Head Injuries
1/29
Earn XP
Description and Tags
These flashcards cover key concepts related to head injuries, including definitions, causes, injuries, symptoms, and treatment.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
What is the definition of a head injury?
A head injury encompasses any damage to the head as a result of trauma.
What are the primary forms of damage to the brain from traumatic injury?
Primary injury (direct contact injury) and secondary injury (evolving damage after initial injury).
What are the most common causes of traumatic brain injuries (TBIs)?
Falls (48%), motor vehicle crashes (14%), being struck by objects (15%), and assaults (10%).
What is the Monro–Kellie hypothesis?
The cranial vault is a closed system; if one component (brain, blood, CSF) increases in volume, the others must decrease or pressure will increase.
What characterizes a concussion?
A temporary loss of neurologic function with no apparent structural brain damage.
What are the symptoms of a basal skull fracture?
Possible drainage of CSF from ears or nose (CSF otorrhea or rhinorrhea), bruising around eyes or mastoid (Battle's sign).
What is an epidural hematoma (EDH)?
A collection of blood between the skull and the dura mater, often linked to skull fractures, causing increased intracranial pressure.
What is diffuse axonal injury (DAI)?
Damage throughout the brain due to widespread shearing and rotational forces, associated with prolonged traumatic coma.
How is the Glasgow Coma Scale (GCS) used?
To assess levels of consciousness based on eye opening, verbal response, and motor response.
What is the treatment focus for patients with TBI?
To preserve brain homeostasis and prevent secondary brain injury.
What is the role of family support in TBI recovery?
Family members need factual information, support, and may experience psychological impacts due to the patient's condition.
What long-term complications can arise from traumatic brain injuries?
Cognitive deficits, emotional changes, seizures, and chronic traumatic encephalopathy.
What should be monitored in patients with head injuries?
Vital signs, level of consciousness, temperature, and neurological status.
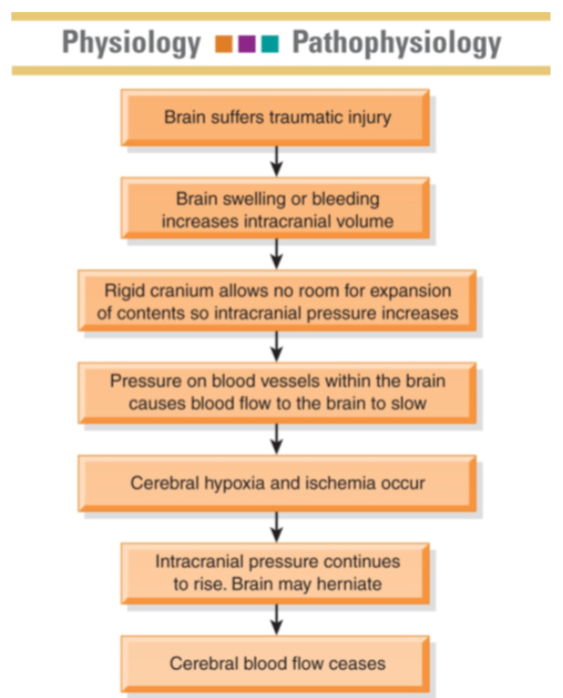
Pathophysiology of Brain Damage
• Primary injury: consequence of direct contact to
head/brain during the instant of initial injury
• Contusions, lacerations, external hematomas, skull fractures,
subdural hematomas, concussion, diffuse axonal
• Secondary injury: damage evolves over ensuing
days and hours after the initial injury
• Caused by cerebral edema, ischemia, or chemical changes
associated with the trauma
Scalp Wounds and Skull Fractures
• Manifestations depend on the severity and location of the
injury
• Scalp wounds
• Tend to bleed heavily and are portals for infection
• Skull fractures
• Usually have localized, persistent pain
• Fractures of the base of the skull
• Bleeding from nose pharynx or ears
• Battle sign—ecchymosis behind the ear
• CSF leak: halo sign—ring of fluid around the blood stain
from drainage
True or False?
Clear rhinorrhea from the nose is a sign of a
basilar fracture.
True
A patient with a head injury has bloody drainage from
the ear. To determine whether CSF is present in the
drainage the nurse
• A. examines the tympanic membrane for a tear.
• B. tests the fluid for a halo sign on a white dressing.
• C. tests the fluid for glucose
• D. collects 5 mls of the fluid in a test tube and sends to the lab
for studies.
tests the fluid for a halo sign on a white dressing.
Brain Injury
• Closed TBI (blunt trauma): acceleration/deceleration injury
occurs when the head accelerates and then rapidly
decelerates, damaging brain tissue
• Open TBI (penetrating): object penetrates the brain or trauma
is so severe that the scalp and skull are opened
• Concussion: a temporary loss of consciousness with no
apparent structural damage
• Contusion: more severe injury with possible surface
hemorrhage
• Symptoms and recovery depend on the amount of damage and
associated cerebral edema
• Longer period of unconsciousness with more symptoms of neurologic
deficits and changes in vital signs
True or False?
Contusion is a temporary loss of neurologic function
with no apparent structural damage to the brain
False
Brain Injury
• Diffuse axonal injury: widespread axon damage in the
brain seen with head trauma. Patient develops
immediate coma
• Intracranial bleeding
• Epidural hematoma
• Subdural hematoma
• Acute and subacute
• Chronic
• Intracerebral hemorrhage and hematoma
Epidural Hematoma
• Blood collection in the space between the skull and the dura
• Patient may have a brief loss of consciousness with return of lucid
state; then as hematoma expands, increased ICP will often
suddenly reduce LOC
• An emergency situation!
• Treatment includes measures to reduce ICP, remove the clot, and
stop bleeding (burr holes or craniotomy)
• Patient will need monitoring and support of vital body functions;
respiratory support
Subdural Hematoma
Collection of blood between the dura and the brain
• Acute or subacute
• Acute: symptoms develop over 24 to 48 hours
• Subacute: symptoms develop over 48 hours to 2 weeks
• Requires immediate craniotomy and control of ICP
• Chronic
• Develops over weeks to months
• Causative injury may be minor and forgotten
• Clinical signs and symptoms may fluctuate
• Treatment is evacuation of the clot
Intracerebral Hemorrhage
• Hemorrhage occurs into the substance of the brain
• May be caused by trauma or a nontraumatic cause
• Treatment
• Supportive care
• Control of ICP
• Administration of fluids, electrolytes, and antihypertensive
medications
• Craniotomy or craniectomy to remove clot and control
hemorrhage; this may not be possible because of the location or
lack of circumscribed area of hemorrhage
Management of the Patient with a Head
Injury
• Assessment and diagnosis of the extent of injury with
initial physical and neurologic examinations
• CT and MRI scans are the main neuroimaging diagnostic
tools
• Positron emission tomography (PET) for assessing brain
function
• Assume cervical spine injury until it is ruled out
• Apply cervical collar and maintain until cleared
Management of the Patient with a Head
Injury
• Therapy to preserve brain homeostasis and prevent
secondary brain injury
• Stabilize cardiovascular and respiratory function to maintain
cerebral perfusion/oxygenation
• Control of hemorrhage and hypovolemia
• Maintain optimal blood gas values
• Treat increased ICP and cerebral edema
• Surgery if indicated
• Monitor ICP and drain CSF as needed
Supportive Measures
• Respiratory support; intubation and mechanical
ventilation
• Seizure precautions and prevention
• NG tube to manage reduced gastric motility and prevent
aspiration
• Fluid and electrolyte maintenance
• Pain and anxiety management
• Nutrition
Potential Complications of the Patient
with TBI
•Decreased cerebral perfusion
•Cerebral edema and herniation
•Impaired oxygenation and ventilation
•Impaired fluid, electrolyte, and nutritional balance
•Risk for posttraumatic seizures
Assessment of the Patient with TBI
• Health history with focus on the immediate injury, time,
cause, and the direction and force of the blow
• Baseline assessment
• LOC—Glasgow Coma Scale
• Frequent and ongoing neurologic assessment
• Multisystem assessment
Nursing Interventions for the Patient with TBI
• Strategies to prevent injury
• Improve coping and support of cognitive function
• Preventing sleep pattern disturbance
• Support of family
• Provide and reinforce information
• Measures to promote effective coping
• Setting of realistic, well-defined short-term goals
• Referral for counseling
• Support groups
• Patient and family teaching
In Summary
• Head injuries can range from minor to major
traumatic brain injury resulting in long-term disability
• Rehabilitation potential is difficult to predict
immediately post-injury
• Rehabilitation is a lengthy process; must include
family/significant others