SECTION 02: MECHANICS OF BREATHING
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
By the end of Section 02, you should be able to:
Describe the different pressures involved in the mechanics of breathing.
Applying the law of Laplace, describe why alveoli do not collapse.
Describe the pressure changes that occur to enable inhalation and expiration.
Describe the pressure-volume relationship of the lung.
🔢 Key Equation for Air Flow
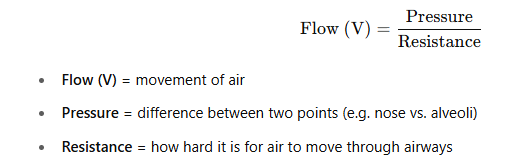
🎯 What Drives Air Flow?
A pressure gradient (difference in pressure) between:
The nose and the alveoli
🫧 When Does Air Flow In?
Alveolar pressure < Nose pressure
Air flows into alveoli (inhalation)
💨 When Does Air Flow Out?
Alveolar pressure > Nose pressure
Air flows out of alveoli (exhalation)
🧱 What the Pressure Must Overcome:
Elastance = Stiffness of lungs/chest (how stretchy they are)
Resistance = Friction in the airways
Inertia = Tendency of tissues/air to resist changes in motion (minor)
📚 Respiratory Mechanics =
How pressures, volume, and resistance interact to allow breathing
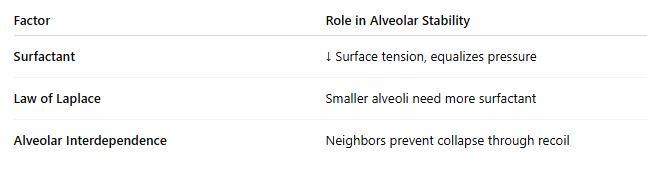
🌬 PRESSURES IN THE RESPIRATORY SYSTEM
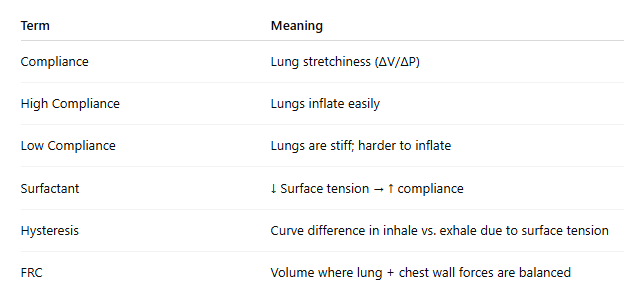
🌎 1. Atmospheric Pressure (PB)
Also called: Barometric Pressure
It’s the air pressure around us from the atmosphere
At sea level = 760 mmHg
➝ In respiratory equations, we treat it as 0 cm H₂OWhy? Because it’s the reference point (same at nose/mouth and alveoli at rest)
🫁 2. Alveolar Pressure (PA)
Also called: Intrapulmonary Pressure
Pressure inside the alveoli
At end of a normal breath (inspiration or expiration): PA = 0 cm H₂O (same as atmosphere)
🟦 3. Pleural Pressure (Ppl)
Also called: Intrapleural Pressure
Pressure in the pleural space (between lungs and chest wall)
Normally around: -5 cm H₂O
Why negative?
Lungs want to collapse inward
Chest wall wants to expand outward
Creates a slight suction effect between them
↔ 4. Transpulmonary Pressure (Ptp)
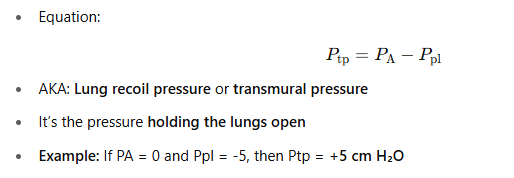
Intrathoracic Pressure:
➝ Pressure inside the thoracic cavity, closely matches pleural pressure
🧪 Summary Table:
🧪 Units Used in Respiratory Physiology
📏 1. mmHg (millimeters of mercury)
📌 Key Conversion:
1 mmHg = 1.36 cm H₂O
So 5 cm H₂O ≈ 3.7 mmHg
🌀 3. Pressure Measurements Are Relative
Respiratory pressures are measured relative to atmospheric pressure (0 cm H₂O)
Example:
If atmospheric pressure = 1034 cm H₂O
And alveolar pressure = 1029 cm H₂O
Then: Alveolar pressure = -5 cm H₂O
❗ Note:
“Negative pressure” doesn't mean less than zero — it just means lower than atmospheric pressure
Manometer
Device that measures pressure (like a ruler for gas or fluid pressure)
🫁 Elastic Recoil of the Lungs
🔁 What Is Elastic Recoil?
The lungs have a natural tendency to deflate after they’ve been stretched (like a balloon shrinking after letting go).
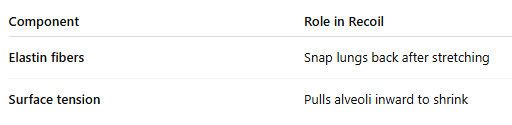
This is due to:
Elastin fibers
Surface tension in alveoli
🧵 1. Elastin Fibers
Found in lung connective tissue
Arranged like a mesh to allow stretching
When stretched during inhalation, they snap back to help push air out
💧 2. Surface Tension
Caused by a thin liquid lining inside the alveoli
Makes up about 70% of the recoil force
Why?
a) Resists Stretching
Water molecules stick together and don’t like being pulled apart
Makes alveoli resist expanding
b) Wants to Shrink
Water molecules pull inward, trying to shrink the alveoli
Without opposing forces (like inhalation), alveoli would collapse and expel air
⚖ Balance of Forces (Shown in Image)
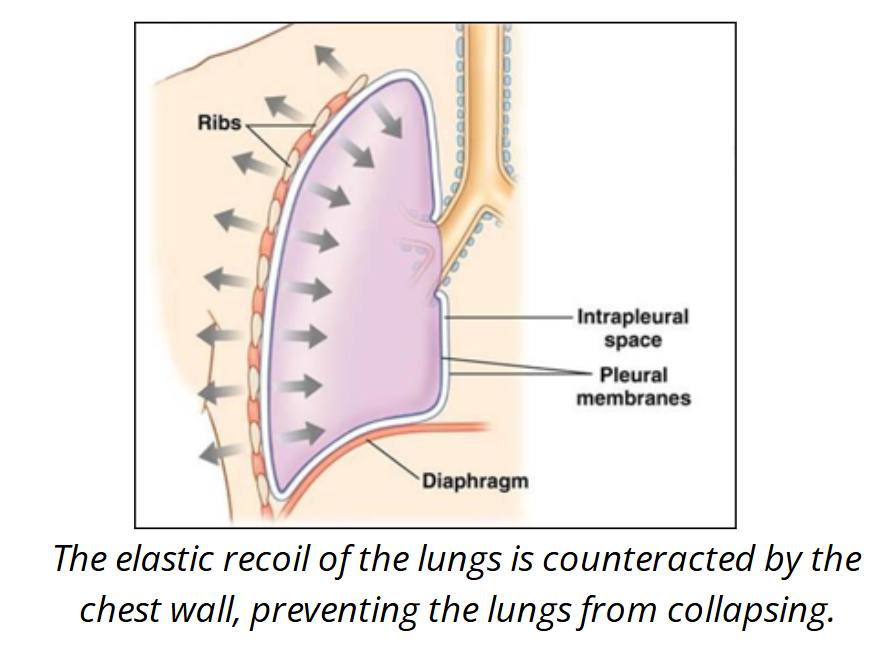
Lungs want to collapse inward
Chest wall wants to spring outward
The pleural space and fluid in it balance these forces, preventing lung collapse
💡 Summary:
🫁 ALVEOLAR STABILITY: Why Alveoli Don’t Collapse
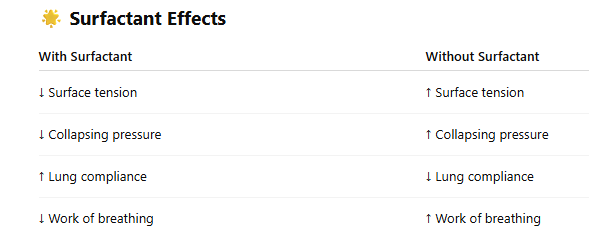
💧 1. Pulmonary Surfactant
What is it?
A mix of lipids + proteins made by type II alveolar cellsWhat does it do?
Spreads over the alveolar lining
Reduces surface tension by separating water molecules
Makes lungs easier to expand (↑ compliance)
Prevents alveoli from collapsing (especially small ones)
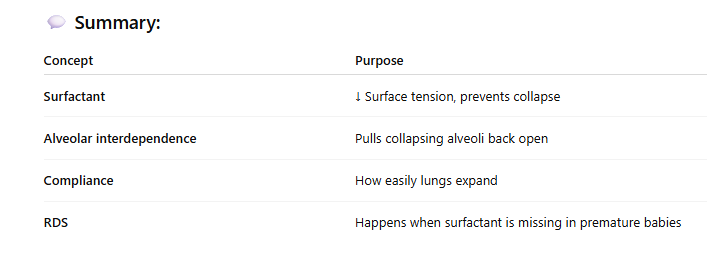
🔄 2. Alveolar Interdependence
What is it?
Alveoli are connected to each other by elastic tissueHow it works:
If one alveolus starts to collapse, neighbors stretch and pull it openHelps stabilize the lung structure
🌟 Surfactant Effects
👶 Clinical Application: Respiratory Distress Syndrome (RDS)
🍼 In Premature Babies:
Surfactant production begins ~24 weeks gestation
Sufficient levels by ~35 weeks
🚨 If born early (<35 weeks):
Not enough surfactant
Alveoli stick together & collapse
Baby’s lungs are less compliant
Breathing becomes very hard
Condition = Neonatal Respiratory Distress Syndrome (RDS)
Surfactant
Surfactant is a fluid made by type II alveolar cells in the lungs.
It’s a mix of lipids and proteins that:
Reduces surface tension in the alveoli
Prevents alveoli from collapsing after exhalation
Makes it easier to breathe by increasing lung compliance
Without surfactant, breathing would require much more effort, especially in newborns.
🫁 Symptoms of RDS
Labored breathing
Weak cry
Blue skin tone (cyanosis)
May require surfactant therapy + oxygen
💬 Summary:
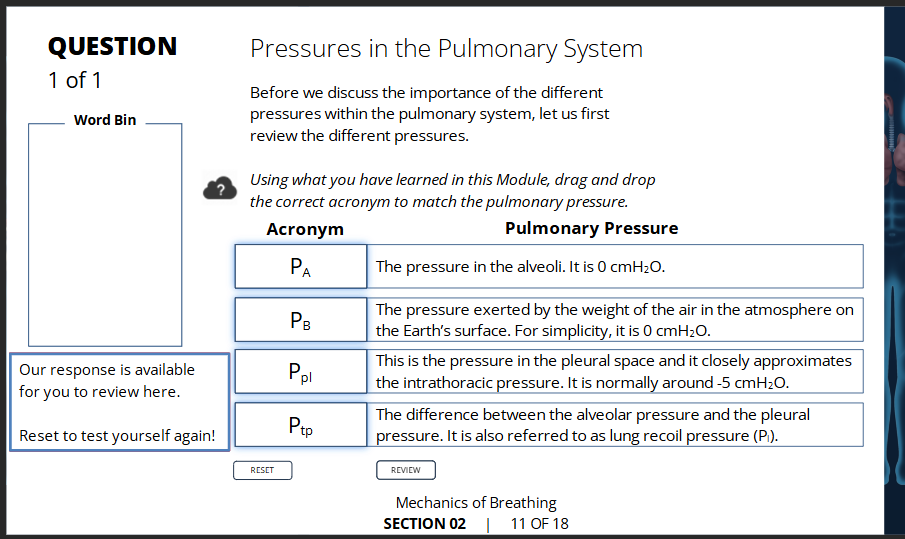
📏 Law of Laplace (for alveoli)
🧪 The Formula:
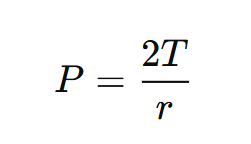
🧠 What the terms mean:
P = Collapsing pressure inside the alveolus
T = Surface tension
r = Radius of the alveolus
🔁 How It Works:
The Law of Laplace - 💡 Why this matters:
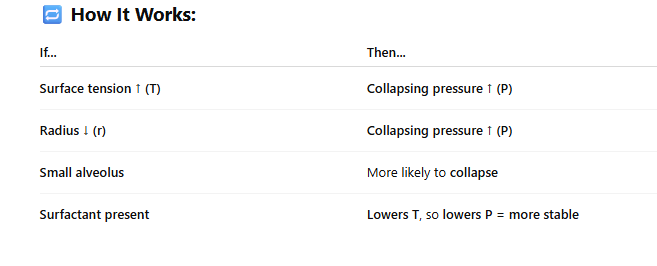
Smaller alveoli are more at risk of collapsing due to higher pressure.
Surfactant reduces T more in small alveoli to equalize pressure across all alveoli.
Keeps alveolar sizes stable and prevents collapse.
🫁 Summary:
The Law of Laplace explains why smaller alveoli need more help (from surfactant) to stay open.
Activity
Activity pt 2
🧮 Law of Laplace Equation
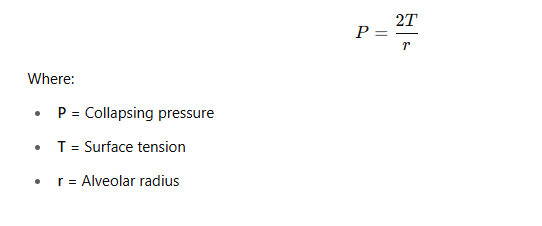
❓ Question: Compare Collapsing Pressure
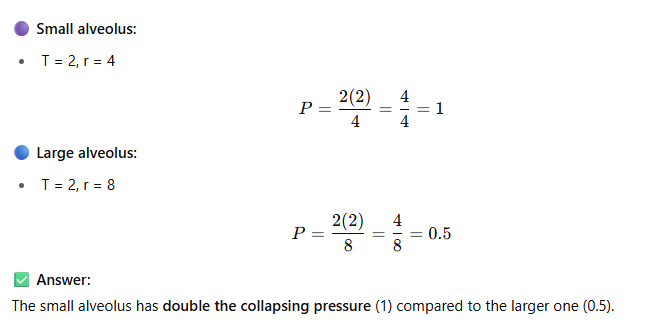
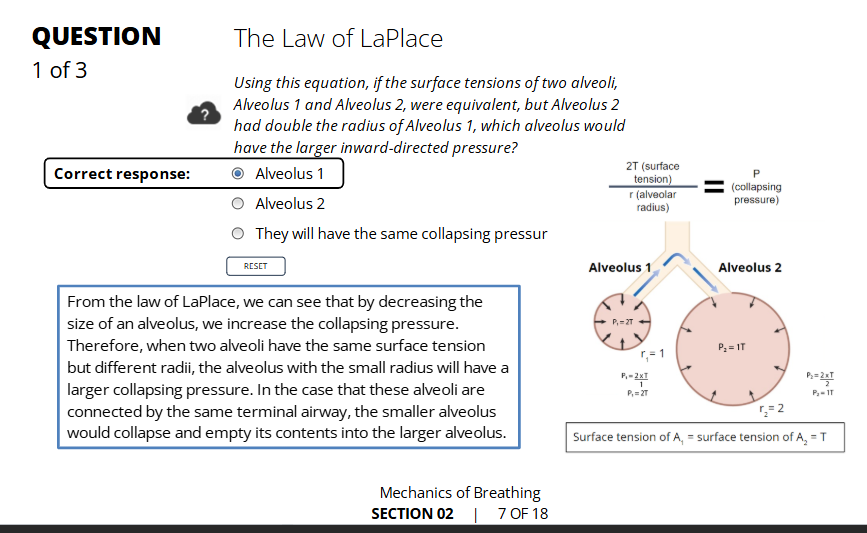
💧 What Is Pulmonary Surfactant?
A lipid + protein mixture secreted by type II alveolar cells
Spreads over the alveolar surface
Reduces surface tension by breaking water-water bonds
Makes lungs more compliant and prevents alveoli from collapsing
🔄 How It Prevents Collapse
Each alveolus adjusts how much surfactant it makes
Smaller alveoli get more surfactant → greater reduction in surface tension
This helps equalize collapsing pressure across alveoli of different sizes
🧱 Other Factor: Alveolar Interdependence
Alveoli are linked together by elastic tissue
If one alveolus starts to collapse, neighboring alveoli pull it back open
This supports alveolar structure
🫁 Summary Table
Activity
💨 Alveolar Pressure (PA) and Airflow
🧠 Key Idea:
Air flows from high pressure → low pressure
So to breathe in, PA < atmospheric pressure
To breathe out, PA > atmospheric pressure
🌍 Atmospheric Pressure
Treated as 0 mmHg (a fixed reference point)
📐 Important Equation:
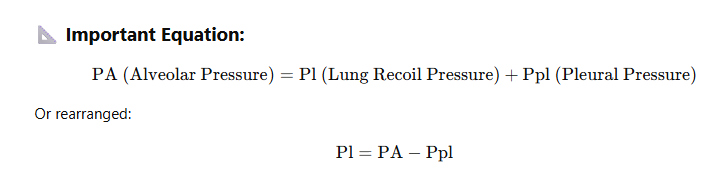
🫁 What Controls PA?
Lung recoil pressure (Pl) is based on lung volume
➝ You can’t change Pl directly to change PASo, you must change pleural pressure (Ppl) to change PA
💪 How Do We Change Ppl?
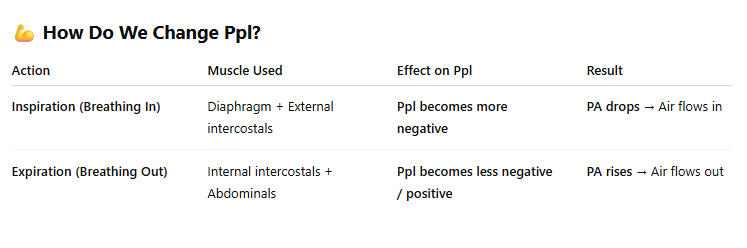
📌 Summary:
To change alveolar pressure (PA) and move air:
You must change pleural pressure (Ppl)
And that’s done by using your respiratory muscles
🫁 Inhalation and Exhalation = Pressure-Driven Airflow
🌬 Before Inhalation (End of Expiration)
🫧 Inhalation Begins
🛑 Inhalation Ends
Inspiratory muscles stop contracting
Lung recoil catches up to Ppl
→ PA rises to match atmospheric pressure
→ Airflow stops
💨 Exhalation Begins
Inspiratory muscles are fully relaxed
Lung recoil now greater than Ppl
→ PA becomes positive
→ Air flows out of alveoli
🔁 Active Exhalation (Extra Effort)
Happens during exercise, coughing, etc.
Expiratory muscles contract
→ Increases Ppl and PA
→ More air pushed out
🌬 Onset of Inhalation
🧘 Before Inhalation Starts
Alveolar Pressure (PA) = Atmospheric Pressure
→ No airflow
💪 Inspiration Begins
Inspiratory muscles contract
→ Pleural Pressure (Ppl) becomes more negative
→ Thoracic cavity expands
🫁 What Happens Next?
Alveolar pressure (PA) drops slightly (≈ -1 cm H₂O)
→ Creates a pressure gradient
→ Air flows into alveoli
📈 Airflow Continues Until...
Alveolar pressure rises (as air fills lungs)
When PA = atmospheric pressure again
→ Inhalation ends
📐 Extra Note:
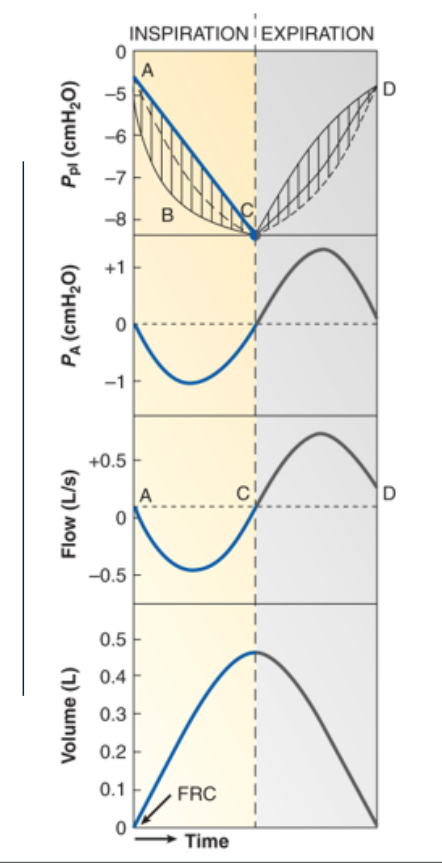
The drop in pleural pressure is not linear
At the beginning of inhalation, there is increased resistance to overcome
🔁 Graph Quick Guide:
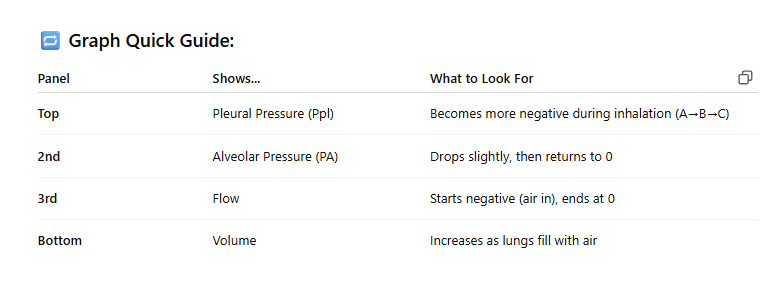
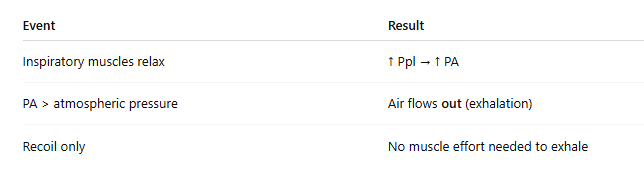
💨 Onset of Exhalation
🛑 End of Inhalation
Inspiratory muscles relax
No more effort to expand the chest
🔁 What Happens Next?
Pleural pressure (Ppl) becomes less negative
→ Alveolar pressure (PA) increases
→ Now PA > atmospheric pressure
🌬 Air Flows Out
Air flows out of the lungs
→ Until PA = atmospheric pressure
→ At this point, airflow stops
❌ No Expiratory Muscles Needed
Normal exhalation is passive
Caused by elastic recoil of the lungs and chest wall
🧠 Summary:
💨 Active Exhalation
🧘♀ At Rest
Expiration is passive (lungs recoil, no muscle use)
🏃♂ During Exercise or Forceful Breathing
Active exhalation helps push air out faster and deeper
Expiratory muscles contract to increase pleural pressure (Ppl)
This helps push more air out of the lungs
💪 Muscles Involved
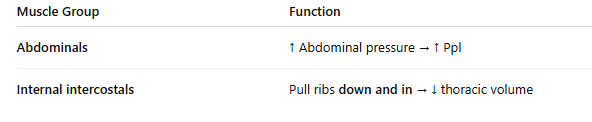
📉 Effect on Lung Volumes
Lowers End-Expiratory Lung Volume (aka FRC)
→ Increases Tidal Volume (more room to inhale)
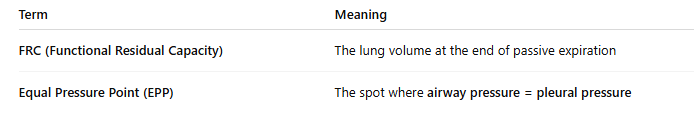
⚠ During Forced Expiration
As air flows out, pressure drops due to resistance
Eventually reaches the Equal Pressure Point (EPP):
Airway pressure = Pleural pressure
Beyond this: airway compresses
→ Transpulmonary pressure (Ptp) becomes negative
→ Further pressure does NOT increase flow
📌 Key Definitions:
🧠 Summary:
Active exhalation = muscle-driven, used during exercise or forced breathing
Flow limit happens at the EPP, where trying harder doesn’t help
💨 Active Expiration & Lung Collapse Prevention
📐 Key Formula:
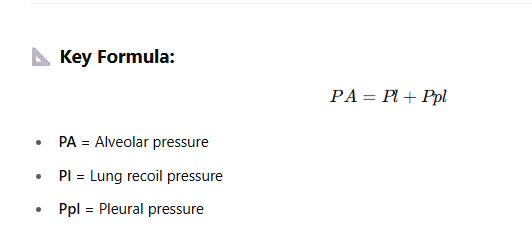
❓ Why Don’t Lungs Collapse in Active Expiration? (3 reasons)—> ✅ 1. Alveolar Pressure Rises with Pleural Pressure
During active expiration, Ppl becomes positive (due to abdominal muscle contraction)
But PA also increases (since PA = Pl + Ppl)
So alveoli stay inflated → no collapse
✅ 2. Airway Compression Limits Flow
High Ppl compresses airways, increasing resistance
Reaches Equal Pressure Point (EPP)
Beyond that point, more pressure = more compression, not more air flow
✅ 3. You Can’t Exhale Below Residual Volume
Because of airway compression, you can’t push all air out
Prevents lungs from fully collapsing or bronchioles from shutting down
🧠 Summary:
🔄 Pressure–Volume Relationships (3 things to note) —> 📈 1. Lung Pressure (Pl)
As lung volume ↑, lung recoil pressure (Pl) ↑
Starts near 0 cm H₂O at residual volume (RV)
Increases to about +30 cm H₂O at total lung capacity (TLC)
The lungs want to deflate when stretched (positive pressure)
🧱 2. Chest Wall Pressure (Pw)
Acts like a spring:
Below 65% of vital capacity: wants to expand (negative pressure = inflating)
At 100% vital capacity: wants to collapse (positive pressure = deflating)
🔄 3. Respiratory System Pressure (Prs)
🧠 Key Concepts
🫁 Visual Notes from the Graph:
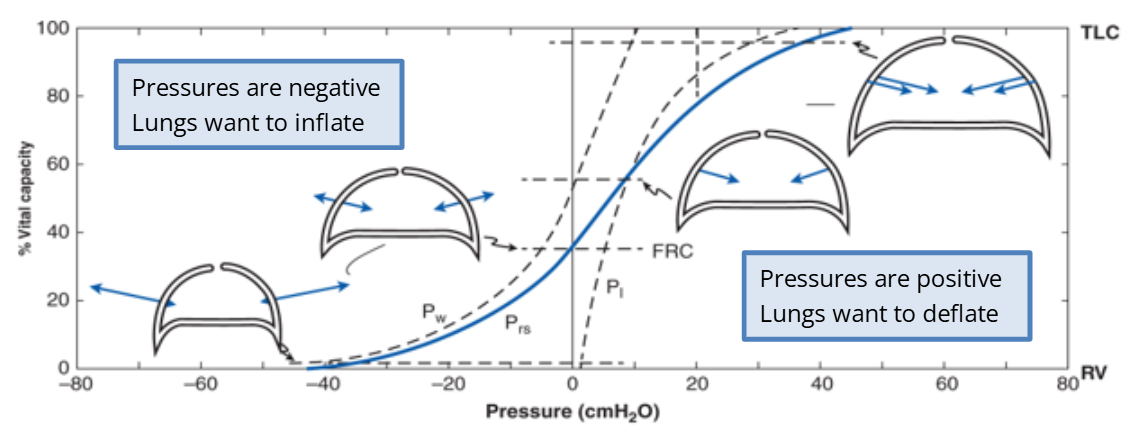
Left side = inward arrows from chest wall = inflating
Right side = outward arrows = deflating
FRC (Functional Residual Capacity) = point where lung recoil and chest wall outward force are balanced
📈 Compliance (C)
💡 Definition:
🔼 High Compliance
Lungs stretch easily
Less pressure needed to move air in/out
Found at Functional Residual Capacity (FRC)
➝ Breathing requires less effort
🔽 Low Compliance
Lungs are stiff or damaged
More pressure needed to breathe
Makes inhalation/exhalation harder
Common in lung diseases (e.g., emphysema)
🫁 Clinical Example: Emphysema
Damaged alveoli → reduced compliance
Even at FRC, breathing becomes more work
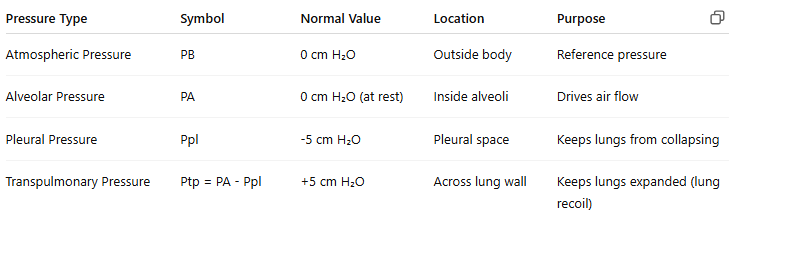
📌 Summary Table
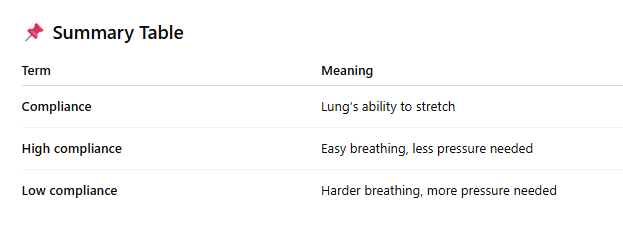
📏 What Is Compliance?
🫁 Compliance Is Greatest At...
Functional Residual Capacity (FRC)
➝ Means less effort is needed to breathe in or out at this volume
🔼 High Compliance
Lungs stretch easily
Requires less pressure to move air
Found in healthy lungs at FRC
🔽 Low Compliance
Lungs are stiff
Requires more pressure to breathe
Seen in diseases like fibrosis or emphysema
💡 What Affects Compliance?
1. Elasticity (Elastin fibers)
Lungs recoil after stretch due to elastin in connective tissue
2. Surface Tension
Water lining alveoli wants to collapse them
Surfactant ↓ surface tension → ↑ compliance
🌊 Surfactant
Made by type II alveolar cells
Reduces surface tension
Increases compliance
Makes breathing easier
🔄 Hysteresis
Pressure–volume curve is different during inspiration and expiration
Reason: Must overcome surface tension during inhalation
🤝 Lung + Chest Wall Compliance
Chest wall wants to expand
Lungs want to collapse
At FRC, these forces balance
Together, their combined compliance is lower than either one alone
🔁 Summary Table: