of a lesion observed.
Retinal photographs- 3d images
- an produce stereopic images
- can see ares that have lifted
Retinal photographs - wide field imaging
allows for a good overview of the entire retina but (depending on the device used) lacks the true colour representation of a colour photograph as it is
obtained by scanning laser methods (Optos and Heidelberg devices).
Diabetic retinopathy Oliver 2010
Found peripheral vessel leakage present as frequ as neovascularization (41% of eyes) + less freq than peripheral nonperfusion (54%) or macular oedema (57%).
Direct relationship btwn presence of peripheral vessel leakage + presence of neovascularisation + peripheral nonperfusion.
Diabetic retinopathy muqit
Wide-field angiography facilitates treatment of proliferative DR w/ targeted laser photocoagulation.
What are the limitations of optos imaging?
- not possible to image the entire peripheral retina (optos assumes that it can gain a 200 degree internal image based on the assumption that the radius of curvature of the eye is 11mm and that the ora serrata is located at an internal angle of 230 degrees)
- the false colour image can be hard to interpret and a high level of training is required to obtain good images
- low resolution in the posterior pole, unlike a standard fundus camera or other imaging system
- optos system fails to image the superior or inferior peripheral retina more frequently than the temporal or nasal retina. other image artefacts are introduced by intraocular lenses and clarity of the ocular media
- image distortion and therefore the measurement distances displayed on an image may not correspond to the actual dimensions of the eye
What is one of the main substances in the retina causing autofluorescence?
- lipofuscin
Formed from phagocytosed PR outer segments stored in liposomes.
Lipofuscin autofluoresces at ~500–800 nm.
After excitation lipofuscin spontaneously releases a photon of light of a longer wavelength than the one used for excitation.
What does hyperfluorescence mean?
- an excess of lipofuscin
What does hypofluorescence mean?
it can either mean that RPE cells are absent OR LF disappearing
What wavelength is used for autoflourencence
- blue and green can be used
- both provide same information
- green longer wavelength so less absorption by lens , penetrates slightly deeper. , better macular view
is lipofuscin the only molecule to fluoresce in the retina?
no, there are others too but lipofuscin has been particularly linked with AMD
What other molecules/ cells can be visualised by autofluorescence?
Melanin can also be visualized by autofluorescence.
Req’s near-infrared wavelength (~790 nm, just below human detection).
Melanin distribution provides different clinical info on disease stage compared to lipofuscin.
Fundus autofloresence - wavelength.
Shows liposfuscin and RPE changes at 500-800 ( short and medium )
Optos = 532nm
Optos detection= 570-780nm
What is angiography?
- an imaging technique which enables visualisation of the lumen of blood vessels with particular interest in the arteries and veins
What was fluorescein first synthesised?
in 1871
- first used intravenously in 1955
- 1960 the technique of fluorescein angiography was developed
What are the biophysical properties of fluorescein?
- maximum fluorescence at a pH of 7.4
- up to 80% is bound to protein
- there is no firm binding with vital tissues
- rapid diffusion through intra and extra cellular spaces
- eliminated rapidly through the liver and kidneys over a 24 to 36 hour period
- stains skin and mucous membranes which can be yellowish for 24 to 36 hours
- creates false positive results in urine tests which measure sugar levels
What are the biophysical properties of fluorescein in the eye?
- diffuses freely in the eye through the choriocapillaris, Bruch's membrane, the optic nerve and sclera
- does not diffuse through retinal blood vessels,RPE or larger choroidal BV’s
What is the blood retinal barrier?
Physiological blood-retinal barrier exists at the endothelium + basement memb of retinal capillaries.
Prevents dye leakage in normal conditions, creating clear retinal vessel imaging.
Endothelial cells have tight junctions that normally block fluorescein leakage.
What are the side effects of FA?
- nausea in 5 to 15 % of patients
- ithcing
- fainting
- thromophlebitis (inflamed veins due to blood clottting)
1 in 100000 risk of anaphylactic shock
What does the time interval between the injection of the dye into systemic circulation and its appearance in the retina depend on?
- age of patient
- their cardiovascular status
What is the typical time interval?
10 to 15 seconds
-dye enters eye from ophthalmic artery into the central retinal artery
or into choroidal circulation via the short posterior ciliary arteries.
Because the path to the ciliary arteries is shorter than to the central retinal artery,
the dye will reach the choroidal circulation first
What are the 2 phases in the principles of fluorescein angiography?
- excitation phase
- emission phase
What is the excitation phase of fluorescein angiography?
- the exciter (blue filter_ is placed in front of the light source of the camera system so that the dye fluoresces in the eye
- not all of the radiation is used and the residual radiation is reflected from or transmitted through the eye. the residual radiation needs to be removed from the optical system to avoid over exposure
What is the emission phase of fluorescein angiography?
- a yellow green barrier filter
prevents the residual exciting radiation from causing exposure on the imaging system.
it transmits only the wavelength of light that is evident as fluorescence
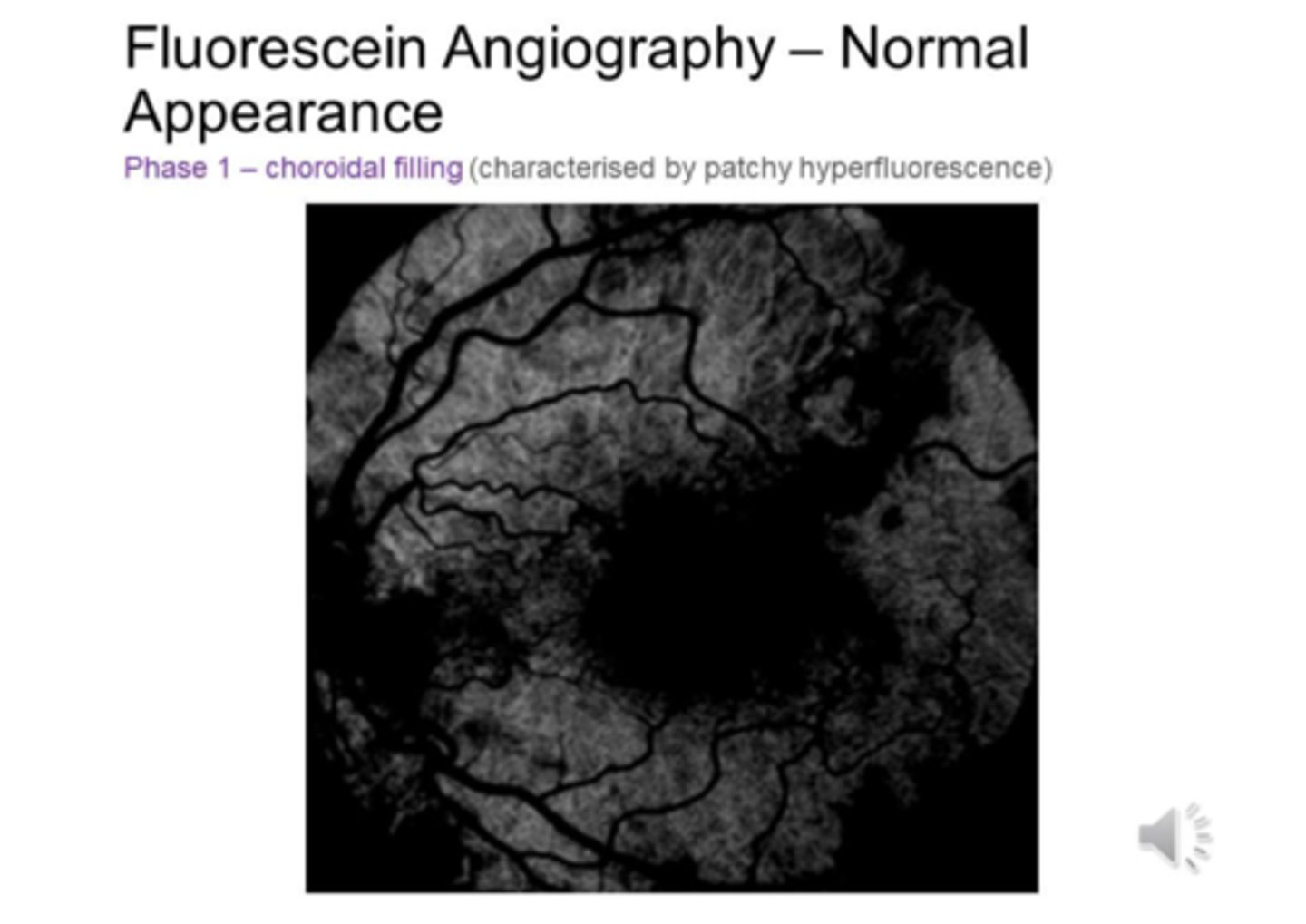
What is phase 1 of FA?
CHOROIDAL FILLING (characterised by patchy hyperfluorescence)
What is phase 2 of FA?
RETINAL ARTERIAL FILLING
What is phase 3 of FA?
CAPILLARY AND EARLY VENOUS PHASE
What is phase 4 of FA?
MID RETINAL VENOUS PHASE
What is phase 5 of FA?
LATE VENOUS PHASE
What is phase 6 of FA?
DELAYED PHASES
- As the dye is recirculated it becomes diluted and the fluorescein gradually fades becoming totally absent after about 5 to 10 mins except for minimal staining in the optic disc and sclera
What is autofluorescence?
seen in pre injection images and is caused by highly reflective substances such as optic disc drusen
What is pseudofluorescence?
when there is overlap between the spectra of the light transmitted by the barrier and exciter filters
define blocking defects?
- where the normal underlying fluorescence is blocked by a barrier to light (e.g., from blood, pigment, exudate etc.)
define filling defects?
areas of hypofluorescence due to ischaemia or occlusion of normal blood flow
define pooling?
the accumulation of fluorescein in an anatomic space
define leakage?
hyperfluorescence that increases in intensity or size from the early to late phases of the angiogram
define staining?
when dye leaks into the tissues and is seen as a late hyperfluorescence
What are the advantages of FA?
- Allows simultaneous assessment of anatomy and function of the retinal and choroidal vasculature
- precisely defines the location of pathologic changes enabling their treatment avoiding normal areas
What are the disadvantages of FA?
- it cannot precisely image the choroidal circulation
- although relatively safe, it is an invasive procedure
- it cannot quantify macular oedema (oct is used for this)
What is indocyanine green angiography (ICG)?
- USES indocyanine green
- it is a water soluble tricarbocyanine dye
- pH is 5.5 to 6.5
- absorbs and fluoresces in the near infrared range 790 to 805nm
- high resolution required because the fluorescence efficacy is only 4% that of fluorescein dye
- 98% protein bound after injection which limits diffusion of the dye through the small fenestrations of the choriocapillaris.
Thus the retention of ICG in the choroidal circulation combined with its low permeability makes ICG angiography ideal for imaging choroidal circulation which is a disadvantage of FA
- metabolised in liver
- excreted into bile
What are the advantages of using indocyanine green angiography?
- ability to fluoresce better through pigment, fluid, lipid and haemorrhage than fluorescein dye
- better at detecting abnormalities such as choroidal neovascular membrane that could be blocked by a subretinal haem on a fluorescein angiogram
What are the indications for ICG angiography?
- CNV
- Pigment epithelial detachment
- central serous chorioretinopathy
- intraocular tumours
- inflammatory conditions of the choroid