Pharm: Antidepressants
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
30 Terms
TRI’S
Amitriptyline
Amitriptyline interactions
Increased CNS effects with alcohol and other CNS depressants
Use with MAOIs can lead to cardiac instability
Amitriptyline S/E
Cardiotoxicity: arrhythmias
Sedation/ dizziness
Anticholinergic effects (blurred vision, dry mouth and eyes, urinary retention, constipation)
Weight gain
GI distress
Sexual dysfunction
Orthotic hypotension
Amitriptyline: Nursing considerations
Teach pt to rise slowly
Teach response is seen in 2-4 weeks
Administer at night if it is causing sedation
Do not withdraw abruptly
Monitor cardiovascular function- avoid use with patients who have cardiac disease
SSRI
Fluoxetine
SSRI function
Block uptake of neurotransmitter serotonin
SSRI uses
Multiple indications including depressive and anxiety disorders
SSRI interactions
Increased CNS effects with alcohol and other CnS depressants
SSRI S/E
Headache, nervousness, restlessness, insomnia, tremors, seizures, GI distress
These decrease over 2-4 weeks
SNRI
Venlafaxine
SNRI action
Inhibit the reuptake of serotonin and norepinephrine increasing these substances in nerve fibers
SNRI: uses
Major depression as well as generalized anxiety disorder and social anxiety disorder
SNRI interactions
Concurrent interaction of venlafaxine and St. John’s wart may increase risk of serotonin syndrome
SNRI S/E
Drowsiness, dizziness, insomnia, headache
Trazodone & Bupropion (Wellbutrin): Action
Affect one or two of the three neurotransmitters serotonin, norepinephrine and dopamine
Trazodone & bupropion: interactions
Do not take with MAOIs and do not use within 12 days after discontinuing MAOIs
MAOIs
Isocarboxazid & phenelzine
MAOIs: action
Monoamine oxidase enzyme cleans up norepinephrine, dopamine, epinephrine, and serotonin by inhibiting MAO, the level of these neurotransmitters rise
MAIOs : uses
Depression not controlled by TCAs and second gen antidepressants
MAIOs interaction
Drugs: vasoconstrictors & cold medicines containing phenylephrine and pseudoephedrine can cause hypersensitive crisis
Food: anything that contains tyramine (some cheeses, cream, coffee, chocolate, bananas, raisins, Italian green beans, liver, pickled foods, sausage, soy sauce, yeast, some nuts, and red wines)
MAOIS S/E
Agitation, restlessness, insomnia, anticholinergic effects, orthotic hypotension, hypersensitive crisis from fatal tyramine interaction
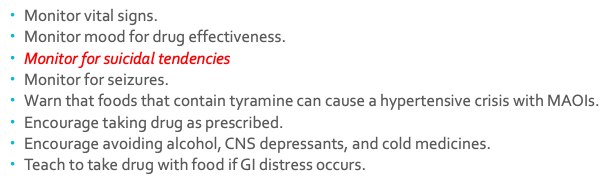
Antidepressant Nursing Interventions
Monitor vital signs.
Monitor mood for drug effectiveness.
Monitor for suicidal tendencies
Monitor for seizures.
Warn that foods that contain tyramine can cause a hypertensive crisis with MAOIs.
Encourage taking drug as prescribed.
Encourage avoiding alcohol, CNS depressants, and cold medicines.
Teach to take drug with food if GI distress occurs.
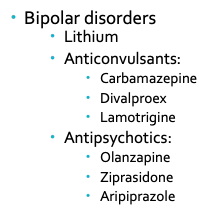
Mood Stabilizers
Bipolar disorders
Lithium
Anticonvulsants:
Carbamazepine
Divalproex
Lamotrigine
Antipsychotics:
Olanzapine
Ziprasidone
Aripiprazole
Lithium- Prototype Drug
Treats manic episodes in bipolar psychosis
Mood Stabilizer Interventions
NSAIDS may increase levels and caffeine may decrease levels
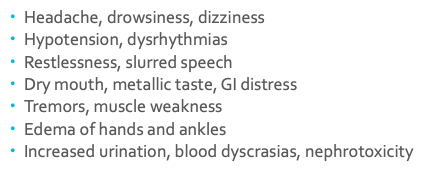
Lithium S/E
Headache, drowsiness, dizziness
Hypotension, dysrhythmias
Restlessness, slurred speech
Dry mouth, metallic taste, GI distress
Tremors, muscle weakness
Edema of hands and ankles
Increased urination, blood dyscrasias, nephrotoxicity
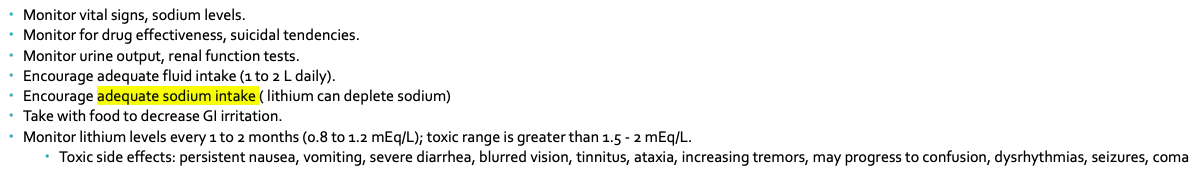
Lithium Nursing Interventions
Monitor vital signs, sodium levels.
Monitor for drug effectiveness, suicidal tendencies.
Monitor urine output, renal function tests.
Encourage adequate fluid intake (1 to 2 L daily).
Encourage adequate sodium intake ( lithium can deplete sodium)
Take with food to decrease GI irritation.
Monitor lithium levels every 1 to 2 months (0.8 to 1.2 mEq/L); toxic range is greater than 1.5 - 2 mEq/L.
Toxic side effects: persistent nausea, vomiting, severe diarrhea, blurred vision, tinnitus, ataxia, increasing tremors, may progress to confusion, dysrhythmias, seizures, coma
Lithium patient teaching
Wear medical alert identification.
Take drug as prescribed and keep medical appointments.
Don’t drive motor vehicles or operate dangerous equipment until drug effect is known.
Drug effect may take 1 to 2 weeks.
Avoid caffeine, crash diets, NSAIDs, diuretics, overheating.
Appropriate protection from pregnancy because of teratogenic effects.
Expected outcomes: Antidepressants
•Changes in affect, behavior, communication
•Brighter affect, positive mood, improved appetite and sleep patterns
•Less isolation, more prosocial interactions, engagement in therapies, increase in volition
•Decreased verbal negativity (increased positivity), increased speech fluidity
Expected outcomes: Mood Stabilizers
•Increased mood stability (fewer mood swings)
•Decreased hyperactive behavior
•Slower speech pattern
•Decrease in hypersexual behaviors
•Improved sleep patterns
•Improved appetite