Human Bio
1/216
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
217 Terms
Negative Feedback Loop
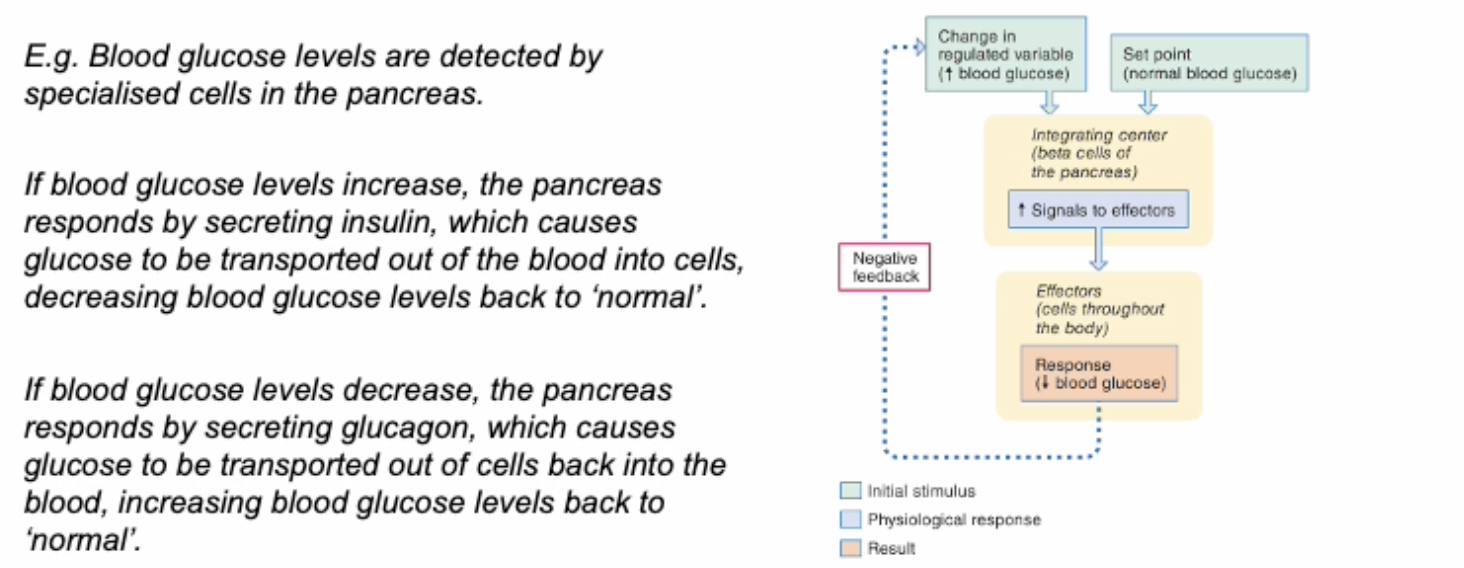
Acts to counteract changes that are sensed by producing a counteractive response
Positive Feedback Loop
Acts to enhance changes
E.g. During childbirth, uterus contracts and the baby pushes against the cervix. This stimulates the oduction of oxytocin in the brain, which causes more uterine contract, pushing the baby further down the birth canal.
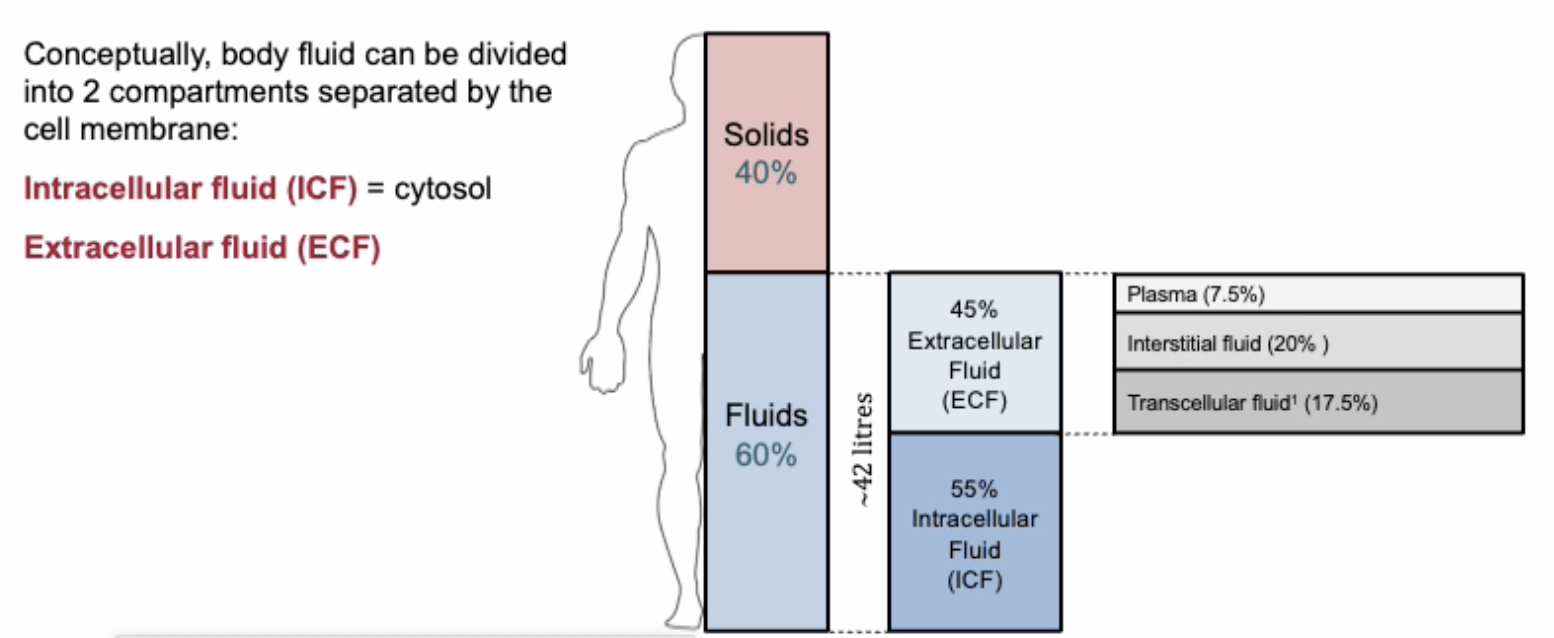
Body Fluid Compartments
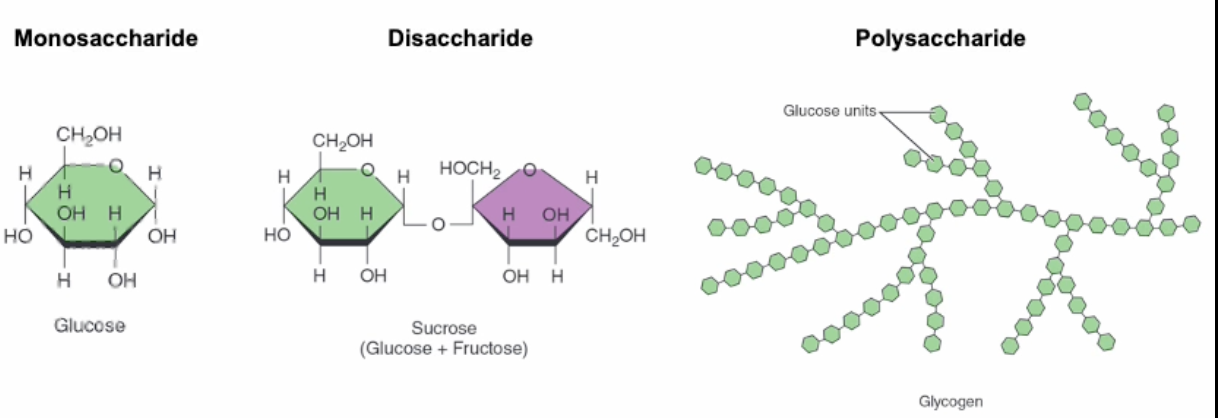
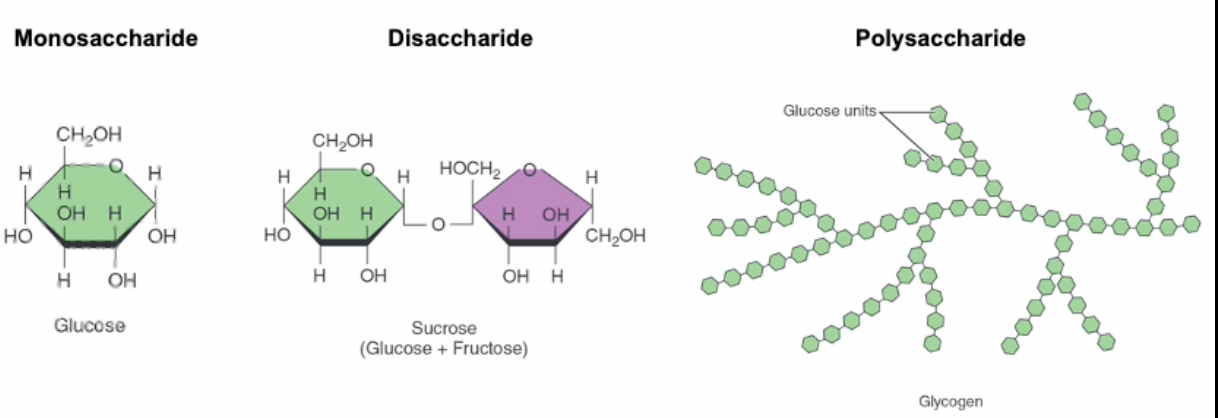
Carbohydrates
Made of carbon, hydrogen and oxygen in a 1:2:1 ratio (2 hydrogen for each oxygen and carbon).
Includes monosaccharides (simple sugars such as glucose), disaccharides (2 monosaccharides) and polysaccharides.
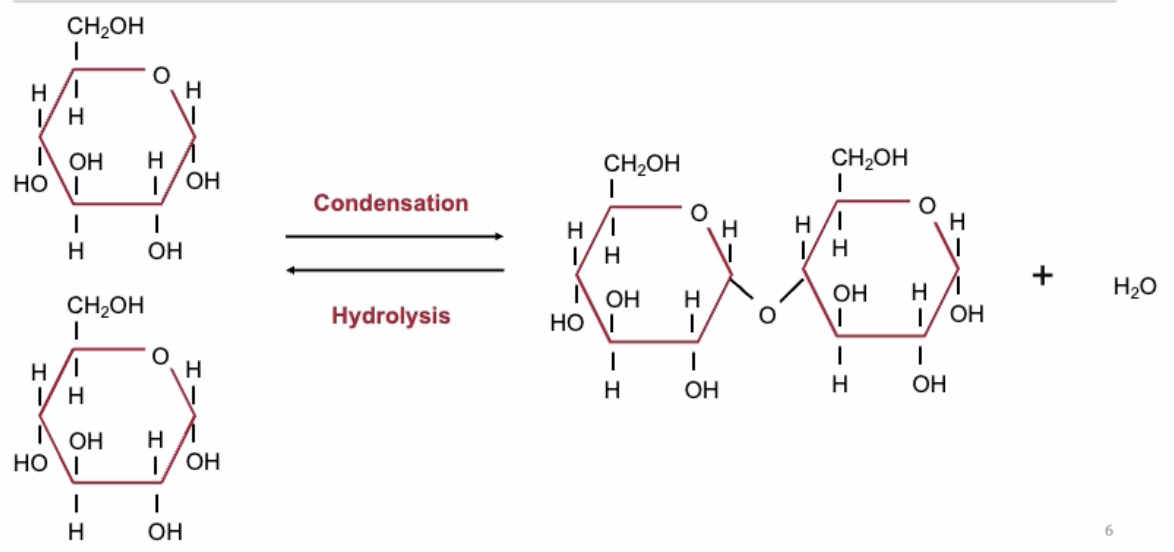
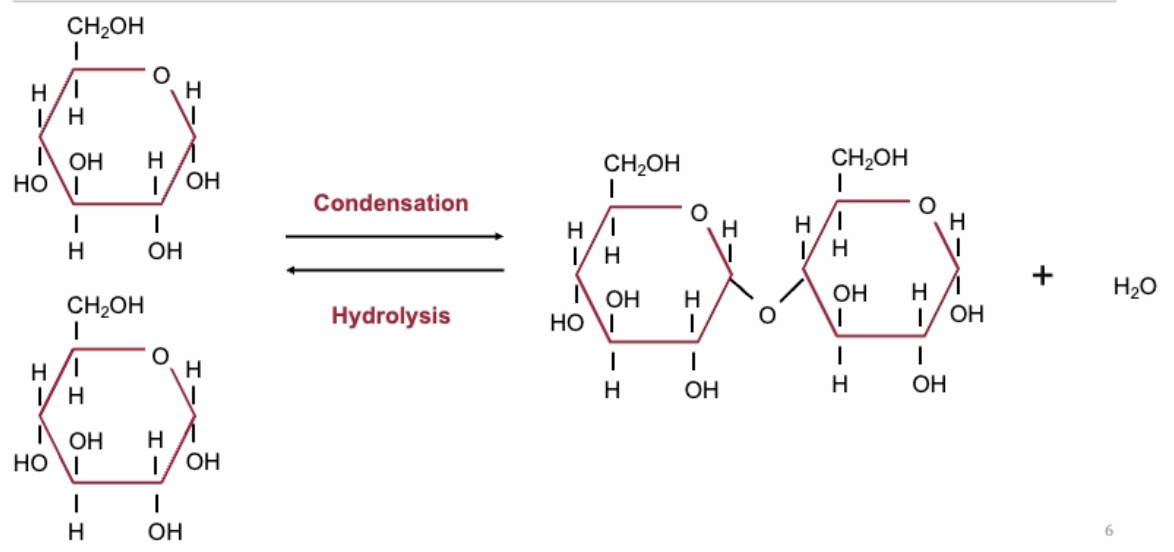
Formation of disaccharides
Formed when two or more monosaccharides join via covalent bonds through condensation, producing water.
They break down via hydrolysis using water.
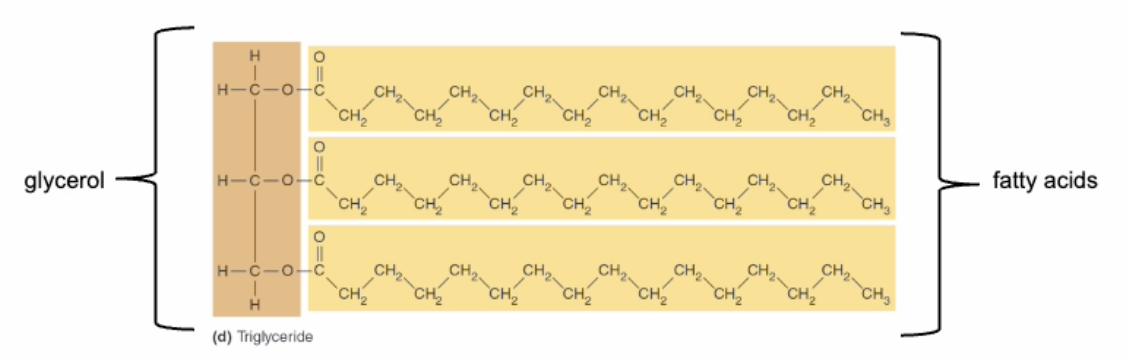
Triglycerides & Keytones
Triglycerides: Fats made of gylcerol and three fatty acids.
There are several subtypes of triglycerides depending on the bonds between the fatty acid chains:
Saturated
Unsaturated
Monounsaturated
Polyunsaturated
Different types have different effects on human health e.g. saturated fats can increase the levels of 'bad' cholesterol in the blood, which can lead to heart disease.
When triglycerides break down (via hydrolysis), some free fatty acids travel via the bloodstream to the liver and are converted into ketones as an alternative energy source.
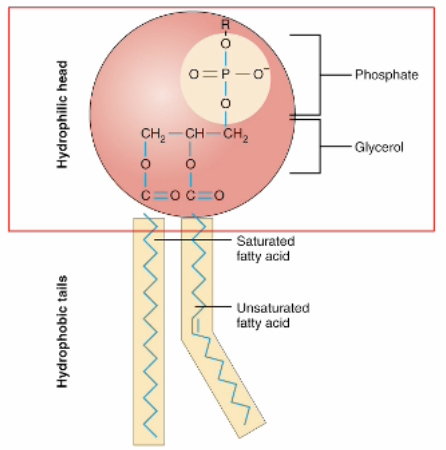
Phospholipids
Have a phosphate on one end
Fatty acid tail that is non-polar forming the hydrophobic end
Phosphate is polar and forms the hydrophilic head.
Type of amphipathic molecule.
Eicosanoids & Steroids
Eicosanoids are modified fatty acids and involved in intercellular communication.
Steroids are carbon ring structures. e.g. Cholesterol, which is a component of the plasma membrane, and a precursor to steroid hormones such as testosterone.
Cytoskeleton
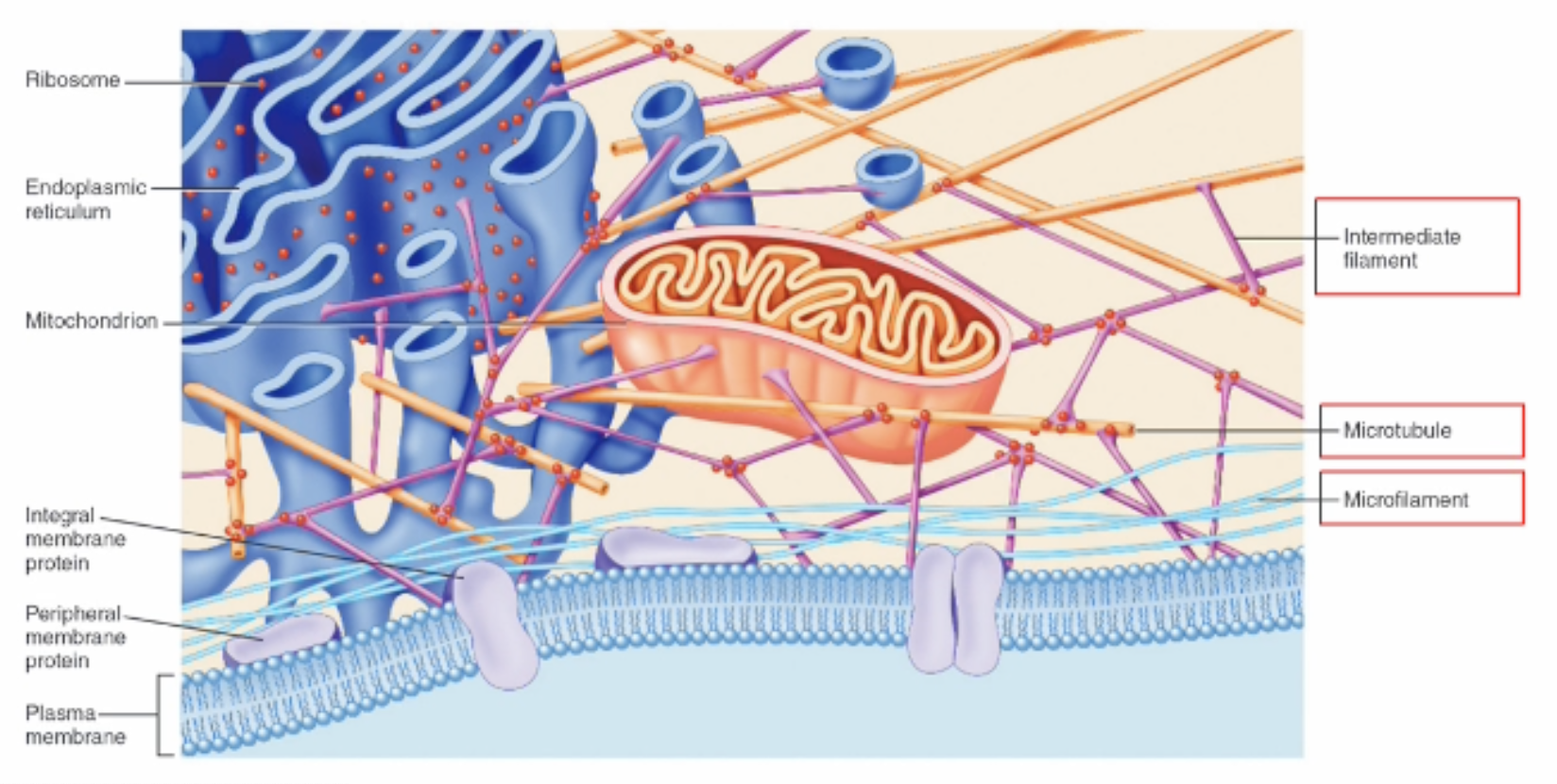
Fibrous proteins that provide structural support for transport, adhesion, contraction and movement.
Actin filaments
Thin Filament
Smallest: 7 nm
Contraction of muscle cells
Structural support
G-actin are round subunits that bind to form f-actin
2 strands of f-actin combine to form double helix microfilament
Continuously assembling and disassembling

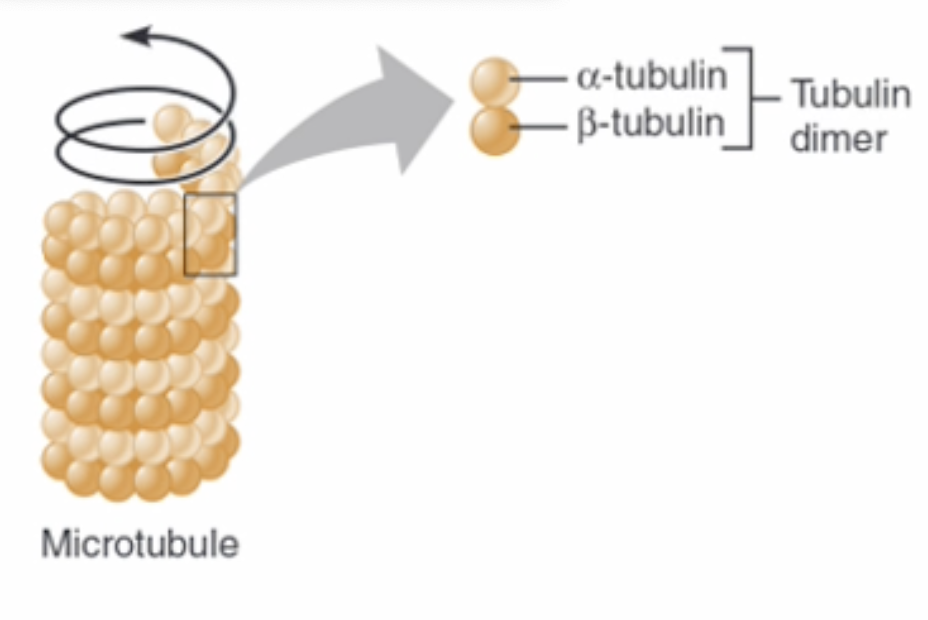
Microtubules
Largest 25 nm
Transport & cell division
Made of 𝜶 and β tubulin proteins to form a hollow tube
Continuously assembling and disassembling
Intermediate Filaments
10 nm
Mechanical strength and structural support
Includes proteins such as keratin & myosin
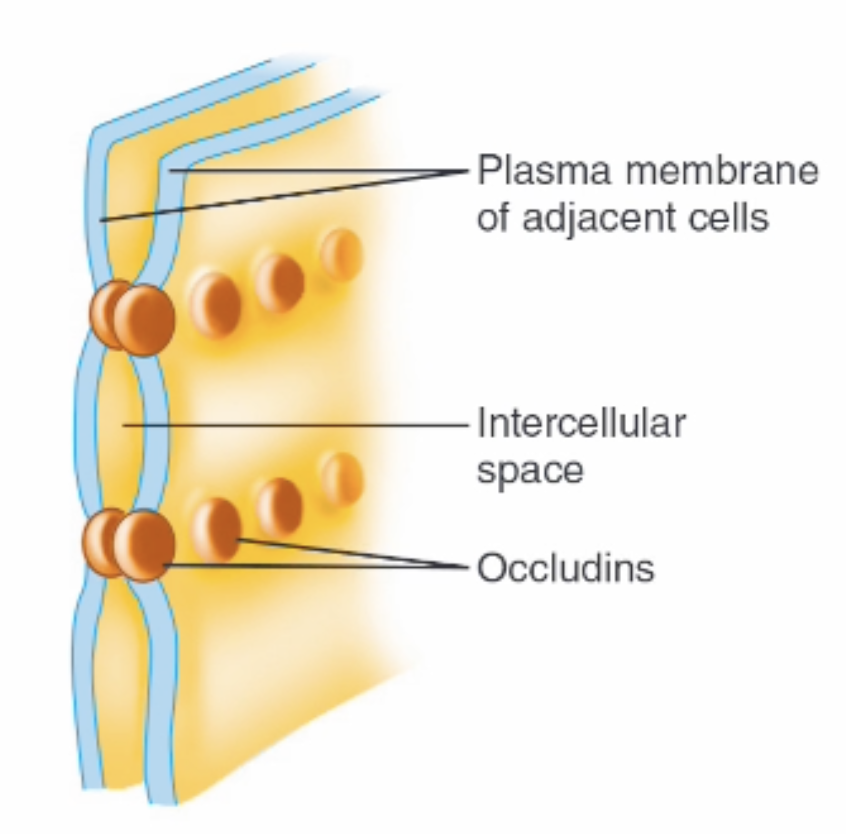
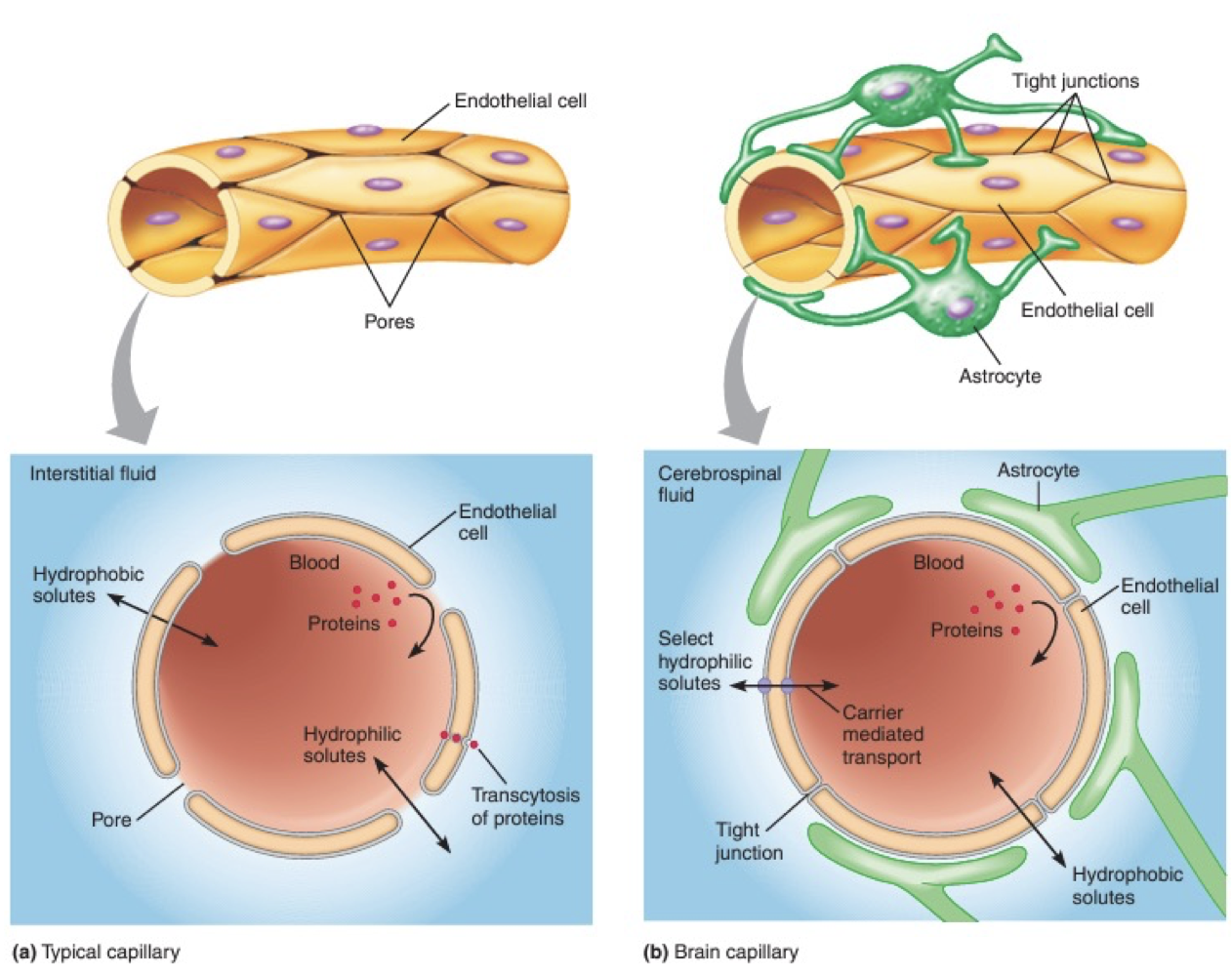
Tight junctions
Seal 2 cells together so liquid cannot move in spaces between cells
Creates an almost impermeable barrier.
Has to go through cell not around the cell
e.g. Blood brain barrier to restrict movement of substances in blood to brain.
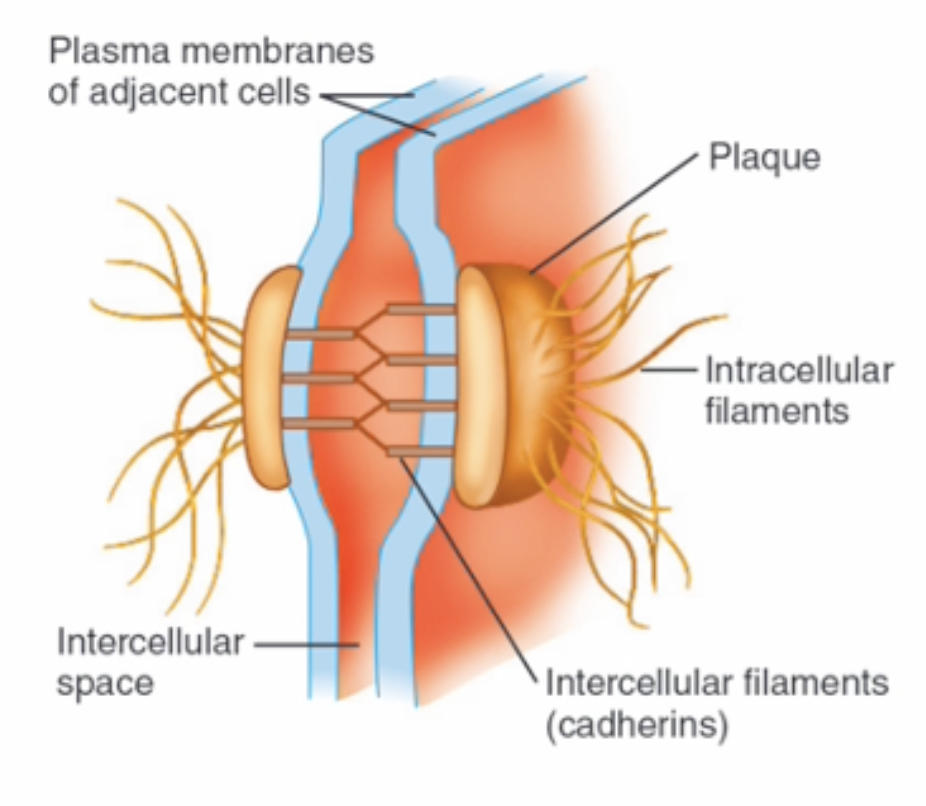
Desmosomes
Hold cells together but allow gap between
Join to cells in flexible way while providing strength during mechanical stress
Specialised proteins attached to intermediate filaments (made of keratin) that cover the cell
e.g. heart
Gap Junction
Form channel to allow molecules to quickly pass through.
Made of connexin proteins which form the channel.
e.g. Gap junctions in the heart for rapid electrical impulses
Catabolic Reactions
Large molecules into smaller molecules
Hydrolysis: Water reacts with a molecule to incorporate water.
Dephosphorylation: Phosphate group is removed from a molecule.
Anabolic Reactions
Anabolic reactions: Smaller molecules bond to produce a larger molecule.
Condensation: Two molecules break down and join together to produce water.
Phosphorylation: Phosphate group is added to a molecule.
Oxidation (reduction): Electrons are moved to a molecule, reducing charge.
ATP
Adosine triphosphate
Provides energy for muscle contraction, nerve impulses, chemical synthesis, and cell division.
Made when ADP is combined with phosphate to produce water. (phosphorylation and condensation)
Energy is stored in ATP as potential energy. To release energy hydrolysis/dephosphorylation must occur.
Aerobic Respiration
Uses oxygen and usually occurs in mitochondria (can occur in cytoplasm)
30 - 32 ATP molecules
CO2 and water as products
Glycolysis (Glucose into 2 ATP, 2 pyruvate, 2 NADH) → linking step (Pyruvate into Acetyl CoA) → Kreb cycle (1 Acetyl CoA into 1 ATP, 2 CO2, 4 co-enzymes and oxaloacetate) → oxidative phosphorylation (26 - 28 ATP per glucose molecule)
Anaerobic Respiration
Doesn’t use oxygen and occurs in the cytoplasm
2 ATP
Will produce lactic acid as a by-product.
Metabolic demand of cell is to high and not enough oxygen can be supplied
Two stages
Glycolysis: Occurs in the cytoplasm to break glucose into 2 ATP, 2 pyruvate, 2 NADH.
Pyruvate fermentation: Pyruvate interacts with lactate dehydrogenase (LDH) to make lactate (lactic acid) and NAD+. NAD+ feeds back into glycolysis to repeat the process generating more until oxygen demand can be met and aerobic respiration can continue.
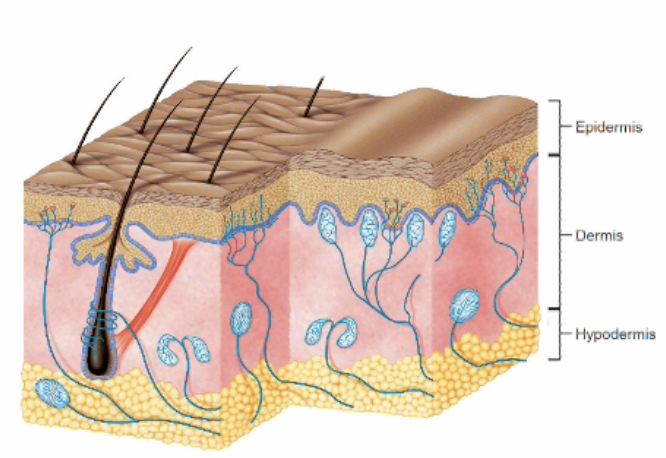
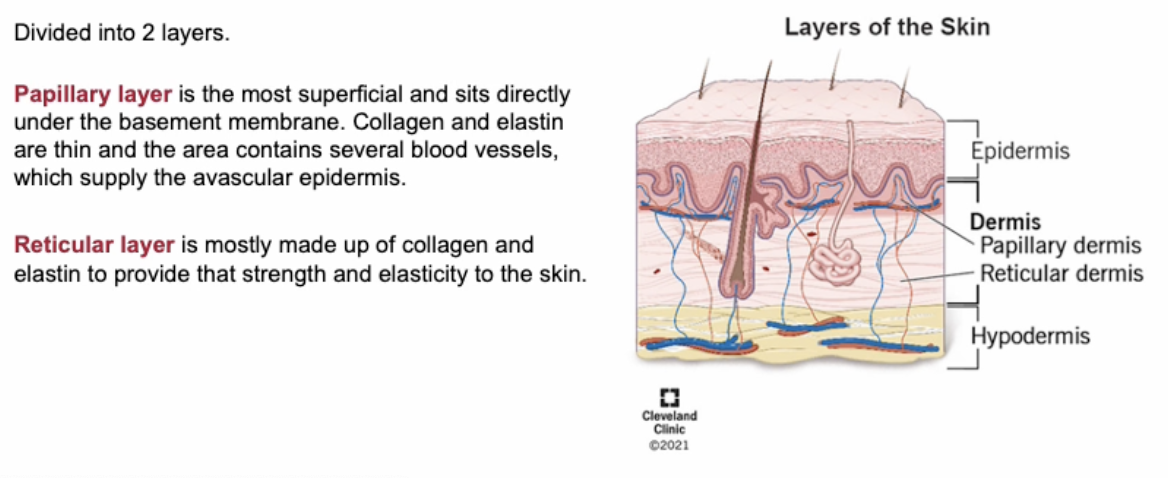
Skin
15-20% of body
Epidermis: Keratinised cells for protection.
Dermis: Collagenous and elastic connective tissue for mechanical support and strength and elasticity.
Hyperdemis: Attached to skin to cusion bones and insule skin and store energy. Adepose.
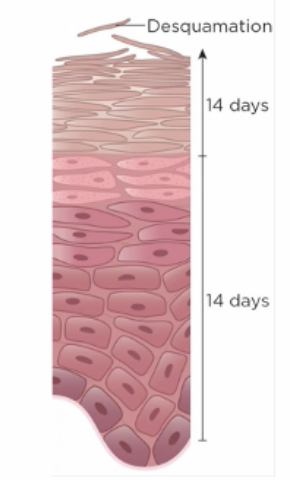
Keratinocytes
Keratinised cells start at base and move up.
As they mature they produce more keratin
Once they reach the top they are dead and just a shell full of keratin and have lost their nucleus and organelles.
Produce lipids that are eventually deposited extracellularly between cells forming the epidermal barrier on the top layer of keratinocytes to limit water loss and reduces chemicals absorbed by skin and preventing entry of microbes.
Langerhans Cells
Immune cells and moniter for pathogens or foreign objects to engulf the substance and activate an immune response
Red Bone Marrow
Red bone marrow is the site of haematopoiesis – the production of red blood cells, white blood cells, and platelets.
In children, most bones contain red bone marrow.
With age, much of it is replaced by yellow bone marrow, which is primarily adipose tissue.
Red marrow contains hematopoietic stem cells, which give rise to all blood cell types.
Oxidative Phosphorylation
Inner mitochondrial membrane and produces majority of ATP molecules.
The co-enzymes produced from kreb release electrons which pass through the electron transport chain and releases energy to transport hydrogen across the matrix.
High concentration of hydrogen on one side creates store of potential energy and ATP synthesis uses this to synthesise (26 - 28 ATP per glucose molecule)
Kreb Cycle
Occurs within the matrix
One cycle produces 1 ATP, 2 CO2, 4 co-enzymes and oxaloacetate.
Linking Step
Before kreb
Pyruvate moves to the mitochondrial matrix where it is converted to Acetyl CoA to start kreb.
1 glucose produces 2 pyruvate producing 2 cycles of kreb.
Glycolysis
Occurs in the cytoplasm to break glucose into 2 ATP, 2 pyruvate, 2 NADH.
Pyruvate fermentation
Pyruvate interacts with lactate dehydrogenase (LDH) to make lactate (lactic acid) and NAD+.
NAD+ feeds back into glycolysis to repeat the process generating more until oxygen demand can be met and aerobic respiration can continue.
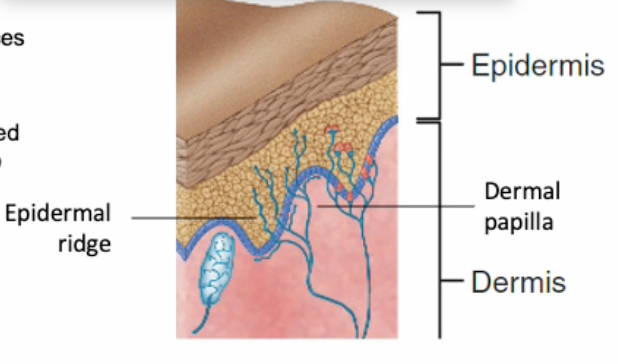
Epidermis
First line of defence.
Thicker in areas with high abrasion.
Avascular so removes all waste and gets nutrients via dermis.
Keratin, langerhans, melanocytes, Merkel cells.
Dermis
Irregular juction with epidermis to increase SA for attachment and reduce chances of epidermis being ripped off during mechanical stress
Made of collagen and elastin produced by fibroblasts
Contains hair folecules, blood vessels, nerves and endocrine sweat glands.
Hair
Hair grows out of hair follicles
Hair follicle is part of the epidermis that extends into the dermis/hypodermis
Pigment comes from melanocytes
Hair follicles have
Sebaceous glands:
Produce sebum which travels along the shaft of the hair where it is secreted onto epidermis to lubricate hair and skin.
Have several on one hair follicle
Nerves: To detect hair movement for sensation of touch
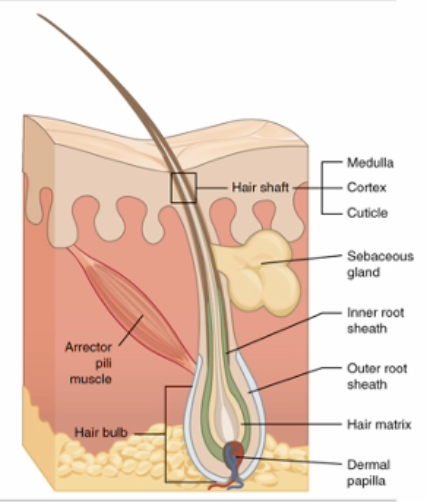
Eccrine sweat glands are found in dermis produce sweat to cool us and metabolic waste.
Apocrine glands secret hormones in armpits and genitalia.
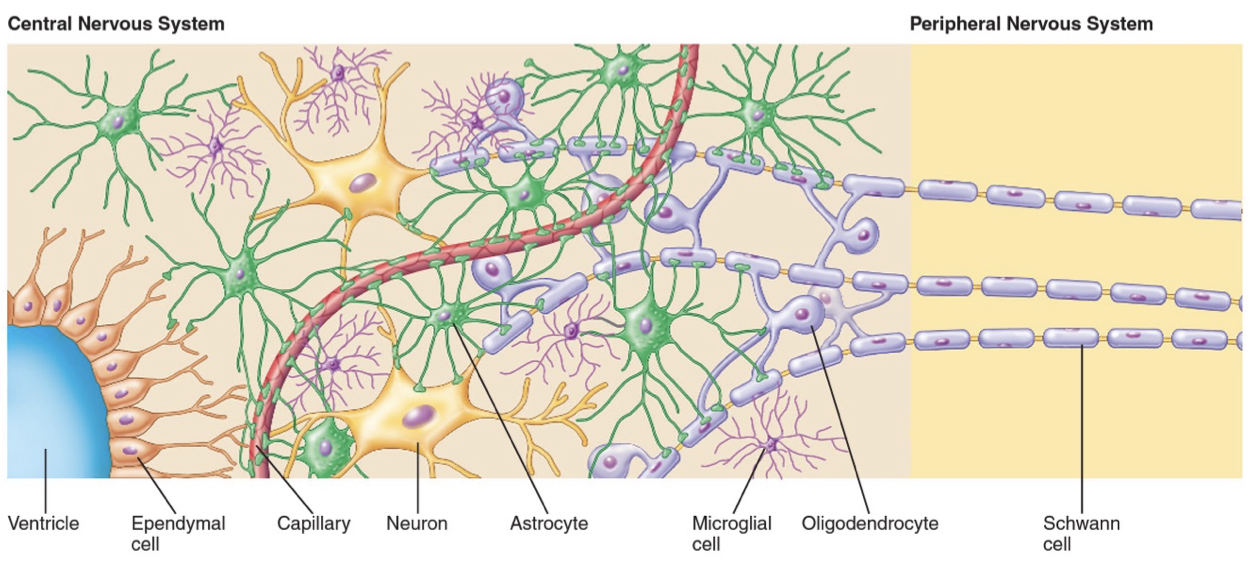
Types of neuroglia
Astrocytes: Transport nutrients such as glucose to neuron’s
Oligodendrocytes: Produce myelin in the CNS
Schwann cells: Produce myelin in the PNS
Microglia: Immune cells of the CNS because they phagocytose debris after injury or pathogens to prevent infection.
Ependymal cells: Line ventricles and central canal of spinal cord to produce CSF to cushion and provide the brain with nutrients.
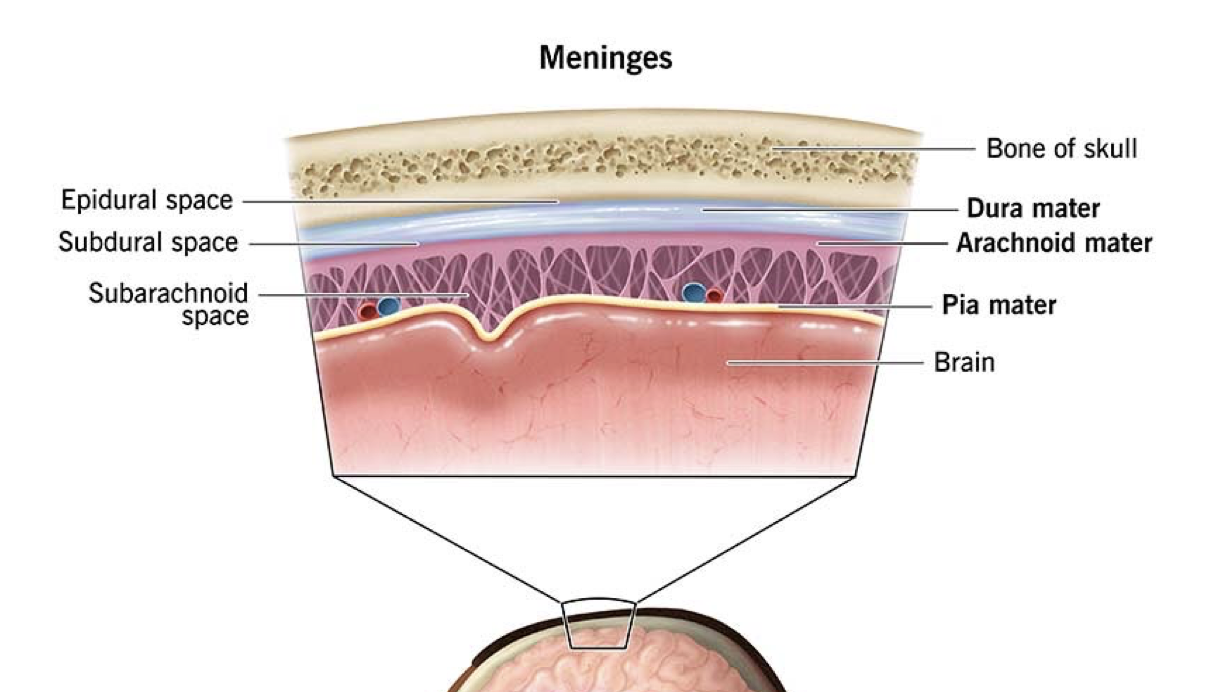
Meninges
Dura matter: Outer, tough, fibrous connective tissue attached to the cranium.
Arachnoid matter: Middle layer, attached to dura matter with a space between it and the pia matter called the subarachnoid space for CSF.
Pia matter: Inner thin layer of connective tissue attached to brain.
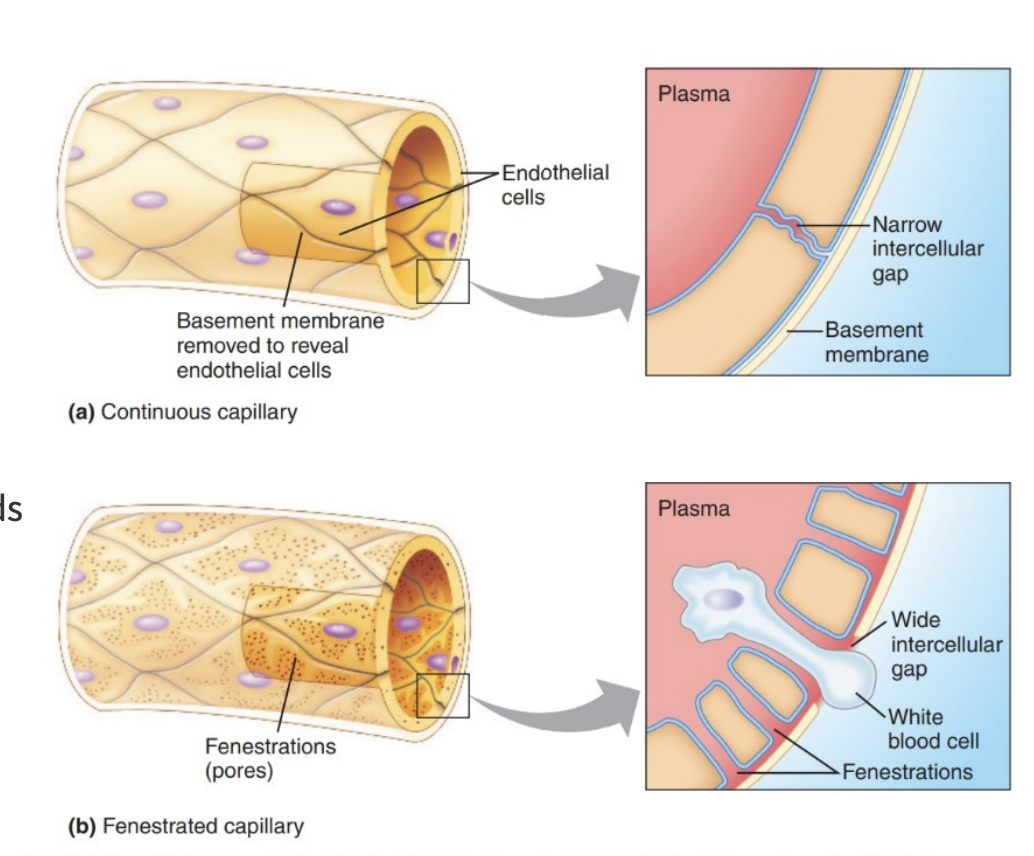
The Blood Brain Barrier
Brain receives 15% of blood supply due to neuron’s high metabolic rate (20% of our oxygen and 50% glucose)
Brain cannot store glucose like the liver
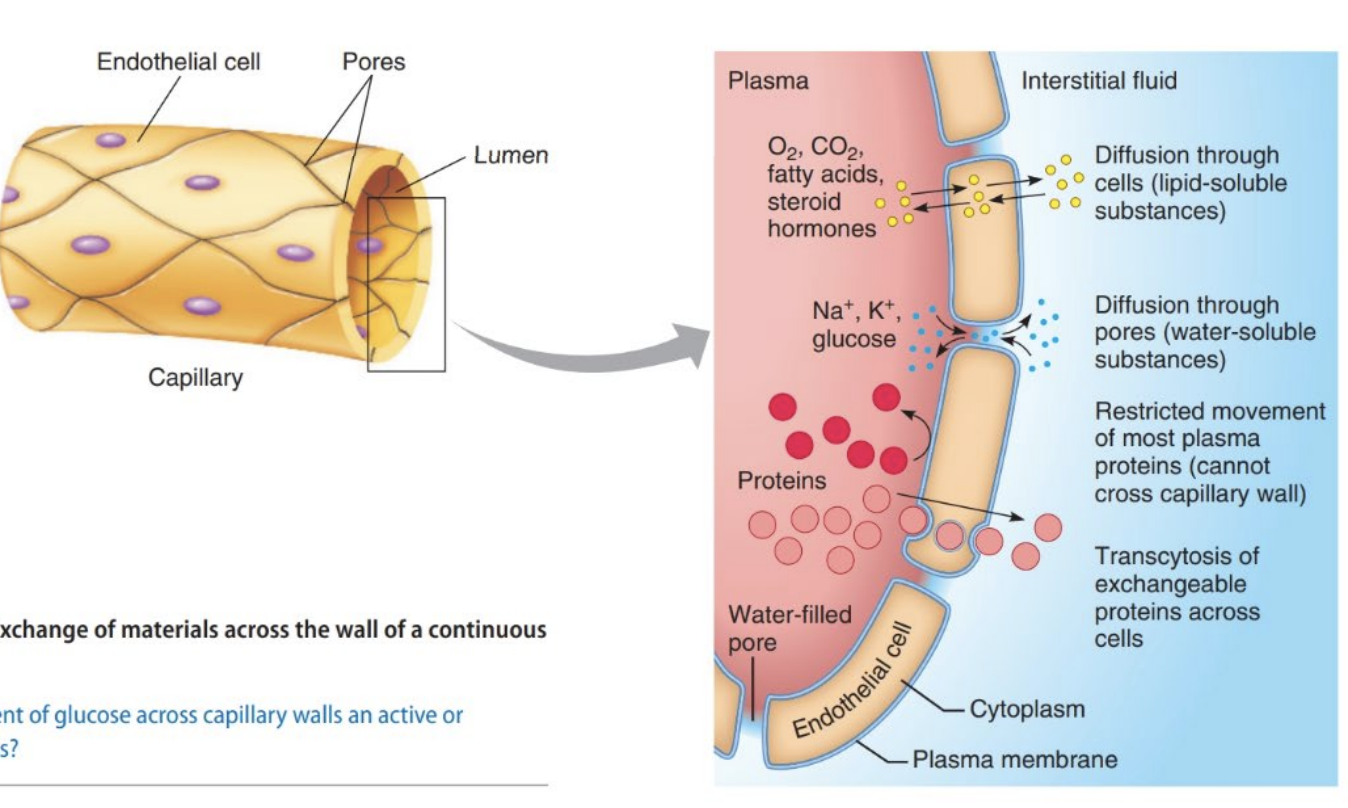
Movement of molecules usually occurs through small pores in the endothelia cells that made up the capillary walls
In the CNS they are held tightly together to restrict the movement of molecules and protect the CNS from harmful things in the blood creating the blood brain barrier.
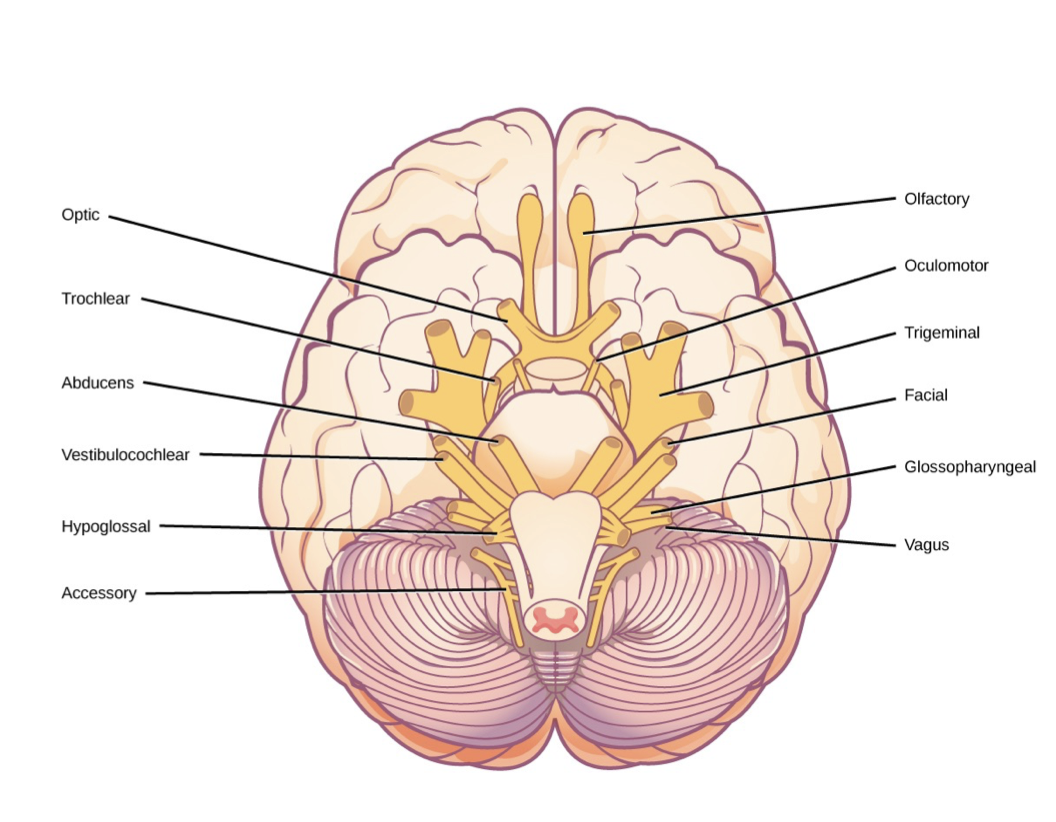
Cranial Nerves
Oh - Olfactory
Oh - Optic
Oh - Oculomotor
To - Trochlear
Touch - Trigeminal
And - Abducens
Feel - Facial
Very - Vestibulococlear
Good - Glossopharyngeal
Velvet - Vagus
Ah - Accessory
Heaven - Hyperglossal
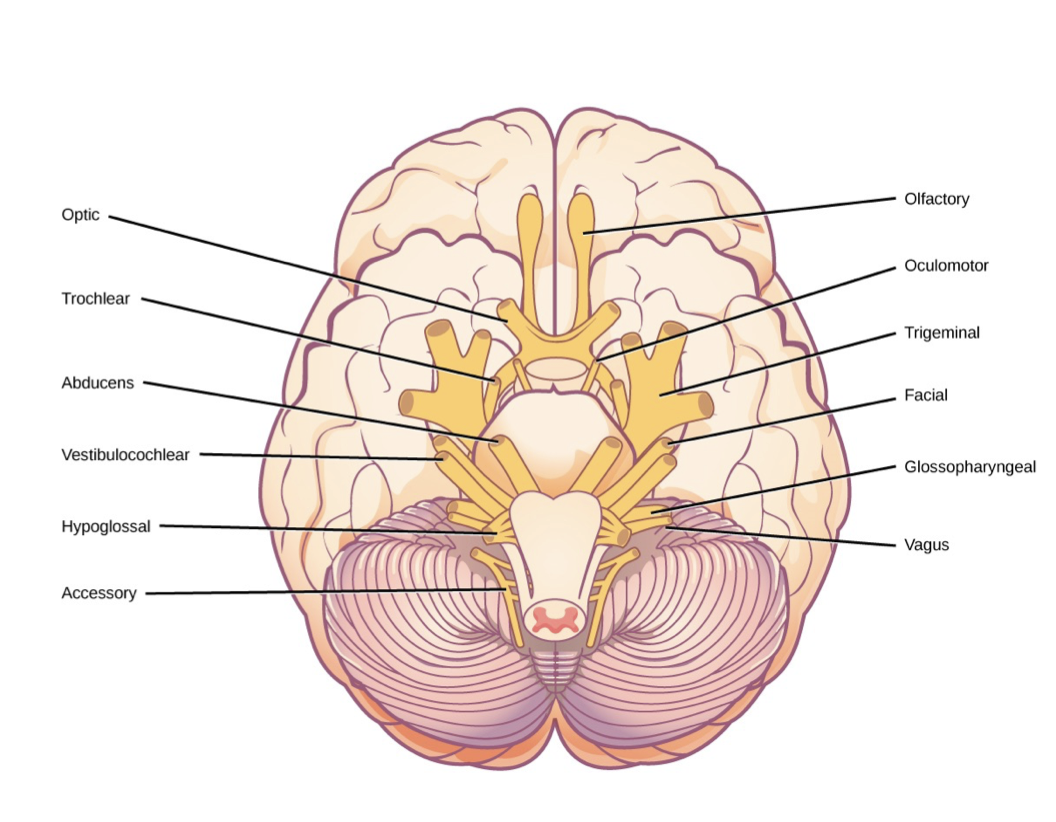
Identify Cranial Nerves
Neural Foramen
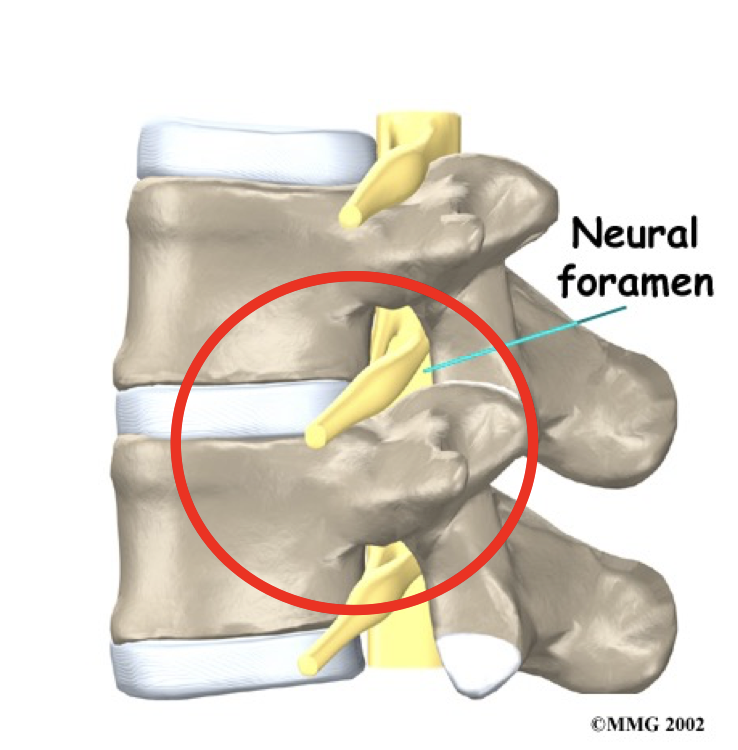
Spinal nerves emerge from the vertebral column through an opening called a neural foramen between adjacent vertebrae.
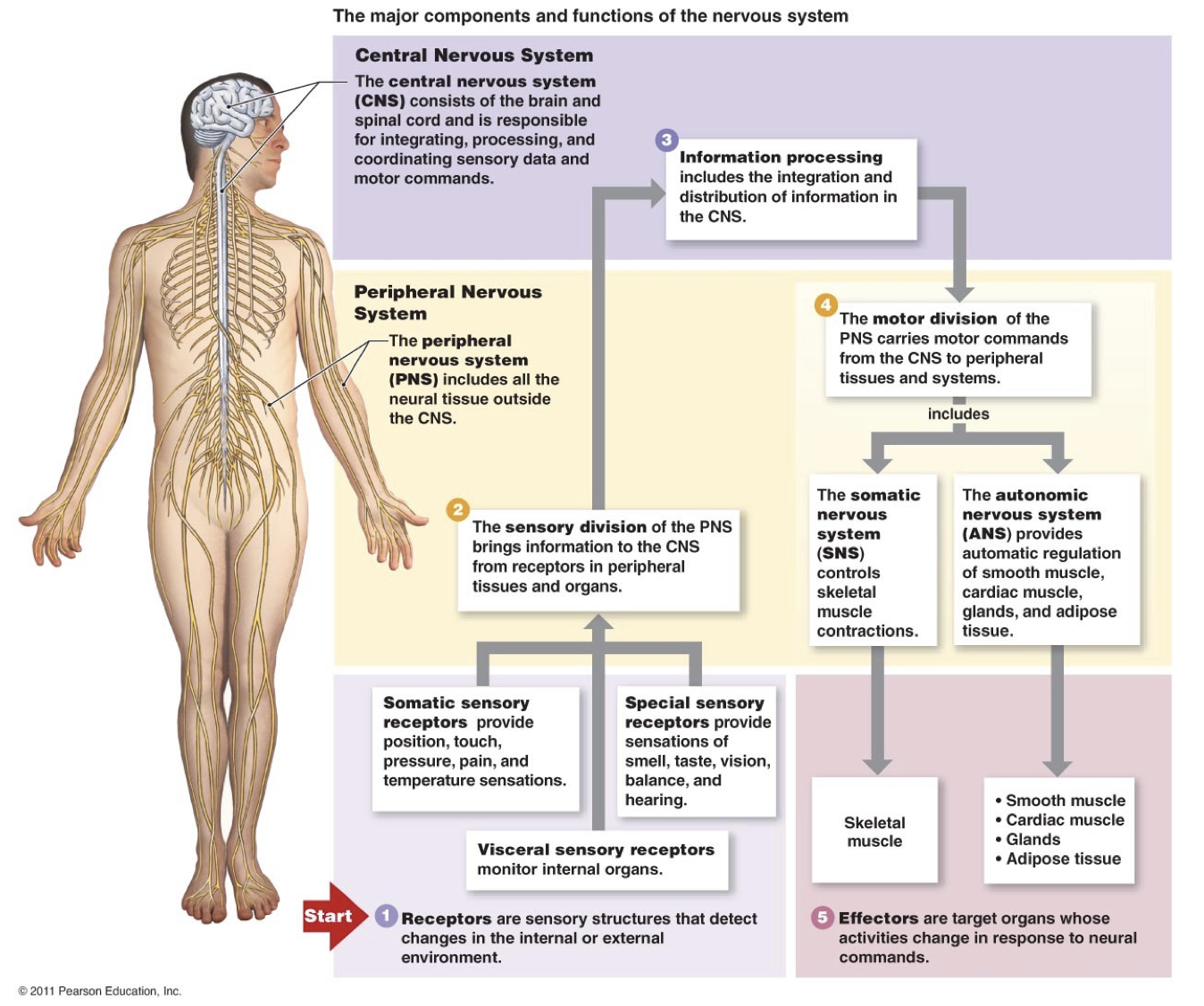
Spinal Nerves
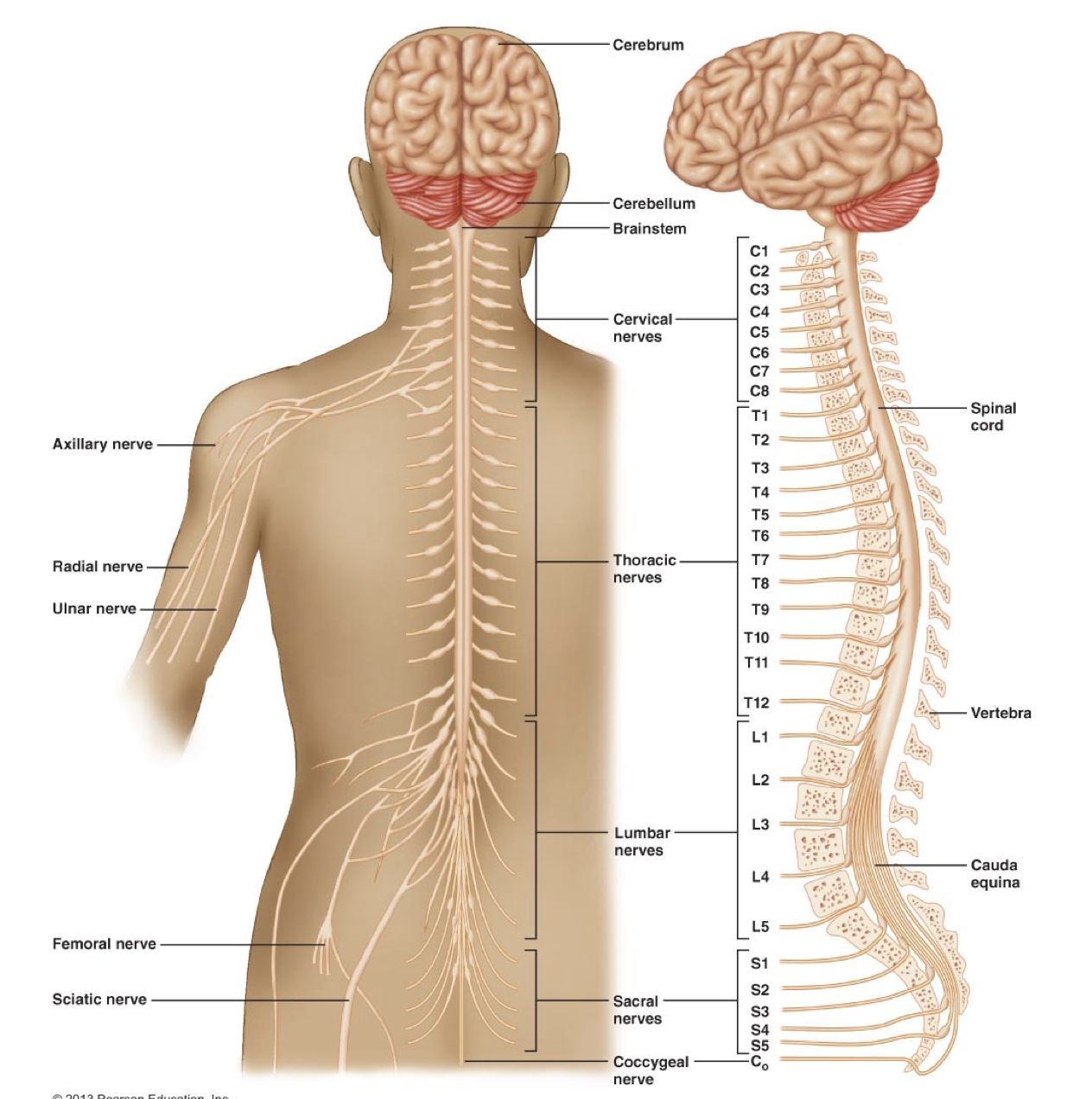
Sensory division of the PNS (Spinal and peripheral nerves)
PNS to CNS
Somatic receptors: Position, touch, pressure, pain and temp
Specialised receptors: Smell, taste, vision, balance, and hearing
Visceral receptors: Internal organs
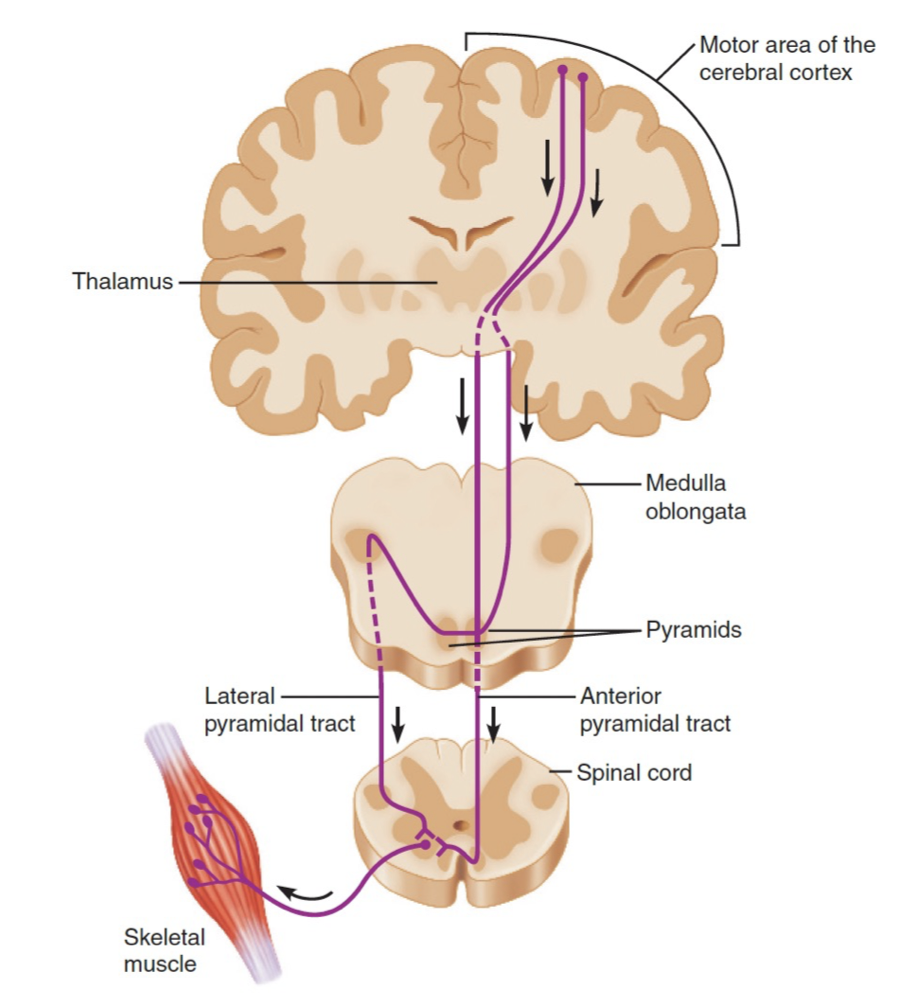
Motor Division of the PNS
CNS to PNS
Somatic nervous sytem: Skeletal muscles (voluntary)
Autonomic nervous system: Smooth muscle, cardiac muscle, glands, adipose tissue (involuntary)
Sympathetic: Fight or flight
Parasympathetic: Rest and digest. Relaxation.
Enteric Nervous System: Complex network of neuron’s that governs gastrointestinal system (second brain for peristalsis and enzyme secretion)
The Major Components and Functions of the Nervous System
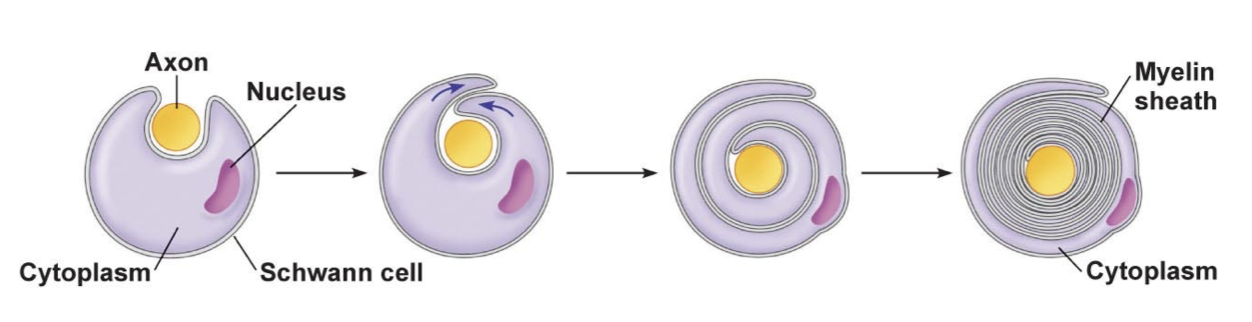
Myelin Sheith
Schwann cell or oligodendrocyte wraps around the axon
Cytoplasm is gradually squeezed out
50 - 150 stacked layers of membrane
Myelin is made of lipids which is a poor conductor of electricity insulating the axon.
Action potentials regenerate at the nodes of ranvier where the is no axon sheath.
Juxtacrine signalling
Membrane bound proteins interact with each other and ligands in the extracellular matrix to communicate with adjacent cells.
Signals travel via hydrophobic membrane channels/pores (gap junctions) between cells.
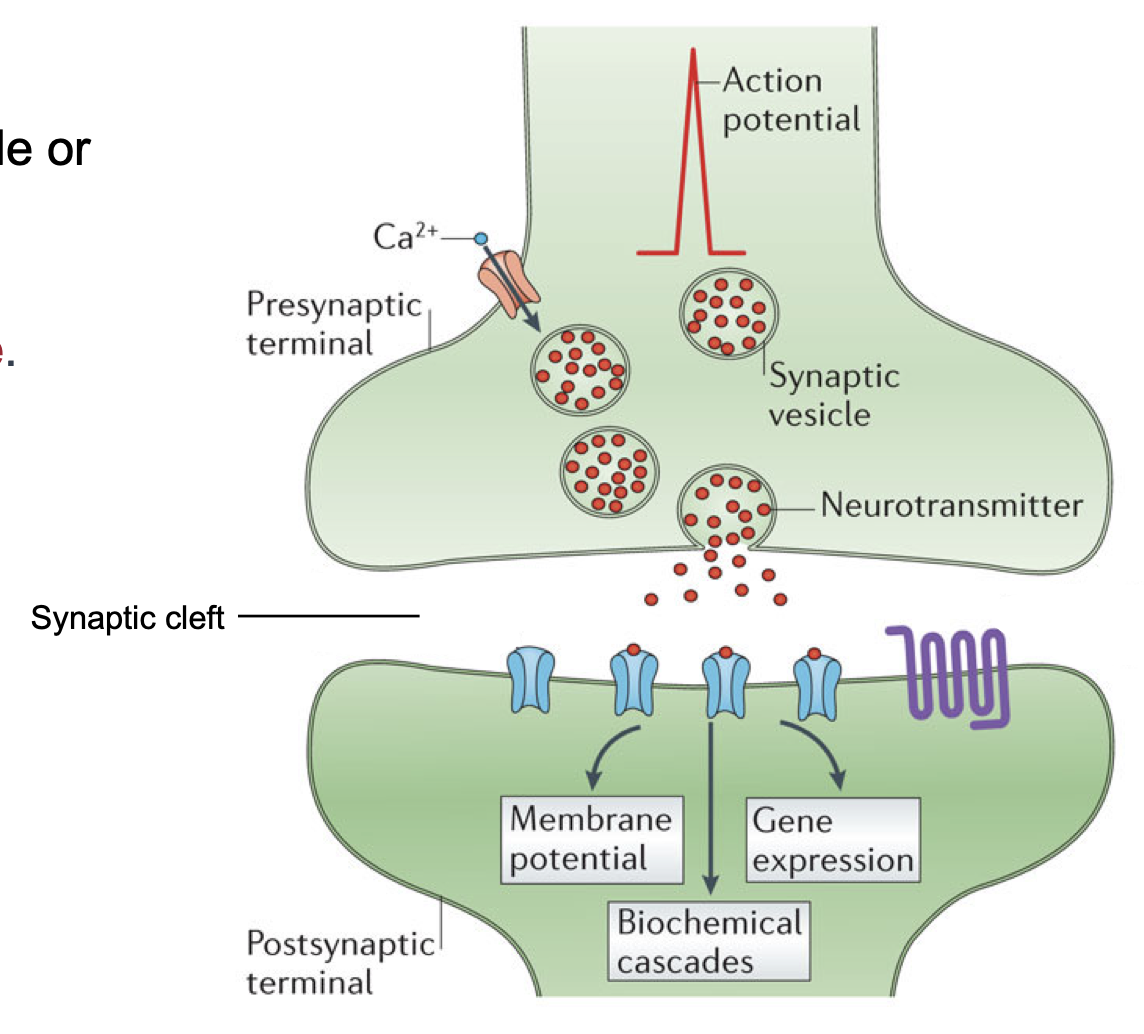
Paracrine signalling
Local communication between cells close together
Release of neurotransmitters from one cell which diffuse to the next cell
Autocrine Signalling
Chemical signals released by a cell bind to the receptors on the same cell
Endocrine signalling
Chemical signals released by endocrine cells into the circulatory system to communicate with distant target organs.
Chemical Synapse
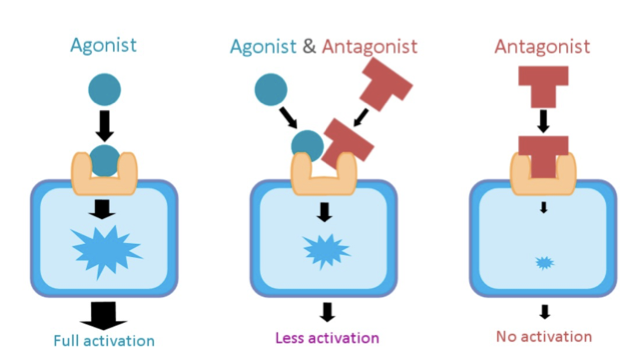
Exogenous VS Endogenous
Endogenous means the NT was naturally produced within the body
Exogenous means it was not produced in the body and they can be
Agonists bind to the receptor and mimic the effects of natural endorphins
Antagonists bind and block the receptor but do not activate the response.
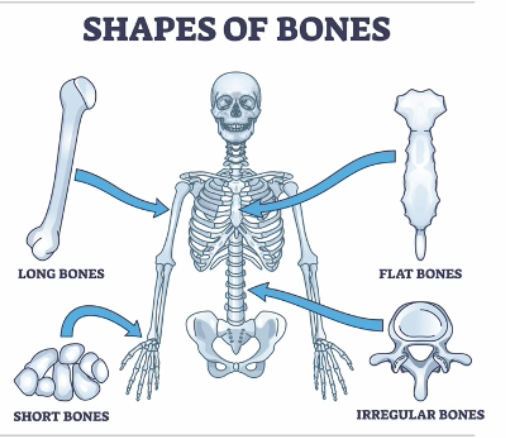
Shapes of bones
Structure of a Bone
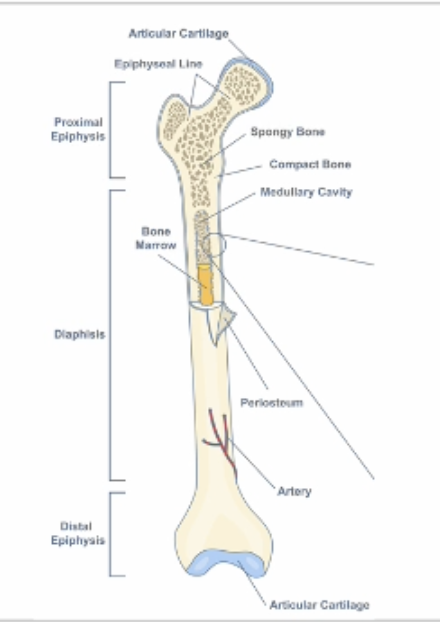
Anatomically, a bone can be divided into the diaphysis, with the epiphysis on either end.
The surface of the bone is covered by the periosteum, a dense fibrous connective tissue for protection.
Ends of the bone, where it forms a joint with another bone, are covered with articular cartilage.
Mineralisation hardens bone matrix
Ligaments connect bone to bone while tendons connect bone to muscle.
Bones help maintain calcium homeostasis and hematopoiesis (making red blood cells)
Components
Calcium phosphate: in the form of hydroxyapatite crystals
Collagen fibres: for structural support and strength
Bone cell: to build, maintain or breakdown bone as needed
Ground substance: for bone growth and maintenance
Compact Bone
Dense and strong.
Composed of Haversian systems (osteons) – cylindrical units made of concentric layers of bone matrix.
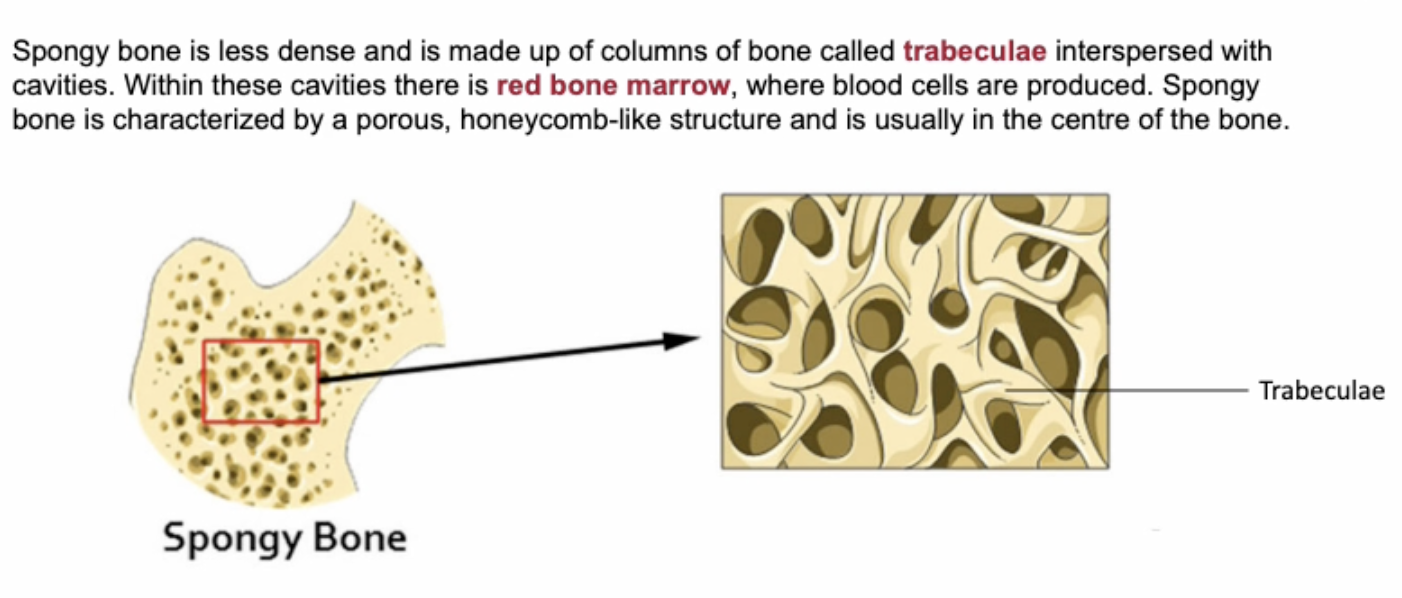
Spongy Bone
Less dense, with a pourous honeycomb structure
Columns called trabeculae interspersed with cavities
In cavities there is red bone marrow (site of haematopoiesis) where red blood cells are produced
Usually the center of the bone
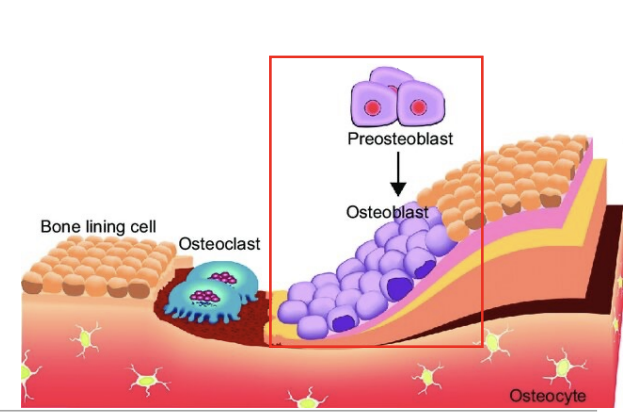
Osteoprogenitor Cells & Osteoblasts
Osteoprogenitor Cells
In bone tissue
Baby osteoblasts formed from stem cells in the red bone marrow
Osteoblasts
Build bone by secreting collagen and bone matrix until completely surrounded.
Calcifies the bone matrix
Osteocytes
When an osteoblast is completely surrounded by bone matrix it turns into an osteocyte.
Sits in a hole called a lacuna and extends out to detect pressure
Maintain bone integrity
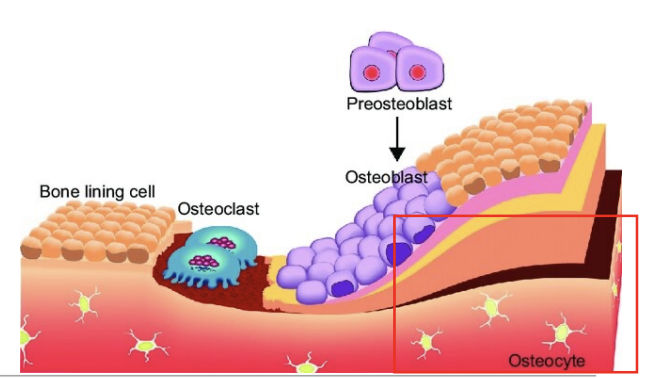
Osteoclasts
Break down bone
Secrete enzymes that digest bone
Form a pit called Howships lacuna
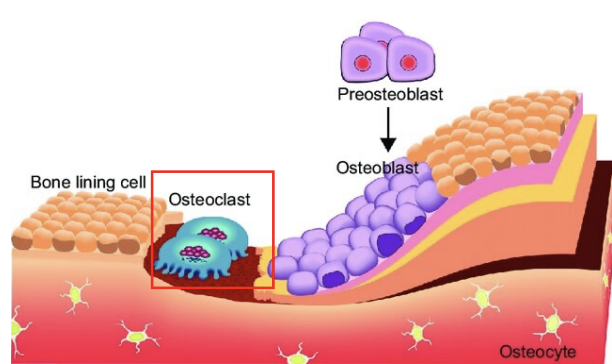
Bone Lining Cells
Derived from osteoblasts
Line the surface of the bone that is not being remodelled.
Maintenance and nutritional support of osteocytes
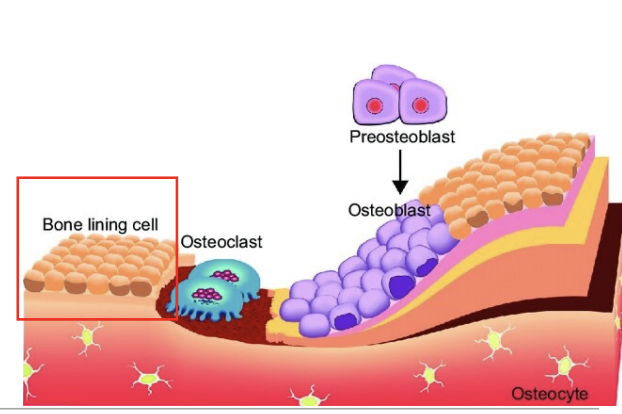
Bone Remodelling Process
Activation: Osteoclasts are attracted to the surface of the bone due to mechanical stress to the bone, damage, or hormonal signals.
Resorption: Osteoclasts begin to secrete enzymes that start to break down the bone, forming a small pit.
Reversal: Additional cells from the bloodstream remove debris from the area and attract osteoblasts to the area.
Formation: Osteoblasts lay down new bone matrix.
Quiescence: Osteoblasts become osteocytes within the bone matrix.
Hormones Involved in Bone Remodelling
Parathyroid hormone (PTH): Stimulates osteoclasts to break down bone and increase blood calcium levels
Calcitonin: Inhibits osteoclasts to reduce blood calcium levels
Sex hormones (Estrogen and Testosterone): Promote osteoblasts to build bone and suppress osteoclast activity
Vitamin D: Enhances calcium absorption from the gut and promotes bone mineralisation.
Skeletal Muscle
Individual skeletal muscles are called myocytes which are bundled into fascicles.
Fascicles are connected by connective tissue to form a whole muscle.
Connective tissue extends beyond the end of muscle fibres to form tendons.
Tendons are non-contractile elastic tissue structures that attach muscle to bone.
Muscle tension is transmitted to bone as the muscle pulls on the tendon → this is the basis of movement.
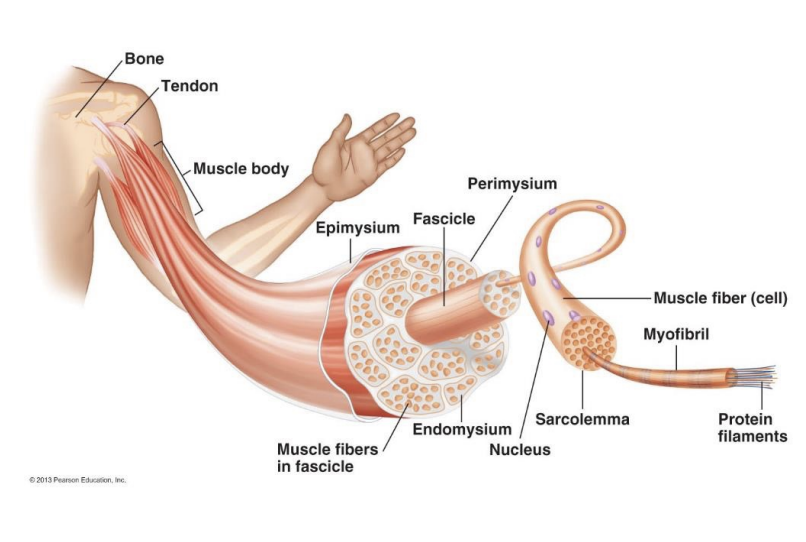
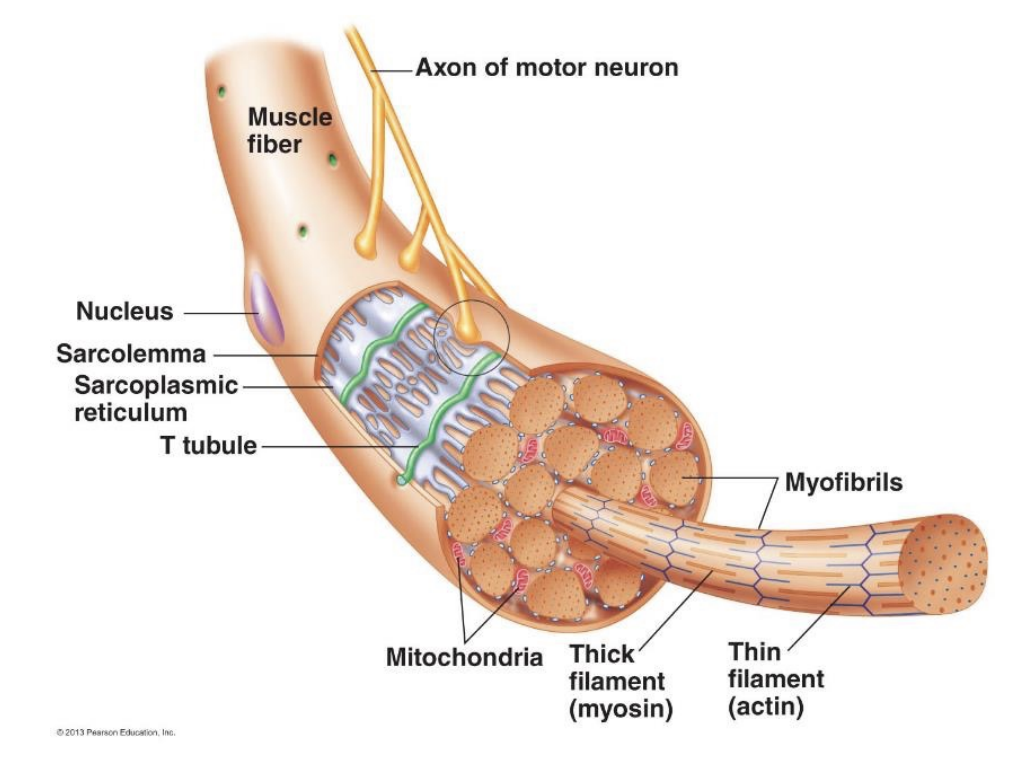
Myocytes
Muscles are made up of individual muscle cells called myocytes, which are composed of many bundles of myofibrils.
Cylindrical (50 micrometres), elongated to the length of the muscle.
Numerous mitochondria due to the high energy demand.
Have bundles of myofibrils that contain two types of protein filaments
Thick (15 micrometres) - myosin
Thin (7 micrometers) - actin
Organised into a chain of contractile units called sarcomeres, which are the functional units (contractile elements) of skeletal muscle.
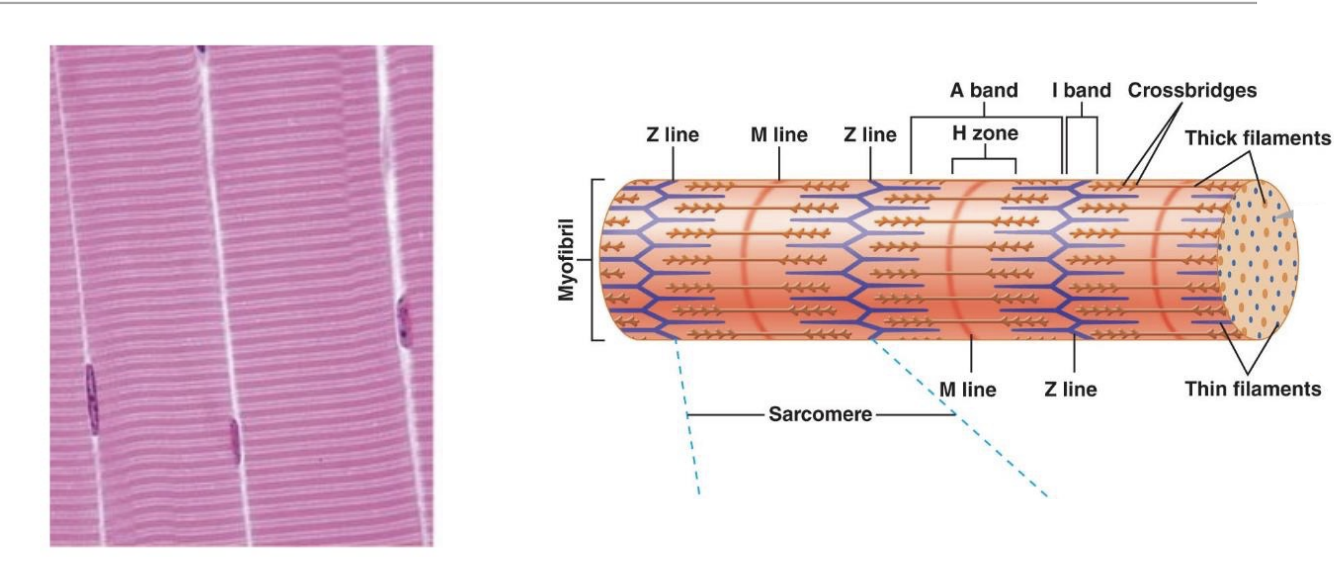
Sarcomere
Z line: Band of structural proteins that anchors the filaments and defines the boundary of the sarcomere
A band: Made of thick filaments with overlapping bits of thin filaments
H zone: Lighter area within the middle of A band where thin filaments do not reach.
M line: Extends vertically down the middle of A band within the centre of H zone
I Band: Remaining thin filaments that do not project into A band.
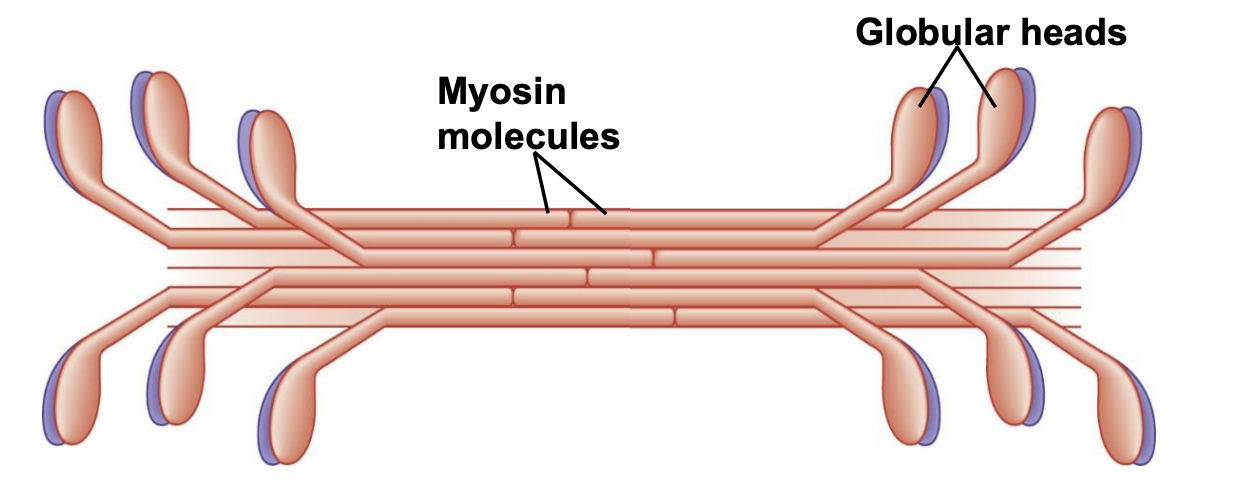
Thick Filaments
Parallel (half one direction, half other direction) myosin molecules
Globular heads protude along the filament forming the bridges that bind to thin fillaments.
Two important binding sites
Actin-Binding site
Myosin ATPase site
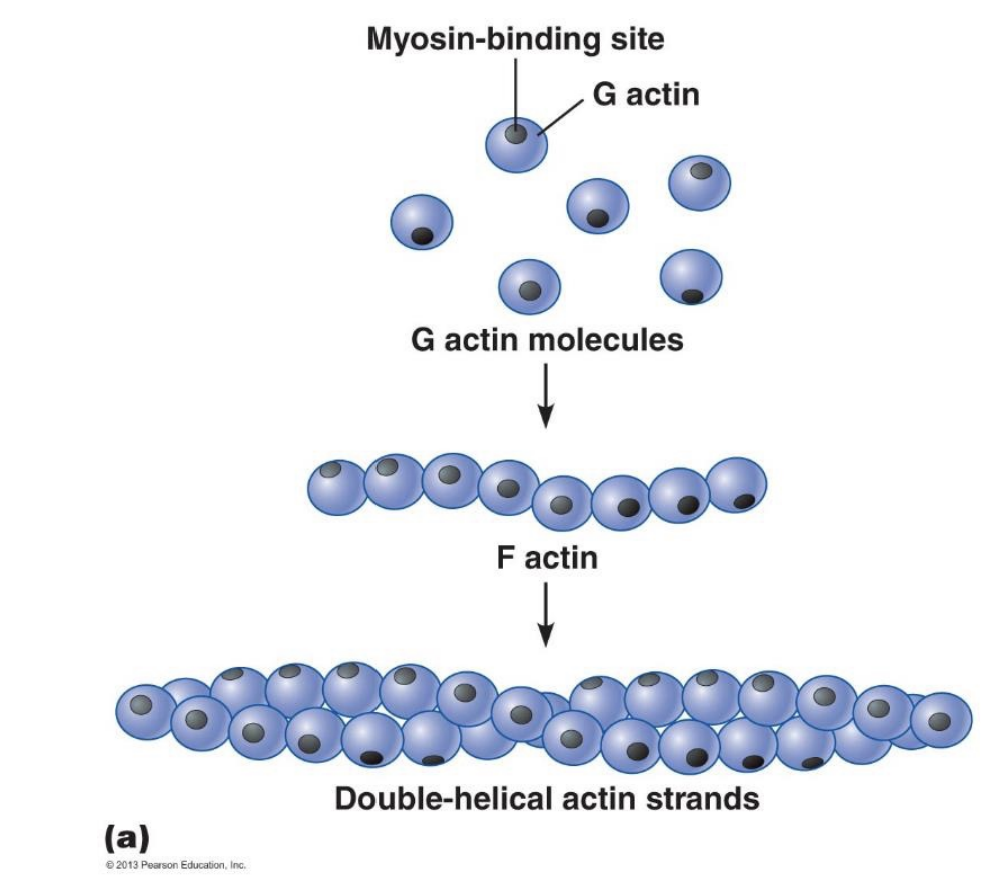
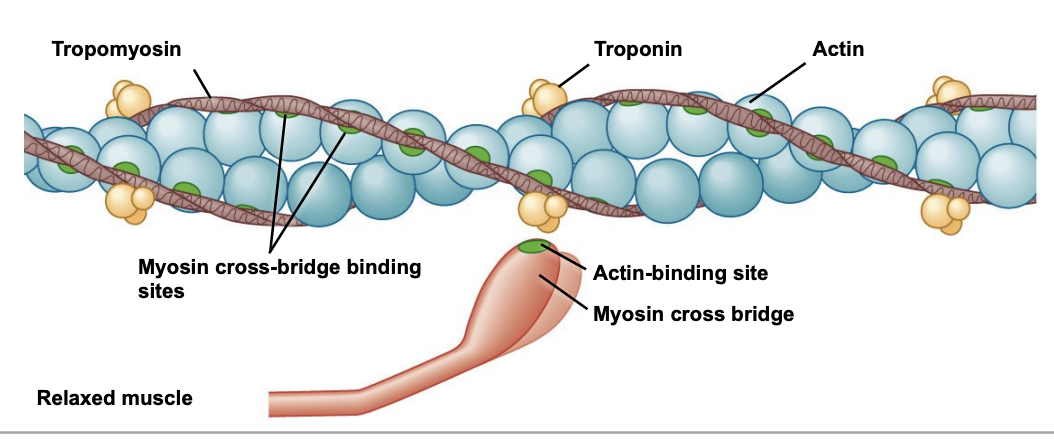
Thin Filaments
Two chains of actin molecules.
Globular actin monomers (G actin) polymerise to form a fibrous chain (F actin).
2 chains are twisted together into a double helix.
Actin interacts with the globular myosin head on the thick filaments
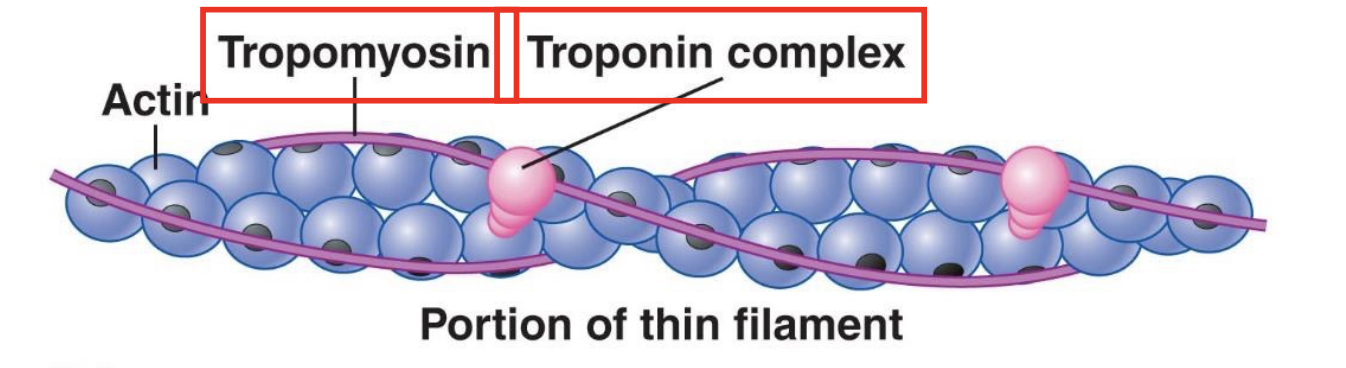
Tropomyosin & Troponin
Tropomyosin is a long fibrous molecule that extends over numerous actin monomers and physically blocks the myosin-binding site on actin. •
Troponin binds to both tropomyosin and actin and maintains tropomyosin in its position.
Both lie across actin and enable or disable the contraction mechanism. In relaxed muscle, they cover myosin-binding sites and block crossbridge attachment.
Transverse tubules
Extensions of the plasma membrane that that penetrate deep into the muscle cell.
Action potential on sarcolemma spreads down into the T-tubule.
Spread of action potential down a T-tubule triggers release of Ca2+ from sarcoplasmic reticulum into cytosol.
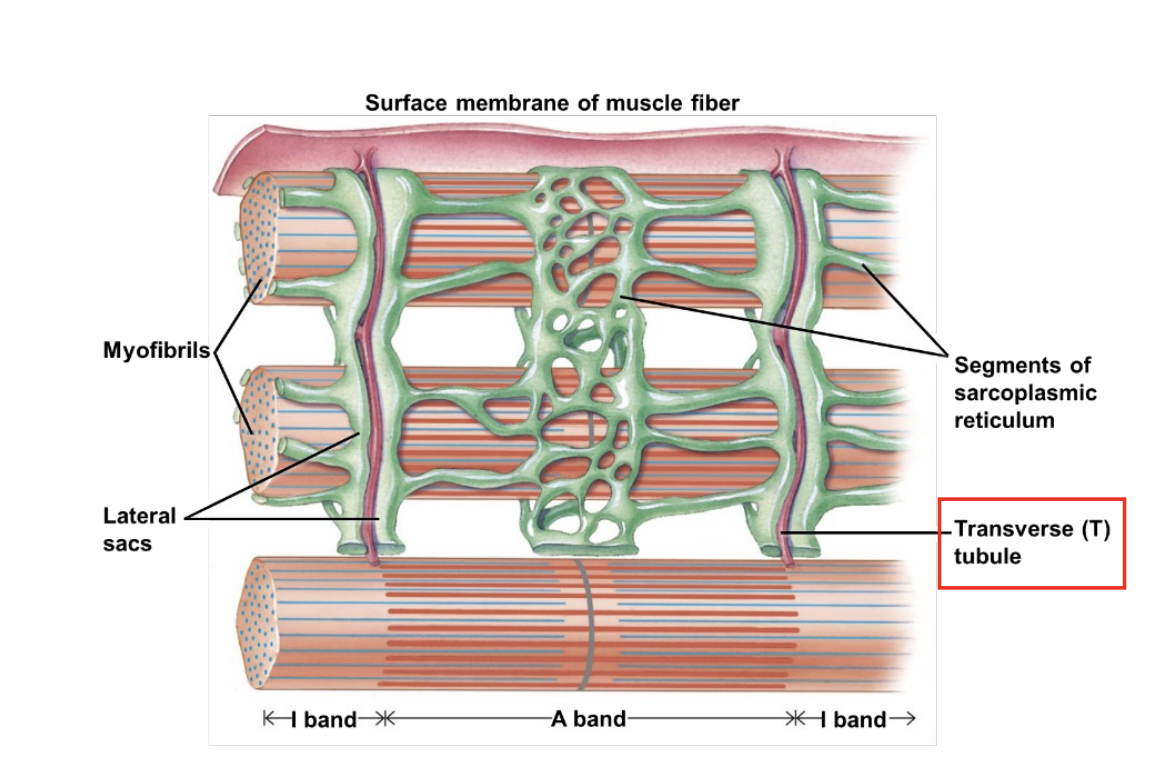
Sarcoplasmic reticulum
Modified endo plastic reticulum
Network of interconnected compartments surrounding myofibril
The ends of each segment are expanded to form lateral sacs next to the adjacent T-tubules
Forms a triad (T-tubule + lateral sacs)
Stores and releases calcium to promote muscle contraction when activated.
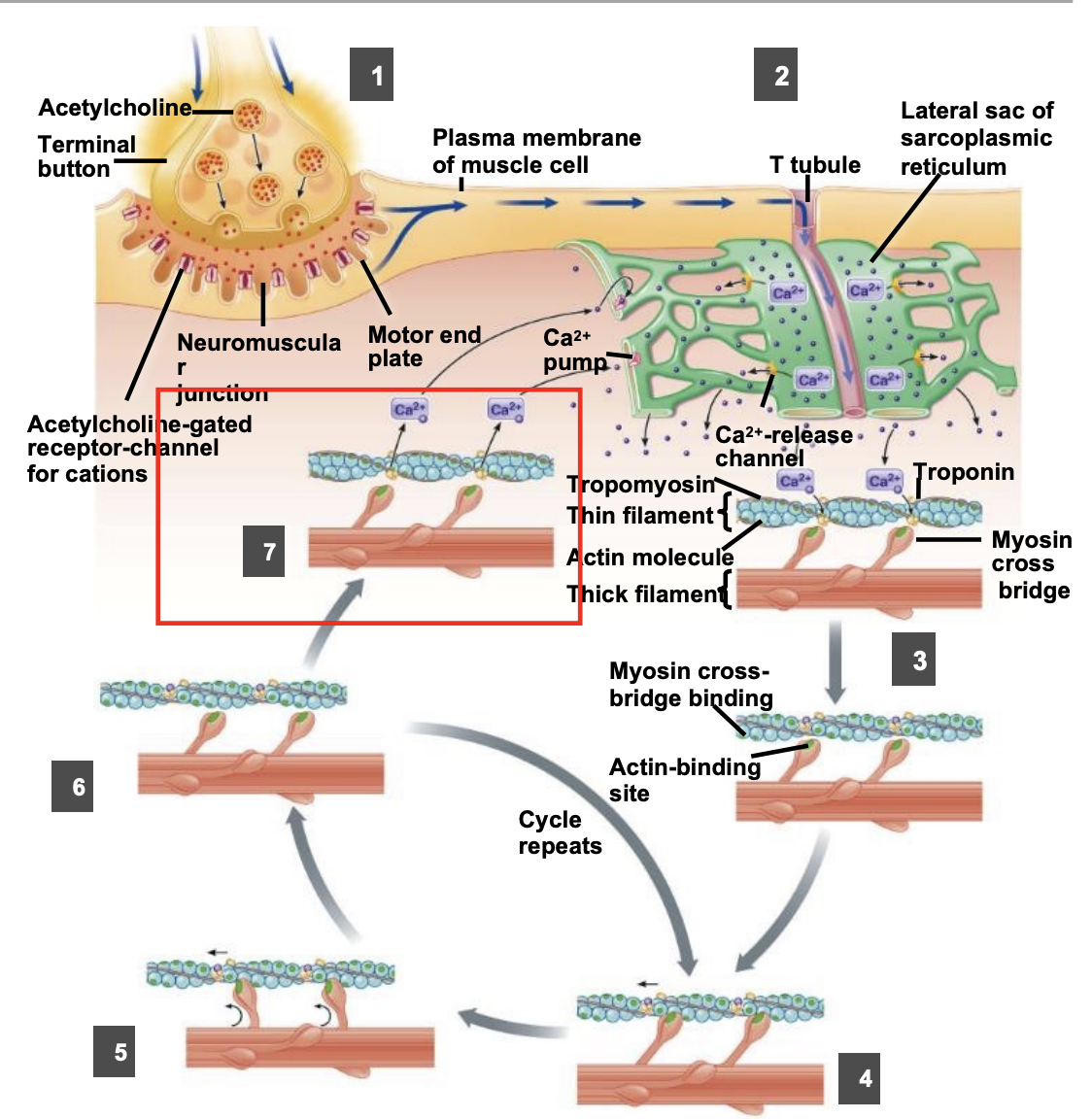
Excitation-Contraction Coupling
When the muscle fibre is relaxed and there is no excitation from the nervous system (no Ca2+ released and no cross bridge binding)
The troponin-tropomyosin complex physically converts the myosin binding site on actin.
When it is excited and an AP is generated in the muscle, Ca2+ is released from the sarcoplastic reticulum.
Calcium binds with troponin, pulling the troponin-tropomyosin complex aside to expose the myosin binding site on actin.
Myosin head binds to actin and triggers a power stroke that pulls thin filament inward during a contraction
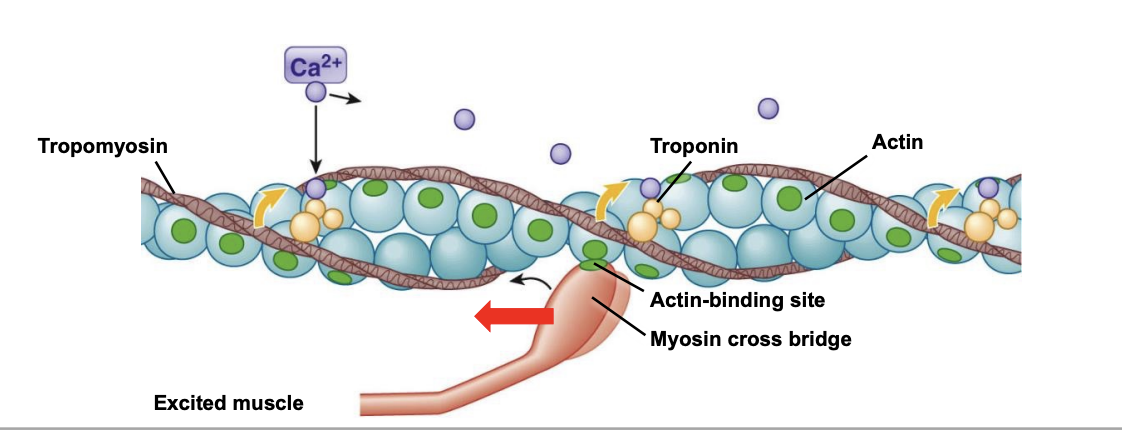
Power Stroke
Myosin binds to actin in crossbridge formation, triggering a power stroke of the myosin head.
The myosin head pulls the thin filament inwards
Crossbridge detaches, returning to original formation after the power stroke.
Crossbridge binds to a more distal actin molecule.
Repetition of this slowly slides the thin filaments inward.
Insufficient ATP (such as after death) results in the myosin head sticking to the thin filaments, resulting in rigor mortis.
Process of Excitation-Contraction Coupling
Action potential arrives at NMJ and stimulates release of ACh, triggering an action potential in the muscle.
Muscle action potential spreads along the cell membrane and down the T tubule, triggering the release of Ca2+ from the sarcoplasmic reticulum into the cytosol.
Ca2+ binds to troponin and causes tropomyosin to change shape, physically moving it away from its blocking position.
This uncovers the binding sites on actin for the myosin cross bridges.
Myosin cross bridges attach to actin at the exposed binding sites triggering the cross bridge to bend, pulling the thin filament over the thick filament toward the centre of the sarcomere.
The power stroke is powered by ATP.
After the power stroke, the cross bridge detaches from actin (if sufficient ATP). ATP hydrolysis cocks the myosin head. If sufficient Ca2+ is still present, this will repeat.
When action potentials stop, Ca2+ is pumped back into the SR and tropomyosin moves back to its original position, blocking myosin crossbridge binding sites on actin.
Contraction stops and the thin filaments passively slide back to their original relaxed positions.
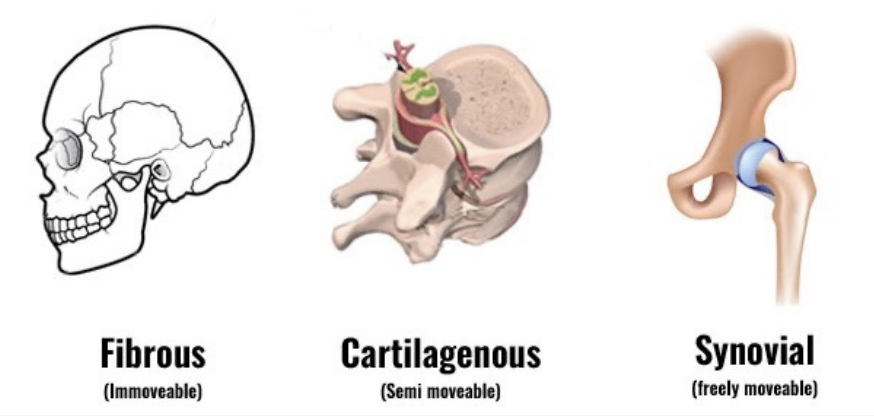
Functional classifications of joints
Blood & Plasmsa
Bloods (5.5L) is a fluid, nearly half its volume is composed of cells.
The most numerous cells are erythrocytes (red blood cells) 2.5L and they lack nuclei, mitocondria and ribosomes.
Their contribution is called haematocrite and is determined by centrifuging a blood sample (%)
Leukocytes (white blood cells) are also found in other tissues
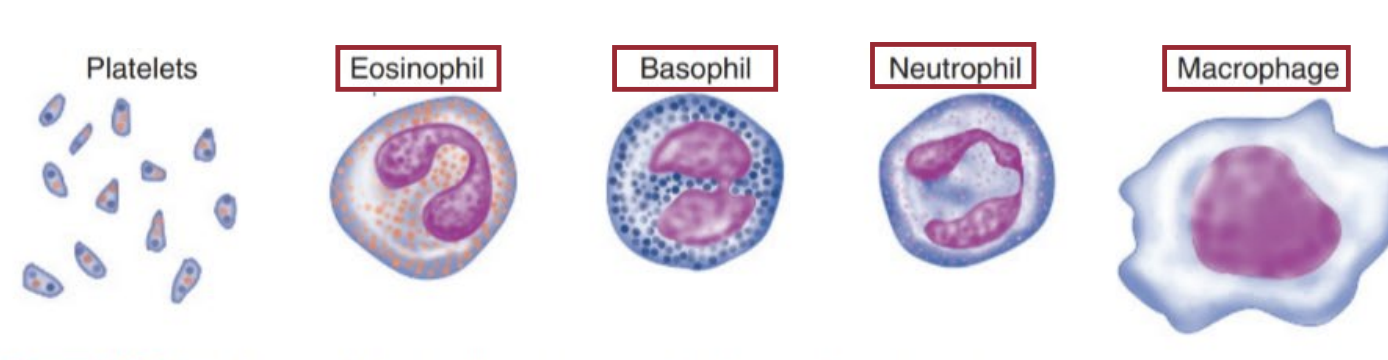
Platelets are cell fragments from parts of large bone-marrow cells (megakaryocytes) that broke off that help blood clotting and have no nucleus.
Plasma (liquid 3L), is made up of water containing dissolved proteins, electrolytes, and other solutes.
Artery VS Vein
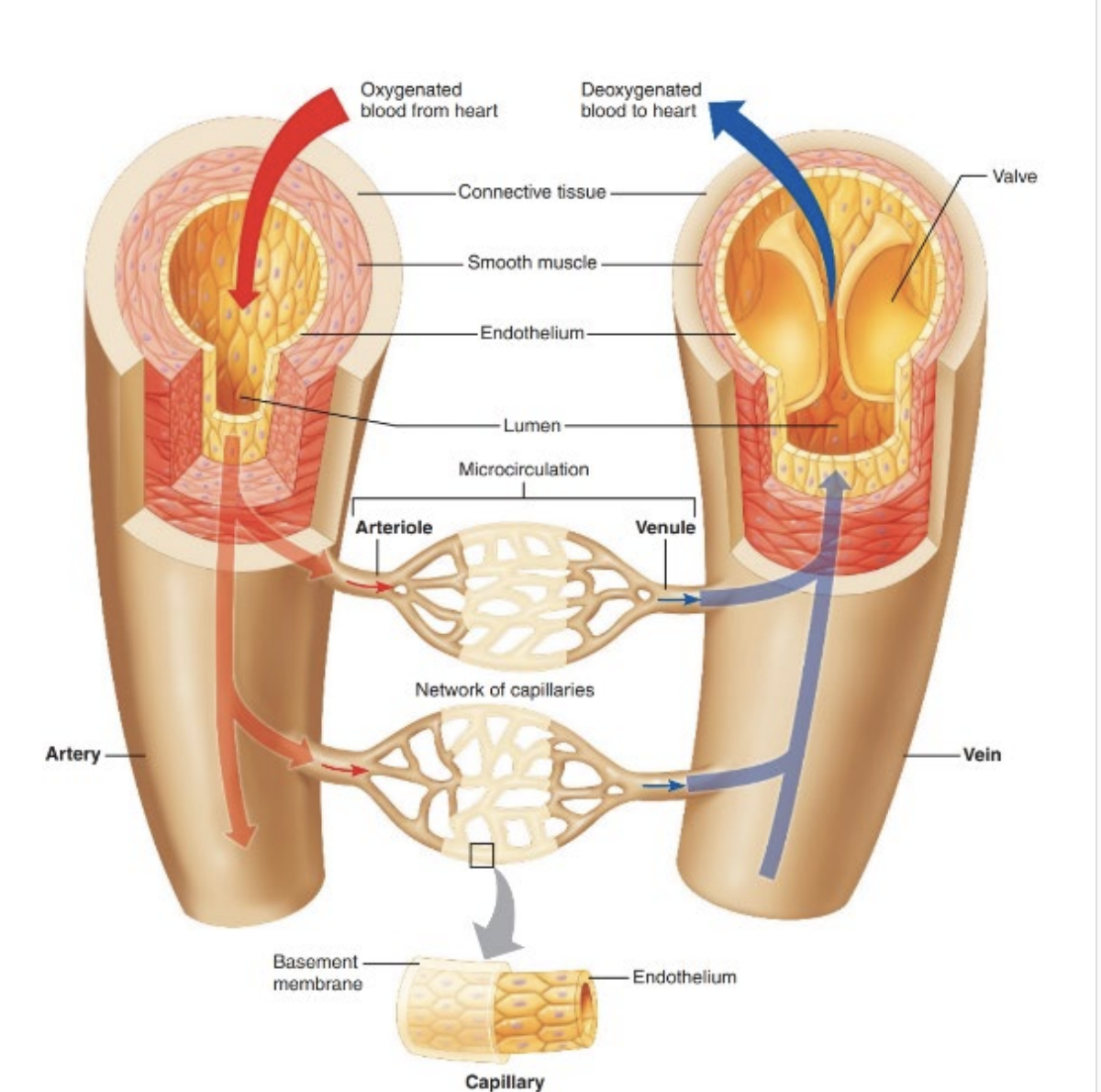
Arterioles
Arteries branch into arterioles
Atrioles lead to capillaries or metarterioles, which then go to capillaries
Walls are elastic & have lots of smooth muscle in rings around the atriole
Smooth muscle can contract or relax, changing diameter to regulate resistance to blood flow
Capillaries
Continuous capilaries are made of endothelial cells
Fenestrated capillaries have pores for the continuous exchange of nutrients, waste and substances between the capillaries and tissues. e.g. kidneys, intestines, pancreas and endocrine glands
Structure of the heart
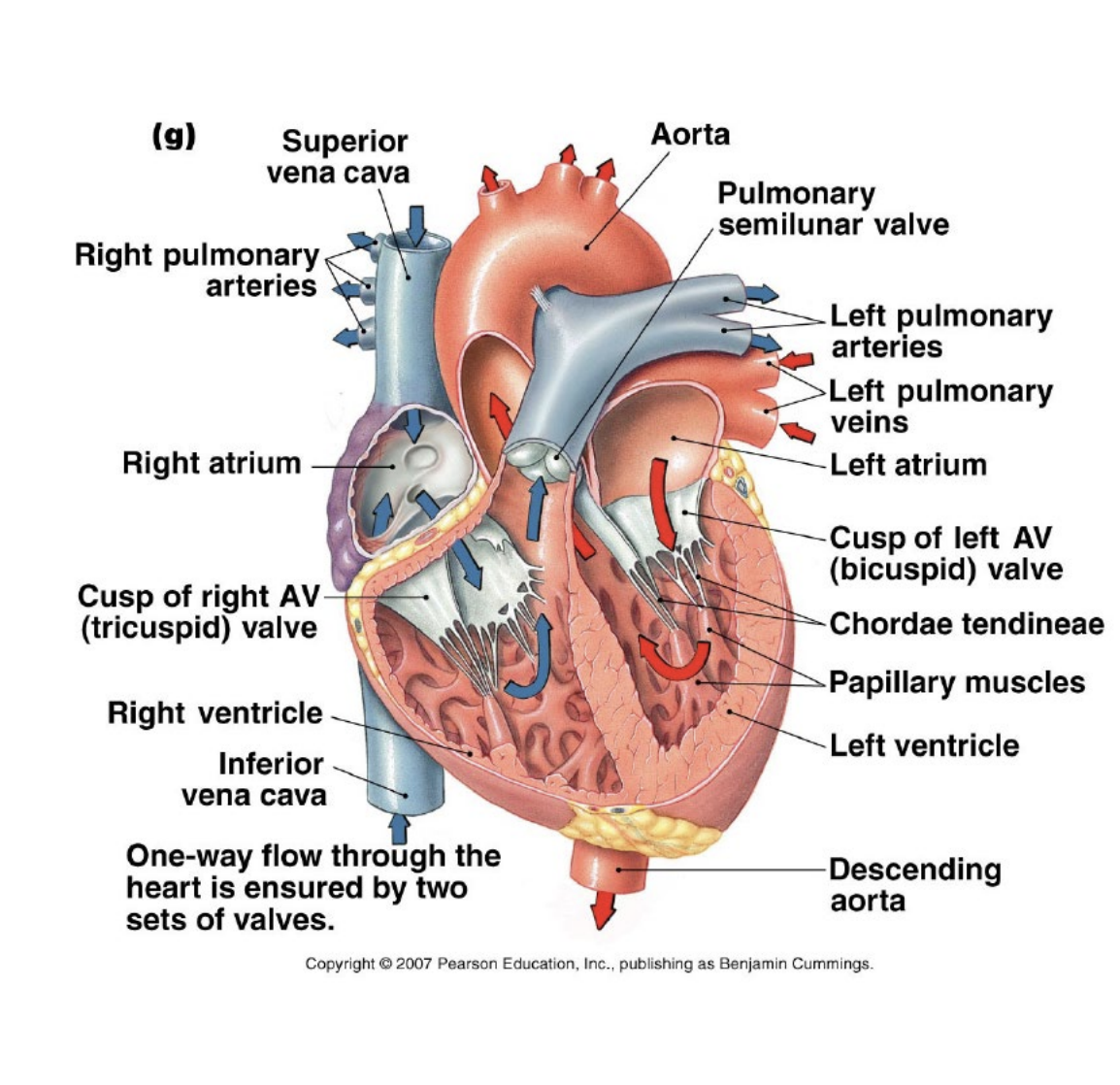
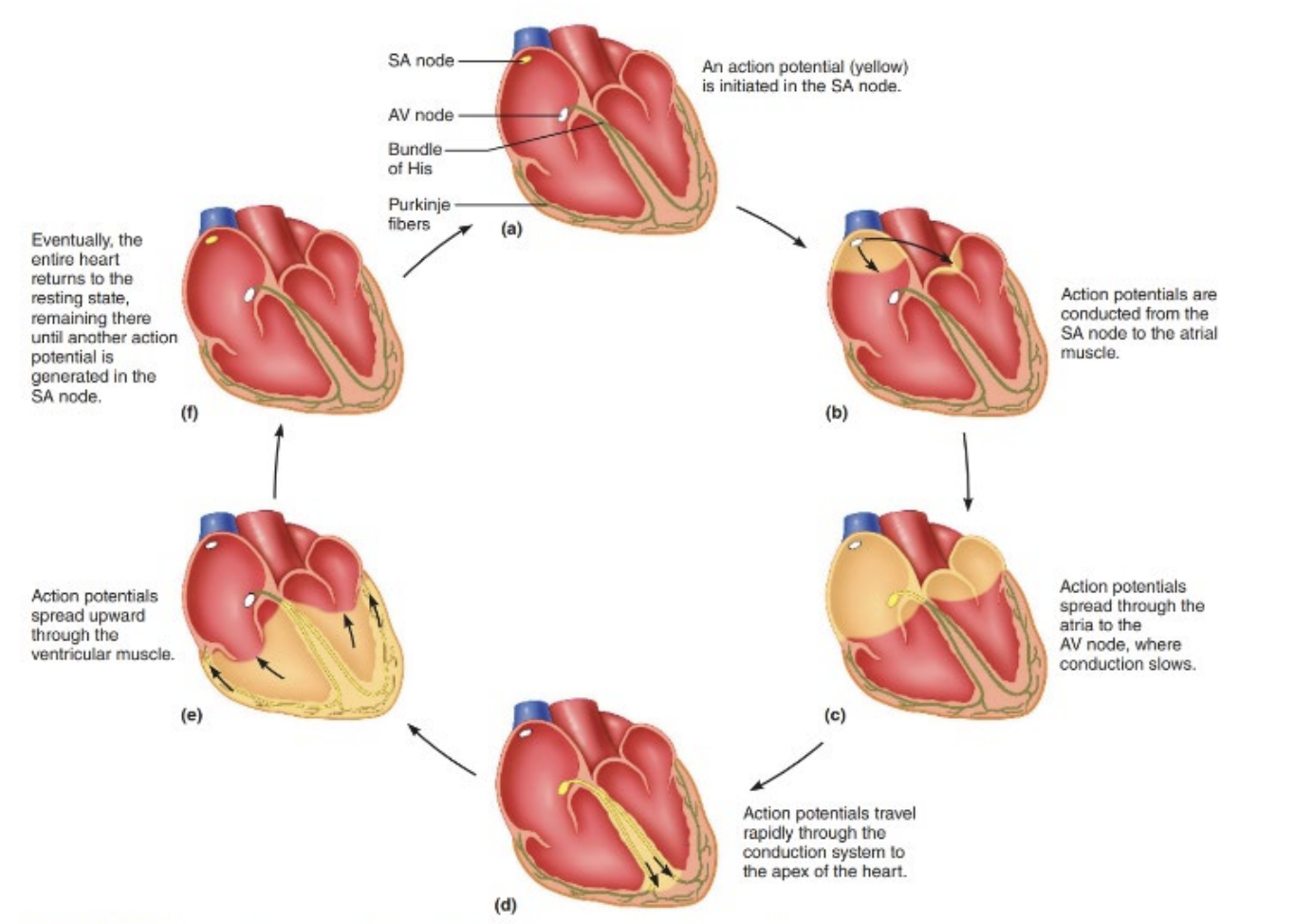
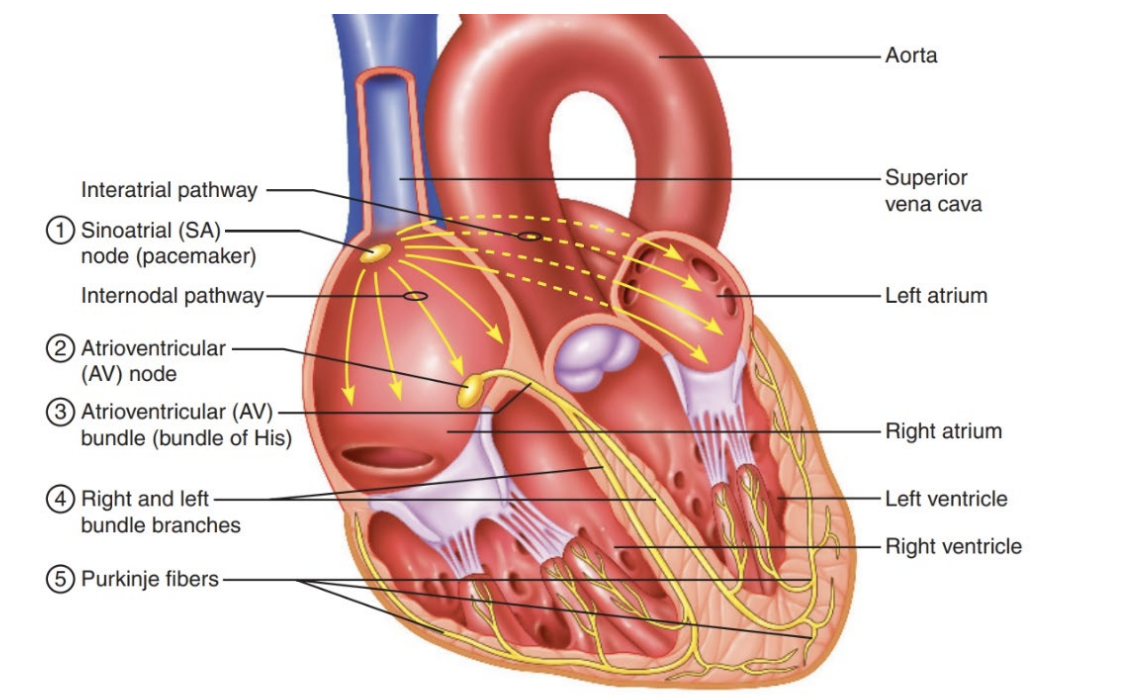
Conduction System of the Heart
Blood comes in via the atria
The atria contract and blood flows into the ventricles
Ventricles send blood into the body
Electrical activity in the heart is controlled by pacemaker cells
It starts in the sinoatrial node (pacemaker), which starts action potentials around the atria to the atrioventricular node.
The atrium contracts when it receives the AP
AV node holds the electrical signal for a little bit so the atrium has time to contract before spreading down the atrioventricular bundle. - HEARTBEAT
It then travels to the Purkinje fibres, which go to cardiac myocytes in the ventricles to contract
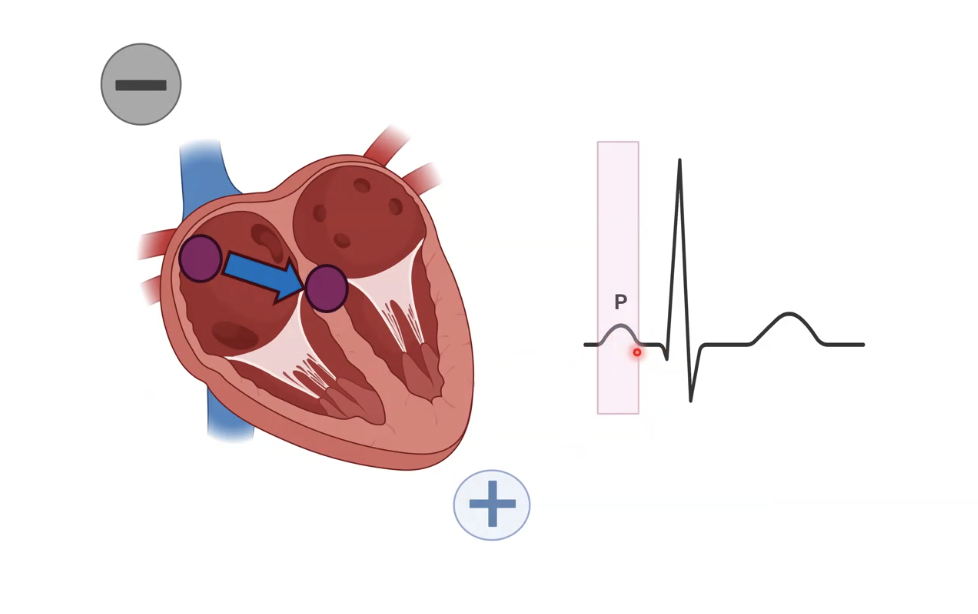
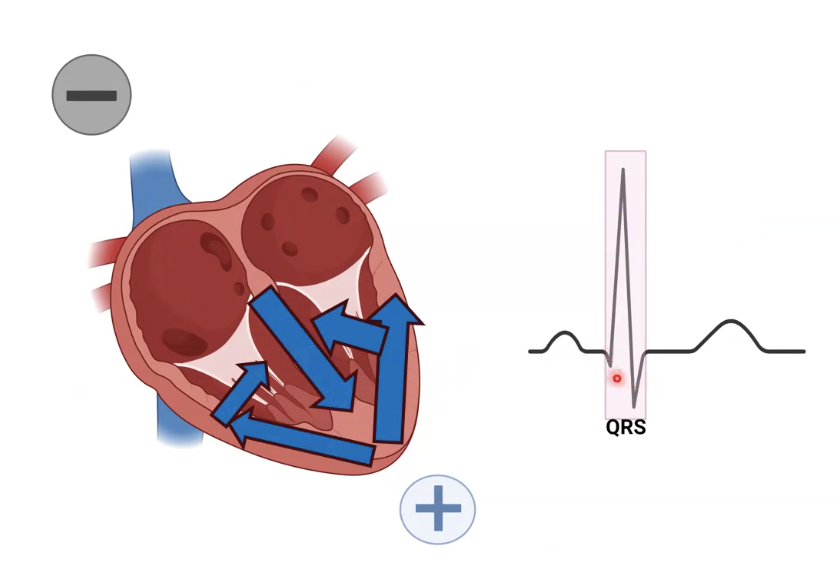
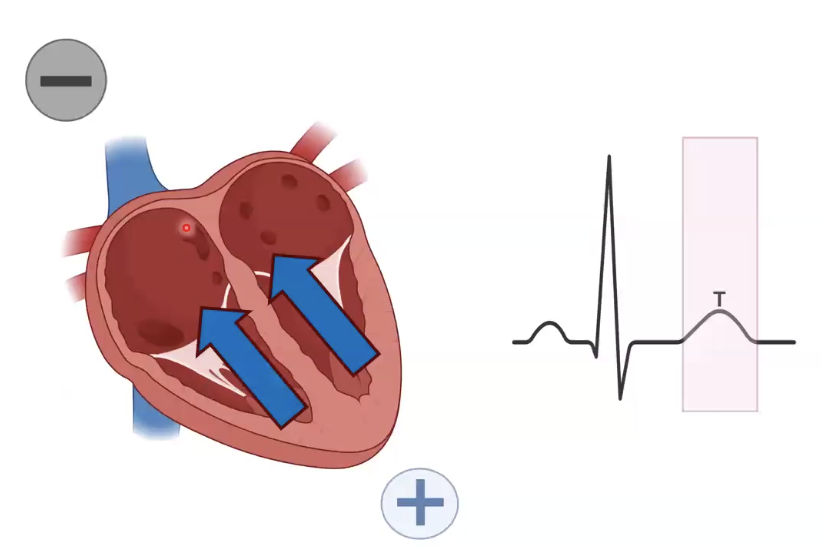
Electrocardiogram (ECG)
Records which way electrical currents go into the heart and each section relates to what is happening in the cardiac cycle.
Measures electrical activity of the heart.
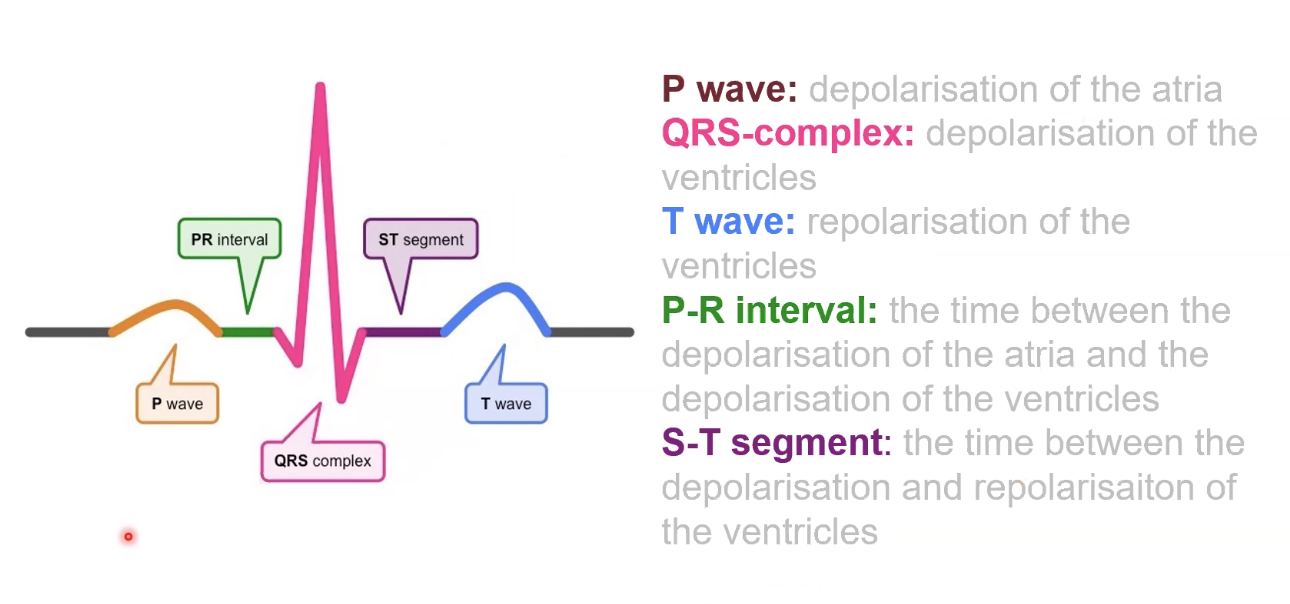
P wave
AP goes from SA node to AV node
QRS complex
Positive charge goes in several directions before contraction of ventricles.
Large due to more electrical activity.
T wave
Repolarisation of the heart.
Negative current going towards the negative electrode gives a positive bump.
Relaxes and resets for the next heartbeat.
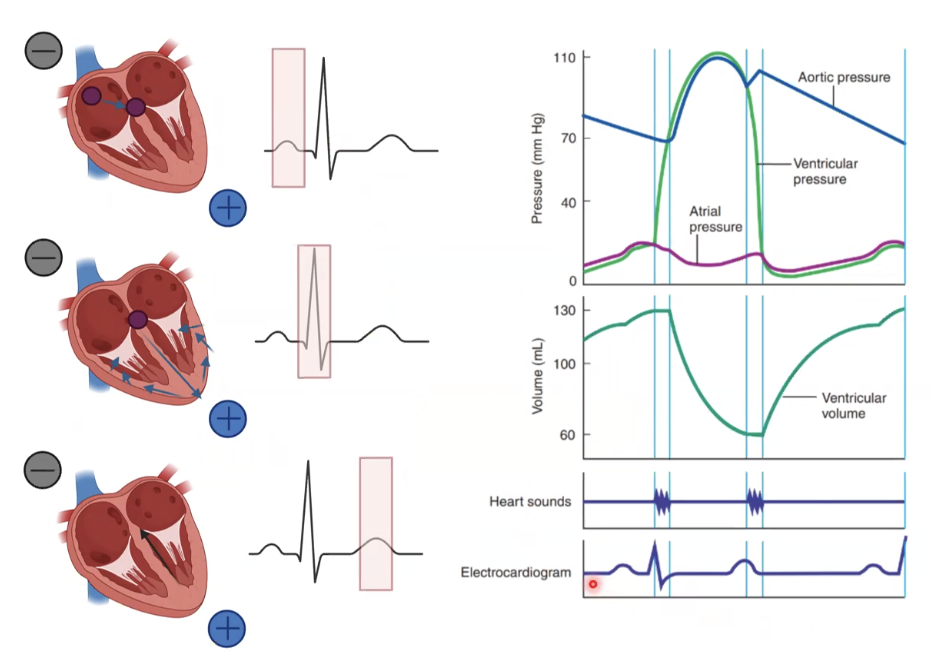
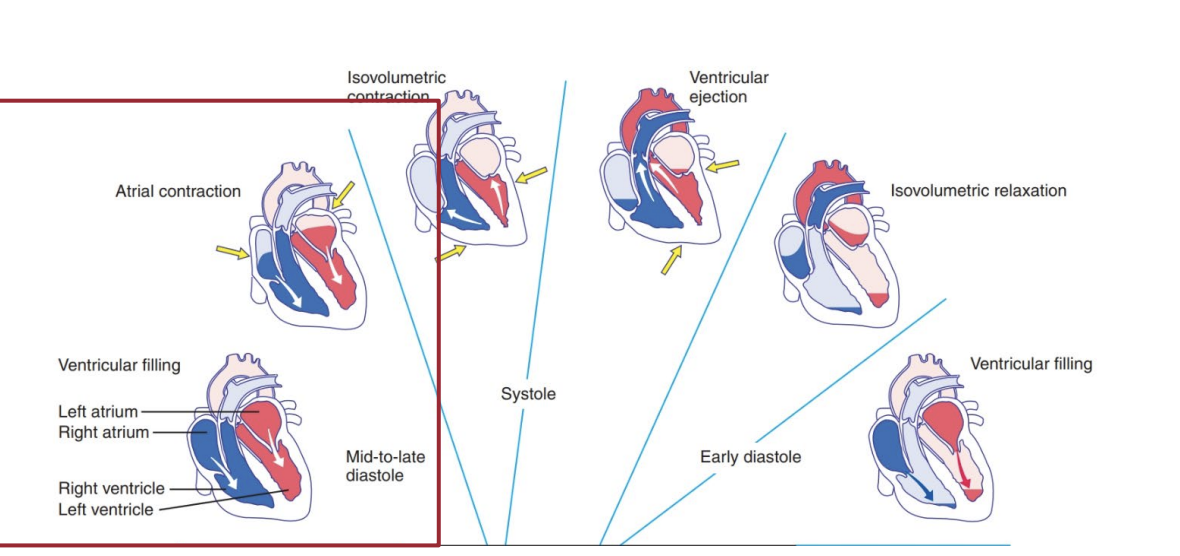
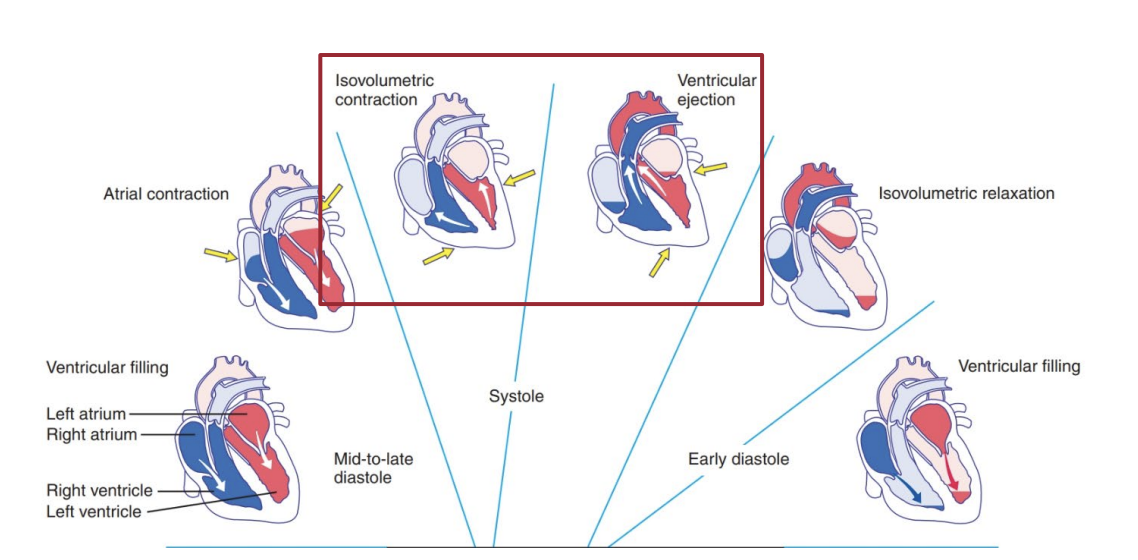
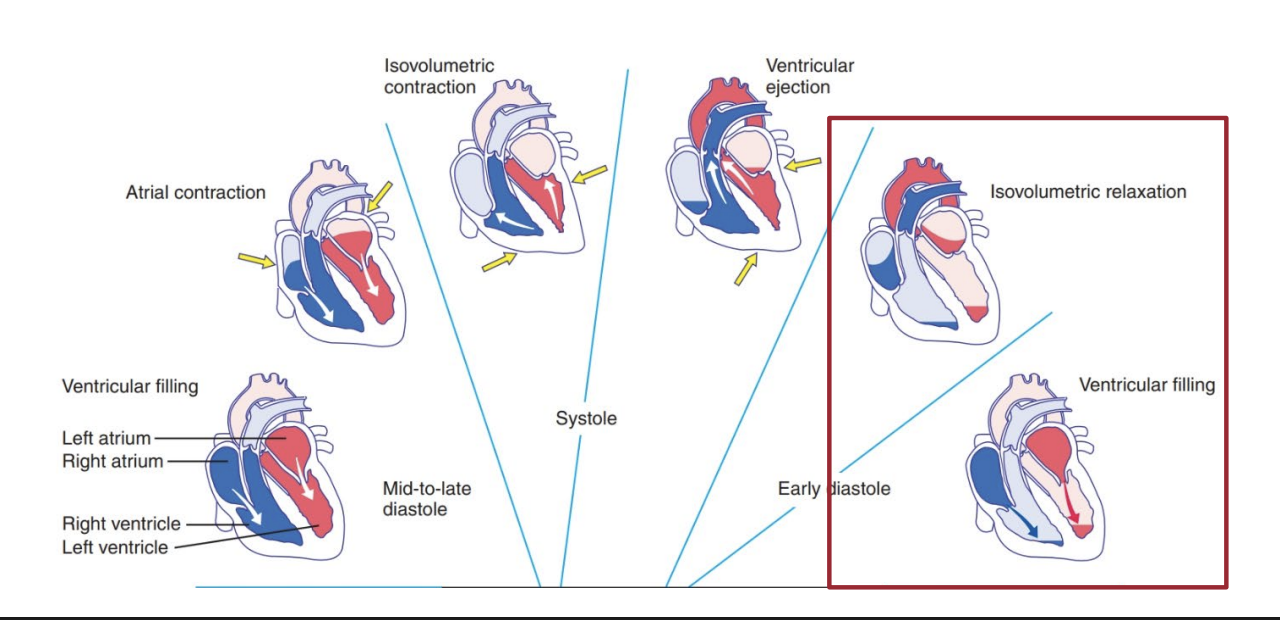
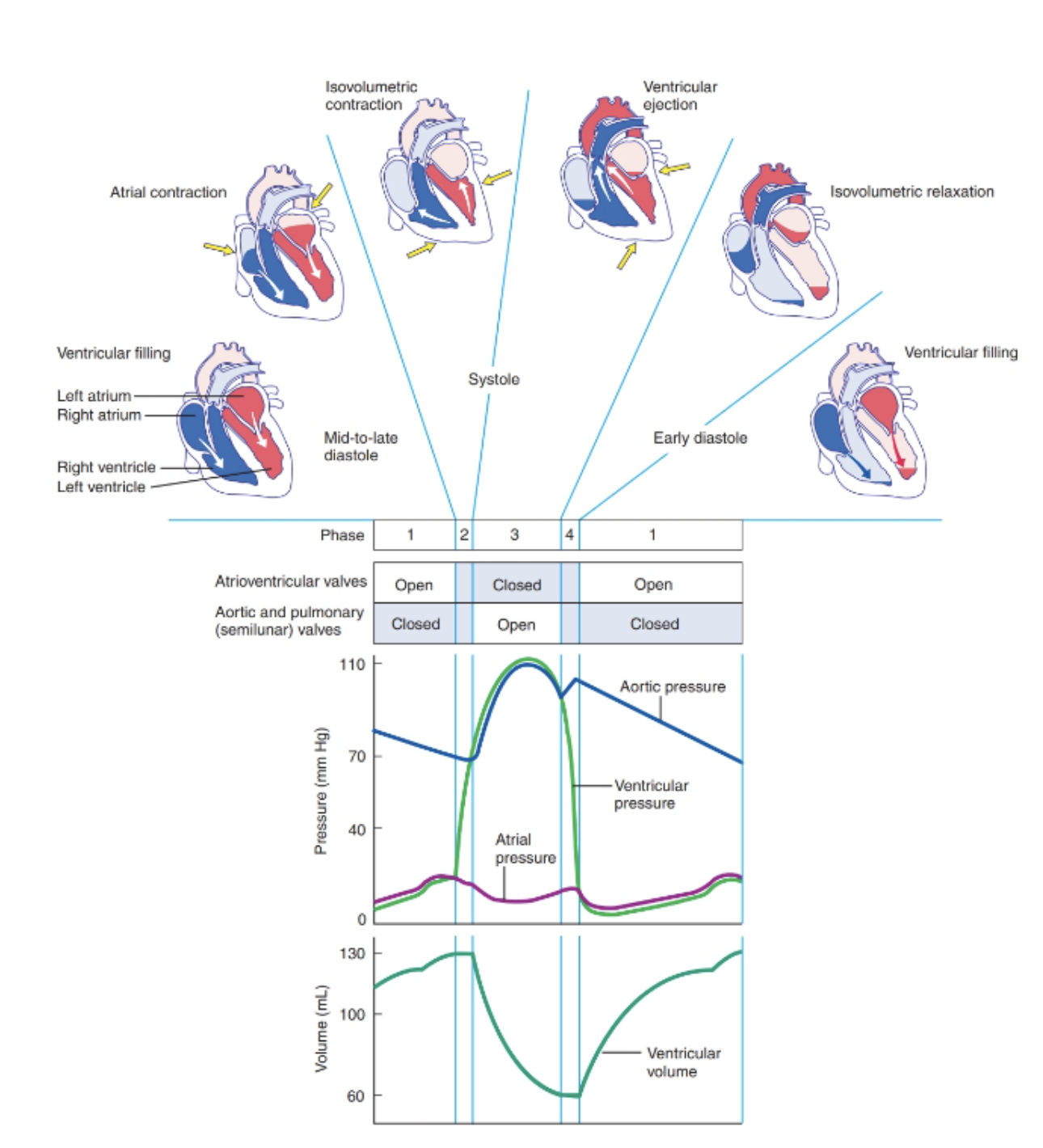
The Cardiac Cycle
Systole: When the heart contracts
Diastole: When the heart relaxes
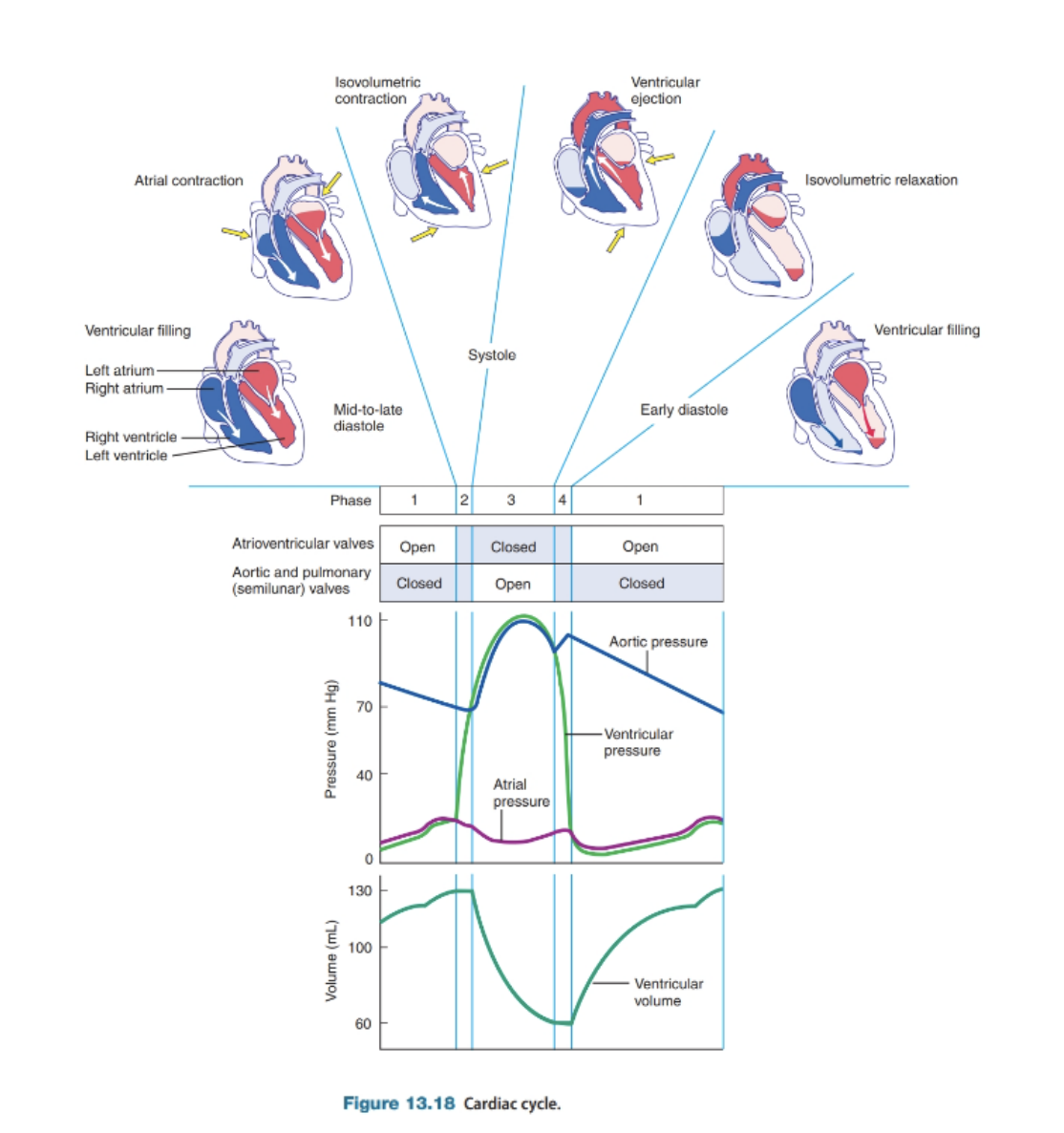
Ventricular Filling
Atria contracts
SA node sends an electrical signal that spreads across both atria, causing them to squeeze and push blood into the ventricles.
AV valves (tricuspid and bicuspid/mitral) are open so blood can flow freely
Ventricles passively receive blood while they’re relaxed.
Short - 0.1 seconds.
Ventricular Systole
Ventricles take over.
The electrical signal has now reached the AV node, traveled through the bundle branches and Purkinje fibers, and finally tells the ventricles to contract.
The AV valves snap shut, preventing backflow into the atria (lub sound in a heartbeat).
The semilunar valves (pulmonary and aortic valves) open, allowing blood to be ejected
Oxygen-poor blood goes to the lungs via the pulmonary artery.
Oxygen-rich blood goes to the body via the aorta.
Longer- 0.3 sec, because the ventricles need to build enough pressure to pump blood effectively.
Diastole
The heart muscle relaxes.
The semilunar valves close to stop blood from flowing backward (‘dub’ sound in a heartbeat).
The atria fill with blood, from the vena cava and pulmonary veins.
The AV valves open again, letting blood flow passively into the ventricles.
Longest - 0.4 seconds, gives the heart time to refill before the next beat.
Cardiac Output
How much blood the heart pumps a minute
Cardiac output = Heart Rate x Stroke Volume
CO = HR x SV
Stroke Volume is how much blood is ejected with each heart beat
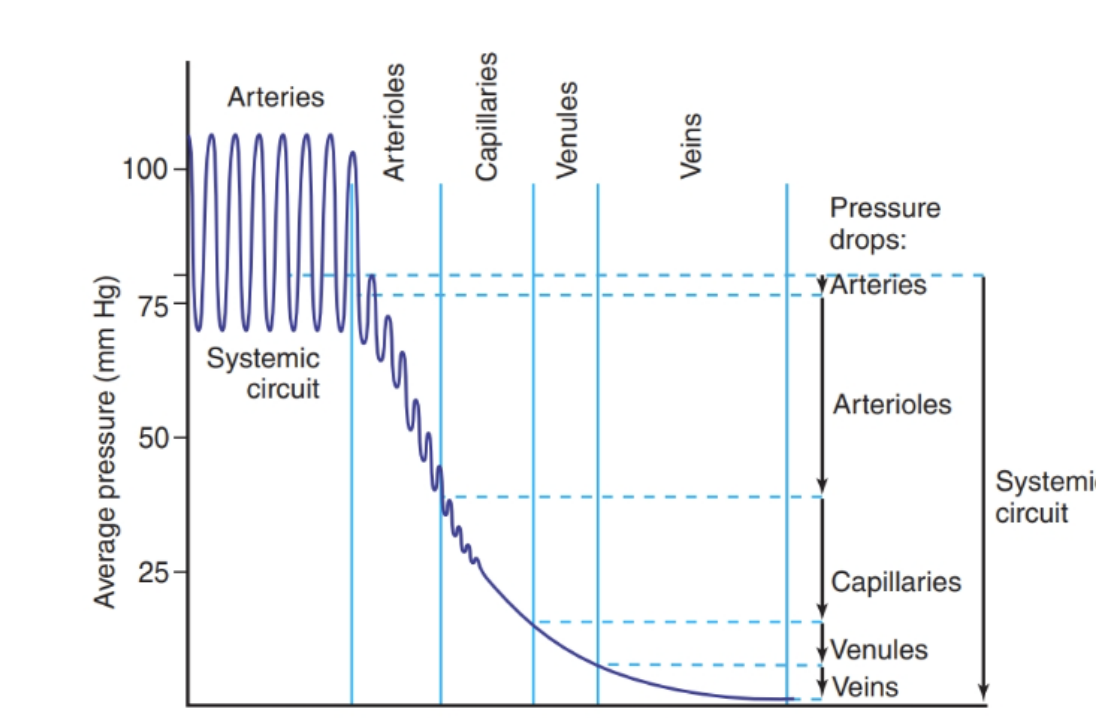
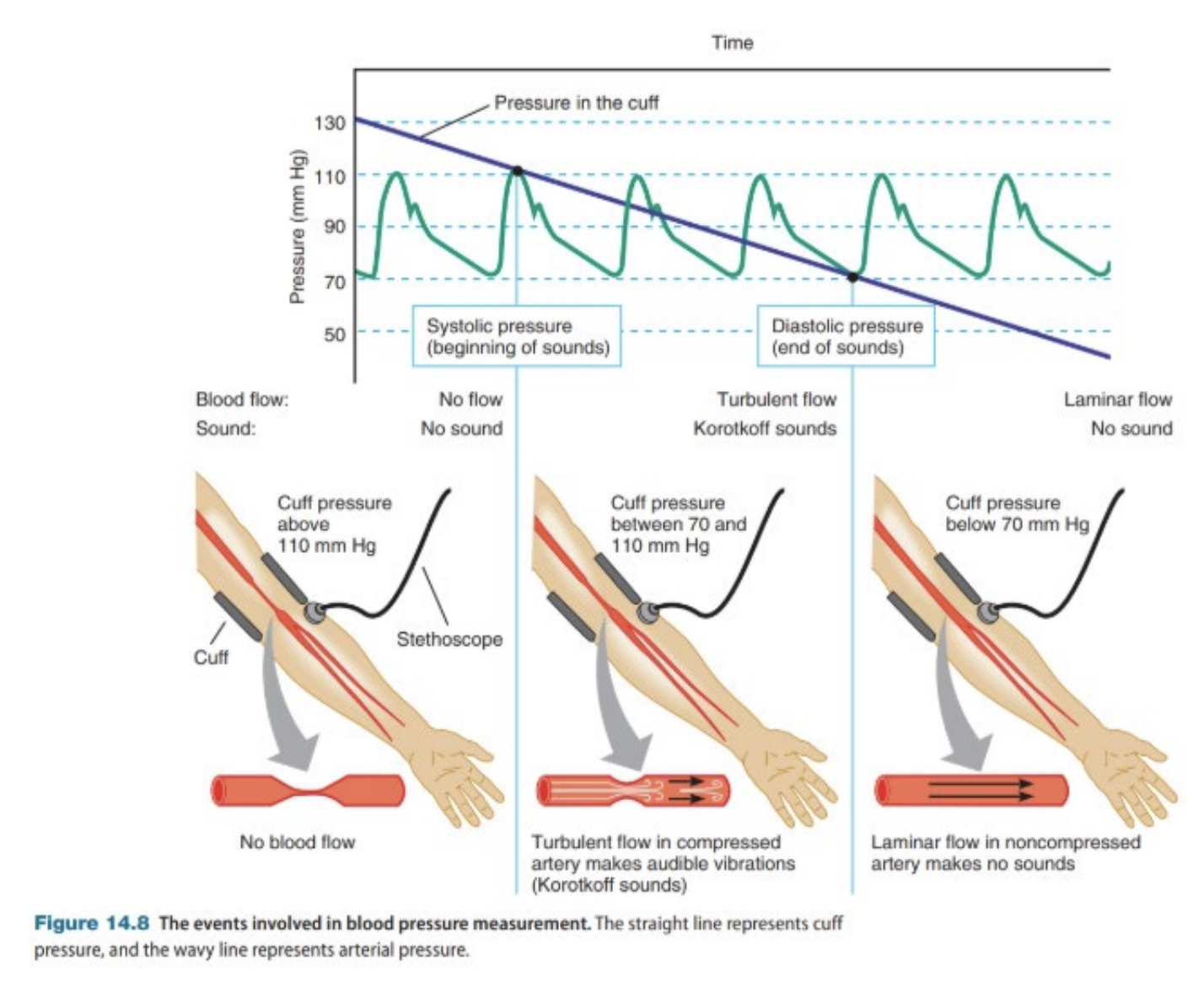
Blood pressure
Force of blood pushing against the walls
Systolic pressure: When the ventricles contract
Distolic pressure: When the heart relaxes
Normal blood pressure is around 120/80mmHg
Baroreceptors (pressure sensors in arteries) that detect changes and adjust heart rate and vessel size
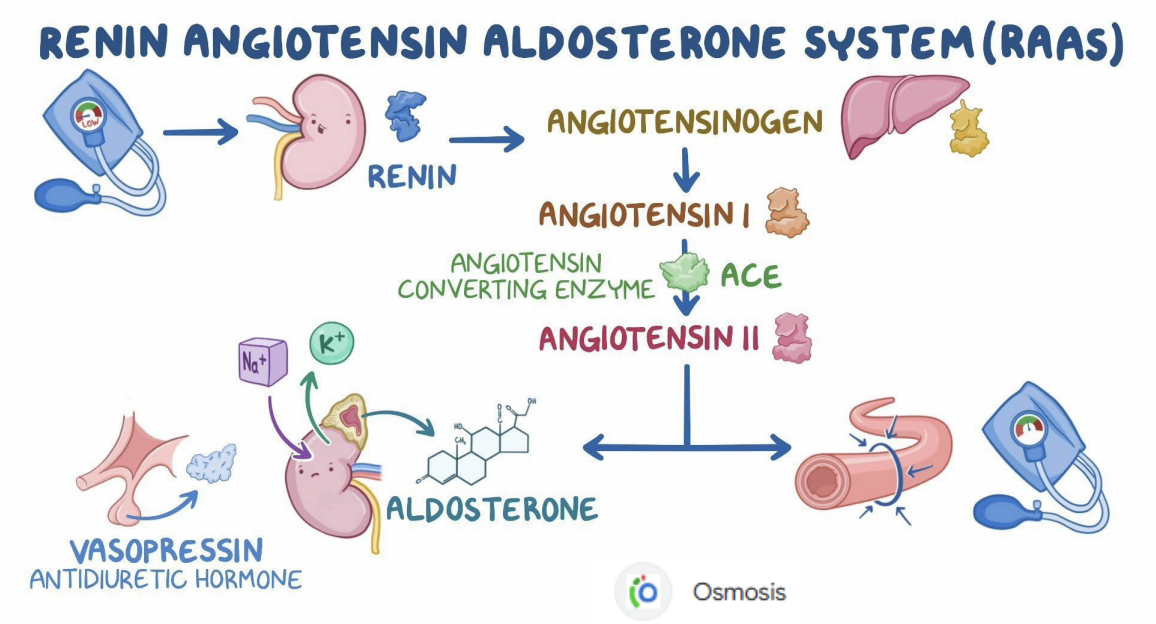
Hormonal control, like the renin-angiotensin system, which helps raise BP when needed
Mean Arterial Pressure (MAP)
Mean Arterial Pressure (MAP) influences blood flow to all organs in the systemic circuit
MAP is a weighted mean
Diastolic pressure is given twice the weight of systolic pressure
During a single cardiac cycle, aortic pressure is near its maximum for a relatively short period and is closer to the minimum about twice as long
MAP = Diastolic BP + 1/3 (Systolic BP−Diastolic BP)
Mean Arterial Pressure = HR X SV X Total Peripheral Resistance
MAP = HR X SV X TPR
If resistance is high, the heart has to work harder
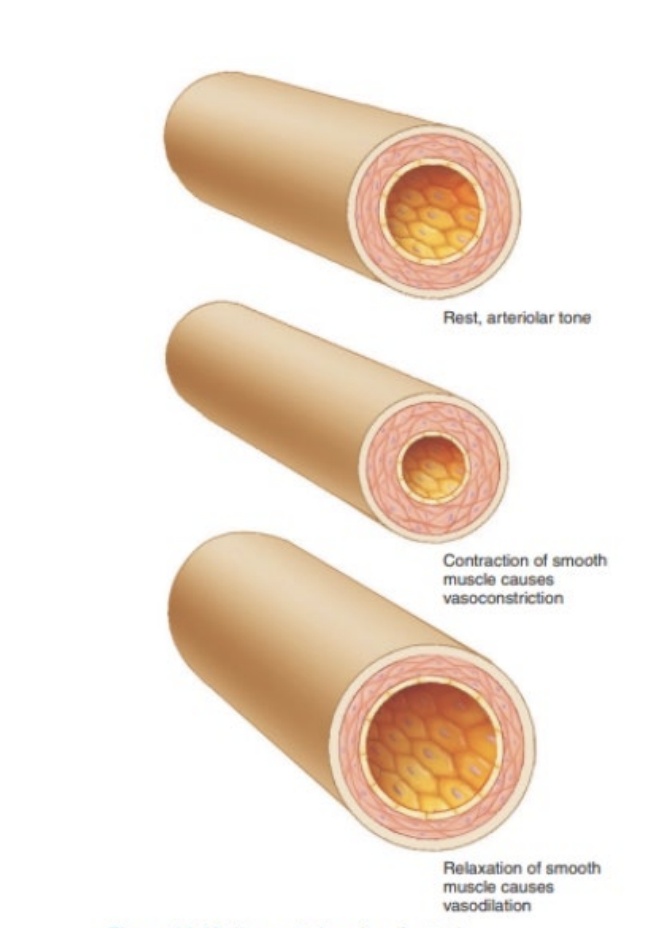
Vessel diameter
Vasoconstriction increases resistance
Vasodilatation decreases resistance
Viscosity and Turbulence
Functions of the Respiratory System
Regulation of pH in the blood
Vocalisation
Defence against pathogens and foreign particles in the airways
Providing a route for water and heat loss
Enhancing venous return
Activating plasma proteins as they pass through the pulmonary circulation
Upper Respiratory System
Air passages in the head and neck
Air & food enter the nasal or oral cavity and goes to the pharynx.
Air enters the first structure in the respiratory tract, the larynx
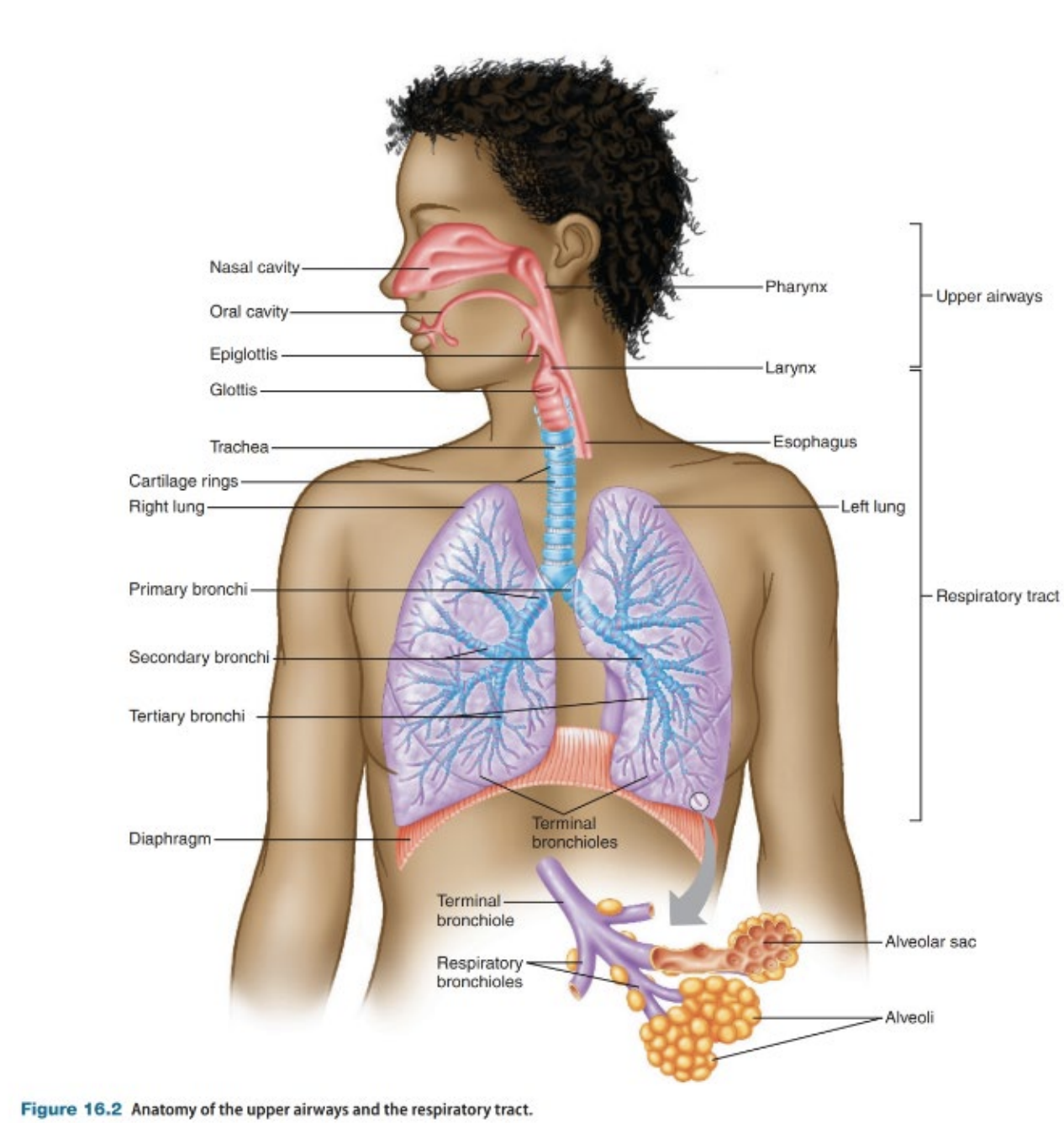
Respiratory tract
All air passages from the pharynx to the lungs
Two parts
The conducting zone
The respiratory zone
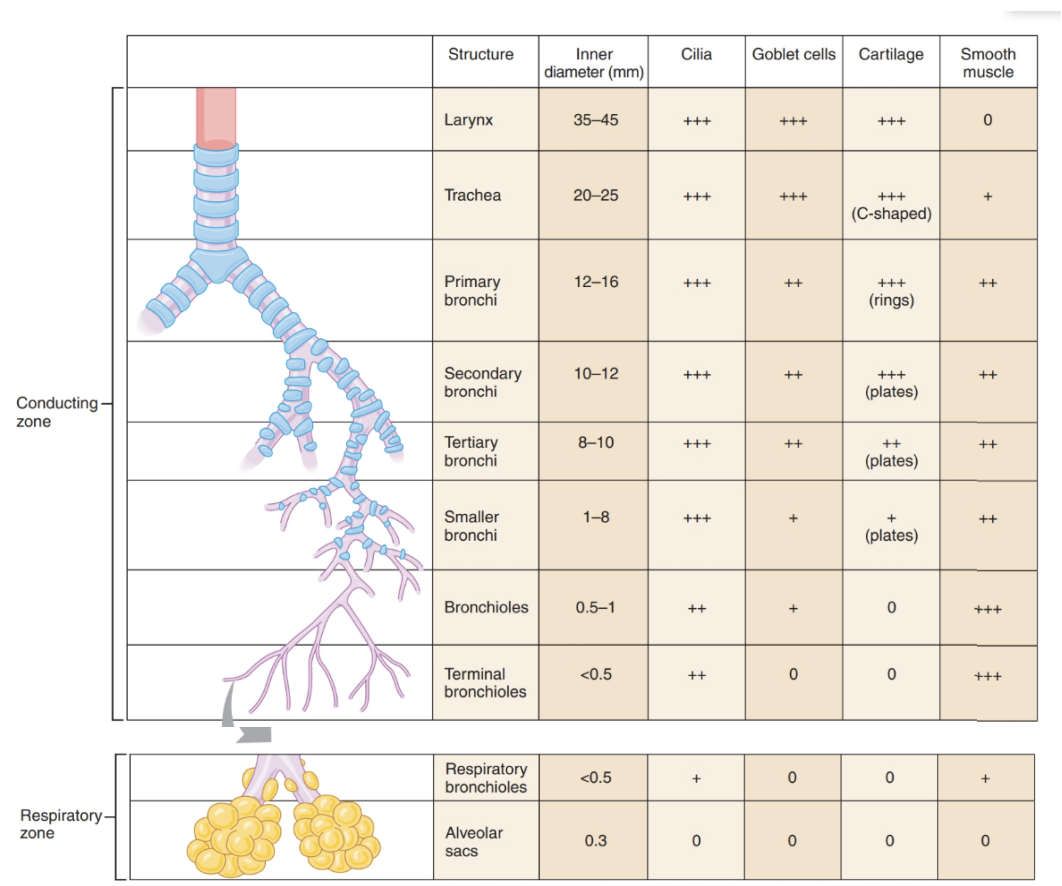
The Conducting Zone
The upper part
Conducts air from the larynx to the lungs
Allows air to enter and exit the respiratory zone
Holds 150ml and is considered dead space.
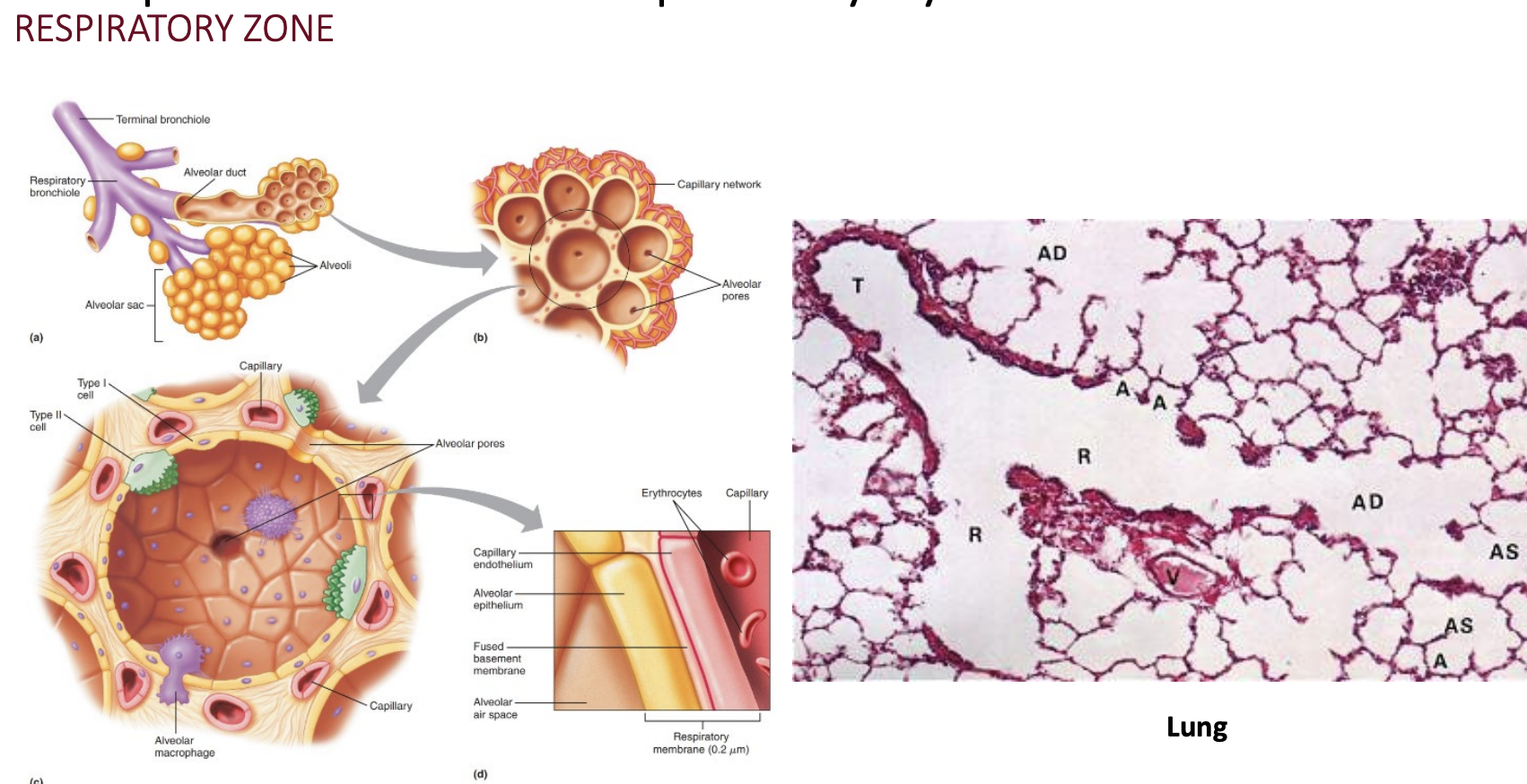
The Respiratory Zone
The lower part where gas exchange occurs.
Thinner walls for gas exchange
Large SA for diffusion of oxygen.
Alveolus: Single layer of epithelial cells (type I) overlying the basement membrane.
Capillary wall: A single layer of endothelial cells underlying the basement membrane.
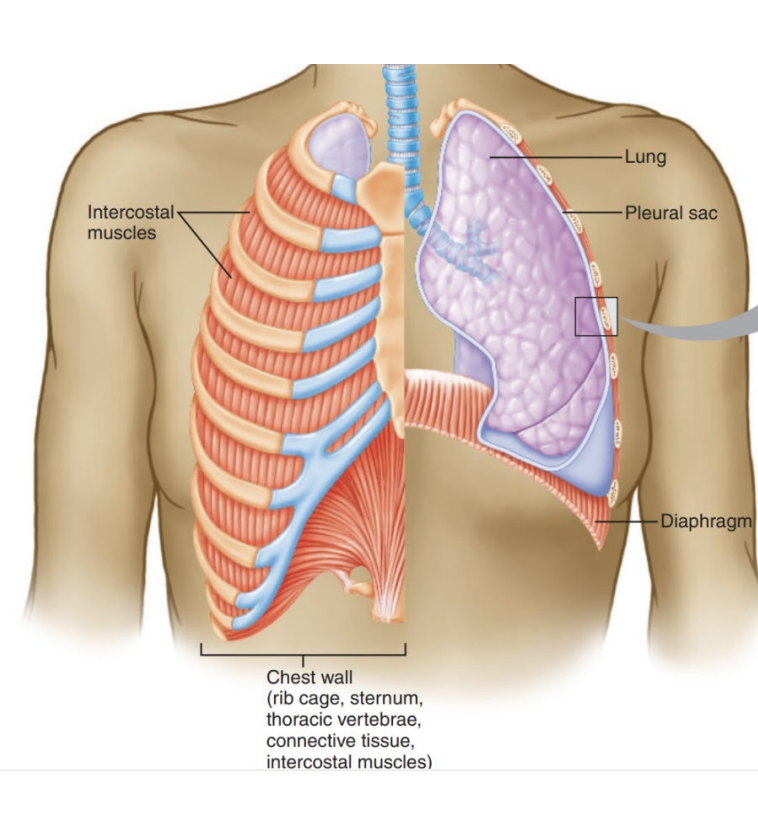
Structures that protect the lungs
Rib cage
Sternum
Thoracic vertebrae
Associated muscles and connective tissue (primarily hyaline cartilage).
Muscles of the chest wall are responsible for breathing
Internal intercostals - push air out
External intercostals - entry of air
Diaphragm
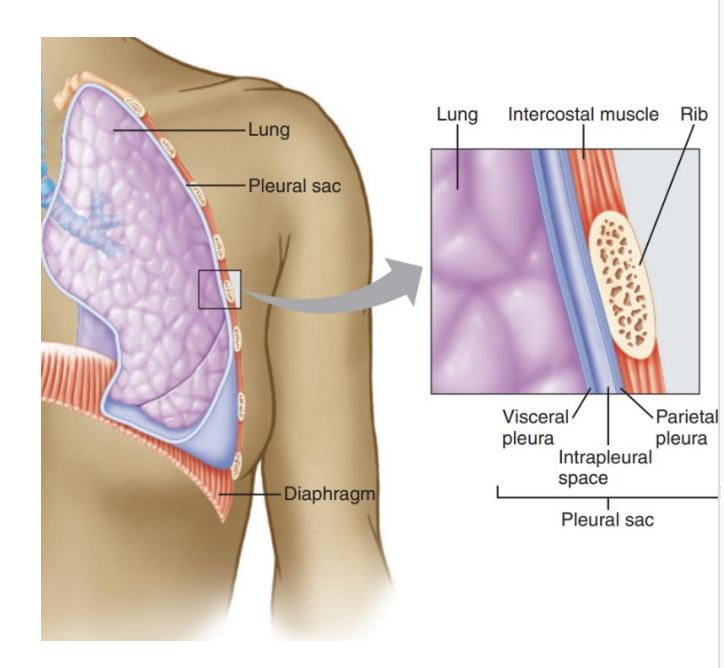
Structure of the lungs
The chest wall forms an airtight, continuous barrier around the lungs
The pleura (epithelial cells and connective tissue) line the interior chest wall and the external surface.
Each lung has a separate pleural sac
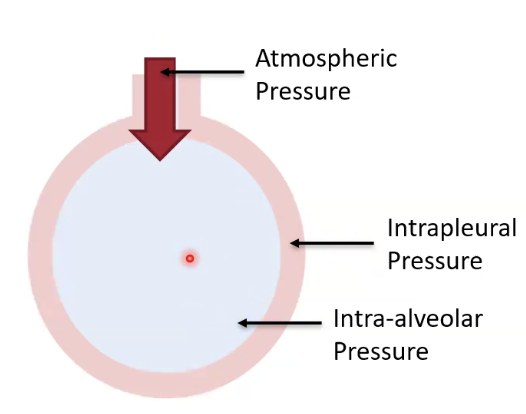
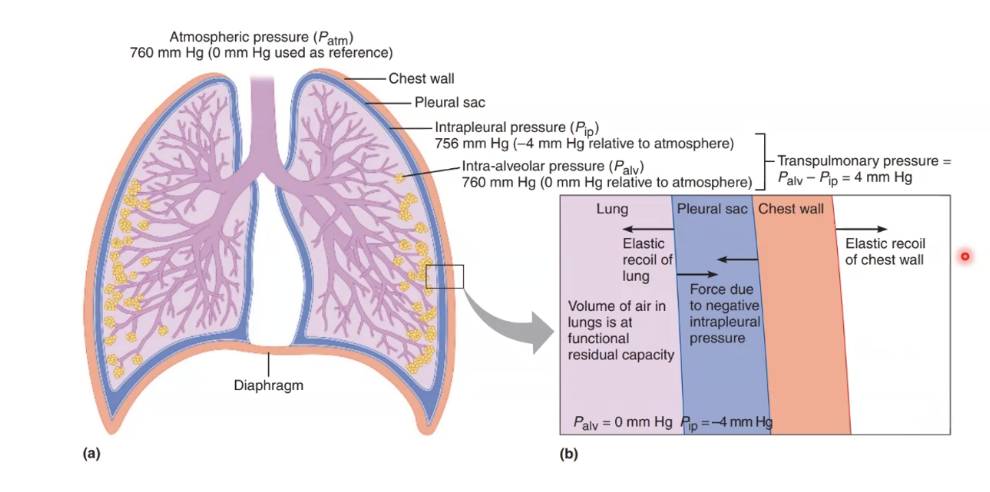
The visceral pleura is the first layer, and then we have the intrapleural space, and then the parietal pleura on top, lining the chest wall (muscles).
Intraplural space makes sure the pleurae are always connected by liquid so the lungs will expand and contact with the muscles.
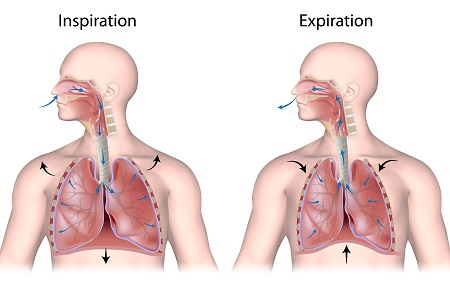
Inspiration
The Diaphragm and external intercostals contract and air flows into the lungs.
Thoracic cavity expands, increasing lung volume and decreasing internal pressure
Pressure gradient is created, where atmospheric pressure is higher than lung pressure and air flows into the lungs to account for the difference.
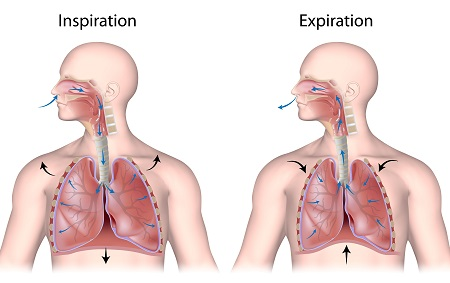
Expiration
The diaphragm relaxes, the external intercostals contract, and air flows out of the lungs.
Thoracic cavity decreases in volume, increasing lung pressure.
Lung pressure is higher than atmospheric pressure, forcing air out of the lungs.
Pressure Gradients
The pressure gradient between the alveoli and the atmosphere causes the air to flow out.
This is produced by the action of inspiratory muscles and the lung's elastic recoil.
Atmospheric pressure 0mm Hg
Intraplural pressure -4 mm Hg
Intra-alveolar pressure 0 mm Hg - changes during expansion and contraction