Bicd 140 Immunology
1/417
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
418 Terms
what are the three principles of immunity
-self vs non-self
-healthy vs sick
-primary vs secondary
self vs nonself
-the collective response upon introduction of a foreign substance is called the immune response
-generally gettin rid of non self however this can be harmful like rejecting a donor organ or overreacting to a foreign body(allergy)
healthy vs sick
immunopathology- mechanisms that eliminate pathogens can also cause tissue damage
-reason you become sick is because of the immune response(want optimal immune response not necessarily always a strong immune response)
primary vs secondary
immunity may decide individual is capable of resolving infection after one encounter or will protect from reinfection of the same pathogen(secondary/memory response)
types of infectious agents
fungus, parasites, bacteria, viruses
where do fungi replicate/propagate
extracellular
where do parasites replicate/propagate
intra and extracellular
where do bacteria replicate/propagate
both intracellular and extracellular bacteria
where do viruses replicate/propagate
intracellular
does where an infectious agent propagates mean it is always found there?
no
major disease killers
malaria, tuberculosis, and HIV
new diseases and battles
SARS, Ebola, MERS
virulence theory
-the ability of a pathogen to do damage to a host
-a pathogen is selected to carry out replication and transmission
-if it kills the host before it replicates it will die too so it doesn’t do this
-more hosts means the parasite is better transmitted
what does the most dangerous pathogen isn’t the deadliest pathogen mean?
the most dangerous pathogen makes the high die so fast(ebola) but the deadliest pathogen may have a low chance of death but causes extreme population spread and damage(COVID)
How are pathogens selected for?
-they are selected to maximize replication and transmission
-THEY ARE NOT SELECTED TO BE DESTRUCTIVE
How is the immune system selected
-it is selected to be slightly different and more effective over time
-it reacts to infection doesn’t necessarily prevent it
innate immunity
-all animals have it
-innate immunity is manifest in all cells of the body
-immediate response (fast)
-no memory response
adaptive immunity
-only in vertebrate animals
-special immune cells only(B and T cells)
-slower response
-highly specific response
what immunity is lacking if the number of microorganisms continues to increase
lacking the innate immune response
what immunity is lacking if the microorganisms increase, stall for a little bit, then increase again
lacking adaptive immunity only
ways to prevent pathogens from crossing the epithelia
mechanical, chemical, and microbiological barriers
mechanical barriers
-physical barriers(epithelial cells joined by tight junctions)
-fluid around(flow of fluid, music, food, and saliva)
chemical barriers
-primarily enzymes and PH levels
-antimicrobial peptides
microbiological barriers
non-pathogenic commensals
-ex) prebiotics in gut
-flora of the gastrointestinal tract
gut lumen commensal bacteria and antibiotics
-the commensal bacteria create a buffer of space that prevents the pathogen from reaching the body(good)
-antibiotics would kill this barrier
-therefore it is better for the body to take care of pathogen if it can before using antibiotics
where do the immune system cells originate
bone marrow
immune cell types
-neutrophils
-macrophages
-dendritic cells
-natural killer cells
neutrophils (walking bomb)
-antimicrobial proteins
-most abundant because when they kill they explode and release their DNA which traps the pathogen
macrophages(garbage collector)
-phagocytosis
-eats pathogens directly and cleans the body
dendritic cells(detectives)
-antigen presentation: presents antigen from the pathogen to the T cells
-con stimulatory signals
natural killer cells(border patrol)
-lysis of viral-infected cells
*it doesn’t kill virus it kills the cells with the virus to remove them and to prevent further damage to the body*
Main innate immune mechanisms
direct killing and accessory roles
direct killing mechanisms of the innate immune system
-phagocytosis
-secreting microbial peptides
-lysis of microbes(perforation of pathogen cell membrane through secreting complement)
accessory role mechanisms of the innate immune system
-increases pathogen uptake(opsonization)
-recruiting more immune cells(complement and chemokines)
-activating more immune cells(cytokines)
-induce systemic inflammatory responses(cytokines)
cytokines
small signaling protein molecules that are secreted by numerous cells to affect the behavior of others-allows immune cells to communicate
interleukins(IL)
group of cytokines that were first expressed in white blood cells- communication
chemokines
family of small cytokines with the ability to induce directed chemotaxis in nearby responsive cells-they are chemotactic cytokines
-direct cells to migrate to a location
process of phagocytosis
-bacteria is phagocytosed
-phagosome fuses with azurophillic and specific granules which have enzymes and change pH for degradation
-
lysis of microbes-C5b
C5b is a major component of complement that forms pores on the membrane of the pathogen that leads to lysis
what is the complement system?
A system of plasma proteins made by the liver that play multiple roles in innate immunity
-liver is making c3 and c5 all the time regardless of infection
-at the time of infection c3 binds the pathogen and is cleaved into c3a and c3b
c3a is released
c3b stays on the pathogen and codes it
essential for c5 to be cleaved into c5a and c5b
c5a is released
c5b inserts pores into pathogen to destroy it
opsonin
any molecule that enhances phagocytosis by marking an antigen for an immune response
increases pathogen uptake(opsonization)
-c3b is on the bacteria
-pathogen coded by c3b causes macrophages to produce CR1(complement receptor 1) that binds c3b and facilitates phagocytosis
recruiting more immune cells-complement
c3a and c5a that were released from complement system increase vascular permeability and recruit more immune cells-causes heat, redness, and pain
what are the 3 pathways of complement activation
-recruitment of inflammatory cells by c3a and c5a
-opsonization of pathogens, facilitating uptake and killing by phagocytosis by c3b
-perforation of pathogen cell membranes by c5b
cytokines and mannose-binding lectin and c-reactive protein
-bacteria induces macrophages to produce IL-6
-IL-6 targets the liver and causes liver to make mannose-binding lectin and c-reactive protein
-c3 recognizes certain patterns but its limited but now these two can serve as opsonin and as a complement activator to cleave c3
Three pathways complement activation
-alternative pathway
-lectin pathway
-classical pathway
*all lead to complement activation and eventually death of pathogen*
alternative pathway
pathogen surface creates local environment conducive to complement activation
-first to act
lectin pathway
mannose-binding lectin binds to the pathogen surface
-second to act
classical pathway
c-reactive protein or antibody binds to specific antigen on pathogen surface
-third to act
cytokines and activating more immune cells
-interferon responds to viral infection by inducing resistance to viral replication in cells, increases expression of ligands for receptors on NK cells, and activating NK cells to kill virus-infected cells more efficiently
TNF alpha
gets neutrophils out of the bone marrow and into the blood stream
chemokines recruiting more immune cells
-provides directional signals for migrating cells
concentration of chemokine stronger by the site of infection telling immune cells where to go
cytokines and inducing systemic inflammatory responses
-IL-1 secreted by phagocytes travels in the blood to the hypothalamus
-increases body temperature to the point set by the hypothalamic thermostat to create a fever to kill pathogen
septic shock
TNF alpha causes cells to make platelet activating factor which prevents pathogens from entering the blood
-in the extreme case this results in systemic edema followed by excessive coagulation and organs are starved and shut down
PAMPs
-pathogen associated molecular patterns
-molecules associated with groups of pathogens that are recognized by cells of the innate immune system
PRRs
-pattern recognition receptors
-innate immune system receptors that recognize different PAMPs
How can pathogens be recognized
-binding of bacteria to phagocytic receptors on macrophages induces their engulfment and degradation
-binding of bacterial components to signaling receptors on macrophages induces the synthesis of inflammatory cytokines
innate defense mechanisms of pathogens in the interstitial spaces, blood, and lymph(extracellular)
-complement system
-macrophages
-neutrophils
innate defense mechanisms for pathogens on epithelial surfaces(extracellular)
-antimicrobial peptides can be produced by skin cells
innate defense mechanisms against pathogens in the cytoplasm(intracellular)
-NK cells
innate defense mechanisms against pathogens in vesicles(intracellular)
-activated macrophages
different types of PRRs
-Toll-like receptors
-mannose receptors
-scavenger receptors
-nod-like sensors
-CARD-family sensors
what are nod-like sensors
for intracellular bacteria detection in cytoplasm
what are CARD-family sensors
detect viruses in the cytoplasm
Toll-like receptors
type of PRR that recognizes molecules that are broadly shared by pathogens and their name is because it is similar to the protein coding Toll gene in drosophila
Types of Toll-like receptors(TLRs)
surface: TLR4(LPS) and TLR5(flagellin)
endosomal: TLR3(dsRNA) TLR7(ssRNA) TLR9(CpGDNA)
what are lipopolysaccharides(LPS)?
a component of the cell wall of gram neg bacteria
-it is a type of PAMP recognized by a PRR
what is an endotoxin
a toxin kept within bacterial cells. presence of endotoxins in the blood can cause unwanted inflammatory responses
what does multiple TLRs may recognize different structures in the same pathogen
for example, TLR4 recognizes LPS but the flagella of the same pathogen is recognized by TLR5
what is CD14
it is the binding receptor that binds LPS and is required for recognition by TLR4
what is CD(cluster of designation)
a protocol used for identifying the cell surface molecules that provide targets for the immunophenotyping of cells. They act as receptors or ligands
TLR engagement and cascade
This is the MyD88 dependent pathway
-complex of TLR4, MD2, CD14, and LPS assembles at the microphage surface
-MyD88 binds TLR4 and activates IRAK4 which leads to activation of IKK
-IKK leads to the degradation of IkB and the release of NFkB which goes into the nucleus
-NFkB activates transcription of genes for inflammatory cytokines which are synthesized in the cytoplasm and secreted
MyD88 independent pathway
-uses TRIF as an adaptor protein
-kinase cascade leads to IRF3 activation and into the nucleus
-synthesis and secretion of IFNs for fighting viral infection
interferon regulatory factors(IRFs)
proteins which regulate the transcription of interferons
Nod-like receptor recognition
-bacteria recognized in cytosol by NOD2
-leads to activation of transcription factor NFkB and cytokine release
CARD-family sensor recognition
-recognize dsRNA and ssRNA by RIG-I in cytosol
-leads to expression of interferons(IFNs) for viral infection
antigen
-substance that the antibody binds to. something the adaptive immune system is able to see and recognize
antigen presenting cells(APGs)
cells that produce antigens and present them to T cells
what do dendritic cells link
the innate immune system to the adaptive immune system
How do NK cells recognize and kill virally infected cells?
-a healthy cell expresses MHC class I which signals the NK cells to not kill it
-an unhealthy cell MHC call I expression is inhibited and signals the NK cells to kill it
where is the innate immune system present in the body
tissue, lymphoid organs, blood
(mostly tissue)
where in the body is the adaptive immune system present
lymphoid organs, blood, tissue
(mostly lymphoid organs)
lymph
plasma that has leaked through blood into tissues and is collected through lymphatic vessels
lymphoid organs
contain lymphocytes and other types of cell structures to support the production, maintenance, and circulation of lymphocytes
primary lymphoid organs
where lymphocytes are generated from immature cells to mature lymphocytes
ex) bone marrow, thymus
secondary lymphoid organs
where mature naive lymphocytes reside and an adaptive immune response can be initiated
how do lymphocytes interact with secondary lymphoid organs
they continuously survey them for infection by traveling through lymph and blood
how do secondary lymphoid organs deal with infection
they compartementalize the infection and provide a meeting place for the cells of the adaptive immune response pa
parts of the lymph node
-afferent lymphatic vessel
-T-cell area
-lymphoid follicle
-artery vein
-efferent lymphatic vessel
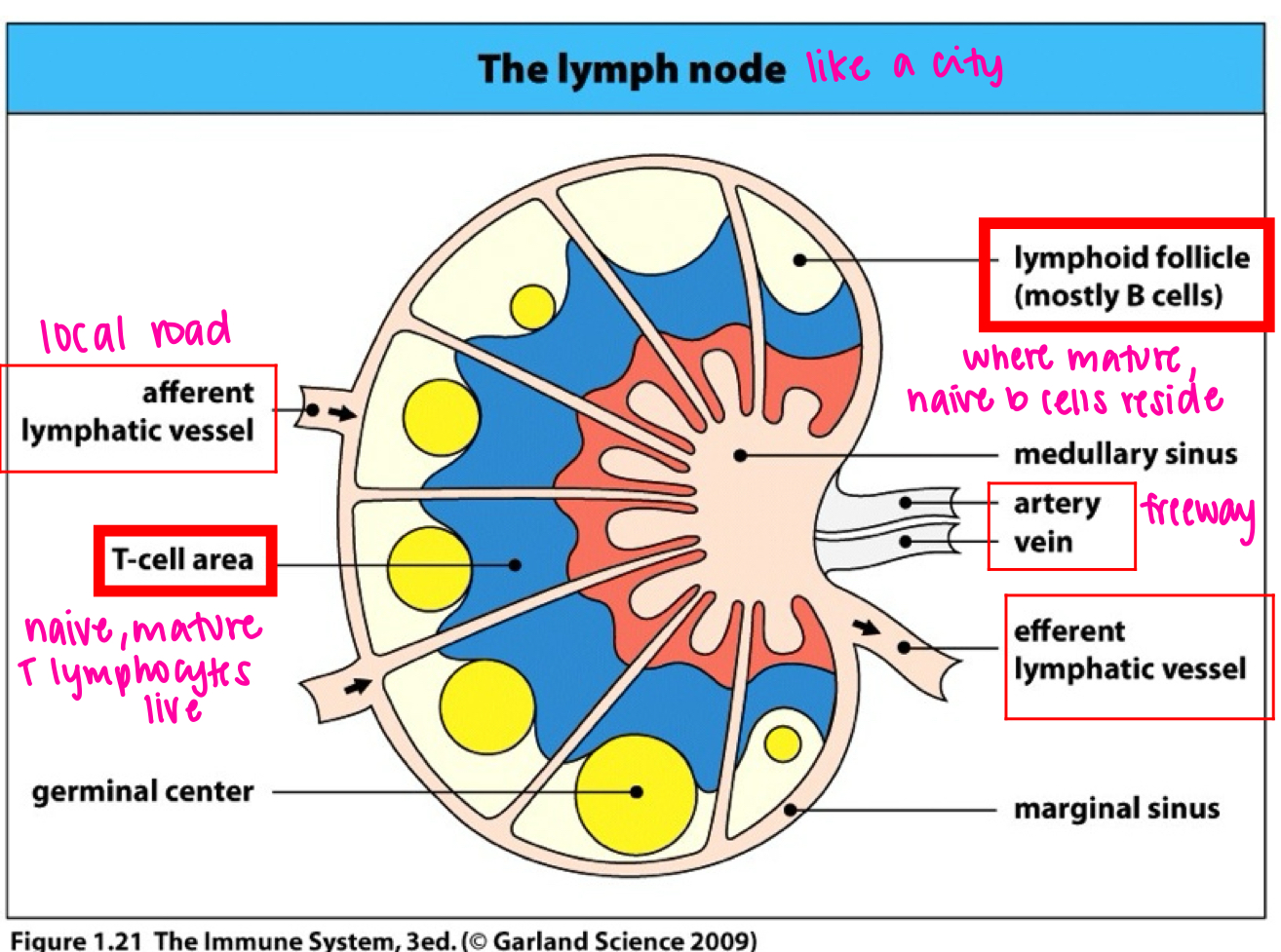
T cell area of lymph node
where naive mature T lymphocytes live
lymphoid follicle of lymph node
where mature naive b cells reside
the spleen
deals with pathogens that make it into the blood
-white pulp contains mini lymphocytes
-pathogens and lymphocytes enter spleen through the blood NO CONNECTIONS TO LYMPHATICS
gut associated lymphoid tissue
gut lumen
-commensals close the to gut in case pathogen enters from eating
-along the intestine
GALT
gut associated lymphoid tissue specialized immune system in digestive tract Mc
M cell in gut lumen
allows dendritic cells to access pathogen before the body does
rules of clonal selection
each lymphocyte bears a single type of receptor with a unique specificity
foreign molecule and lymphocyte receptor capable of binding with high affinity leads to lymphocyte activation
effector cells derived from activated lymphocyte bear receptors of identical specificity to those of the parental cell from which the lymphocyte was derived
lymphocytes bearing receptors for self molecules are deleted in early lymphoid development and absent from mature lymphocytes
B cells
secrete antigen receptor
-make antibodies
-once antibody produced you dont need B cell anymore
T cells
do not secrete antigen receptor but they kill infected cells directly and can activate other cells to do so too hu
humoral immunity
eliminations pathogens outside cells
-B cells
-not needed once antibodies are made
cell-mediated immunity
-eliminates pathogens inside the cell
-lymphocytes
-macrophage by microbial killing by helper T cells
-lysis of infected cell by cytotoxic T cells