3.3 organisms exchange substances with their environment
1/71
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
72 Terms
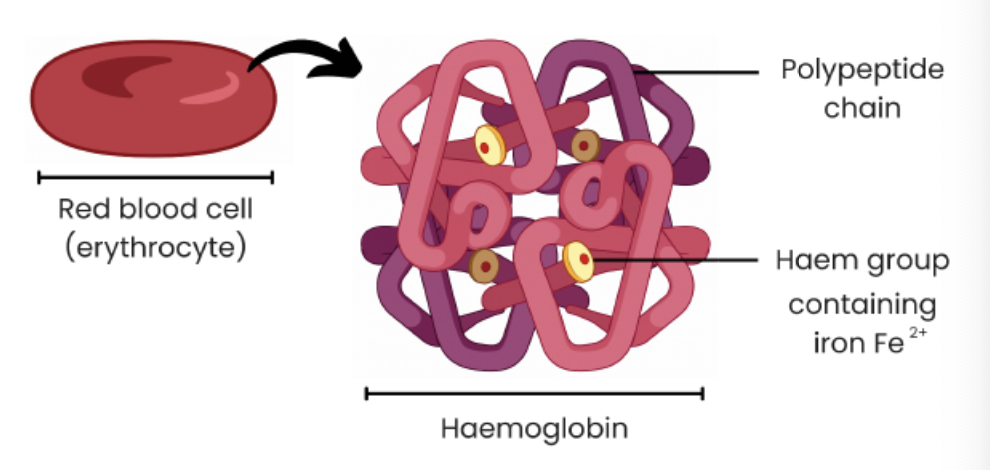
what is haemoglobin and structure
protein with a quaternary structure
made of 4 polypeptide chains
each contains a Haem group containing an iron ion
role of haemoglobin
associates with oxygen at gas exchange surfaces where the partial pressure of oxygen is high
forming oxyhemoglobin which transports oxygen
dissociates from oxygen near tissue where partial pressure of oxygen is low
what is meant by the partial pressure of oxygen
the pressure exerted by oxygen within a mixture of gases; a measure of oxygen concentration
areas of low partial pressure - respiring tissues
haemoglobin has a low affinity for oxygen
so oxygen readily dissociates with haemoglobin
so % saturation is low
areas of high partial pressure - gas exchange surfaces
haemoglobin has a high affinity for oxygen
so oxygen readily associates with haemoglobin
so % saturation is high
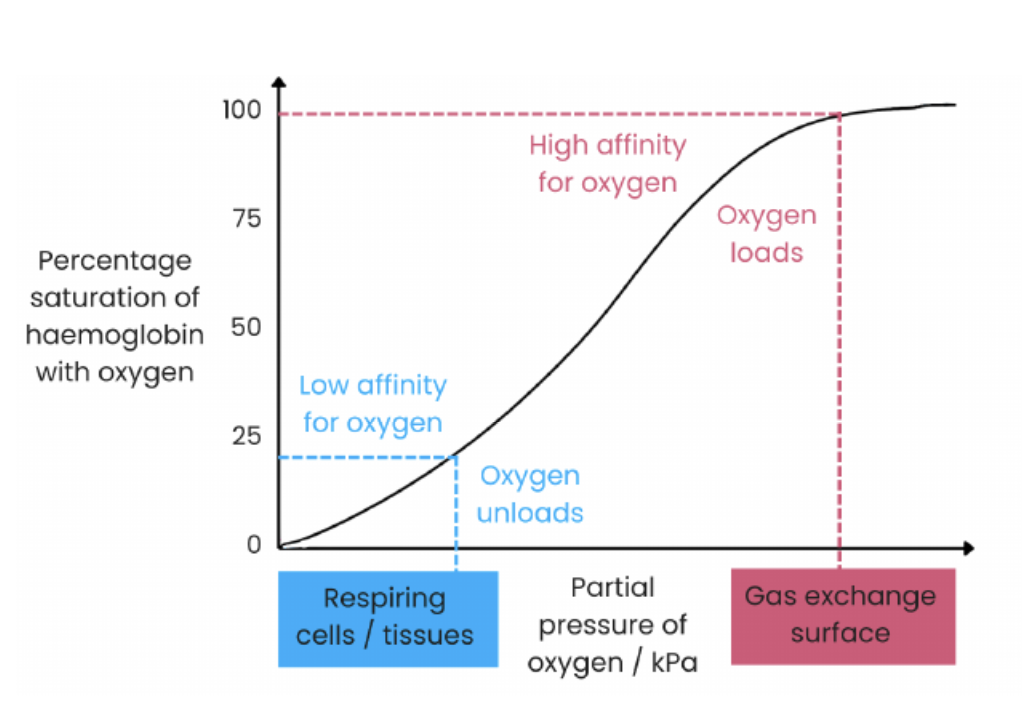
explain this dissociation curve
the oxyhemoglobin curve shows how saturation of haemoglobin with oxygen changes as partial pressure of oxygen changes
at areas of low partial pressure of oxygen such as respiring tissues the oxygen dissociates as there is a low affinity for oxygen
at areas of high partial pressure of oxygen such as gas exchange surfaces the oxygen readily associates as there is a high affinity for oxygen
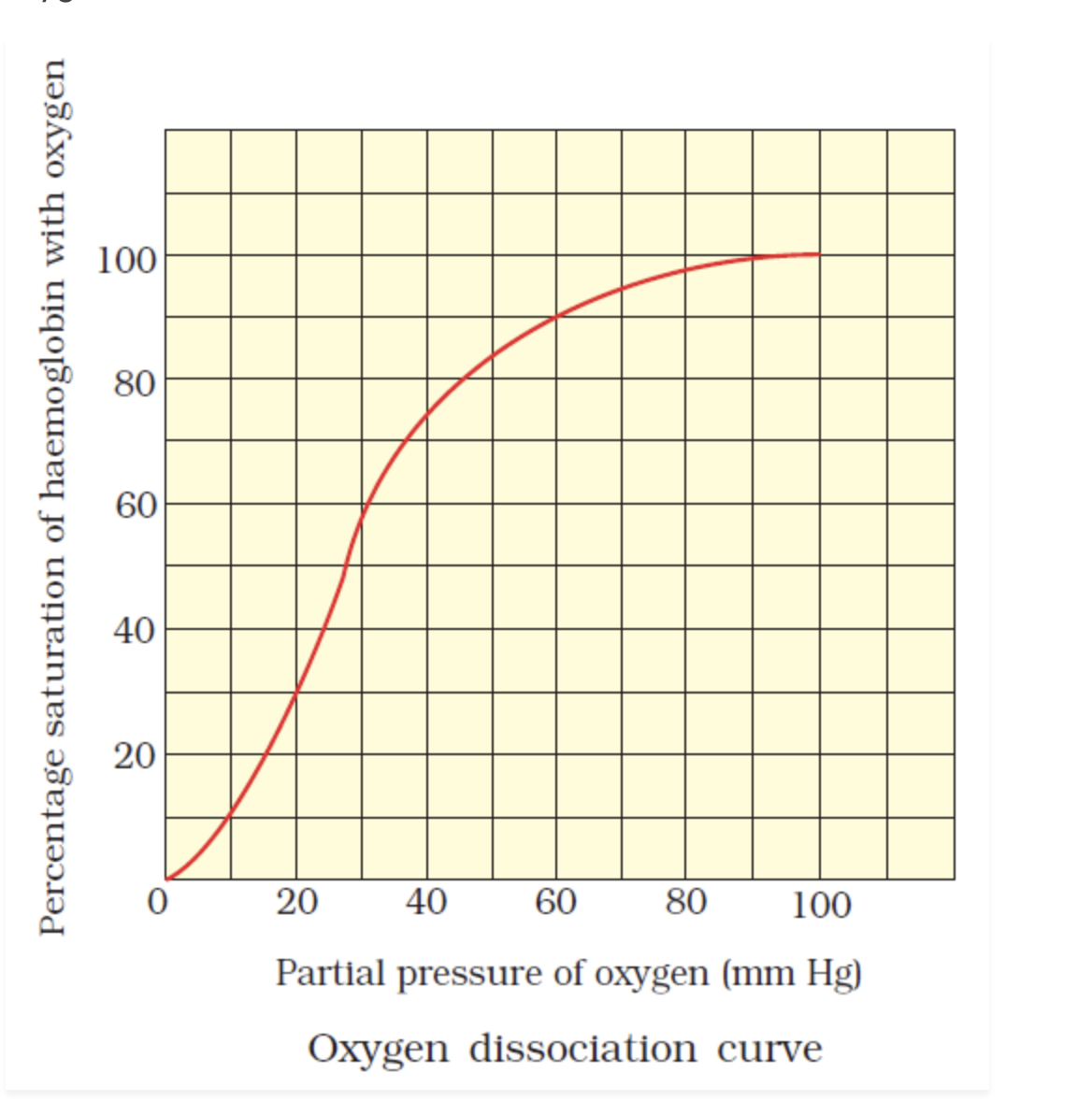
explain this sigmoid curve oxyhemoglobin dissociation curve
binding of the first oxygen causes haemoglobin to change quaternary structure
uncovering haem group binding sites
making further binding of oxygen easier
evidence
at low partial pressure of oxygen, as oxygen increases there is a slow increase in % saturation of haemoglobin with oxygen when first oxygen binds
at a higher partial pressure of oxygen as oxygen increases there is a rapid increase in % saturation of haemoglobin with oxygen showing it has got easier for oxygen to bind
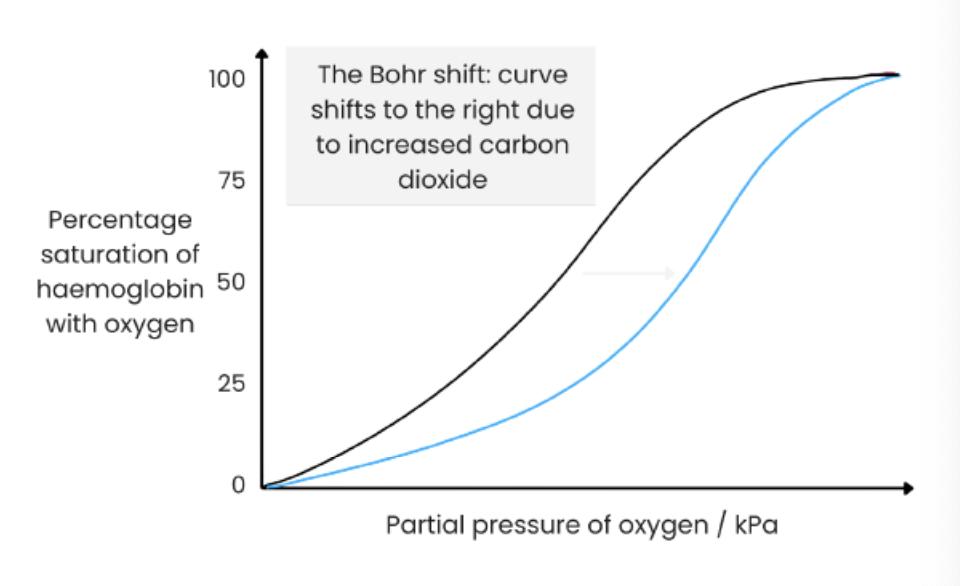
BOHR EFFECT: oxygen dissociation curve for oxyhemoglobin shifts to the right
increasing blood CO2 levels (e.g., due to increased rate of respiration)
lowers blood ph (more acidic)
reducing haemoglobin’s affinity for oxygen as quaternary structure changes
faster dissociation of oxygen to respiring cells at a given partial pressure of oxygen
evidence:
at a given partial pressure for oxygen the % saturation of haemoglobin is low
advantage:
more oxygen for tissue for aerobic respiration > produce more ATP for muscle contraction
different haemoglobins for different organisms
different transport properties
made of different polypeptide chains with different amino acid sequences > different shapes > different affinities for oxygen
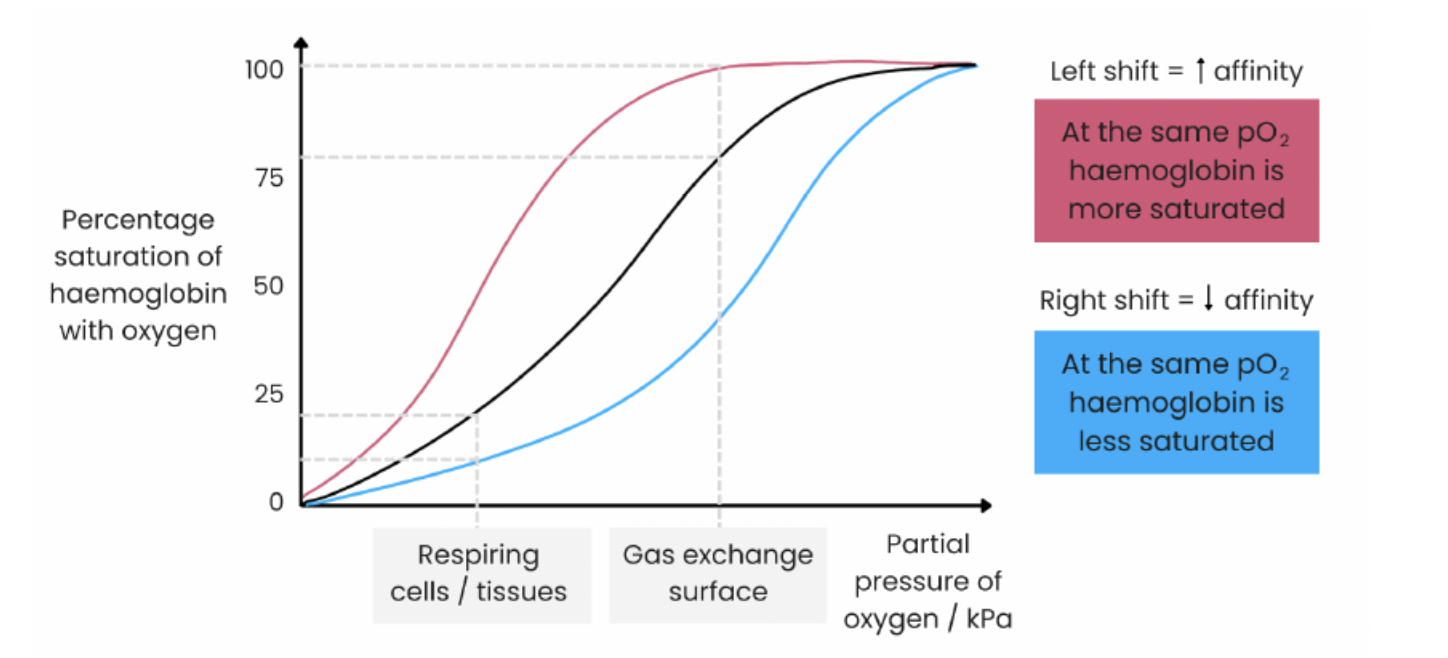
curves shift to the LEFT
haemoglobin has a higher affinity for oxygen
more oxygen associates with haemoglobin more readily
at gas exchange surfaces where partial pressure of oxygen is lower
example: organisms in low oxygen environments (high altitudes, underground, foetuses)
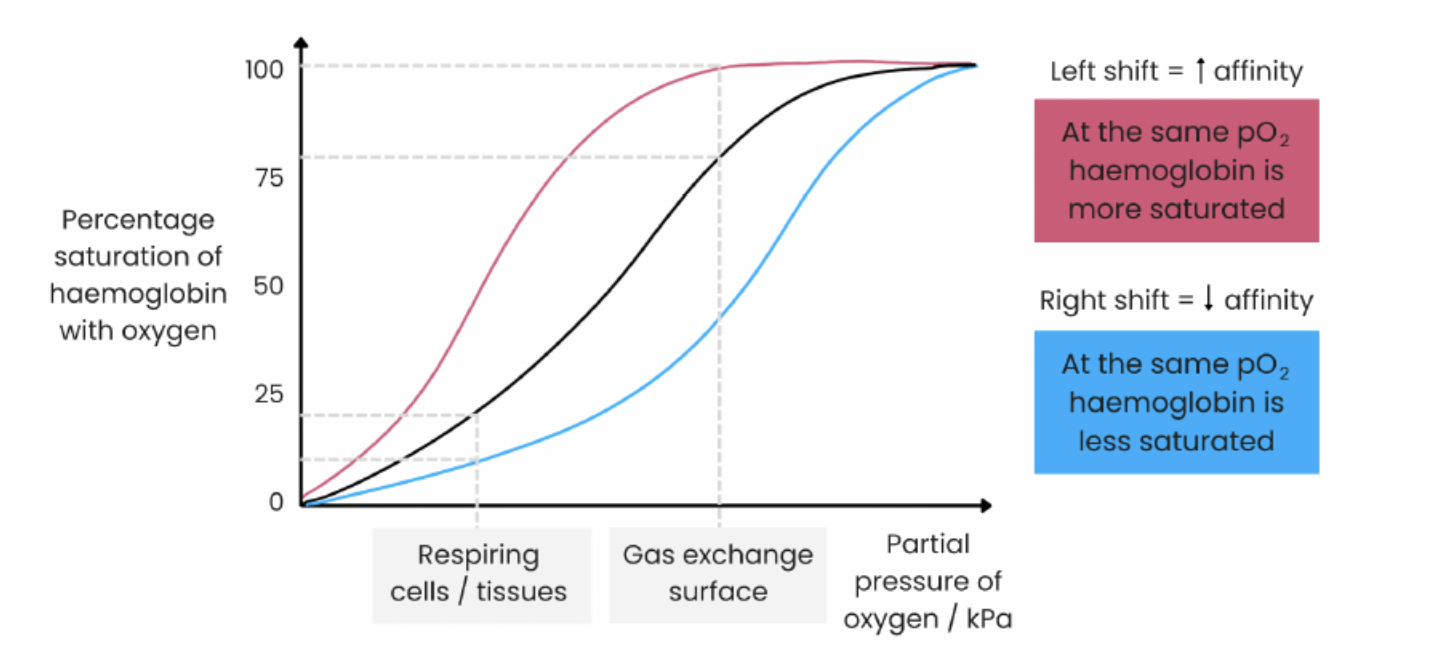
curve shifts to the RIGHT
haemoglobin has a lower affinity for oxygen
more oxygen dissociates from haemoglobin more readily
at respiring tissues where more oxygen is needed
example: with high rates of respiration/ metabolic rates (rats/birds)
loading tension
the oxygen tension at which 95% of the haemoglobin molecules are saturated
unloading tension
the oxygen tension at which 50% of the haemoglobin molecules are saturated
effect of carbon dioxide
CO2 can bind to haemoglobin and change the shape pf the molecule so it has a lower affinity for oxygen
CO2 also dissolves in water (alot of water in the blood plasma) to form carbonic acid
H+ ions change the shape of haemoglobin so it has a lower affinity for oxygen
in respiring tissue:
more CO2 produced
HB has lower affinity for oxygen
more oxygen dissociation
in the lungs:
less CO2 present
HB has higher affinity for oxygen
more oxygen binding
xylem
transports water and ions up through the stem to the leaves of the plant
how is xylem tissue adapted for its function
cells joined with no end walls to form a long continuous tube
cells contain no cytoplasm/ nucleus - easier for water to flow
thick cell walls with lignin - provide support as withstands tension and prevents water loss
pits in side walls - allow lateral water movements
cohesion-tension theory in the xylem
LEAF
water lost from leaf by transpiration; water evaporates from mesophyll cells into air spaces and water vapour diffuses through open stomata
reducing water potential of mesophyll cells
so water drawn out of xylem down a water potential gradient
XYLEM
creating tension in xylem
hydrogen bonds result in cohesion between water molecules
so water is pulled up as a continuous column
water also adheres to walls of xylem
ROOT
water lost enters the roots via osmosis

cohesion-tension theory
how water moves up the xylem against gravity via the transpiration stream
transpiration
loss of water vapour from plant leaves by evaporation through stomata
phloem tissue
transports organic substances e.g., sucrose in plants
sieve tube elements
no nucleus/ few organelles - easier flow of organic substances
end walls between cells perforated = sieve plate
companion cells
many mitochondria - high rate of respiration to make ATP for active transport of solutes
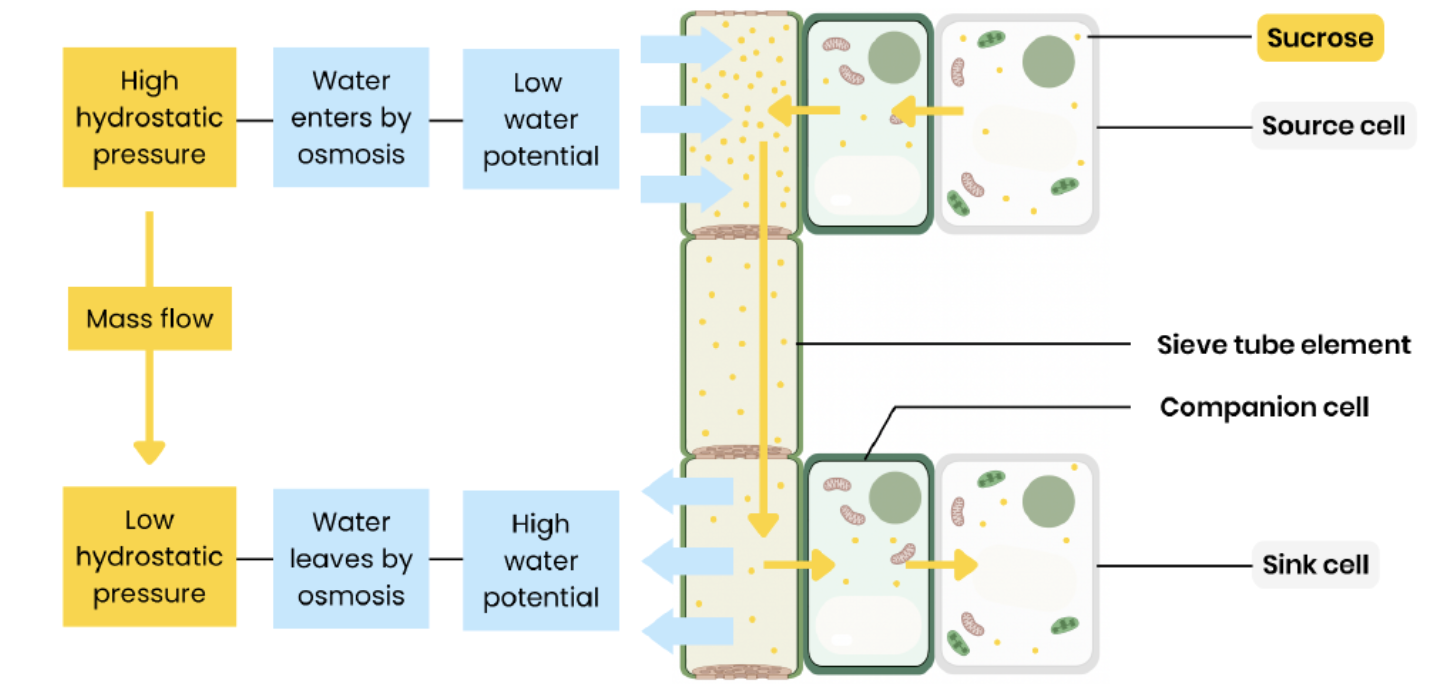
translocation
movement of solutes (assimilates) from sources to sinks (where used/ stored) by mass flow
translocation
at the source
active transport loads solutes from companion cells to phloem sieve tubes - high conc
lowering water potential in sieve tubes
so water enter phloem by osmosis from xylem/ companion cells
increasing hydrostatic pressure in sieve tubes near source
at the sink
solutes removed to be used up or stored - low conc
increasing water potential in sieve tubes
so water leaves phloem by osmosis
lowering hydrostatic pressure in sieve tubes near sink
mass flow
pressure gradient from source to sink pushes solutes from source to sink
tracer experiments
leaf supplied with radioactive tracer (eg, CO2 containing radioactive isotope 14C
radioactive carbon incorporated into organic substances during photosynthesis
these move around plant by translocation
movement traced using autoradiography or a geiger counter
ringing experiment
remove all phloem (eg, remove a ring of bark)
bulge from on source side of ring
fluid from bulge has a higher conc. of sugars than below - shows sugar is transported in phloem
tissues below ring die as cannot get organic substances
how does light intensity affect transpiration rate
TRANSPIRATION INCREASE
stomata open in light to let in CO2 for photosynthesis
allowing more water to evaporate faster
stomata close when its dark so there is a low transpiration rate
how does temperature affect transpiration rate
TRANSPIRATION INCREASES
water molecules gain kinetic energy as temperature increase
so water evaporated faster
how does wind intensity affect transpiration
TRANSPIRATION INCREASE
wind blows away water molecules from around stomata
decreasing water potential of air around stomata
increasing water potential gradient so water evaporates faster
how does humidity affect transpiration
TRANSPIRATION DECREASES
more water in air so it has a higher water potential
decreasing water potential gradient from leaf to air
water evaporates slower
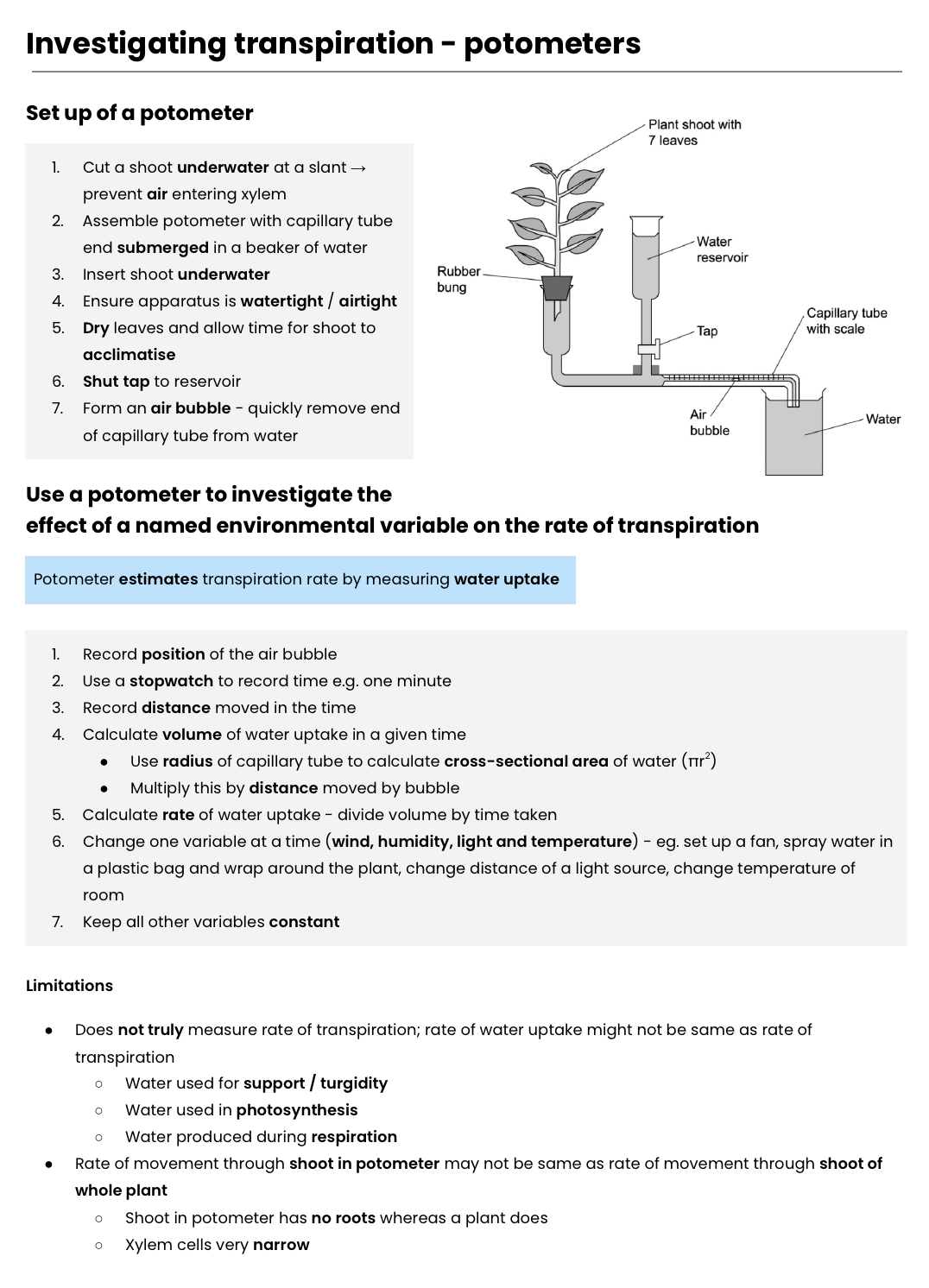
POTOMETERS - investigating transpiration
arteries
carry blood away from the heart at high pressure
a narrower lumen than a vein
thick muscular wall
elastic tissue and a folded endothelium
veins
carries blood back to the heart at lower pressure
wide lumen, thin muscular wall, smooth endothelium
pocket valves that prevent the back flow of blood
capillaries
thin blood vessels that surround all cells for exchange of substances
the endothelium is one cell thick and they have a large surface area
renal artery and vein
blood vessels carrying blood to and from the kidneys
pulmonary artery
carries deoxygenated blood from the right ventricle of the heart to the lungs
pulmonary vein
carries oxygenated blood from the lungs to the left atrium of the heart
vena cava
vein that carries deoxygenated blood from the body to the right atrium of the heart
aorta
the largest artery in the body which carries oxygenated blood from the heart to the rest of the body
right atrium
contracts to push blood into the right ventricle
right ventricle
contracts to push deoxygenated blood into the pulmonary artery
left atrium
contracts to push blood into the left ventricle
left ventricle
has a much thicker muscular wall and contracts to push oxygenated blood to the rest of the body
tissue fluid formation
arteriole: hydrostatic pressure > water potential
venule: hydrostatic pressure < water potential
remaining fluid returns to circulation via the lymphatics system
pattern of circulation
oxygenated blood leaves the heart through the aorta (artery) to supply oxygen to the respiring tissue for respiration.
deoxygenated blood enters the heart through the vena cava, the blood leaves to the lungs via the pulmonary artery, picks up oxygen from the lungs, then enters the left side of the heart via the pulmonary vein, to be pumped out through the aorta
the renal artery takes blood to the kidneys, where it leaves by the renal vein
the coronary arteries take oxygenated blood to the heart cells
what are the two types of valves:
atrioventricular valves between the atria and the ventricles on either side
semi-lunar valves between the ventricle chamber and opening of the aorta
how is the direction of blood in one way maintained
valves open in way oly
whether they open or close depends upon the pressure that builds up in the heart chambers (atria and ventricles)
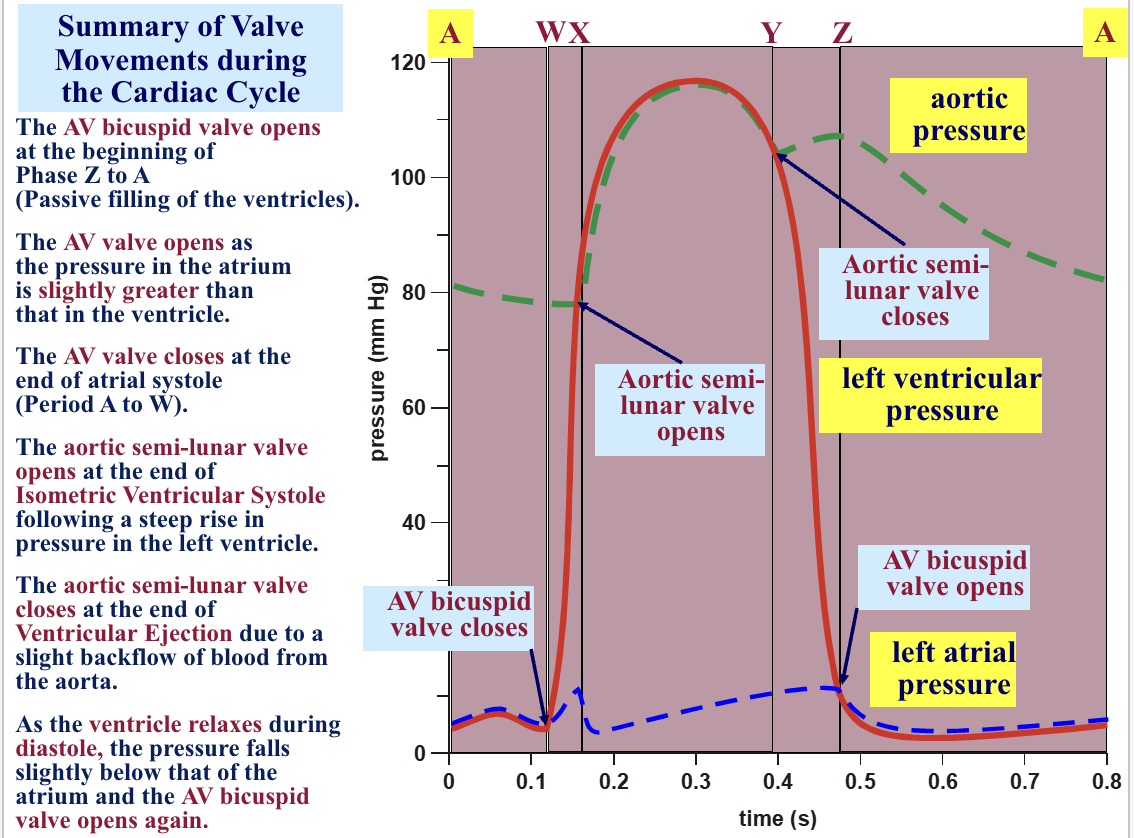
if the pressure in the atrium is higher than the ventricles , the atrioventiruclar valve opens, then as the pressure decreases the valve closes again
if the pressure in the ventricles increases too much (a pressure higher than the aorta), the semi-lunar vlave opens, then as the pressure decrease the valve closes again
systole def
contraction
diastole def
relaxation
cardiac diastole (both atria and ventricles are relaxed)
passive filling of blood (in through the vena cava) into the atria
the pressure behind the AV valves increases, so the AV valves open and blood enters the ventricles from the atria and the SL valves remain closed
atrial systole (atria contract and ventricles are relaxed)
the atria contract to push any remained blood into the ventricles, SL valves remain closed
ventricular systole (atria relax and the ventricles contract)
the ventricles contract after the pressure builds, increasing the pressure, closing the AV valves. Due to the pressure the SL valves open (so the blood flows through the arteries out the heart). Pressure in the ventricles decrease the SL valves close.
late diastole & atrial systole
AV valves = open
SL valves = closed
passive filling of the ventricles, then atrial systole
ventricular systole (isometric phase)
AV valves = closed (at the end of atrial systole)
all valves closed as the ventricle muscles contract without shortening, pressure builds up in the ventricles
ventricular systole (isotonic phase)
SL valves = open
blood is ejected into the aorta and pulmonary artery
muscles shorten as they contract
ventricular diastole (relaxation)
SL valves = close as the ventricles begin to relax
pressure falls in the ventricles and the AV valves = open
valve movementt during the cardiac cycle
what enzyme digests carbohydrates
amylases and membrane-bound disaccharidases
what enzyme digests lipids
lipase, and action of bile salts
what enzyme digests proteins
endopeptidases, exopeptidase and membrane-bound dipeptidases
mechanisms for the absorbtion of the products of digestion by cells lining the ileum of mammals include:
co-transport of amino acids and monosaccharides
micelles in the absorption of lipids
digestions of carbohydrates
takes place in the mouth as well as the small intestine
digestion in the mouth takes place with the help of salivary amylase at an alkaline pH of 7.5-8
digestions of lipids
digestions of lipids takes place in duodenum of small intestine
fats are broken down into small droplet to increase the surface area
emulsification of fats: breaking down of fats into small droplets in presence of bile salts
5 steps of digesting lipids
lipids are emulsifies by the bile
lipase break down triglycerides into fatty acids and monoglyerides
fatty acids and monoglycerides are packaged into micelles that are absorbed by microvilli
fatty acids and monoglyceriedes are converted back into triglycerides, the triglycerides aggregate with cholesterol, proteins and phospholipids to form chylomicrons
the chylomicrons move into a lymph capillary, which transports them to the rest of the body
digestions of proteins
takes place in the stomach and duodenum of small intestine
when entering the stomach the food has an alkaline pH, which then turns acidic (when mixing with HCL and enzymes etc.)
HCL maintains acidic pH of 1-2, optimum for pepsine action
digestions in the small intestine
dipeptidases: hydrolyses the peptide bond between two amino acids, creating single amino acids
endopeptidases: hydrolyse the peptide bond in the middle of the peptide chain
exopeptidase: hydrolyse the peptide bond at the end of the peptide chain
advantage: expose more ends, for more surface area
how is the tracheal system adapted
tracheoles have thin walls so short diffusion distance to cells
high branched so short diffusion distance to cells, large surface area for exchange
tracheae provide tubes full of air so fast diffusion
types of diffusion
simple diffusion: from a high to low concentration gradient where small nonpolar lipid soluble molecules pass via the phospholipid bilayer
large polar water soluble molecules go through the proteins (carrier or channel)
water modifies via osmosis from a high water potential to a low water potential
facilitated diffusion: active transport is the movement from a high to a low concentration against the concentration gradient - involved carrier proteins
active transport required energy in the form of ATP
co transport can also occur with sodium and glucose